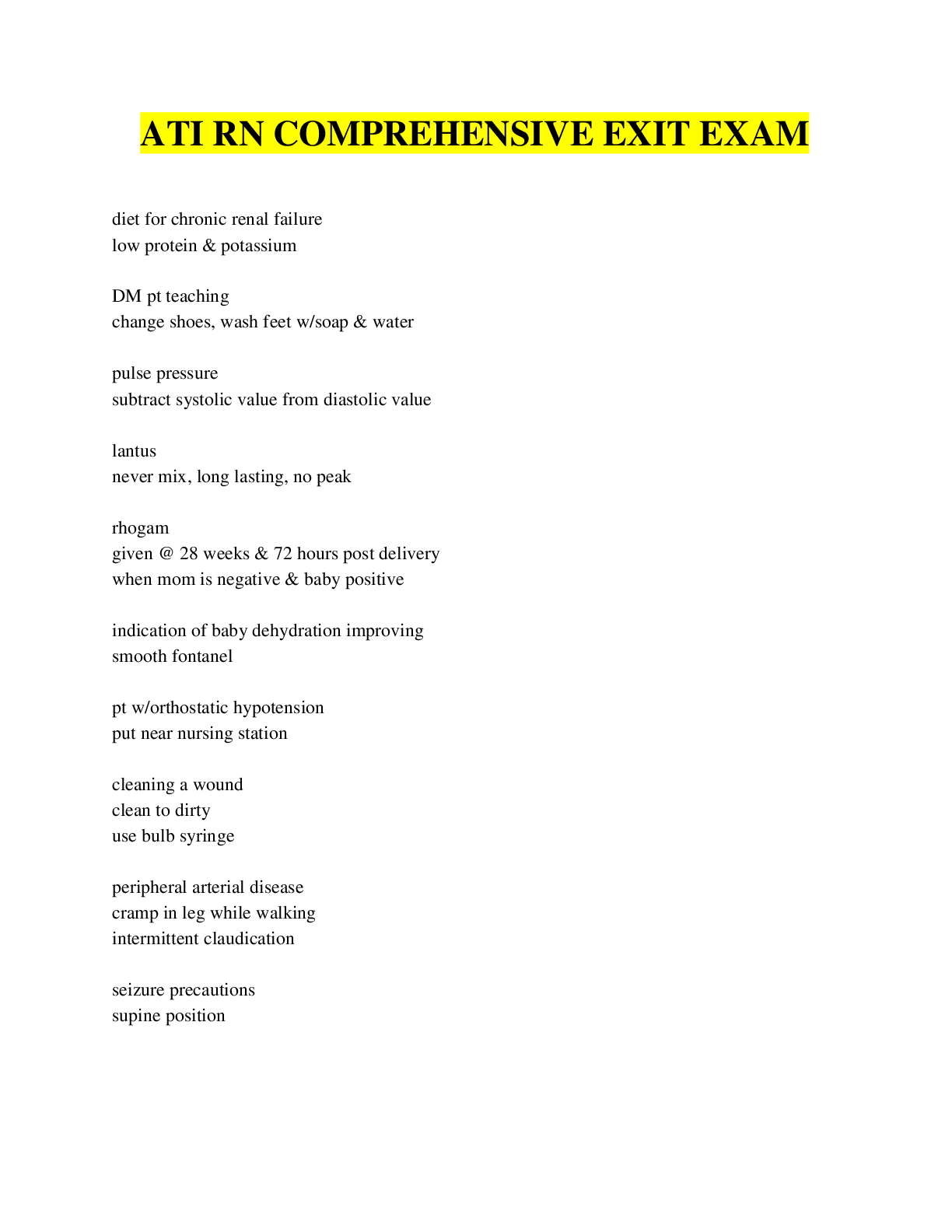
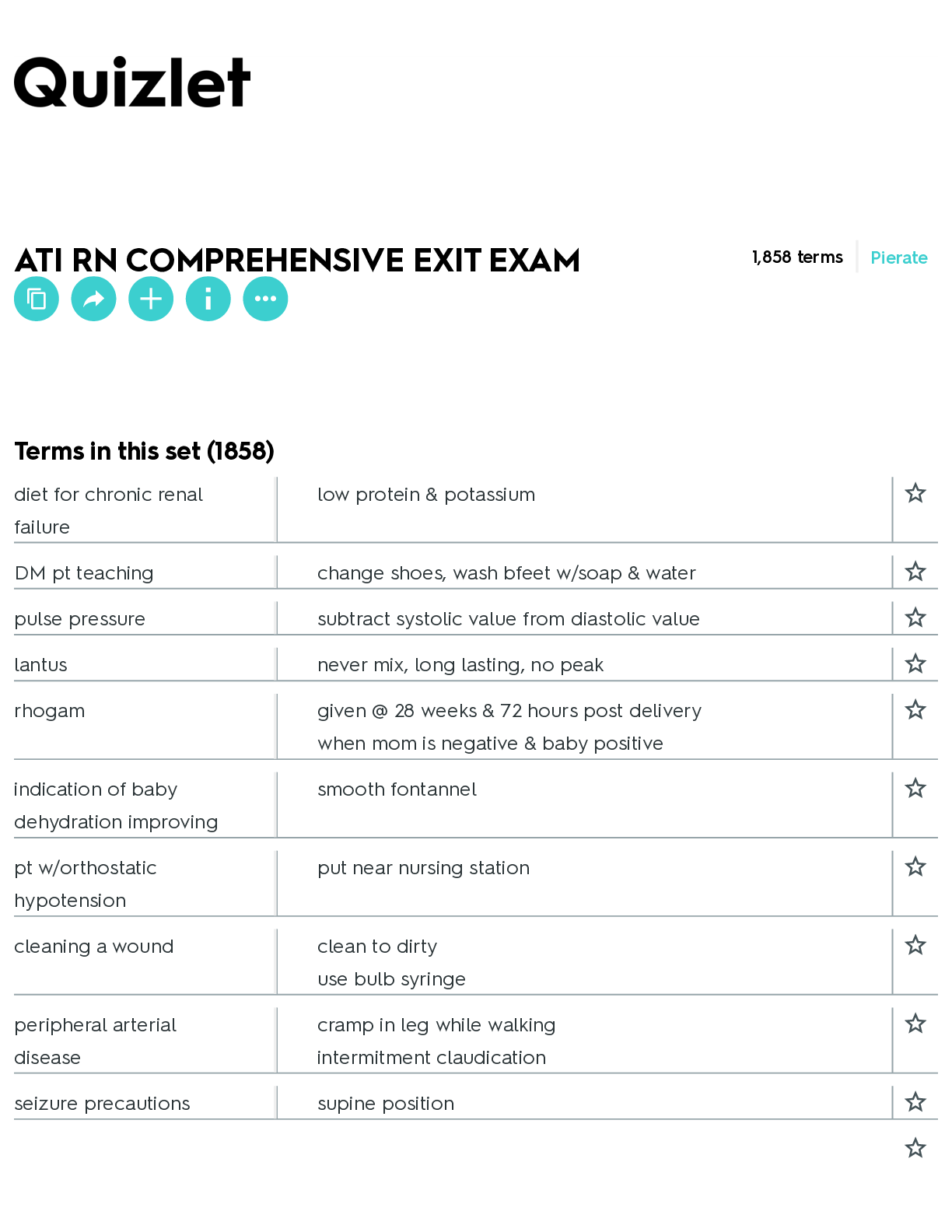
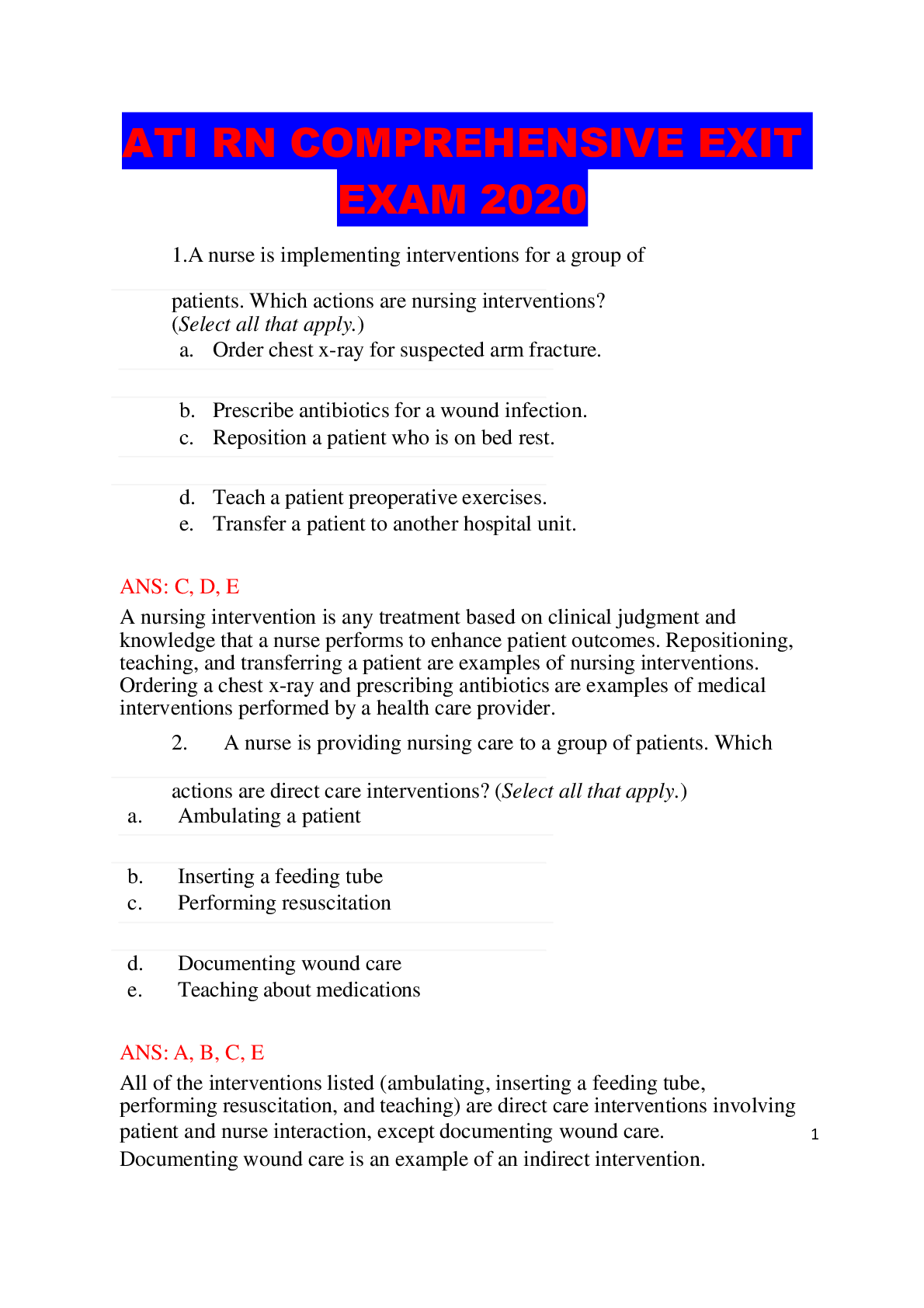
*NURSING > QUESTIONS and ANSWERS > NR 452 ATI RN COMPREHENSIVE EXIT EXAM _2022 | NR452 ATI RN COMPREHENSIVE EXIT EXAM _2022/2023 (All)
NR 452 ATI RN COMPREHENSIVE EXIT EXAM _2022 | NR452 ATI RN COMPREHENSIVE EXIT EXAM _2022/2023
Document Content and Description Below
diet forchronic renal failure low protein &potassium DM ptteaching changeshoes,washbfeetw/soap&water pulse pressure subtract systolic value from diastolic value lantus never mix, long lasting, no... peak rhogam given@28weeks&72hourspostdelivery when mom is negative & baby positive indication ofbaby dehydration improving smooth fontannel pt w/orthostatic hypotension putnearnursing station cleaningawound clean todirty use bulb syringe peripheral arterial disease crampinlegwhilewalking intermitment claudication seizure precautions supine position NR 452 ATI RN COMPREHENSIVE EXIT EXAM Flashcards – Chamberlain College of Nursing ATI RN COMPREHENSIVEEXITEXAM Terms in this set (1858)reporttonewnurse@ shift change pt@xray s/sofhemolytic blood transfusion flank pain ER rape victim priority acessanxiety nutrition carbs 45%,protein10-15% latexallergy tape up cords first ingredient on a food label most content thoracentesis,&painful w/breathing put pt on UNAFFECTED side for1 hourorlonger pt w/IVsedation check LOC if not responsive help olderbrotherget used to baby get a gift forbig brother early decelerations head compressions methergine contraindication HTN delegate toAP I &O HF monitoring weights locationforperipheral line radial prioritizingcarefor multiple pt's lowflankpain ativan for seizures 20 weeks gestation, having urinary frequency u/a&c/sMAOI'sdiet nopepperoni,notyramine,COTTAGECHEESEOKJ stomacolor pinkorredisnormal total gastrectomy lack b 12 takes30-60mealtoeatameal amniocentesis go pee before procedure mitral valvelocation 5thintercostal newborn withdrawal from heroin (opioids) hypertonicity psychotic disorder assessment finding flataffect non-pharm relation technique for pain management inlabor hypnosis antigout meddecreases uric acid level allopurinol uricacidstones eatlowfatyogurt radiation tatoo usemildsoap&water medfordiabetes insipidus desmopressinclozarilinterventions monitor WBC mag sulfate decreased urine output decreased respirations decreased pulmonary edema antidote for mag sulfate calcium gluconate haldol lipsmacking statins contraindication Grapefruitjuice give iron w/? OJdiuretics don't skipdoses DIG adverse effects N/V & HA prednisone takewithmilk hemo/peritoneal dialysis pt teaching medical asepsis cranialnerve 11 shoulder peripheral catheter insertion advancecatheterwhenyouseeflashbackofbloodreturn dispose ofinsulin needles@home incoffeecontainer confirmation of ng placement xray swallowing difficulty referral speech therapy acrabose skipameal,skipdose,givew/1stbiteoffood sprains &strains RICE v thaylp roro idicmae cdid l wiveeig r h futnlo ct sis on effectivenesspt DNR-CC & family asking questionsrelated to. therapeutic communication: THERAPEUTIC RESPONSE delegating to AP about skeletal traction: NEEDS MORE TEACHING Whatdidthedrtellyou? APplacesweightonbedgoodnursesetsthese when sheworks GOALS daughter feeling guilty aboutadmitting parent into long-term facility: THERAPEUTIC RESPONSE rephrase what daughter is feeling ptgetsbaddx,&asks you not to tell her spouse:YOUR RESPONSE you have a right to privacy baby in contact precautions in aprivate room,whatwouldyou do tosavehospital$? how does a nurse properly manage her time mid-shift? bring formula prn reevaluates goals dementia pt @ ER, w/marks on coccyx & wrist,suspectedabuse. what do youdo? whichpsychptwould you see first? hallucinations delegate toAP CPR howgood nurseplans her day rechecks her priorities half way through her shiftask pt. INTERVIEW HIM psychptyellinginfront of group. very agitated, what do youdo? isolateptptinseclusion documentation whathappenedpriortoseclusionthatcausedfor seclusion parkinson's : pt teaching nutrition-thickenliquids ptreceivingradiation, whatshouldyouwear? lead apron pt sufferingfrom hyperthermia seizure precautions xerostoma humidifier vagina procedure, cervical cancer place catheter Lyme disease reportit lice (pediculodiscapitis) cansurviveonsurfacesforupto48hours RSV keep stethescope in room (droplet) 16 weeks gestation can get AFP test done bacterial meningitis whencankidreturnto droplet precautions school forchicken pox kicks a ball: whenlesionsarecrustedover developmental stage 24months charge nurse scheduling resolution between nurses nurse listens to both sides ptrefuseslastminute for a procedure he already consentedfor okay to stopprocedure s/sofsmallpox rashontongue respitecare givesfamilyabreakaftermale circumcision applypetroleumjellyw/everydiaperchange breastfeedingw/hepc don'tbreastfeedifyouhavecrackednipples contraindication w/oral contraceptives HTN combination contraceptives contraindications pt w/migraines when percussingRUQ, what should we feel dullness dementia pt offer finger foods black males @ great risk for CVA med foralcohol withdrawal disulfiran (antabuse) betternutririon canola oil healthyeating 45 % carbs topreventneurotube defects folate prevntingdelaysof healing protein&o2 pt raped &@ ER assess anxiety ptreportsabuse assesspt, check forinjuries anorexia 60% refeeding-pre-albumin of 10 telemetry is used for check fordysrythmia b warobnygwo/cslteofmt lyipcare u ch na tinegainrmgse&vepry edrfaoyrmaRyOleMad to skin irritationdiet forhf dry spices to flavorfood TURP: closed intrermittment irrigation letitdrain Cranial nerveXI (hot spot)shoulder Proper lifting technique (picture) bending at knees 24monthold walkupsteps Food label greatest weight listed first IV technique advance catheter Refeeding syndrome 60% Lowfatdiet canola oilinstead ofvegetable oil Priorto amniocentesis empty bladder Radiation implant limitvisitorsto 30minutes Levothyroxine takeonempty stomach, in am; increases tsh Metformin contraindication kidney disease, severe infection, shock, hypoxic conditions Mastectomy layofaffectedsidetopromotedrainage,support armon pillow, HOB 30 Circumcision use petroleum jelly with every diaper change Check forNG tube placement in the jejunum X-ray Colostomycare cutthe bag Seizure precautions salinelockIV Ethical medical error veracity donotgivemmr tochildbearingptb4pregnancytest pt w/hx of blood transfusionSafetyforparkinson's cleararea Warfarin vitamin kfortoxicity; INR 2-3;PT11-12.5 Contraindication of MMR blood transfusion Diabeticfootcare (select all) change shoes frequently, wash feet with soap and water Sprains avoid warm compress Expectedfindingof small pox rashin mouth 16weekspregnant alpha protein Psych med lipsmacking WheretostartIVfirst (picture)hand PRBCneedfurther teaching startIVonotherarm Delegate toAP CPR compressions Delegate toLPN sterile dressing Postural drainage givealbuterol,trendelenberg;1hourbeforemealsor2 hours after Dumping syndrome highproteinand fat; avoid milk, sweets, and sugar; small, frequent meals E Maarg lynd ee sic uemlesrualtfia otnes h (seeale dcctoam ll)pcraelscsiiuomnsgluconate, stop infusion, UO less than interventions 30, RR less than 12, decreased reflexes Thoracentesis causes pneumothorax expected finding not friction rub; tracheal deviation AP's talking in cafeteria tellthemtostoptalkingCleftpalaterepair periodic restraints Nephrotic syndrome vitamin K Perniciousanemia schilling's test Peritonealdialysis report cloudy; monitor glucose; warm solution before Gastric surgery eat3meals Gastrectomy small,frequentmeals;vitaminB12,D,iron,andfolate Statin grapefruit Preventing uric acid stones yogurt RSV haveownstethoscopeinroom Changeofshiftreport orthostatic hypotension by nurses station Confused patient raise 1 side rail Hypoglycemia cool and clammy skin Hyperglycemia thirst Glycosylatedblood test HbA1C Priority for patient in seclusion document Buddhistpatient vegetarian Positive TB hard raised bump Heart murmur sound blowing or swishing Dehydration oliguria NST ... D BaAbSyHwditih etreflux i snmca re lla,sfe refqrue itn , v te mgeeatlasb, l te hs ic,kaenndfloorwmufala t dwait irhy;rikc,emcge,re cal, HOB 30Cast with white extremity compartment syndrome Alcoholwithdrawal expected finding n&v, tachycardia, diaphoresis, tremors, seizures Varicella scabs okay Hyperthermia not blanket orice Purpose ofice decrease inflammation Sexual assault assess anxiety THA avoidflexiongreaterthan90 Beta blocker teaching don't stop abruptly; avoid in asthma; take with food Combination contraceptives increase BP Myelosuppression flushot Glucocorticoid increase dose in DM; take with meals; avoid NSAIDs; Addison's crisis if stopped abruptly Extreme focus mildanxiety Good diet 30%carbs Family concern whathasthe doctortoldyou Adolescent 1300 mg of calcium Lyme disease report to healthdepartment Organizeworkload goals forthe day Intervene pacingaroundwife Renal failure decrease protein, K, Na, increase carbs, strict I&O PAD pain/cramping when walking, calf muscle atrophy, shiny cool extremities;elevate legsLice canlivefor48hoursonsurfaces Chest tube complications bubblinginwaterseal Elderly abuse ask privately Informed consent signed willingly Sibling bonding offergifteachtimesiblinggetsone TURP complication hematuria African american over Caucasian heart disease Sickle cell priority hydration Sickle cell complication SOB Respite care give caretakerbreak Acarbuse takewithfirstbiteofeachmeal Hallucination Iunderstandyouarescared Fire extinguisher PASS Advanced directive don'tneedalawyer Breastfeeding and hepatitis c aslongasyoudon'thavecrackednipples ICP keepHOBmidline Long term use of proton pumpinhibitors osteoporosis Diabetesinsipidus polyuria Difficulty voiding warm water P Urreineeclfare mqpuseiancy in p urionteeisneunrs iaitivity test pregnancyNegotiation strategy understand bothsides Dying patient wants to be alone depression or dysfunctional Wife progressing quickly can youtellme more What causes constipation iron Patient can'tsleep don'tdrinkcaffeinebeforebed Collecting urine culture on baby Electrolytes straight cath Na- 136-145 K -3.5-5 Ca- 9-10.5 Mg-1.3-2.1 P -3-4.5 Hypervolemia Anorexia Cl bounding, prealbumin - 98-106 JVD, 10 edema, confusion, increase everything A WChEatindhoibyit oourshear when c reosuognhance you palpate abdomen Pregnant nonpharmacological pain management