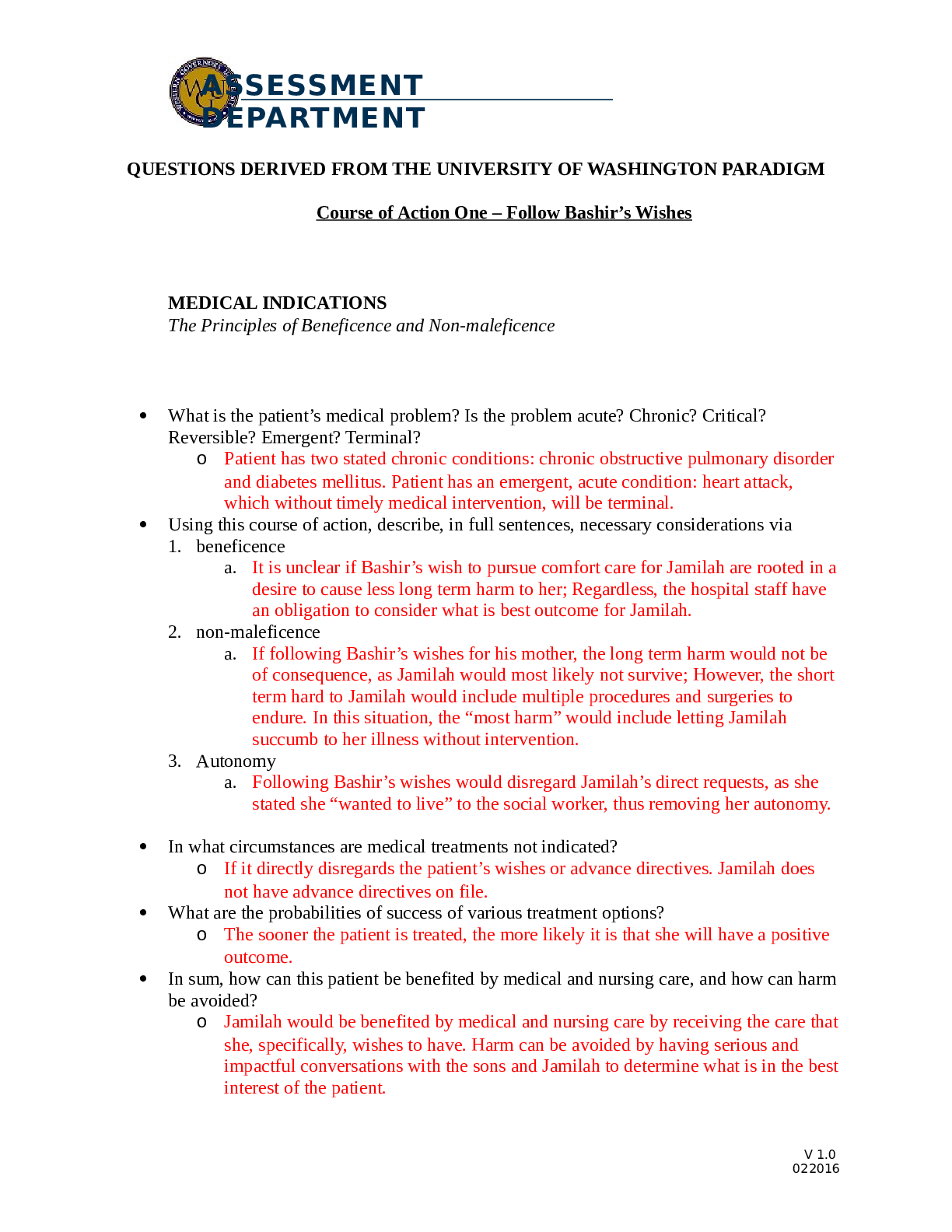
MEDICAL INDICATIONS
The Principles of Beneficence and Non-maleficence
What is the patient’s medical problem? Is the problem acute? Chronic? Critical?
Reversible? Emergent? Terminal?
o Patient has two stated chronic
...
MEDICAL INDICATIONS
The Principles of Beneficence and Non-maleficence
What is the patient’s medical problem? Is the problem acute? Chronic? Critical?
Reversible? Emergent? Terminal?
o Patient has two stated chronic conditions: chronic obstructive pulmonary disorder
and diabetes mellitus. Patient has an emergent, acute condition: heart attack,
which without timely medical intervention, will be terminal.
Using this course of action, describe, in full sentences, necessary considerations via
1. beneficence
a. It is unclear if Bashir’s wish to pursue comfort care for Jamilah are rooted in a
desire to cause less long term harm to her; Regardless, the hospital staff have
an obligation to consider what is best outcome for Jamilah.
2. non-maleficence
a. If following Bashir’s wishes for his mother, the long term harm would not be
of consequence, as Jamilah would most likely not survive; However, the short
term hard to Jamilah would include multiple procedures and surgeries to
endure. In this situation, the “most harm” would include letting Jamilah
succumb to her illness without intervention.
3. Autonomy
a. Following Bashir’s wishes would disregard Jamilah’s direct requests, as she
stated she “wanted to live” to the social worker, thus removing her autonomy.
In what circumstances are medical treatments not indicated?
o If it directly disregards the patient’s wishes or advance directives. Jamilah does
not have advance directives on file.
What are the probabilities of success of various treatment options?
o The sooner the patient is treated, the more likely it is that she will have a positive
outcome.
In sum, how can this patient be benefited by medical and nursing care, and how can harm
be avoided?
o Jamilah would be benefited by medical and nursing care by receiving the care that
she, specifically, wishes to have. Harm can be avoided by having serious and
impactful conversations with the sons and Jamilah to determine what is in the best
interest of the patient.
V 1.0
022016
ASSESSMENT
DEPARTMENTPATIENT PREFERENCES
The Principle of Respect for Autonomy
Has the patient been informed of benefits and risks, understood this information, and
given consent?
o It is unclear if the patient has been informed, due to the language and cultural
barrier. If the son is refusing medical treatment, it is unlikely the patient has given
consent on any further treatment beyond comfort care.
Is the patient mentally capable and legally competent, and is there evidence of
incapacity?
o There is not stated evidence of incapacity.
If mentally capable, what preferences about treatment is the patient stating?
o Patient’s statement was vague, but indicated that she would like to pursue
treatment.
If incapacitated, has the patient expressed prior preferences?
o As stated above, the patient has not expressed clear and concise preferences on
how she would like treatment to proceed. The patient does not have any advance
directives on file to follow.
Who is the appropriate surrogate to make decisions for the incapacitated patient?
o Bashir was listed as the emergency contact at the extended care facility and has
elected himself as the primary decision maker; However, it is unclear if he is the
most appropriate surrogate to make decisions for Jamilah, if she is incapacitated.
Is the patient unwilling or unable to cooperate with medical treatment? If so, why?
o Patient seems willing to proceed with medical treatment.
QUALITY OF LIFE
The Principles of Beneficence, Non-maleficence, and Respect for Autonomy
What are the prospects, with or without treatment, for a return to normal life, and what
physical, mental, and social deficits might the patient experience even if treatment
succeeds?
o Without treatment, patient will most likely expire in less than a week. Due to
Jamilah’s age and disease state(s), she may or may not regain all physical, mental,
and social functionality.
On what grounds can anyone judge that some quality of life would be undesirable for a
patient who cannot make or express such a judgment?
o An advance directive can be used in this situation to meet a patient’s wishes. If
advance directive is not file, this type of decision will most likely be made
between the physician/provider and the patient’s family
[Show More]