*NURSING > EXAM REVIEW > NR601 Final Exam Study Guide ALL ANSWERS FALL-2021 LATEST SOLUTION 100% GUARANTEED GRADE A+ (All)
NR601 Final Exam Study Guide ALL ANSWERS FALL-2021 LATEST SOLUTION 100% GUARANTEED GRADE A+
Document Content and Description Below
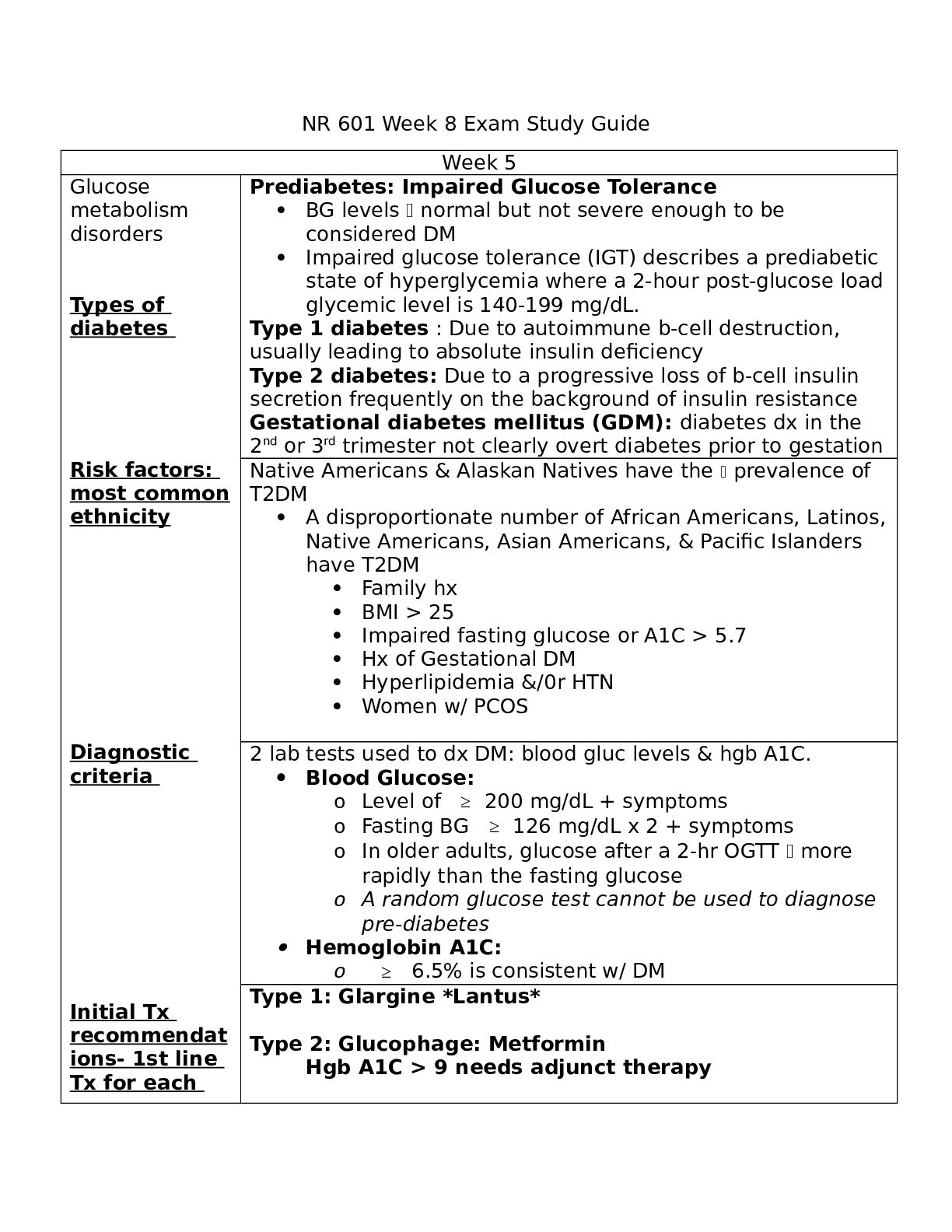
Islet cell-specific antibodies may be identified in 70-80% of people with prediabetes & those newly dx with DM1 and hyperglycemia typically develops once 80-90% of beta cells have been destroyed. In ... Type I diabetes, an auto-immune attack on the beta cells of the pancreas prevents the production and secretion of insulin into the blood. Thus, Type I diabetes inhibits this first step in the insulin pathway. And since it decreases the production of insulin, it's referred to as an insulin deficiency. In DM2, drug-induced, and GDM, the pancreas continues to secrete insulin. However, it's the cells throughout the body that are unable to adequately respond to it (decrease in beta cell function), so these mechanisms inhibit the second step in the insulin pathway = insulin resistance, which can be thought of as a relative insulin deficiency. o Diagnostic criteria is based on: ketonuria, age of onset, & BMI ▪ Antibody testing and c-peptide levels determine type: Ab to islet & beta cells are present in 70-80% for Type 1 (not for Type 2), extremely low levels of c-peptide are only seen in Type 1; Type 2 usually occurs ≥ 40 y.o. & BMI > 27 with no or minimal ketonuria ▪ DX is with either 2 FBG ≥ 126 mg/dL or a random BG ≥ 200mg/dL with sx present ▪ Patients who are symptomatic & have 1 + test are dx with DM2; if asymptomatic, 2 + tests are necessary for dx (Khan videos) ▪ HbA1c ≥ 6.5 = DM2 ▪ When hyperglycemia is evident, fasting urine should be checked for ketones to determine Type 1 or 2 and the need for insulin therapy ▪ Screening recommended for anyone who is overweight and has additional risk factors. ▪ Screening should begin at 45 years old and repeated Q3 years (or frequently if multiple risk factors are