aromatherapy,breathingtechniques,imagery,music,useof focal points, subdued lighting Complication of conscious sedationwith RR 6 stop infusion or give something Majordepression,OCD give fluoxetine Hypnosis purpose alterperception ofpainUnsaturated fat coconut oil Priority abdominal pain and went away Opioidagonist naloxone (Narcan) COPD increase calories and protein Needle disposalat home coffee containeron top shelf Give RhoGAMin second pregnancy protectfuturepregnancy Swallowproblem refer to speechtherapist Nutrition forheart failure Decrease Na, increase fluids, increase fiber; increase K with diuretic Adverse affects of dogoxin Bleeding gums, bloody urine and stools, arrhythmias, petichiae NG nutrition Increase K Methotrexate adverse affect High blood pressure I.M. site for children VASTUSLATERALISorantelolateralthighisthesiteforIM injections in children < 2 yrs. of age Peak Levels show the highest concentration Time for drawing Peak levels: OralIntake 1 to 2 hour after administration Time for drawing Peak levels: I.M. 1 hour afteradministration Time for drawing Peak levels: I.V. 30 minutes after administration Dehydration improving baby flatfontanelleTreatmentof Infiltration stop, remove, cold compress, elevate extremity, insert new cath in oppositeextremity Preventing Extravasation know vesicant potential before giving medication Treatment of Extravasation stop, discontinue, aspirate med if possible, cold compress, document Preventing Phlebitis& Thrombophlebitis rotate sites every 72 to 96 hrs, secure catheter, aseptic techniqueforPICClines,limitactivitywithextremity Treatment of Phlebitis & Thrombophlebitis stop, remove, heat compress, insert new cath in opposite extremity Preventing Hematoma avoid veins not easily seen or palpated, obtain hemostasis after insertion Treatment of Hematoma remove, apply pressure, monitor for signs of phlebitis and treat Preventing Venous Spasm allow time for vein diameter to return after tourniquet removed, infuse fluids at room temp Trough Levels Can meds be administeredthrough blood tubing? show the lowest concentration or residual level, usually obtained within15minutesbeforenextdose.Donot administer until confirmed. NO.Neveradministermedsthroughtubingbeingusedfor blood administration Complications associated withIV infusion infiltration, extravasation, phlebitis, thrombophlebitis, hematoma, venous spasm PreventingInfiltration use smallest catheter for prescribed therapy, stabilize portaccess, assess bloodreturn Howlong should fluids be infused? Fluids should be infused within 24 hours, discard unused potion, to preventinfectionCare for TPN Complications of central venous catheters Pneumothoraxduring insertion Air Embolism verifywithanothernurse,useinfusionpump,monitordaily weights,I &O,fluidbalance,serumglucoseq4to6hrs, infection,change dressingq48to72hrs,changetubing and fluid q24 hours, if TPN is unavailable, administer dextrose10%inwatertoprevent hypoglycemia pneumothoraxduringinsertion,airembolism,lumen occlusion, bloodstream infection use ultrasound to locate veins, avoid subclavian insertion when possible, treat with O2, assist with chest tube insertion have client lie flat when changing administration set or needlelessconnectors,askclienttoperformValsava maneuver, treat by placing client in left lateral trendelenberg, andO2 BloodstreamInfection maintainsteriletechnique,treatbychangingentireinfusion system, notify MD, obtain cultures, and administer antibiotics Antidote for Acetaminophen Acetylcysteine, Mucomyst Lumen Occlusion flushpromptlywithNSbetween,before,andaftereach med, treat with 10 cc syringe with pulsing motion TPN hypertonic solution, contains dextrose, proteins, electrolytes, minerals, trace elements, and insulin prescribed, administered via central venous device like PICC line, subclavian, or internal jugular vein Treatment of Venous Spasm temporarily slow infusion rate, warm compressAntidote for Benzodiazepine Flumazenil, romaziconAntidote for Digitalis digoxin immune FAB, Digibind Antidote for ethylene poisioning fomepizole, antizol Antidote for Magnesium Sulfate calcium gluconate 10%, kalcinate AntidoteforNarcotics naloxone, narcan AntidoteforWarfarin phytonadione,vitaminK aminophylline 10 to 20 mcg/ml carbamazepine 5 to 12 mcg/ml digoxin 0.8 to 2.0 mcg/ml gentamicin 0.5 to 0.8 mcg/ml lidocaine 1.5to5.0mcg/ml lithium 0.4to1.4mcg/ml magnesium sulfate 4 to 8 mcg/ml phenobarbital 10 to 30 mcg/ml phenytoin 10 to 20 mcg/ml quinidine salicylate theophylline 2 100 toto5 to20 mcg/ml 250 mcg/ml mcg/ml Antidote for Cu ya ranrie de e mdertohpyh leonneiubmlu,e tensilon Poisoning AntidoteforHeparin and enoxaparin or Lovenox Protamine Sulfate AntidoteforIron Deferoxamine, desferalaminophyllinetoxicity >20 amitriptyline toxicity >500 digoxin toxicity > 2.4 gentamicin toxicity > 12 lidocaine toxicity >5 lithium toxicity > 2.0 magnesium sulfate toxicty >9 methotrexatetoxicity >10over24hours phenobarbital toxicity > 40 phenytoin toxicity > 30 quinidinetoxicity > 10 salicylatetoxicity >300 theophylline toxicity >20 tobramycin toxicity > 12 PRIL ace inhibitors, captopril, enalapril VIR antivirals, acyclovir,valacylovir AZOLE anti fungals, fluconazole, variconazole STATIN antilipidemics, atorvastatin, simvastatin SARTAN angiotensin 2 receptorblockers, ARBS, valsartan, losartan OLOL betablockers,metoprolol,nadolol DIPINE calcium channel blockers, amlodipine, nifedipine t aocbertamyincoinphen toxicity 5 > 2to5010 mcg/mlPRAZOLE proton pump inhibitors, pantoprazole CAINE anesthetics PAM, LAM benzodiazepine ASONE, SOLONE corticosteroid CILLIN penecillin IDE oral hypoglycemic ASE thromolytic AZINE antiemetic PHYLLINE bronchodilator ARIN anticoagulant TIDINE anti ulcer ZINE anti histamine CYCLINE antibiotic MYCIN aminoglycoside FLOXACIN antibiotic TYLINE tryciclicantidepressant PRAM,INE SSRI A DFINILE e hirsetcatmileinedy2sfruenccetpiotonrmbelodcsk,esr ids,ernaanfiitili,dtiandea, lfaaafmil otidineanti hypertensives ACE inhibitors (angiotensinconverting enzyme) assess weight, VS, hydration, ortho BP, renal function, coagulation, educate to take same time each day, avoid hottubs andsaunas,donotdiscontinueabruptly block the conversion of angiotensin 1 to angiotensin 2ACE inhibitors and ARBs ACE inhibitors and ARBs side effects ACE inhibitors and ARBs nursing interventions Calcium Channel Blockers for HTN, heart failure, MI, and diabetic nephropathy, monitor potassium,usewithcautionifdiuretictherapyisin use persistent non productive cough with ACE inhibitors, angio edema, hypotension,contrafor2ndand3rdtrimesterin pregnancy captopril should be taken 1 hr before meals, monitor BP, monitor for angio edema and promptly administer epinephrine0.5ml of1:1000solutionsubq slowsmovementofcalciumintosmoothmusclecells, resulting in arterial dilation and decreased BP, examples are nifedipine/adalat/procardia, verapamil/calan, dilitiazem/cardizem,amlodipine/norvasc Calcium Channel Blockers Precautions use cautiously in clients taking digoxin and beta blockers, contrafor clientwhohaveheartfailure,heartblock,or bradycardia,avoid grapefruitjuice (toxic) Calcium Channel Blockers nursing interventions Calcium Channel Blockers side effects constipation, reflextachycardia, peripheral edema, toxicity Calcium Channel Blockers Use forangina,HTN,veripamilanddiltiazemmaybeusedforA Fib, A flutter, or SVT ARBs losartan or cozaar, valsartan or diovan, irbesartan or avapro ACE Inhibitors captoprilorcapoten,enalaprilorvasotec,enalaripator vasotec IV, fosinoprilormonopril, lisinoprilorprinivil Angiotensin 2 Receptor Blockers selectivelyblockthebindingofangiotensin2to angiotensin 1 receptors found in tissuesdo not crush or chew sustai ned release tablets , admin ister IV injecti on over 2 to 3 mins, slowly taper dose if discon tinuin g, monit orHR and BPLorazepam antidote flumazenil Fluid overload dyspneas/s,backupoffluidinpulmsystem Rheumatoid arthritis pain freqrestduringtheday casemgr arranges for transportation to health care appts w/mental health Totalhip install raised toilet seat at home verapamil and grapefruit causes hypotension, g. increases blood levels of v. by inhibiting metabolism vaso occlusive crisis in sickle cell start iv fluids 1st to promote hydration and circulation Alpha Adrenergic Blockers (symphatholytics) Alpha Adrenergic Blockers (symphatholytics) Use selectivelyinhibit alpha, adrenergic receptors, resulting in peripheralarterialandvenousdilationthatlowersBP, esamples are for primary HTN, cardura may be used in treatment of BPH Alpha Adrenergic increased risk of hypotension and syncope if given with Blockers other anti hypertensives, beta blockers, or diuretics, (symphatholytics) NSAIDs may decrease effect of prazosin Precautions Alpha Adrenergic Blockers (symphatholytics) side effects dizziness, fainting Alpha Adrenergic monitor HR and BP, take meds at bed time to minimize Blockers effects of hypotension, advise to notify prescriber (symphatholytics) immediately about adverse reactions, consult prescriber nursing interventions before taking any OTC meds.hyperglycemia polyuria Oneormoresurgical drains after? masectomy, exercise after 24 hrs TBmeds___ orlonger 6 mo blowing bubbles to make the"hurtgoaway" isan exampleofwhat? nonpharm visualization for pain mgmt w/kids Ifclientisdisorientated andcombativeduring the night,whatshould Rn do? hypoglycemia irritability enoxaparin aka lovenox N/Vwillcause what lab value to elevate? urine specificgravity-dehydration narrow QRS complex, irregular170bpm,nop waves a fib hemianopsia hemi=half, an=without, opsia=seeing *use scanningtequnique whenambulating Donotincreasethisif pt has COPD exaserbation O2Changing this is final step in trach care trach ties Diazepam (benzo) should be givenfor? statusepileptcus move client closer to Rn station Wash clients hand with soap/water prior to? CBGClonidinesideaffect dry mouth Clozapine side affect wt gain Unstable vs are immediate threat to life? t/f true! TPN pt's need this monitored frequently bloodglucose,24hrTPNatfirstthen8-12hrsperday once stable ECTcancause short term memory loss Nurseshould use__with transfusion 0.9% sodium chloride to preventclotting, **not D5W Expected finding in cardiac tamponade pulsus paradoxus-drop in bp during inspiration Nonmaleficence duty todo noharm autonomy informed consent pattern paced breathingduringthis phase of labor transition HUsAeisve an dtvre orgsleutefafe lc sittte of? f olu bo ex setine, hypotension too with these patients for IMTremors canindicate hyperthyroidism Cloudiness with blurred vision cataracts positionclientwhoisat risk for pressure ulcer at this level 30 degree lateral position in bed Pt with femur fracture highest prioroty upper chest petechiae-risk for fat embolism syndrometo decreseicp putinquietenv quick notesduring h-t assessment Pt admitted with dka, first priority? vs If INR is 1.8and pttis 98 hold heparininfusion 6-8wetdiapersaday indicates? Brat diets are effective breastfeeding contraindicated with Askthisifptrefusesto diarrhea ambulateaftersurgery pain Haveptlieonthisside during gastric levage for NGtube left-prevents aspiration Diaphram should be removedhowlongafter intercourse? 