Focused Exam: Cough Results | Graded A)
Document Content and Description Below
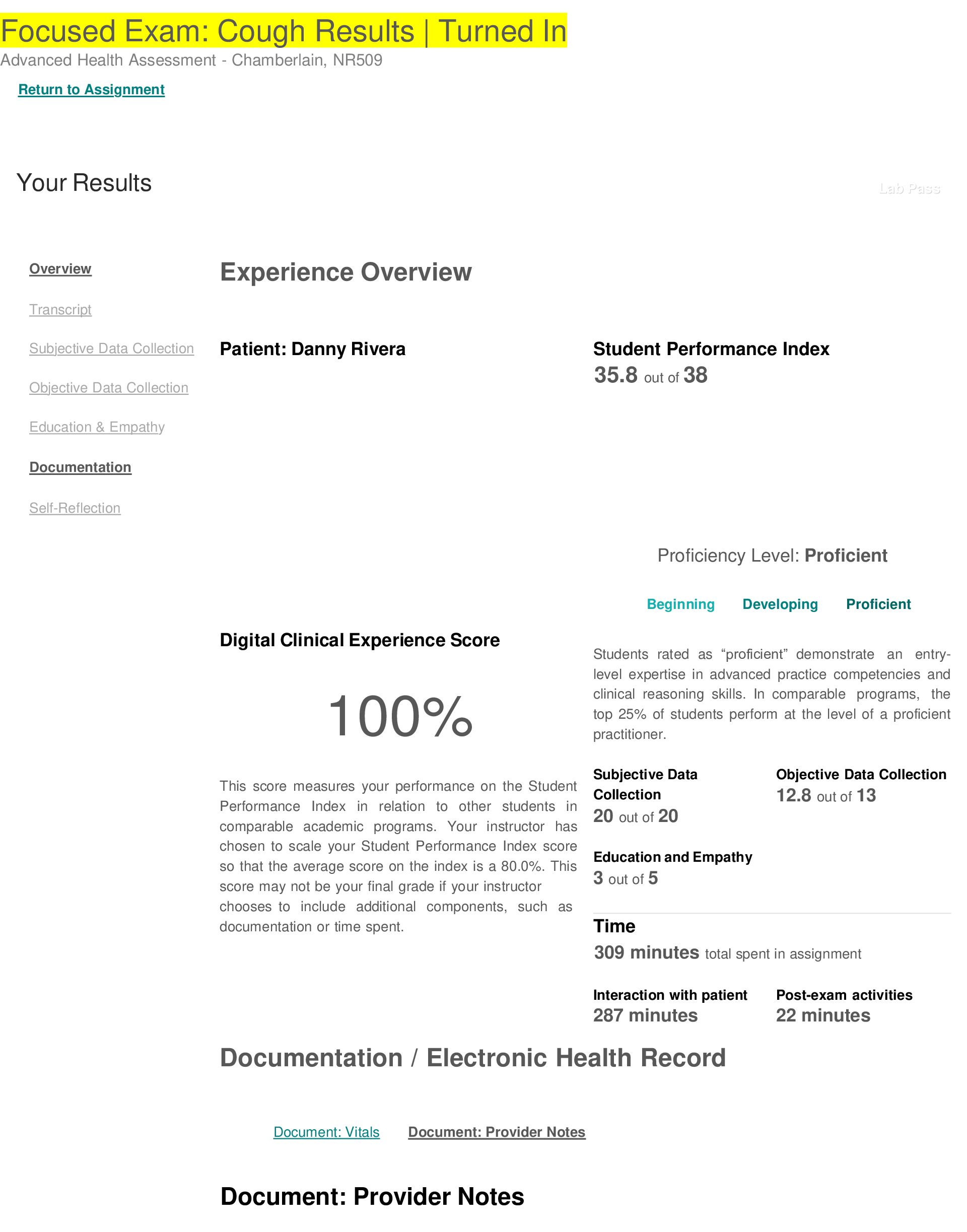
Focused Exam: Cough Results | Turned In Advanced Health Assessment - Chamberlain, NR509 Return to Assignment Your Results Lab Pass Overview Transcript Subj ... ective Data Collection Objective Data Collection Experience Overview Patient: Danny Rivera Student Performance Index 35.8 out of 38 Education & Empathy Documentation Self-Reflection Proficiency Level: Proficient Digital Clinical Experience Score 100% Beginning Developing Proficient Students rated as “proficient” demonstrate an entry- level expertise in advanced practice competencies and clinical reasoning skills. In comparable programs, the top 25% of students perform at the level of a proficient practitioner. This score measures your performance on the Student Performance Index in relation to other students in comparable academic programs. Your instructor has chosen to scale your Student Performance Index score so that the average score on the index is a 80.0%. This score may not be your final grade if your instructor Subjective Data Collection 20 out of 20 Education and Empathy 3 out of 5 Objective Data Collection 12.8 out of 13 chooses to include additional components, such as documentation or time spent. Time 309 minutes total spent in assignment Interaction with patient 287 minutes Documentation / Electronic Health Record Post-exam activities 22 minutes Document: Vitals Document: Provider Notes Document: Provider Notes Subjective CC: Cough HPI Onset: 4-5 days ago Location: right ear pain Duration: "a couple of minutes" Characteristics: sore throat (mild), fatigue Aggravating factors: night time Relieving factors: cough syrup Treatment: OTC cough syrup Current medications: multivitamins and cough syrup Allergies: none PMHx: pneumonia, frequent ear infections during early childhood Social Hx: The patient lives with his mother, father, and maternal grandmother and grandfather. Father sometimes smoke in the house. Family Hx: Father had asthma as a child and is a current positive smoker. Maternal grandfather also has a smoking history and diagnosed with eczema. ROS Constitutional: Positive for fatigue related to cough that keeps him up at night. Denies night sweats, fevers, chills, and weight loss. HEENT: Denies headaches and dizziness. Denies nosebleeds. Positive for right ear pain. Denies ear drainage. Positive for clear nasal discharge. Denies eye redness, watery eyes, eye pain and visual disturbances. Positive for sore throat. Cardiac: Denies chest pain and tightness Resp: Positive for dry cough. Denies shortness of breath. GI: Denies nausea, vomiting, diarrhea. Denies abdominal pain and discomfort. Last BM was today before school. Danny reports a cough lasting four to five days. He describes the cough as “watery and gurgly.” He reports the cough is worse at night and keeps him up. He reports general fatigue due to lack of sleep. He reports pain in his right ear. He is experiencing mild soreness in his throat. He reports his mother treated his cough symptoms with over-the-counter medicine, but it was only temporarily effective. He reports frequent cold and runny nose, and he states that he had frequent ear infections as a child. He reports a history of pneumonia in the past year. He reports normal bowel movements. He denies fever, headache, dizziness, trouble swallowing, nosebleed, phlegm or sputum, chest pain, trouble breathing and abdominal pain. He denies cough aggravation with activity. Objective Danny Rivera is an 8 year old Puerto Rican male who presents to the clinic with a cough. He is alert He is answering questions appropriately. He is in no acute distress. • General Survey: Fatigued appearing young boy seated on nursing station bench. Appears stable. HEENT: Head is normocephalic and atraumatic. Sclera white, conjunctive moist and pink with no drainage. Right ear positive for pain. Inflammation and redness noted in right tympanic membrane. Nasal cavities