*NURSING > STUDY GUIDE > N5315 Advanced Pathophysiology Gastrointestinal Best Study Guide Ever Already Graded A+ (All)
N5315 Advanced Pathophysiology Gastrointestinal Best Study Guide Ever Already Graded A+
Document Content and Description Below
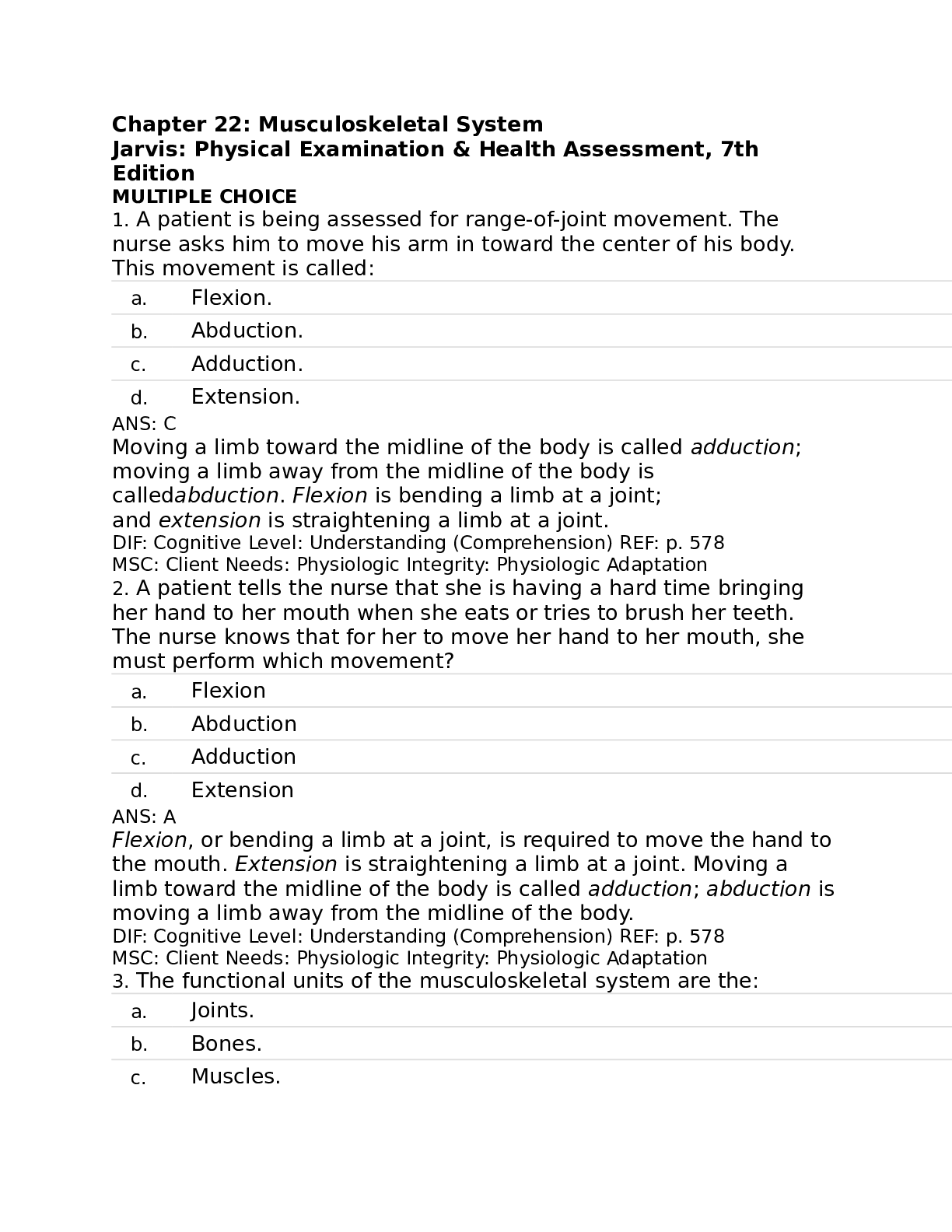
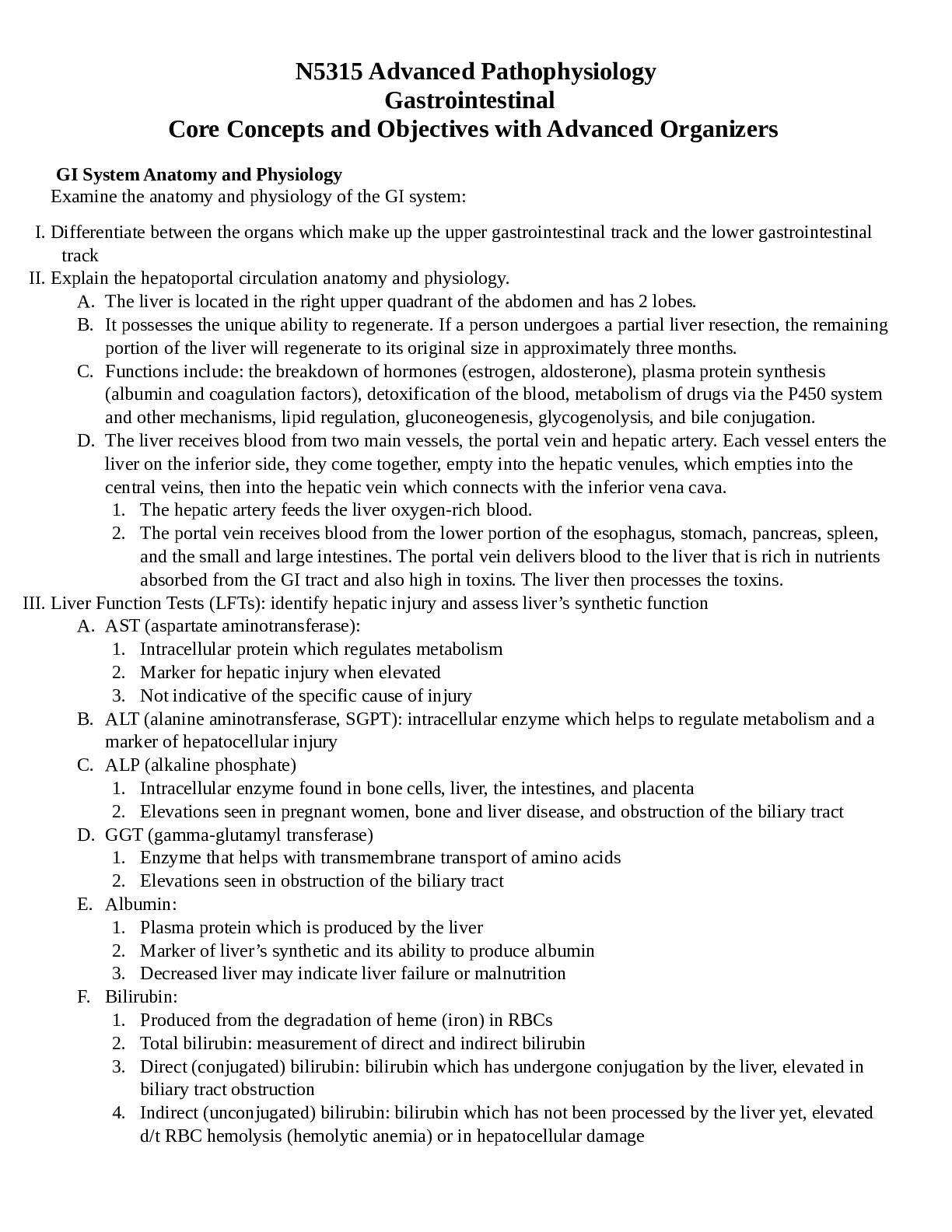
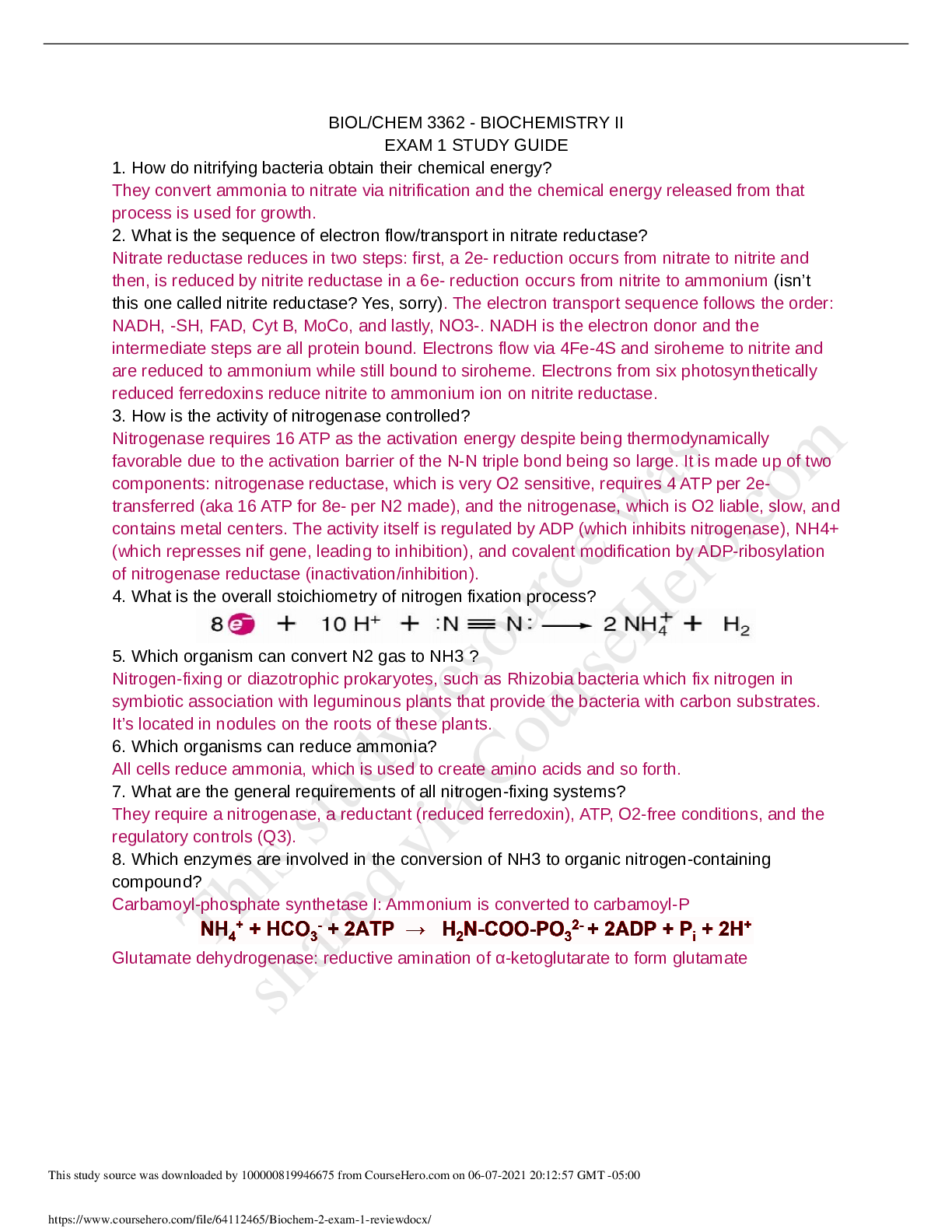
GI System Anatomy and Physiology Examine the anatomy and physiology of the GI system: I. Differentiate between the organs which make up the upper gastrointestinal track and the lower gastrointestina... l track II. Explain the hepatoportal circulation anatomy and physiology. A. The liver is located in the right upper quadrant of the abdomen and has 2 lobes. B. It possesses the unique ability to regenerate. If a person undergoes a partial liver resection, the remaining portion of the liver will regenerate to its original size in approximately three months. C. Functions include: the breakdown of hormones (estrogen, aldosterone), plasma protein synthesis (albumin and coagulation factors), detoxification of the blood, metabolism of drugs via the P450 system and other mechanisms, lipid regulation, gluconeogenesis, glycogenolysis, and bile conjugation. D. The liver receives blood from two main vessels, the portal vein and hepatic artery. Each vessel enters the liver on the inferior side, they come together, empty into the hepatic venules, which empties into the central veins, then into the hepatic vein which connects with the inferior vena cava. 1. The hepatic artery feeds the liver oxygen-rich blood. 