6 hrs ormore intervention toprevent heat loss with infant padscalewithpaper Celiac diet glutenfree-chickenandwildrice Occupational therapy for difficulty performing personal hygeine __precautions with hsv contact ___lung expansion with age decreased thismedwillhelp reduce icp mannitol-osmoticLPNcaninsert NG pt with this needs private room with negative air pressure pulmtb ifptisunconsiousand needs erhelp proceed without consent opioid side effect u. retention Use 1:100 chlorine solution to clean kitchensurfaces with this illness hep A make referral forsocial services for pt with this terminal illness serummagnesiumof2.5 initiate continuous cardiac monitoring Coldtherapyforthese patients Rheumatoid arthritisto relieveinflammed joints fluoxetine SSRI antidepressant-watch for tremors since this can cause serotonin syndrome w/in2-72 stage II pressure ulcer partialthicknessskinloss stage III pressure ulcer visible sq tissue stage IV muscle damage, tendon exposure Cyclophosphamide treatscancer,drink 1-1.5xh2o topreventhemmoragic cystitis and prevent dehydration Valporic acid treats seizures-can cause hepatic toxicity digoxin toxicitysign nausea Review chest x-ray report priorto initiating infusion in piccChlorpromazine antipsychotic to decrease hallucinations Theophylline toxicity bronchodilator-can cause anorexia Checkthispulsewithan infant duringcpr brachial Advance Directives 2componentsofanadvancedirectivearethelivingwill, and a durable power of attorney. Legal documents that allow people to choose what kind of medical care they wish to have if they cannot make decisions themselves. Nsg responsibil ities areproviding info regaurding advance Nsg responsibilities are-providing info regaurding advance dir,documentingstatusofadvancedir,ensuringtheyare current, and reflect pt. status. Recognizing they take prioritiy forthe pt.Ensuring that all healthcare team members are aware. Report findings for pt rigid, board likeabdomen post rupturedappendix absent bowel sounds 48 hr ago elevated temp elevated wbc (could be indication of peritonitis) Clientisinactivelabor and receiving oxytocin. FHR shows variability w/accelerations. Whatis correct response? Document and continue to monitor.Thisisareassuring pattern indicating intact fetal CNS and healthy placental/fetal exchange of oxygen. Indication of oxygen toxicity Bradypnea-hypoxic drive isremoved estradiol (estrace) side effect HAAssigning theprocessoftransferring authority, accountability, responsibility of pt, care to another health care member. durable power of attorney enablespatient(calledthe"principal"inthepowerof attorney document)toappointan"agent,"suchasa trusted relative or friend, to handle healthcare decisions on behalf ofpatient. delegating supervising casemanagement The process oftransferring authorityand responsibility to another team member to complete atask while retaining accountability. Process of directing monitoring and evaluating performance of tasks by another member of the health care team. a methodology for moving a patient through the healthcaresystem whilestreamliningcostsandmaintaining quality,Exploreresources availabletoassistwiththept.in achieving ormaintaining independence. airway1st Identify airway concern( obstruction,stridor) Establish a patent airway recognize that 3-5 mins without o2 is irreversible brain damage 2ndary to cerebral anoxia. advocacy supporting pts. by ensuring that they are properly informed, that their rights are respected, and that they are receiving the proper level of care. Nurses must act as advocatesevenwhentheydisagreewith pts.wishes. Nursesare thepts.voicewhenhealthcare systemisnot acting in pt. best interest. living will legal document that expresses client's wishes regarding medical treatment in the event the client becomes incapacitatedandisfacingend-of-lifeissues.Ex.cpr, mechanical ventilation, and feeding by artificial means.Breathing 2nd circulation 3rd disability 4th Pt. Rights Nurses role Prioritizesystemic before local. (life before limb) Prioritizeacutebefore chronic prioritize actual problems beforefuture potential problems. Accesseffectivenessofpt.breathing(apnea,depressed, respiratory rate, Intervene as appropriate(reposition, administer narcan). Identify circulation concern (hypotension ,dysrhythmia, inadequate cardiac output, compartment syndrome) identify waysto minimize orreversecirculatoryalteration). Access for current evolving disability (neurological deficits stroke evolution) Implement actions to slow down disability. Beinformedaboutallaspectsofcareandtakeanactive role in decision making process. Acceptrefuseorrequestamodificationtoaplanofcare. Receive carethatisdeliveredbyacompetentindividual. prioritizeinterventions forapt.inshockoverinterventions fora pt. with a localized limb injury. Care ofpts. with new injuries/illness( confusion, chest pain) overacute exacerbationofapreviousillness,overthecare over a pt. with a longterm chronic illness. prioritize administration of medication to a pt. experiencing acute pain overapt. ambulating and at risk forthrombophlebitis. Hypoglycemia risk POST TERM, IUGR, ASPHYXIA, COLD STRESS, factors forNewborns, Maternal diabetes, Gestational hypertension, Tocolytic Blood glucose <40 in therapy, Prematurity, LGA, SGA, Perinatal hypoxia, term newborn, <25 in Infection, Hypothermia preterm newborndysphagia ... Latex allergies must use latex free equipment, gloves and supplies. Prioritizing care in clients with hyperthyroidism Alternate periods of activity with rest provide calmenvironment access mental status increased calories and protein monitor intake and output, wt pt. eye protection for pt. with exophthalmos report a degree of 1 ormore to MD prepare for thyroidectomy if meds become unresponsive. Pt. education r/t report fever, sore throat, or bruising to md hyperthyroidism report any jaundice or dark urine medications, follow md instructions about daily intake of iodine. methimazole (tapazole) and (PTU) propylthiouracil. These inhibit the production of thyroid hormone. RiskFactorsofDiabetes Dilantin (phenytoin) being African American, Hispanic, or Asian obesityandfatdistribution,inactivity,familyhistory,race, age,prediabetes,Overweight,familyhx,ethnicity,HTN, gestational diabetes,age,viruses,lifestyle,diseaseof pancreas. Anticonvulsant Seizures, therapeutic levels are determined by blood test. Meds should be taken at the same everyday. Some antieplitic cause overgrowth of the gums, routine oral hygiene. NO ORAL CONTRACEPTIVES OR COUMADIN.X1 (spinal accessory) Cranial nerve11 Motor turning the head, shrugging shoulders. Head and neck. Seclusion/restraints In emergency situation where there is immediate danger to the pt. or others, the nurse may place the pt. in restraints, nurse must maintain prescription as soon as possible usually within 1 hour. Nsgassess skin integrity, offerfoodandfluid,providehygieneandelimination,vss, romq2hr.quickreleaseknots to bed frame. Postpartum Assess fundus for height firmness and position. If boggy hemorrhage/ massage fundus to increase muscle contraction. postpartum disorders Assess lochia for color, quantity, and clots. appropriate assessment. Assess for signs of bleeding from lacerations, episiotomy site, orhematomas. Assess for bladder distention, may need to insert urinary catheter to assess kidney function. Pitocin, methergine, IV fluids. cultural/spiritual nursing care, use of a interpreter Dietary guidelines for celiac disease Facility approved interpreter, don't designate the family, or anon designated employee. Inform the interpreterthe type of questions that will be answered. Allowtimeforfamilyandinterpretertobeintroduced. Direct the questions toward family/pt. not interpreter. Followingthe interview ask the interpreterifthey have any thoughts about pt. verbalornon verbal. children-s/s diarrhea, steatorrhea, anemia abdominal distention, impairedgrowth,lackofappetiteandfatigue. Adults- diarrhea, abdominal pain, bloating, anemia, steatorrhea, and osteomalacia. Dietary Foods that are gluten free-milk, cheese, rice, corn, eggs, potatoes, fruit, veg, fresh poultry, meats, fish, dried beans. Gravy mixes sauces,cold cuts, and soups, have gluten.Parkinson client safety Nephrotic Syndrome dietary modifications prevention ofuricacid stones Pt. teaching about self blood glucose monitoring Encourageexercise(yoga),assistivedevices,rom,teachpt. to stop when walking to slow down and reduce speed. paceactivitiesby providingrestperiods.assistwithadls. D/Tproteinloss,youwillneedadequateamountofprotein and low sodium. Protein-0.7to1.0g/kg/day.Soybasedproteins,Lowsodium 1000- 2000g per day. Carbohydrates, trans fat and cholesterolislimited, and total fatshould be less than 30% perday,providemultivitamin supplements. Increase fluid consumption 1500-3000 ml at least preferably h20, atnightbecause that's when urineis most concentrated. Foodshighin oxlate such asspinach,rhubarb, beets, nuts, chocolate, tea, wheat bran, and strawberries., Avoidmega dosesofvitaminc, andlimitfoodshighinpurinelean meats,organmeats,whole grainsandlegumes. Check the accuracy of the strips with the solution usethecorrectcodenumberinthemetertomatchstrip. store strips in closed container adequate amountofblood proper handhygiene fresh lancets avoidsharing keeprecordofbloodsugarsthecaloriesandexercise taken in. foodandothereventsmayalterbloodglucose metabolismsuchasactivityorillness. Pt. care following a mastectomy ...Assessment findings for increased intracranial pressure. Deep Vein thrombosis Interventions Delegationthe5rights providingcosteffective care Severe HA,deteriorating loc, restlessness, irritiability, dilated pinpoint pupils, asymmetric pupils, slow to react or nonreactive, alterationwithbreathingpatterns,cheyne