Pathophysiology > EXAM > BIOLOGY BIO 1150 Intro to Pathophysiology. Exam 25 Most Common Questions and Answers. (All)
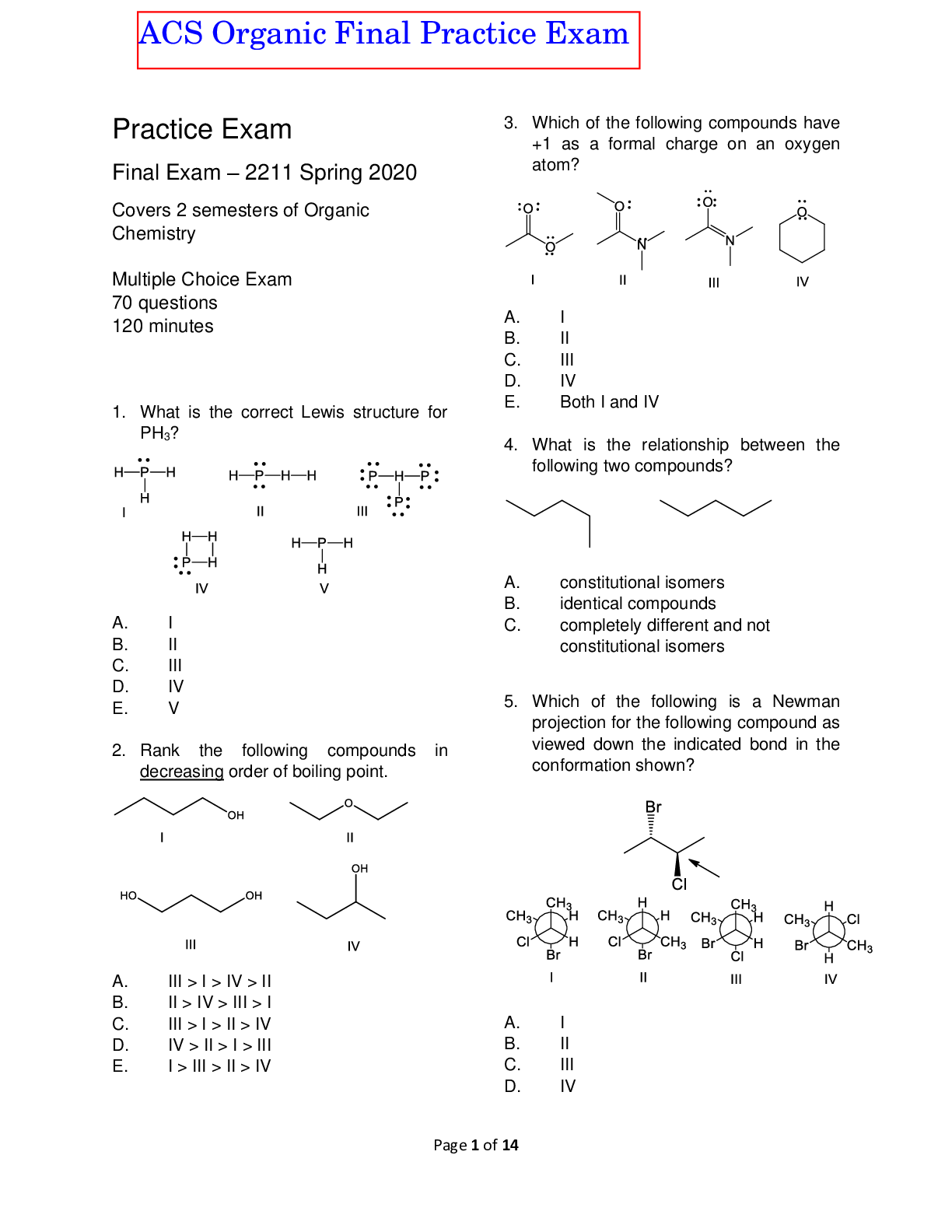
BIOLOGY BIO 1150 Intro to Pathophysiology. Exam 25 Most Common Questions and Answers.