present) ▪ Additional labs at dx, then annually: fasting lipid profile, eGFR, creatinine, UA, & liver function o Initial treatment recommendations for Type 2: the goal of tx is glycemic control, good nutritional status through weight management and exercise (insulin is usually considered 2nd line therapy when combo therapy fails) ▪ Lifestyle modifications are 1st line therapy for new dx with mild-moderate hyperglycemia (weight loss and exercise)- if after 3-6 months non-pharm tx fails or FBG is 200-300 (or random BG is 250- 350) then add an oral agent like Metformin; dual agent pharmacotherapy not recommended unless A1c ≥ 9% ▪ Metformin (Glucophage) is a biguanide that acts by decreasing hepatic glucose production, decreasing glucose intestinal absorption, & increasing insulin sensitivity. May be used with insulin 1st line oral agent: initial dosing is 500mg daily with breakfast or dinner x 1 week, then BID with meals (long-term tx may decrease B12 absorption, so check annually especially w/ complaints of peripheral neuropathy) ▪ Sulfonylureas (glipizide, glimepiride, glyburide[Beers PIM]) are insulin secretagogues and act by increasing pancreatic insulin secretion and lower HbA1c by 1.25% ▪ Meglitinides (nateglinide-Starlix & repaglinide-Prandin) are insulin secretagogues that increase endogenous release of insulin from the pancreas, and reduce A1c by about 1% ▪ Thiazolidinedines (TZDs) May be used with insulin (piaglitazone (Actos) & rosiglitazone (Avandia) are insulin sensitizers that increase insulin sensitivity to increase glucose utilization and decrease hepatic glucose production, and reduce A1c by 1-1.5% *don’t use in pts with HF, bladder cancer, osteoporosis, or liver disease [Show More]
Last updated: 3 years ago
Preview 1 out of 6 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$13.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Oct 21, 2021
Number of pages
6
Written in
All
Additional information
This document has been written for:
Uploaded
Oct 21, 2021
Downloads
0
Views
168