stokesrespirations, hyperventilation,apnea,deteriationin motor function, abnormal posturing, decerebrate, decorticate, or flaccidity, cushing reflex, htn, widening pulsepressure,andbradycardia,csfleakage,halo sign, seizures,. Encourage pt. torest Facilitatebedrestandelevationofextremity donot massage extremity thighhighcompressionstockings monitor APTT, and platelet count. right task right circumstance right person right communication right evaluation/supervison usingalllevelsofpersonneltofullestwhenmaking assignments. providing necessary equipment and charging the pt. Returning uncontaminated orunused equipment to appropriate dept. forcredit. Using equipment properly to prevent wastage providing training to staff unfamiliar with equipment, Returningequipmentto properdept.assoonasitsno longer needed. Heart failure nutrition recommendations Reduce sodiumintake to2000 mg/dayorless monitorfluid intake restrict to 1.5 liters fluid a day.Magnesium signsof toxicity ... Psychotic disorders assessment findings Adolescent nutritional needs Newborn withdrawl from opioids medications Alcohol withdrawl Contraindications to oral contraceptives Hallucinations,deluisons,alterationsinspeech,bizarre behavior arepositivesignsofschizophrenia. Negative signs-affect orflat facial expression, alogia- povertyof thoughtofspeech,Anergia-lackofenergy, anhedonia-lackof pleasureorjoy,avolition-lackof motivation inactivities and hygiene 00 2000 cal for female and 4000 cal for male. They need aadequate dietin folate, vita&e, iron, zinc, mag, cal and fiber. opiate withdrawl, can last 2 to 3 weeks rapid mood changes, hypersensitivity to noise and external stimuli, dehydration,and poorweight gain. nabdominal cramping, vomiting, tremors, restlessness, inabilityto sleep,increased heartrate,hallucinations, illusions, anxiety, increased blood pressure,respiratory rate, temp, and tonic clonic seizures. Mayoccur2-3daysaftercessationofalcohol,andmay last for2-3 days, *THIS IS A MEDICAL EMERGENCY. severe disorientation, severehtn,psychoticsymptoms,cardiac dysthymias,delirium.Medsvalium,Ativan,carbamazepine (tegretrol) seizures, clonidine (catapres) Librium (chlordiazepoxide) Hx of blood clots, stroke, cardiac problems, breast or estrogen related cancers, pregnancy or smoking if over 35, are advised notto take oralcontraceptives. Oralcontraceptivesdecreasesitseffectivenesswhen taking meds thateffectliverenzymes,suchasATB's,and anticonvulsants. Antibiotics affecting bacterial cellwall Penicillin,cillians.amoxicillinetc.Access to medical records Discharge teaching regarding circumsion Strokepriorityassess findings Clientshave arighttoreadtheironrecords. Nurses maynotphotocopyanypartofmar. Communication should only take place in a private setting. Shredany printedwrittenpt.infoafterpt.careoruse. A tub bath should not be given unti healed Notifymdofredness,discharge,swelling,strongodor, tenderness, decreasein urination, orexcessivecrying, will heal completely in 2 weeks. Give Tylenol for first 24 to 48 hours. Assess forbleeding every15 min forthe first hour, then everyhour foratleast12hour,thenthe1stvoiding. Expressiveandreceptiveaphasia,agnosia,(unableto recognize objects), alexia(difficultyto reading), agraphic (writing difficulty), hemiplegia,(paralysis), or hemiparesis (weakness), slow behavior, depression, anger, visual changes(hemianopsia). Stimulant withdrawl (cocaine) Withdrawl stimulant (tobacco) COPDmanaging nutrition Occurs within1 hour to several days, depression,fatigue,craving,excess sleeping, insomnia, dramatic unpleasantdreams,psychomotorretardation, possible suicide ideation. Abstinenceirritabilitycraving nervousnessrestlessness anxiety insomnia increased appetite difficulty concentrating anger depressed mood, Highcaloriefoodsforenergy Encourage restperiods. Drinkplentyoffluidstoliquidfymucous,andpromote hydration. Findings of recent cocaine use Rush of euphoria, pleasure, increased energy.Phlebitis Edema, throbbing, or burning at site. Increased skin temp, erythemaredlineupthearm,withapalpablebandatthe vein,slowedrateinfusion.Treatment-discontinueIVand remove catheter, elevate extremity, warm compresses 3x daily, restart proximal to site, culture the site and catheterif drainage is present. Use surgical aseptic technique. Rotate sites q 72hours. IV Therapy documenting complications. Require notification of MD, and documentation, all IV infusionsshouldberestartedwithnewtubingand catheters. Ecchymosis Fluidoverload Don't apply alcohol apply pressure after IV catheter removal. Use warm compress and elevate after bleeding hassubsided. Prevention-minimizetourniquettime, removetourniquetbefore starting IVinfusion, maintain pressure after removalof catheter. Distended neck veins, increased BP, tachycardia, sob, cracklesin lungs,edema.Treatment-stopinfusion,raise hob, assess vs & O2 saturation, adjust the rate as prescribed,andadminister diureticsasprescribed. Prevention- monitor I&O. Respiration assessing them Observingtherate,depthandrhythmofchestwall movements. Inflitration Infiltration-pallorandlocalswellingatsite,slowedrateof infusion,treatment-stopandremovecatheter,elevate extremity,encourage active ROM, applywarm orcold compress.Restartproximaltositeoranotherextremity.Cane Keep cane on stronger side of body Support body weight on bothlegs, movecane forward6- 10 inches, then move weaker leg forward, next advance the stronger leg past the cane. Postarthroplasty Use elevated seat, orraised toilet seat. Use straightchairswitharms Useabductionpillow,orpillowifprescribed,b/wthept. legswhile inbed,andwithturning,ifrestlessorina altered mentalstate. Externally rotate pt.toes. Donotdo,crosslegs,avoidlowchairs,avoidflexionof hipsat90 degrees,donotinternallyrotatethetoes. Crutch walking Insertion of a urinary catheter Ototoxic medications Nursing care of a pt. who is pregnant and has gonorrhea Do not alter after crutches after fitting Supportbodyweightatthehandgrips,withelbowsflexed at30 degrees,positionthecrutchesontheunaffected side when sitting orrising froma chair. Usually 8-10 French for kids, 12-14 for women, and 16-18 for men.Use siliconorTeflonifpt.haslatexallergies.Explain procedure,aclosed intermittentirrigation.ifpt.reports fullness in bladder area, check for kinks in tubing or sediment,mayneedirrigated,make surebagisbelow bladder. Multiple antibiotics, gentamicin, amikacin, metronidazole(flagyl), lasix, NSAIDs, chemotherapeutic agents. Urethraldischarge, yellowish green vaginal discharge, reddened vulvaand vaginal walls. Ceftriaxone (rocephin) and azithromycin (Zithromax) pro for gonorrhea, take entire prescription, repeat culture, and educate on safe sexpractices. Preventing foot drop ...Esophageal prescription for a pt. with esophageal varices Interventions for prolapse cord Interventions for dementia Dumping syndromeS/S No selective beta blockers, propranolol (inderal), are prescribed to decrease heart rate, and reduce hepatic pressure. VasoconstrictorsIVterlipressin andsomatostatin increase portal inflow. And vasopressin (desmopressin) and ortreotide(sandostatin) areavoidedd/tmultipleadverse reactions. CallforassistanceASAP,notifyMD,useasterilegloved hand, insert 2 fingers in vagina, and apply finger pressure ononeithersideofthe cord,tofetalpresentingpartto elevate it off cord, reposition knee chest position, or trendelenburg,orsidelyingwitharolledtowel underthe pt.rightorlefthip,torelievepressureoncord.Applya warmsalinesoakedsteriletoweltocordtopreventfrom drying. Provide cont electronic monitoring of FHR for variable decels. O2 at 8-10 liters, IVaccess, prepare for c- section,educateand informpt.oninterventions. Provide clocks and memory aids, photographs, memorabilia, seasonaldecorations,familiarobjects,orient if necessary. Daily routine, allow for safe pacing and wandering.Assignroomclosets tonursesstation,welllit environment.Restraintsasalastresort, COverorremove mirrors to reduce anxiety and frustration. Encourage pt. to talk aboutgood times, breakinstructions and activitiesinto short timeframes. Fullness, faintness, diaphoresis, tachycardia, palpitations, hypotension, nausea, abdominal distinction, cramping, diarrhea, weakness, and syncope.Do not delegate What you can EAT E-evaluate A-assess T-teach APGAR Appearance (all pink, pink and blue, blue (pale) Pulse (>100, <100, absent) Grimace (cough, grimace, no response) Activity (flexed, flaccid, limp) Respirations (strong cry, weakcry, absent) Psychotic disorders long term adverse reactions Newonsetofdiabetes,orlossofglucosecontrolinpets. With diabetes,weightgain,increasedcholesterolwith HTN,orthostatic hypotension, anticholinergic effects such asurinaryhesitancyor retention,anddrymouth.agitation, dizziness, sedation, and sleep disruption, mild eps such as tremor. Treating xerostomia following radiation Post procedure following a throcentesis Avoid spicy, salty, acidic foods, hot foods may not be tolerated. Gentlywashoverirradiatedskinwithmildsoap andwater,patdry. Dipsofh20,andcandiestopreventdry mouth. Apply dressing and assess for bleeding, or drainage, monitorvs, and resp hourly. Auscultation lungs for reduced breathsounds, encouragedeepbreathingtoassistwith lung expansion. CHESTXRAYpost procedure. Addison's &Cushings Addison's=downdowndownupdown Cushings= upupupdown up hypo/hypernatremia,hypo/hypertension,bloodvolume, hypo/hyperkalemia, hypo/hyperglycemia Better peripheral perfusion? EleVateVeins,DAngleArteries Interventions foricp Hob 30 degrees, avoid extreme flexion, midline neutral position, keep body aligned. Decrease stimuli. Seizure precautions Suction equipment at bedside, Valium or Ativan.Droplet precautions Contactprecaution spiderman!sepsis,scarletfever,streptococcalpharyngitis, parvovirus, pneumonia,pertussis, influenza, diptheria, epiglottitis, rubella, mumps, meningitis, mycoplasma or meningeal pneumonia, adeNovirus (Private room andmask) MRS WHISE protectvisitors&caregiverswhen3ftofthept. Multidrug-resistant organisms RSV,Shigella,Woundinfections,Herpessimplex,Impetigo, Scabies, Entericdiseasescausedbymicro-organisms(C diff), Glovesandgownswornbythecaregiversandvisitors Disposalof infectiousdressingmaterialintoasingle, nonporousbagwithout touchingtheoutsideofthebag PMGG= Private room/sharesame illness, mask, gown and gloves Airborne precautions protective equip private room, neg pressure with 6-12 airexchanges/hr mask & respirator N95 for TB Airborne precautions MTVorMychickenheztbmeasles,chickenpox(varicella) Herpes zoster/shingles TBduring Continuous BladderIrrigation(CBI) catheter is taped to the thigh. leg must be kept straight. After Myringotomy positiononthesideofAFFECTEDear,allowsdrainage. After Cateract surgery ptsleeponUNAFFECTEDsidewithanightshieldfor1-4 weeks afterThyroidectomy low or semi-fowler's position, support head, neck and shoulders. InfantwithSpinaBifida Pronesothatsacdoesnotrupture Buck's Traction (skin) elevate foot of bed forcounter traction AirorPulmonary Embolism Woman in labor (unreassuringFHR) S/Schestpain,dyspnea,tachycardia,pale/cyanotic,sense of impendingdoom.