Document Content and Description Below
Pathophysiology BIO 1150 Exam Question and Answers Questions Answered step-by-step What do we do when a good tPA candidate fails IV tPA? Know... 1. What do we do when a good tPA candidate fails I... V tPA? Know intraarterial tPA and when do we use it. Know thrombectomy and when we use it. 2. Once a patient has a TIA or CVA, how do we prevent further strokes? Reduce risks like further embolic events or a thrombotic event with anticoagulation or carotid endarterectomy and know common anticoagulants used like dabigatran or Pradaxa, dipyridamole or Aggrenox. 3. Know the contraindications to tPA. They usually deal with increased bleeding risks. 4. Know your neurotransmitters: Serotonin, dopamine, acetylcholine, gamma amino butyric acid or GABA. What diseases can manifest if there are issues with these neurotransmitters? For example, Tourette's syndrome can come about from problems with dopamine, but so can Parkinson's disease. 5. How is athetosis related to Huntington's disease? 6. What is the pathophysiological cause of multiple sclerosis or MS? 7. How do you treat MS? 8. What is a polysomnogram? 9. How can you best see if a patient has a narrowing of the spinal cord or spinal stenosis? Which imaging modality is best for this? What if the patient has metal in the body and cannot undergo MRI? 10. Define and be able to recognize the signs and symptoms of: Epilepsy, cluster headache, Parkinson's disease, tension headache, Huntington's chorea, 11. What is Babinski's reflex, when do we use it and what is a positive response? 12. What is prodrome or aura, interictal and post ictal mean when it comes to epilepsy? 13. A patient is unconscious, what would you monitor on them to assess the cause? 14. What is Guillain-Barre syndrome and what usually causes it? This is a very rare condition usually comes from having a bacterial or viral infection and is an autoimmune attack of the nervous system. It begins with very distal neurosensory and motor loss and then makes its way to the body trunk if more severe. The patient may need a ventilator for a period till they recover. They will need good physical and occupational therapies as well. Some more severe cases can go into shock, so monitoring their hemodynamics is very crucial. 15. What are the risk factors, symptoms, and treatments for migraine? Who gets migraine most often? Men versus women and young or old? 16. Huntington's disease is a dominant genetic disease, but does not manifest till the patient is about middle aged, how could you tell if a patient will develop this disease later in life? Think genetic testing. 17. If a patient has damage to part of the brain from trauma, what will their symptoms be? This is based on where they were injured, for example, if they damaged the cerebellum, then they would have issues with balance and coordination. 18. What is amyotrophic lateral sclerosis and how is it treated? 19. What is multiple sclerosis and what is the pathophysiology of this disease? 20. Why do we do Babinski's reflex? Know a patient with this reflex positive is very sick if they are an adult, but it is normal for a baby to have this reflex positive. Positive is a flaring of the toes in response to stimulation of the sole of the foot. 21. What is neurogenic shock? What are the signs, pathophysiology, and symptoms? 22. What is the motor testing score from 1 to 5? 23. If a patient had an MVA causing damage between C1 and C3, what would be the symptoms? Quadriplegia and likely needs the ventilator to live. What about between C4 and C7? The patient would have some arm movement and not need the ventilator, but still with bladder and bowel incontinence and unable to sit up on their own. Thoracic spine damage in same patient? Paraplegia but also loss of trunk movement and still with bladder and bowel incontinence. What about lumbar and sacral spinal injury? Loss of movement and sensation in legs, but able to sit up on their own and may have some leg movement. Basically, the patient gains function the lower the injury as the nerves that come off the spine have communication with the brain. The lower the injury, the better the outcome. 24. Myelography is used to see injury to CSF flow, MRI is the best image of the nerves of the spine, and CT shows the bones of the vertebrae best for fractures etc. 25. Know Brown-Sequard syndrome, cauda equina syndrome, Horner's syndrome, and conus medullaris syndrome. How do patient's present with these conditions? Know your skull fractures: Linear, basilar, and depressed. Which one of these cannot cause meningeal damage or significant brain injury? Which one is associated [Show More]
Last updated: 2 years ago
Preview 1 out of 15 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$6.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Apr 12, 2022
Number of pages
15
Written in
Additional information
This document has been written for:
Uploaded
Apr 12, 2022
Downloads
0
Views
154





.png)


.png)