2. The portal vein receives blood from the lower portion of the esophagus, stomach, pancreas, spleen, and the small and large intestines. The portal vein delivers blood to the liver that is rich in nutrients absorbed from the GI tract and also high in toxins. The liver then processes the toxins. III. Liver Function Tests (LFTs): identify hepatic injury and assess liver’s synthetic function A. AST (aspartate aminotransferase): 1. Intracellular protein which regulates metabolism 2. Marker for hepatic injury when elevated 3. Not indicative of the specific cause of injury B. ALT (alanine aminotransferase, SGPT): intracellular enzyme which helps to regulate metabolism and a marker of hepatocellular injury C. ALP (alkaline phosphate) 1. Intracellular enzyme found in bone cells, liver, the intestines, and placenta 2. Elevations seen in pregnant women, bone and liver disease, and obstruction of the biliary tract D. GGT (gamma-glutamyl transferase) 1. Enzyme that helps with transmembrane transport of amino acids 2. Elevations seen in obstruction of the biliary tract E. Albumin: 1. Plasma protein which is produced by the liver 2. Marker of liver’s synthetic and its ability to produce albumin 3. Decreased liver may indicate liver failure or malnutrition F. Bilirubin: 1. Produced from the degradation of heme (iron) in RBCs 2. Total bilirubin: measurement of direct and indirect bilirubin 3. Direct (conjugated) bilirubin: bilirubin which has undergone conjugation by the liver, elevated in biliary tract obstruction 4. Indirect (unconjugated) bilirubin: bilirubin which has not been processed by the liver yet, elevated d/t RBC hemolysis (hemolytic anemia) or in hepatocellular damage IV. Discuss the effects of aging on the gastrointestinal tract. Examine the pathologic basis of adult and pediatric disorders which affect the GI system: Gastrointestinal Bleeds V. Analyze the etiologies and pathophysiology of osmotic, secretory, and motility related diarrhea. Type of Diarrhea Etiology Pathophysiology Osmotic Secretory Motility VI. Analyze the etiology, clinical manifestations, and pathophysiology of the upper and lower GI bleed and describe the implications this has for your clinical practice as a nurse practitioner. Disease Etiology Clinical Manifestations Pathophysiology Upper GI Bleed Commonly caused by bleeding varices (varicose veins) in the esophagus or stomach, peptic ulcers, gastritis, or a Mallory-Weis tear (tearing of the esophagus from the stomach) Characterized by frank, bright red, or “coffee ground” (affected by the stomach) emesis Hematemesis: bright, red bloody emesis, usually required emergent intervention Coffee ground emesis: not necessary emergent Shock: decreased cardiac output, hypotension, acute renal failure, tachycardia, and anemia Any source of bleeding which occurs in the esophagus, stomach, or the duodenum If left untreated or if severe may lead to shock GI bleeds are very common in individuals with cirrhosis Three etiologies of an upper GI bleed which are specific to individuals with cirrhosis: esophageal varices, portal hypertensive gastropathy (PHG), and gastric antral vascular ectasia (GAVE) Some research which suggests that GI bleeds in persons with cirrhosis may be caused by a bacterial infection, recommended that antibiotic therapy be added to the standard therapy for GI bleeds in individuals with cirrhosis Lower GI Bleed Occult GI bleed: commonly associated with colon cancer, stools must be tested for blood Hematochezia: presence of bright red blood in the stools, usually suggests bleed in rectum, sigmoid colon, or descending colon Any source bleeding in the jejunum, ileum, and color, or rectum Occult GI bleed: not visible and results in iron deficiency May lead to shock [Show More]
Last updated: 2 years ago
Preview 1 out of 12 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$12.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Sep 04, 2021
Number of pages
12
Written in
Additional information
This document has been written for:
Uploaded
Sep 04, 2021
Downloads
0
Views
100










.png)
.png)



.png)