(turnpttoLEFTsideandLOWERthe head of bed.) (late decels, decreased variability, fetalbradycardia, etc) Turnpton Leftside,giveO2,stoppitocin,IncreaseIV fluids! After lumbarpuncture and oil based myelogram pt is flat SUPINE (prevent headache and leaking of CSF) Ptwithheatstroke flatwithlegselevated Tube feeding with decreased LOC PtonRightside(promotesemptyingofthestomach)Head of bed elevated (prevent aspiration) Skin infection VCHIPS Varicella zoster Cutaneous diptheria Herpes simplez Impetigo Peduculosis ScabiesCleft Lip positiononbackorininfantseattopreventtraumatothe suture line. while feeding hold in upright position. BKA(belowknee amputation) footof bed elevatedforfirst 24 hours. position proneto provide hip extension. detached retina areaofdetachmentshouldbeinthedependentposition administrationofenema ptshouldbeleftsidelying(Sim's)withkneeflexed. Aftersupratentorial surgery (incision behind hairline on forhead) elevate HOB 30-40 degrees After infratentorial surgery (incisionatthenapeofneck)positionptflatandlateralon either side. During internal radiation onbedrestwhileimplantinplace Aftertotalhip replacement don'tsleeponsideofsurgery,don'tflexhipmorethan45- 60 degress, don't elevate Head Of Bed more than 45 degrees. Maintain hip abduction by separating thighs with pillows. To prevent dumping syndrome (post operative ulcer/stomach surgeries) eatin reclining position. Liedown aftermeals for20-30 min. alsorestrict fluids during meals, low CHO and fiber diet. small, frequent meals. AKA(aboveknee amputation) elevateforfirst24hoursonpillow.positionpronedailyto maintain hip extension. Prolapsed cord KneetochestorTrendelenburg oxygen 8 to 10 LAutonomic Dysreflexia/Hyperreflex ia S/S pounding headache, profuse sweating, nasal congestion, chills, bradycardia, hypertension. Placeclient in sitting position (elevateHOB) FIRST! Shock bedrest with extremities elevated 20 degrees. knees straight, head slightly elevated (modified Trendelenberg)LumbarPuncture Aftertheprocedure,theptshouldbesupinefor4-12hours as prescribed. MyestheniaGravis worsens with exercise and improves with rest MyestheniaGravis a positive reaction to Tensilon---will improve symptoms Cholinergic Crisis Caused by excessive medication ---stop giving Tensilon...will make it worse. Liver biopsy (prior) must have lab results for prothrombin time Myxedema/ hypothyroidism slowed physical and mental function, sensitivity to cold, dry skin andhair. Grave'sDisease/ hyperthyroidism accelerated physical and mental function. Sensitivity to heat. Fine/soft hair. Thyroid storm increased temp, pulse and HTN Post-Thyroidectomy semi-fowler's. Prevent neck flexion/hyperextension. Trach at bedside HPeraitdon Ineja ulryDialysis e tule rnvaptt efHroOmBs3 id0edte ogsrie deeesBtE oFdOeRcErecahsecIkCinPg for kinks in (when outflow is inadequate) tubing Hypo-parathyroid Hyper-parathyroidHypervolemia bounding pulse, SOB, dyspnea, rales/crackles, peripheral edema, HTN, urine specific gravity<1.010. semi fowler's CATS--- Convulsi ons, Arrhyth mias, Tetany, Spasms, Stridor. (decreasedcalcium)givehighcalcium,lowphosphorus diet fatigue,muscleweakness,renalcalculi,backandjointpain (increased calcium)givealowcalciumhighphosphorous diet Hypovolemia increased temp, rapid/weak pulse,increase respiration, hypotension,anxiety.Urinespecificgravity>1.030Hypernatremia increased temp, weakness, disorientation, dilusions, hypotension, tachycardia. give hypotonic solution. Hypocalcemia CATSConvulsions, Arrythmias,Tetany,spasmsand stridor Hyper Mg depresses the CNS. Hypotension, facial flushing, muscle weakness, absent deep tendon reflexes, shallow respirations. EMERGENCY Addison's Hypo Na, HyperK, Hypoglycemia, dark pigmentation, decreased resistance to stress fx, alopecia, weight loss. GI stress. Cushings Hyper Na, Hypo K, hyperglycemia, prone to infection, muscle wasting, weakness, edema, HTN,hirsutism, moonface/buffalo hump Hyperkalemia MURDER Muscle weakness, Urine (olig, anuria) Resp depression, decreased cardiac contractility, ECG changes, reflexes Hypercalcemia muscle weakness, lack of coordination, abdominal pain, confusion, absent tendon reflexes, shallow respirations, emergency! Hypo Mg Tremors, tetany, seizures, dysthythmias, depression, confusion, dysphagia, (dig toxicity) Hyponatremia nausea,musclecramps,increasedICP,musculartwitching, convulsions.giveosmoticdiuretics(Mannitol)andfluids hypokalemia muscle weakness, dysrhythmias, increase K (rasins bananas apricots, oranges, beans, potatoes, carrots, celery) SIADH (increased ADH) change in LOC, decreased deep tendon reflexes, tachycardia. N/V HA administer Declomycin, diuretics Diabetesinsipidus (decreased ADH) excessiveurine outputand thirst, dehydration,weakness, administer PitressinPheochromocytoma hypersecretion of epi/norepi. persistent HTN, increased HR, hyperglycemia, diaphoresis, tremor, pounding HA; avoidstress, frequent bathing and rest breaks, avoidcold andstimulatingfoods (surgerytoremovetumor) Autonomic Dysreflexia FHR patterns for OB whattocheckwith pregnancy Positionofthebabyby fetal heartsounds Ventilatory alarms (potentiallylifethreatening emergency!) HOB elevate 90 degrees, loosen constrictive clothing, assess for full bladder or bowel impaction, (trigger) administer antihypertensives(maycause stroke,MI,seizure) Think VEALCHOP! V-variabledecels;C-cordcompressioncaused E-early decels; H- head compression caused A-accels; O-okay, noproblem L- late decels; P- placental insufficiency, can't fill Nevercheckthemonitorormachineasafirstaction. Always assessthepatientfirst.Ex..listentofetalheart tones with stethoscope. Posterior --heard at sides Anterior---midline by unbilicus and side Breechhigh upin thefundus nearumbilicus Vertex-bythe symphysis pubis. HOLD High alarm--Obstruction due to secretions, kink, pt cough etc Low alarm--Disconnection, leak,etc Tetrology ofFallot DROP (Defect, septal, Right ventricular hypertrophy, Overriding aortas, Pulmonary stenosis) Addesonian crisis N/Vconfusion, abdominal pain, extreme weakness, hypoglycemia, dehydration, decreased BPICPandShock ICP- IncreasedBP, decreasedpulse, decreasedresp Shock--Decreased BP, increased pulse, increased respIn anemergency patientswithagreaterchancetolivearetreatedfirst CardinalsignofARDS hypoxemia Edemaislocated in the interstitial space, not the cardiovascular space (outside of the circulatory system) thebestindicatorof dehydration? weight---and skin turgor heat/cold hotforchronicpain;coldforaccutepain(sprainetc) NCLEXanswertips chooseassessmentfirst!(assess,collect,auscultate, monitor, palpate) only choose intervention in an emergency or stress situation. If the answer has an absolute, discardit.Give priority to the answers that deal withthepatient'sbody,notmachines,or equipment. ARDSand DIC are always secondary to another disease or trauma forphobias use systematic desensitization whenaptcomesinand is in active labor firstactionofnurseistolistentofetalhearttones/rate ptwithleukemiamay have epistaxisduetolowplatelets Before starting IV antibiotics obtain cultures! lead poisoning testat12monthsofage brachial pulse pulseareaonaninfant Heroin withdrawal neonate irritable, poor sucking Cor pumonae Rightsidedheartfailurecausedbyleftventricularfailure (edema, jugular vein distention)before IV antibiotics? check allergies (esp. penicillin) make sure cultures and sensitivity has been done before first dose. Neutropenic pts nofreshfruitsorflowers Chesttubesareplaced inthepleuralspace Unstable Angina notrelievedbynitro PVC's canturnintoVfib. 1 tsp 5mL 1 oz 30mL 1 pint cup quart 8 2pints cups oz When pt is in distress. medication administration is rarely a good choice COPD and O2 with COPD baroreceptors that detect CO2 level are destroyed, therefore,O2mustbelowbecausehighO2 concentrationtakes awaythept'sstimulationtobreathe. Preload/Afterload Preload affects the amount of blood going into Right ventricle. Afterload is the systemic resistance afterleaving the heart. CABG GreatSaphenousveininlegistakenandturnedinsideout (becauseofvalvesinside).Usedforbypasssurgeryofthe heart. Prednisone toxicity Cushings (buffalo hump, moon face, high blood sugar, HTN) pneumonia feverandchillsareusuallypresent.Fortheelderly confusion is oftenpresent.I lb 16oz centigrade to Fahrenheit conversion F= C+40 multiply 5/9 and subtract 40 C=F+40 multiply 9/5 and subtract 40 Angiotenson II Inthelungs...potentvasodialator,aldosterone attracts sodium. Iron toxicityreversal deferoxamine S3 sound normalinCHF.NotnormalinMI Afterendoscopy check gag reflex TPNgivenin subclavianline painwithdiverticulitis located inLLQ appendicitis pain located in RLQ Trousseau and Chvostek'ssigns observed in Hypocalcemia nevergive K+in IVpush DKAis rare inDMII(thereisenoughinsulintopreventfatbreakdown) Glaucoma patientslose peripheral vision. Autonomic dysreflexia patients with spinal cord injuries are at risk for developing autonomic dyreflexia (T-7 or above) Spinal shock occurs immediately after injury multiple sclerosis myelin sheath destruction. disruptions in nerveimpulse conduction 1 g kg(gram) 1 20.200lbms gTIA transientischemic attack. mini stroke,nodead tissue. CVA cerebriovascularaccident. brain tissue dies. Hodgkin's disease cancerofthelymph.verycurableinearlystages if HR is <100 (children) Hold Dig earlysignofcystic fibrosis meconium in ileus at birth Meningitis--check for Kernig's/ brudinski's signs wilm's tumor encapsulatedabovekidneys...causesflankpain hemophilia is x linked passedfrommothertoson when phenylaline increases brainproblemsoccur buck's russell dunlaptraction traction traction knee femur skeletal immobility; or orlower skin leg dontadjustweights Myastheniagravis decrease in receptor sites for acetylcholine. weakness observed in muscles, eyes mastication and pharyngeal musles. watch for aspiration. burnsruleofNines