pink, patent with clear drainage. Negative for tenderness on palpation at frontal and maxillary sinuses. Oral mucosa moist and pink. Erythema noted to tonsils. Posterior throat is red with cobblestoning. Right sided cervical lymph nodes are tender on palpation. Resp: Lung sounds are present and clear on auscultation in all lobes. Positive dry cough. Positive tachypnea. Negative for bronchophony. Chest wall is symmetrical and resonant in all areas on percussion. No areas of dullness noted. Fremitus symmetrical and equal bilaterally on palpation. Spirometry result: FEV1/FEVC 80.5% Cardio: S1 and S2 heart sounds on auscultation. No murmurs, rubs, or gallops detected. • HEENT: Mucus membranes are moist, clear nasal discharge. Redness, cobblestoning in the back of throat. Eyes are dull in appearance, pink conjunctiva. Right Tympanic membrane is red and inflamed. Right cervical lymph node enlarged with reported tenderness. • Cardiovascular: S1, S2, no murmurs, gallops or rubs. • Respiratory: Respiratory rate increased, but no acute distress. Able to speak in full sentences. Breath sounds clear to auscultation. Negative bronchophony. Chest wall resonant to percussion. Expected fremitus, equal bilaterally. Spirometry: FEV1: 3.15 L, FVC 3.91L (FEV1/FVC: 80.5%) Assessment Cough/Viral rhinitis- dry cough for 4-5 days, sore throat Strep throat- throat redness, tenderness, and cobblestoning Viral respiratory infection- clear nasal discharge and dry cough Asthma- cough, fatigue, frequent exposure to cigarette smoke. Allergies: clear nasal drainage Cough. Differential diagnoses include cold, strep throat, rhinitis, allergies, and asthma Plan Diagnostics: Order rapid strep test to rule out strep throat. Order sputum culture to rule out an respiratory infection. Consider ordering WBC and PFTs to help rule out asthma. Medication: Order antibiotics if rapid strep test is positive. Order robutussin DM 5mL every 6 hours PRN for cough for five days, do not administer more than 40mL a day. Order claritin (chewable tabs) 5mg twice daily for five days. Education: Educate patient to increase fluids. Educate patient to wash his hands frequently, demonstrate appropriate technique and assess return demonstration. Educate patient's mother to wash bed linen weekly. Educate patient to avoid areas of smoke exposure. Educate and emphasize to the adult family members on the importance of not smoking in the house or in any area that the child will likely experience exposure. Educate Diagnostics • Implement Centor criteria assessment • Obtain rapid strep test Medication • Pending rapid strep test results, may order appropriate antibiotic therapy • Initiate Rx or OTC antitussive therapy at bedtime for 10 days Education • Educate caregiver and patient to minimize exposure to allergens, practice good hand washing, and recommend cleaning bed sheets weekly • Request no smoking in house Referral/Consultation • Refer to allergy specialist for allergy testing • Refer for lung function testing to rule out asthma fever >101.5, chest pain or tightness, shortness of breath, and dizziness. Follow-up Planning • Instruct caregiver and patient to seek immediate Referral/Consultation: Refer patient to ENT specialist for allergy testing. Refer patient to an pulmonologist or asthma specialist to rule out asthma. Follow-up: Have family bring patient back to the clinic in 7-10 days for follow-up. medical attention if high fever, shortness of breath, chest pain, and dizziness or faintness • Revisit clinic in 1-2 weeks for follow up and evaluation Comments If your instructor provides individual feedback on this assignment, it will appear here. © Shadow Health® 2018 [Show More]
Last updated: 3 years ago
Preview 1 out of 4 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$10.50
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Aug 05, 2021
Number of pages
4
Written in
All
Additional information
This document has been written for:
Uploaded
Aug 05, 2021
Downloads
0
Views
112







.png)
.png)