head and neck 9% each upper ext 9% each lower ext 9% fronttrunk18% back trunk 18% genitalia 1% birth weight doublesby6months triples by1 year Gullian -Barre syndrome ascending paralysis. watch for respiratory problems.performamniocentesis before20weekstocheckforcardiacandpulmonary abnormalities Rh mothersreceive Rhogam toprotect nextbaby anterior fontanelle closes by...posterior by.. 18 months, 6-8 weeks caput succedaneum diffuseedemaofthefetalscalpthatcrossesthesuture lines. reabsorbes within 1 to 3 days placenta previa s/s placental abrutions/s there is no pain, but there is bleeding thereispain,butnobleeding(boardlikeabd) bethamethasone (celestone) surfactant.prematurebabies milieu therapy taking care of pt and environmental therapy cognitive therapy counseling pathological jaundice before 24 hours (lasts 7 days) occurs: after 24 hours physiological jaundice occurs: b ecrylamntp'sstiaraicstion c ahsieldizre ur ne<3 y <35 lbs with femur fxSSRI's takeabout3weekstowork five interventionsfor safety psych patients setting limits establish trusting relationship meds least restrictivemethods/environment patients with hallucinations patientswithdelusions redirect them distractthemdrawupregularand NHP? AirintoNHP,airintoRegular.Drawregular,thenNHP T Ahlz ohra ez imineeer'a snd Haldol c 6a 0n %coafuaslel d EePmSentias, chronic, progressive degenerative cognitive disorder. Cranialnerves S=sensory M=motor B=both Oh (Olfactory I) Some Oh (Optic II ) Say Oh (Oculomotor III) Marry To (trochlear IV) Money Touch (trigeminalV)But And (Abducens VI ) My Feel(facial VII) Brother A (auditory VIII) Says Girl's(glossopharyngealIX)Big Vagina(vagusX) Bras And (accessory XI) Matter Hymen (Hypoglossal XII)More Developmental 2-3months:turns headsidetoside 4-5 months:grasps,switchandroll 6-7months:sitat6andwavesbyebye 8-9 months: stands straight at 8 10-11 months: belly to butt 12-13 months: 12 and up, drink from a cup Hypernatremia S(Skin flushed) A (agitation) L(low grade fever) T (thirst)Hepatitis b B=bloodandbodyfluids(hepcisthesame) Apgar measures HRRRMuscletone,reflexes,skincolor. Each0-2points. 8-10ok, 0-3resuscitate Hepatitis A Endsinavowel,comesfromthebowelCushing's triad r/t ICP (HTN, bradycardia, irritability, sleep, widening pulse pressure) Thyroid storm HOT (hyperthermia) Myxedema coma COLD (hypothermia) Glaucoma No atropine Non Dairy calcium Rhubarb sardines collardgreens Koplick's spots prodomalstageofmeasles.Redspotswithbluecenter,in the mouth--think kopLICK in the mouth INH cancause peripheral neuritis Take vitamin B6 to prevent. Hepatotoxic Dumping syndrome Disseminatedherpes zoster localizedherpeszoster increasefatandprotein,smallfrequentmeals,liedown aftermeal to decreaseperistalsis. Wait1 hraftermealsto drink Disseminated herpes=airborne precautions Localized herpes= contact precautions. Anursewith localizedmaytakecareofpatientsaslongasptsarenot immunosuppressedandthelesionsmustbecovered! Weighted NI(naso intestinaltubes) Must float from stomach to intestine. Don't tape right away after placement. May leave coiled next to pt on HOB. Position pt on RIGHT to facilitate movement through pyloris Cushings ulcers r/tbraininjury Isoniazid causesperipheral neuritis Addison's disease: Cushing's syndrome: "add" hormone have extra "cushion" of hormone Glasgowcomascale eyes, verbal,motor Max-15pts,below8=comaCullen's sign ecchymosis in umbilical area, seen withpancreatitis Turner's sign Flank--greyish blue. (turn around to see yourflanks) Seen with pancreatitis McBurney's point Pain in RLQ with appendicitis LLQ Diverticulitis RLQ appendicitis watch for peritonitis Guthrietest TestsforPKU.Babyshouldhaveeatenproteinfirst shillingtest Test for pernicious anemia pancreatitispts put them in fetal position, NPO, gut rest, Prepare anticubital siteforPICC,theyareprobablygoingtoget TPN/Lipids Peritonealdialysis Its ok to have abd cramps, blood tinged outflow and leaking around site ifthe cath (tenkoff) was placed in the last 1-2weeks. Cloudyoutflowis neverok Latex allergies assessforallergiestobananas, apricots,cherries,grapes, kiwis, passion fruit, avocados, chestnuts, tomatoes and peaches Hyper reflexes absent reflexes uppermotorneuronissue(yourreflexesareoverthetop) Lower motor neuron issue Murphy's sign Painwithpalplationofgallbladder(seenwith cholecystitis)ALS (amyotrophiclateralsclerosis)degenerationofmotor neurons in both upper and lower motor neuron systems Transesophageal fistula esophagusdoesn'tfullydevelop.Thisisasurgical emergency (3 signs in newborn: choking, coughing, cyanosis) MMR is givenSQnotIM Tensilon used in myesthenia gravis to confirm diagnosiswhattoaskbeforeflu shot allergy to eggs whattoaskbefore MMR allergytoeggsorneomycin when onnitroprusside monitor: cyanide. normal value should be 1. William'sposition semiFowler'swithkneesflexedtoreducelowbackpain S/Sof hip fx External rotation, shortening adduction Fatembolism blood tinged sputum r/t inflammations. Increase ESR, respiratoryalkalosis. Hypocalcemia, increased serum lipids. complications of mechanical ventilation pneumothorax,ulcers Paget's disease tinnitus, bone pain, elnargement of bone, thick bones with allopurinol no vitamin C or warfarin! IVP requires bowel prep so bladder can be visualized acidashdiet cheese,corn,cranberries,plums,prunes,meat,poultry, pastry, bread alk ash diet milk, veggies, rhubarb, salmon codes forpt care Red-unstable,ie..occludedairway,activelybleeding...see first Yellow--stable, can wait up to an hour for treatment Green-- stable can wait even longer to be seen---walking wounded Black--unstable, probably will not make it, need comfort care DOA--dead on arrival Contraindication for Hep B vaccine anaphylactic reaction to baker's yeastTidalvolume is 7-10 ml/kg COPDpatients and O2 2LNCorless.TheyarechronicCO2retainersexpectsats to be 90% or less Kidney glucose threshold 180 Strangeranxiety is greatest at what age? 7-9months..separation anxiety peaks in toddlerhood whendrawinganABG put in heparinized tube. Ice immediately, be sure there are no bubbles and label if pt was on O2 pancreatic enzymesare taken with each meal! infants IM site Vastuslateralis Toddler 18 months+IM site Ventrogluteal IMsiteforchildren deltoid and gluteus maximus Munchausen syndrome vs munchausen by proxy multiple sclerosis hungtington's Munchausenwillselfinflictinjuryorillnesstofabricate symptoms of physical or mental illness to receive medical careor hospitalization.byproxymotherorothercare takerfabricates illness in child motors/slimbweakness,paralysis,slowspeech.sensory s/s numbness, tingling, tinnitis cerebral s/s nystagmus, atazia, dysphagia,dysarthia 50% genetic autosomal dominanat disorder.. s/s uncontrolled muscle movements of face, limbs and body. no cure WBCleftshift ptwithpyelo.neutrophilskickintofightinfections o thryarnogide mtaegdinsipdseycehffects inseommenrigae. nbtopdsyymchetabolism increaseslumbarpuncture fetalposition. post-neuro assess q15-30 untilstable. flat2-3 hour. encourage fluids, oral analgesics for headache. ECG no sleep the night before, meals allowed, no stimulants/tranquilizers for24-48 hours before.may be askedtohyperventilate3-4minandwatchabright flashinglight.watchforseizuresaftertheprocedure. laparoscopy CO2 used to enhance visual. general anesthesia. foley. post--ambulate to decrease CO2 buildup PTB lowgradeafternoon fever Thoracentesis: Cardiac cath positionptonsideoroverbedtable.nomorethan1000 ccremoved atatime.Listenforbilateralbreathsounds, V.S,check leakage, sterile dressing NPO8-12hours.emptybladder,pulses,tellptmayfeel heat, palpitationsordesiretocoughwithinjectionofdye. Post: V.S.--keep leg straight. bedrest for 6-8 hr Myelogram Liver biopsy NPO for 4-6 hours. allergy hx phenothiazines, cns depressants and stimulants withheld 48 hours prior.Table moved to various positions during test. Post--neuro assessment q2-4 hours, water soluble HOB UP. oil soluble HOBdown.oralanalgesicsforHA.Nopo fluids.assessfor distended bladder. Inspectsite administerVitaminK,NPOmorningofexam6hrs.Give sedative. Teachpttoexpecttobeaskedtoholdbreathfor 5-10sec.supide position, lateralwith upperarms elevated. Post--positiononRIGHT side.frequentVS.reportsevere ab pain STAT.no heavy lifting 1 wk Paracentesis semifowler'soruprightonedgeofbed.Emptybladder. postVS--reportelevatedtemp.watchforhypovolemia Cerebral angioprep well hydrated, lie flat, site shaved, pulses marked. Post-- keepflatfor12-14 hr. checksite,pulses,force fluids.emphysema barrel chest kawasaki syndrome strawberry tongue perniciousanemia redbeefy tongue downs syndrome protruding tongue cholera ricewaterystool malaria stepladder like fever--withchills typhoid rosespotson theabdomen diptheria pseudo membrane formation measles koplick's spots sle (systemic lupus) butterfly rash pyloric stenosis olive likemass Addison's bronze like skin pigmentation Cushing's moon face, buffalohump hyperthyroidism/ grave's disease exophthalmos myasthenia gravis descending musle weakness gullian-barre syndrome ascending muscle weakness angina crushing, stabbing chest pain relieved by nitro MI crushing stabbing chest pain unrelieved by nitro cystic fibrosis salty skin DM polyuria, polydipsia,polyphagia DKA kussmal'sbreathing(deeprapid) p asntehummaonia r wuhsetyezspinugtuomn;ewxhpeirnatpioenrcuss-will hear dull soundsretinal detachment floaters and flashes of light. curtain vision glaucoma painfulvision loss. tunnelvision. halo retino blastoma cat'seyereflex increased ICP hypertension,bradypnea,,bradycarday(cushing'striad) shock Hypotension, tachypnea, tachycardia Lymesdisease bullseye rash glomuloneprhitis the most important assessment is blood pressure children5 and up shouldhaveanexplanationofwhatwillhappenaweek before surgery Kawasakidisease (inflammation of blood vessles, hence the strawberry tongue) causes coronary artery aneurysms. intraosseous infusion oftenusedinpedswhenvenousaccesscan'tbeobtained. hand drilled through tibia where cryatalloids, colloids, blood products and meds are administered into the marrow. one med that CANNOT be administered IO is isoproterenol, a beta agonist. sicklecellcrisis two interventions to prioritize: fluids and pain relief. BPaHdder CA p readinulceessdhseizmeaatnudriaforce of urineventriculoperitoneal shunt watchforabdominaldistention.watchfors/sofICPsuch ashigh pitchcry,irritabilityandbulgingfontanels.Ina toddler watch for loss of appetite and headache. After shuntisplacedbedpositionis FLATsofluiddoesn'treduce toorapidly.Ifpresentings/sofICPthen raisetheHOB15- 30 degrees 3-4cupsofmilkaday for a child? NOtoomuchmilkcanreducetheintakeofothernutrients especially iron. Watch for ANEMIAHeadinjuryorskullfx no nasotracheal suctioning otitismedia feed upright to avoid otitis media! antiplatelet drug hypersensitivity bronchospasm bowel obstruction more important to maintain fluid balance than to establish a normal bowel pattern (they cant take in oral fluids) Basophils reliease histamine duringanallergicresponse Iatragenic means it was caused by treatment, procedure or medication Tamoxifen watch for visual changes--indicates toxicity post spelectomy pneumovax 23 is administered to prevent pneumococcal sepsis Alkalosis/ Acidosis and K+ ALKalosis=al K= low sis. Acidosis (K+ high) No phenylalanine nevergive potassium toakid ptwho withhas PKU. lowNourine meat, output! dairyoraspartame cryptorchidism undescendedtesticles!riskfactorfortesticularcancer later in life. Teach self exam for boys around age 12--most cases occurin adolescence positioning for pneumonia lay on affected side, this will splint and reduce pain. However,if youaretryingtoreducecongestion,thesick lunggoesup!(like whenyouhaveastuffynoseandyou laywith that side up, it clears!) for neutropenic pts nofreshflowers,freshfruitsorveggiesandnomilk CSF meningitis HIGH protein LOW glucose MMR and varicella immunizaions after15 months!Digitalis increasesventricularirritability ---couldconvertarhythm to v-fib followingcardioversion Coldstressandthe newborn biggest concern resp. distress Parathyroid relies on vitaminDtowork Glucagon increases the effects of? anticoagulants PE NeedsO2! DKA acetone and keytones increase! once treated expect postassium to drop! have K+ ready normal PCWC (pulmonary capillary wedge pressure) is 8-13 readings 18-20 are considered high Sucking stabwound coverwoundandtapeon3sidestoallowairtoescape.If you cover and occlude it--it could turn into a closed pneumo ortension pneumo! chesttubepulledout? occlusive dressing firstsignofPE suddenchestpainfollowedbydyspneaandtachypnea thefirstsignofARDS increased respirations! followed by dyspneaand tachypnea nephrotic syndrome characterized by massive proteinuria caused by glomerulardamage. corticosteroids are the mainstayHirschprung's Intussusception diagnosedwithrectalbiopsy.S/Sinfant-failuretopass meconium and later the classic ribbon-like/foulsmelling stools Common inkids with CF.Obstruction may cause fecal emesis, current jelly stools. enema---resolution=bowel movementsTBdrugsare hepatotoxic! clozapine, Clozaril antipsychotic anticholinergic clozapine s/e weightgain,hypotension,hyperglycemia,agranulocytosis dehydration -hypovolemia -elevatedurinespecificgravity flumazenil, umbilical cord Romazicon benzo overdose compression repositionsidetosideorknee-chest short cord discontinue pictocin upstairs withcrutches? down stairs with crutches? good legfirstfollowedbycrutches(good girlsgoto heaven) crutches with the injured leg followed by the good leg. dumping syndrome? uselowfowler'stoavoid.limitfluids nitrazine paper turns blue with alkaline amniotic fluid. turns pink with other fluids a nurse makes a mistake? takeittohim/herfirstthentakeupthechain CF chiefconcern? Respiratory problems pancreatitis firstpainrelief,secondcoughanddeepbreathe Addison's causes severhypotension! Toddlers needto express independence! laboring mom'swater breaks? first thing--worry aboutprolapsed cord!Defamation isafalsecommunicationorcarelessdisregardforthetruth that causes damage to someone's reputation. in writing(Libel) or Verbally(Slander) quadcane place of unaffected side of body placeit6-12ininfrontofthebodybeforewalking steps forward with affected legfirst bringtheunaffectedlegaswell,bringingthefootpastthe cane Sprain or Strain RICE Rest Ice Compress Elevate Imprisonment Tellingtheclientyoucannotleavethehospital Assault Threatening to give pt. medication puttinganotherpersoninfearofaharmfuloranoffensive contact. Battery performing procedure without consent TB ApositiveMantouxtestindicatesptdevelopedanimmune response to TB. Acid-fast bacilli smear and culture:(+suggests an active infection)thediagnosisisCONFIRMbyapositiveculture for M TB Achestx-raymaybeorderedtodetectactivelesionsin the lungs QuantiFERON-TB Gold: DIAGNOSTIC for infection, whether it is active or latenthandrollineachhand maintainsfunctionalpositionbacterial meningitis Kernig sign, nuchal rigidity,areclinicalmanifestations fetalheartrateend of first trimester place the scope midline just above the symphysis pubis and apply firmpressure thrombocytopenia dont blow yournose=bleeding delirium fluctuating level of consciousness; more agitated in the evening; acute memory deficit ptonseizure precautions havesuctionnexttobedavailable,keepsiderailsup outcome audit goodtocheckifinfectionrateshavedeclined;thisaudit determine results from a specific intervention impaired vision client colortapestairs-goodforsafety Ethambutol (Myambutol)-for tb loss of color discrimination-discontinue Fluoxetine (Prozac) asthma kid report tremors, agitation, confusion, anxiety, hallucinations=serotonin syndrome (risk in the first 2-72 hrs after givenfirsttime); clientwillstopthemeds;weight gain/diabetes/ hyperglicemia should participate in sports, inhalerpriorto sports, stay inside whencold,usepeakflowmetereverydaysame time, annual influentavaccine important increased ICPin bacterialmeningitissign memory lossNitropatch effective 20 to 60 min afterapplied; chest, back, abdomen, anterior tight-bestlocations;keeppatchon12to14hrsa day,not more so tolerance is prevented Celebrex(OA) contraindicated in pt's allergic to sulfa meds-because it cotains sulfafullliquiddiet peanut butter, ice cream, grape juice vancomyocyn hearring loss stage II pressure ulcer partialthicknessskinloss stage III vissible subq fat-full thickness skin loss stage IV exposed muscle DexamethasoneforRA intermittententeraltube feeding diarrhea after each feeding AE: hyperglycemia, glicosuria, adrenal insufficiency, osteoporosis, infection, myopathy, fluid and electrolyte imbalance, cataracts, pud intervention: reduce rate of feeding or switch to continuous feeding breast CAsigns after CVA-possible problems swallowing and risk foraspiration report: dumpling of the tissue=tissue is retracted, silver striaeexpected, new nipple inversion-report, if pthad it eversince menarche-ok,visiblesymmetricalvenous pattern-ok, not symmetrical-not ok chin to chest will help Digoxin levels report 3.0-toxic intermittententeraltube feeding room temperature formula, not cold-if not-cramps, nausea, vomiting;elevate bedtoatleast30degreeswhilefeedingwrapping culf to loose on the arm falsehighBP modified3pointcrutch gait-going upstairs order standandbearweightontheunaffectedleg transfer body weight to the crutches advancetheunaffectedlegbetweenthecrutches shiftleg fromthecrutchestotheunaffectedleg alling crutches on the stairs enema position sims-onthesidewithkneesflexedHeparin giveinthebelly afterpartial mastectomy expect drainage tubes, they can start ROM within 25 hrs, no pick upthings delegate toUAP feeding a alzheimer pt with aphasia borderline personality disorder would cut himself/harm self/self mutilation antisocial lackofremorse followingtotalknee arthroplasty CPM receive-stop during meal times signsforincreasedICP irritability dehydration increased urine specific gravity hypotonic dehydration willhavelowsodium,sonormalsodiumwillshowthatptis responding well to oral rehydration solution thoracentesis avoiddeepbreathingduringprocedure-willavoid puncture of thepelura boggyuterusPP massage to preventbleeding preeclampsia report decreased urine output, edema of hands and face; don decrease fluids-drink 2-3 L a day failure tothrive checkformomandbabybonding;developastructure routine with baby; feed as needed c Tu hlofrtaozoinweide fdarlysemlooouwthB,Pph reoatdoisnegnsitivityNGtubeverify placement if new-xray if not new, just to verify before new feeding-aspirate contents ofthe tube and verifyPH (1-4) Crohn's disease pt with enteroenteric fistula low fiber diet, increased K, increased protein, increased caloriesPAD (peripheralarterial disease) lubricate skin offeetwith lotion, don't use heating pads, trim toenailsstraight,dontelevatefeetabovelevelof heart Theophylline (Theochron) toxicity anorexia, tachycardia, albuminuria, hypotension Oppositional defiant disorder disobedience Autismkid lackof responsiveness, less interest inothers, impaired social interactions, repetitive movements ?, incidence report dontmentioninachart sickle cell anemia crisis fluids first, pain after Babinski strokeouterareaoffootmovingupwardstoma care barrier-hold itfor30 secsbeforeputtingthe bag on infant pulsecheck brachialartery Digoxin(Lanoxin) toxicity s/s nausea, diarrhea Estradiol (Climara) report headache eye drops administration keepeyesclosedfor1minaftervacuum assisted birth complications formom perineal, vaginal and cervical lacerations good coping exercising,doingahobby crisis interventions helpclientfindoutthecauseofhisreaction AIDS no exposure to soil=no gardening; dont use pepper; dont eatfoodthathasbeensittingoutformorethan1hr;wash toothbrush in dishwasher weeklyRACE assessptfirst evisceration staywithptandcallforhelp,coverwith sterile,putpt supine with bend knees, assess vitals newborn ascultate pulse listen apical pulse for 1 min episiotomy sitz bath 24 hrs after (will increase circulation), sit on hard surface, ice packs (reduce edema and discomfort) Cushings moon face, hypertension, weight gain Arthroplasty postop primarything-prevent bleeding newborn prevent conduction heat loss putapaperinbetweenbabyandmetaltable Post partumclient riskofDVT-unilaterallegpain,calftenderness,legswelling Cyclophosphomide (Cytoxan)foratoddler for neuroblastoma increase fluids to preventhemorrhagic cystitis, giveearly in theday intravenous pylogram laxativerightbeforeprocedure,clearliquidsornothing after midnight, check forallergies for seafood, milk, eggs, chocolate; encourage fluidsaftertoremovedye immobile client usetrochanterrolls,lotsoffluids,nomassage Coumadin first5days-bloodworkqday,don'ttakeacetaminophenRespiratory acidosis uncompensated lowph,highCO2,normalbicarb sterile field/ aseptic technique maintain things within line of vision, 1 in border is contaminated, nothing bellow waist, dont tie dr's gown in the BACKthats contaminated, dont turn your back on the field, tight hands togetherabove waist Infertility aftertryingoneyear,refertosupportgroupMAOI avoid tyramine foods like: avocado, smoked meats, cheeses, Cefazolin infusion piggybagwith0.9NaCl-ifNaClisalreadyrunning thrombocytopenia low platelets; risk for bleeding; avoid venipunctures neutropenia wbclow;nofreshflowerorfruits;limittimewithfamily peritonitis members when visiting rigidboardlikeabdomen,absentbowelsounds,wbc RDS 20,000; fever; REPORT maintain normalbody temp-main priority Suctioning-pt with tracheostomy following a laryngectomy pass catheter no more than three times, cough is normal- expected, surgicalNotmedicalasepsisused,resistance-> withdraw catheter1- 2 cm crutchesgoingupthe stairs advanceunaffectedlegtothestairs,placetheputweight ongoodleg andcruthes,weightonunaffectedlegand thecrutches,advance affectedlegandcrutchesforward up thestairs nauseaalternative method adjustable band with bead Amitryptaline (Elavil)for depression-TCA anticholinergic, watch for dry mouth and constipation; take it with or right after food, urine could turn blue-green, Brethine (Terbutaline) and MagSulfate eitheronearegiventodecreasepretermlabor contractions-its a muscle relaxant Nubain/Nalbuphine painreliefduringlabor Pitocin postpartumbleedingprevention;heavylochiaandboggy fundus Respiratory acidosis compensated lowph,highCO2,increasedbicarbEvisceration and dehiscence require emergency treatment. ■ Call forhelp. ■ Stay with theclient. ■ Coverthewoundandanyprotrudingorganswithsterile towels or dressings soaked with sterile normal saline solution.Donot attempttoreinserttheorgans. ■ Positiontheclientsupinewiththehipsandkneesbent. ■ Observe forsigns ofshock. ■ Maintain acalmenvironment. ■ KeeptheclientNPOinpreparationforreturningto surgery. estrogen replacement therapy helps prevent osteoporosis; also exercisedoes earlydecells continuetoobserv neuborn-REPORT and immediateattention grunting, tachypnea,nasalflaringhypertrophic pyloric stenosis (peds) Projectilevomiting,Drymucusmembranes,Constant hunger Hirschsprung disease (peds) surgery to remove the affected segment of the intestine, low-fiber, high-protein, high-calorie diet. Meckel's diverticulum bed restto preventbleeding Ulcers ◯ Stage I - Intact skin with an area of persistent, nonblanchable redness, typically over a bony prominence, thatmayfeelwarmeror coolerthantheadjacenttissue. Thetissueisswollenandhascongestion,withpossible discomfortat thesite. Withdarkerskintones,theulcermay appear blue or purple. ◯ Stage II - Partial-thickness skin loss involving the epidermis and the dermis. The ulcer is visible and superficial and may appear as an abrasion, blister, or shallow crater. Edema persists, and the ulcer may become infected,possiblywithpainandscant drainage. ◯StageIII-Full-thickness tissueloss with damage toor necrosisof subcutaneoustissue.Theulcermayextend downto,butnot through,underlyingfascia.Theulcer appearsasadeepcraterwith orwithoutunderminingof adjacenttissueandwithoutexposed muscleorbone. Drainage and infection are common. ◯StageIV-Full-thicknesstissuelosswithdestruction, tissue necrosis, ordamage to muscle, bone, or supporting structures. There may be sinus tracts, deep pockets ofinfection, tunneling, undermining, eschar (blackscab-like material), orslough (tan, yellow,orgreen scab-like material). ◯Unstageable-Nodeterminationofstagebecause eschar or slough obscures the wound. Intussusception (peds) red currant jelly stools, bloody mucus stools, telescoping intestine,resultingsausageshapedabdominalmass.Meckel's diverticulum Abdominal pain, Mucus, bloody stools risk fornewborn hypoglicemia motherhasdiabetes mellitus postoperativefollowing cleft lip and palate repair prone position to facilitate drainage RDS newborn ■ Tachypnea(respiratoryrategreaterthan 60/min) ■ Nasalflaring ■ Expiratorygrunting ■ Retractions ■ Laboredbreathing with prolongedexpiration ■ Fine crackles onauscultation ■ Cyanosis ■ Unresponsiveness, flaccidity,andapneawithdecreased breath sounds(manifestationsofworsenedRDS) cleft lip and palate bottlewithaone-wayvalve,wide-basednipplebottlecroup Dry, barking cough phototherapy forhigh billirubin ■ Maintainaneyemaskoverthenewborn'seyesfor protection of corneas and retinas. ■ Keepthenewbornundressedwiththeexceptionofa male newborn.Asurgicalmaskshouldbeplaced(likea bikini)overthe genitaliatopreventpossibletesticular damagefromheatandlight waves.Besuretoremovethe metalstripfromthe masktoprevent burning. ■ Avoidapplyinglotionsorointmentstotheskinbecause they absorb heatand can cause burns. ■ Removethenewbornfromphototherapyevery4hr,and unmask the newborn'seyes, checking for inflammation or injury. ■ Repositionthenewbornevery2hrtoexposeallofthe body surfacestothephototherapylightsandprevent pressure sores. ■ Checkthelampenergywithaphotometerperfacility protocol. ■ Turnoffthephototherapylightsbeforedrawingblood for testing. Authoritative Makes decisions for the group. ◻ Motivates by coercion. ◻ Communication occurs down the chain of command. ◻ Work output by staff is usually high - good for crisis situations and bureaucratic settings. ◻ Effective for employees with little or no formal education. epiglottitis Difficulty swallowing, high fever, Drooling, stridorDemocratic ◻ Includes the group when decisions are made. ◻ Motivates by supporting staff achievements. ◻ Communication occurs up and down the chain of command. ◻ Work output by staff is usually of good quality - good when cooperation andcollaboration are necessary Laissez-faire ◻ Makes very few decisions, and does little planning. ◻ Motivation is largely the responsibility of individual staff members. ◻ Communication occurs up and down the chain of command and between group members. ◻ Work output is low unless an informal leader evolves from the group. ◻ Effective with professional employees.Quality Improvement ◯ Outcome, or clinical, indicators reflect desired client outcomes related to the standard under review. ◯ Structure indicators reflect the setting in which care is being provided and the available human and material resources. ◯ Process indicators reflect how client care is provided and are established by policies and procedures (clinical practice guidelines). ◯ Benchmarks are goals that are set to determine at what level the outcome indicators should be met QI eg Cane,leftlegis affectedW h il e p r o c e s s i n d ic a t o r s p r o vi d e i m p o rt a n t i n formation about how a procedure is being carried out, an outcome indicatormeasures whether that procedure is effective in meeting the desired benchmark. For example: the use of incentive spirometersinpostoperativeclients may be determined to be 92% (process indicator) but the rate of postoperative pneumonia may be determined tobe 8%(outcome indicator).Ifthe benchmarkissetat5%,thebenchmarkfor that outcome indicatoris not being met and the structure and process variables need to be analyzed to identify potential areas for improvement holdcaneonstrongside,keeptwopointssupportallthe timeonthe ground,placecane6to10ininfrontbefore advancing,advance weaklegfirstfollowedbygoodleg, advance strong lef past the canePericarditis pericardial friction rub MAOI's SE-metallic taste Fluoxetine/Prozac-SSRI SEROTONIN SYNDROME-headache hypotension, urinary frequency, Sodium (Na) 136-145 mEq/L Calcium 9.0-10 mg/dL Chloride 98-106 mEq/L Bicarb HCO 21-28mEq/L Potassium 3.5-5.0 mg/L PhosphorusPO4 3.0-4.5 mg/dL Magnesium 1.3- 2.1mEq/L Stomach pH 1.5-2.5 Ammonia 15-110 mg/dL Bilirubin • Total 0-1.0 • Unconjugated (indirect) 0.2-0.8mg/dL • Conjugated (direct) 0.1 1.0 mg/dL C Pnaerduimacothaomrpaxonade m traucffhleadlhdeeavritatsiounnds, pulsus paradoxus,Cholesterol Liverenzymes • Total <200mg/dL • LDL ("bad") <100 • HDL ("good)>40 • Triglycerides <150mg/dL • ALT/SGPT 8-20units/L • AST/SGOT 5-40units/L • ALP 42-128units/L • Total protein 6-8gm/dLRBC • Females 4.2-5.4 million/uL • Males4.7-6.1million/uL WBC 5000-10,000 MCV 80-90mm3 MCH 27 -31pg/cell TIBC 250-460 mcg/dL Iron • Females60-160mcg/dL • Males 80-180 mcg/dL Platelets 150,000-450,000 Hemoglobin (Hgb) • Females 12-16g/dL • Males 14-18 g/dL Hematocrit (Hct) • Females 37-47% • Males 42-52% ProthrombinTime (PT) (Coumadin) 11-14 seconds: therapeutic range 1.5-2x normal or control value Partial thromboplastin Time (aPTT) (Heparin) 16-40range; therapeutic range1.5-2xnormalorcontrol value INR 0.9- 1.2 but 2 to 3on Coumadin therapy (therapeutic) D-dimer • 0.43- 2.33 mcg/mL • 0 to 250 ng/mL Fibrinogen levels 170- 340mg/dL Pancreatic enzymes • Amylase 56-90IU/L • Lipase 0-110 units/L • Prothrombin time 0.8-1.2 Glucose • Preprandial(fasting)70-110mg/dL • Postprandial 70-140mg/dL • HbA1c (glycosylated hemoglobin) <6%Urine specific gravity 1.015-1.030 Urine pH average6.0;range4.6-8.0 Urinalysis Negative for glucose, RBC, WBC, Albumin, bacteria: <1000 colonies/ml Glomerularfiltration rate (GFR) 90-120 ml/min BUN 10-20 mg/dL Creatinine males 0.6- 1.2 mg/dL;female 0.5-1.1 Arterial BloodGases pH 7.35 -7.45 (ABG) Pa02 80-100 mmHg PaC02 35-45 mmHg HCO3 21 - 28 mEq/L Sa O2 95-100% Cl 98-106 Creatinine phosphokinase MB (CK- MB) normal 30-170 units/L *increase 4-6 hrs after MI and remains elevated 24-72hrs troponin normal <0.2 ng/dL *gold standard for MI Fibrin degradation products < then 10 mcg/mLDescribe the following ECG findings in 2nd degree block - Mobitz Type 1 (Wenckebach): rhythm rate QRS duration P:QRS ratio Pwaverate P-Rinterval Describe the following ECG findings in 1st degree AV block: rhythm rate QRS duration Pwave Pwaverate P-RintervalWhat causes a 2nd degree block - Mobitz Type 2? What type of heart block is associated with a QRS drop? 2nd degree heartblock Describe the following ECG findings in 2nd degree block - Mobitz Type 2: rhythm rate QRS duration P:QRS ratio Pwaverate P-RintervalList 3 causes of sinus tachycardia. List the 3 basic mechanisms for tachyarrhythmias. Which is mostcommon? increased automaticity of pacemaker spontaneous depolarizations re-entrant circuit (most common) Describe the following ECG findings in 3rd degreeblock(complete AV block): rhythm rate QRS duration Pwave Pwaverate P-RintervalReduced function of what channelsleadsto a prolonged plateau period, leading to a prolongedQT interval? potassium channels Duringwhich2phases of the ventricular action potential do spontaneous depolarizationsoccur? phase3 phase4 What phase of the ventricular action potential corresponds to the ST segment? phase 2 Describe the following ECGfindingsinsinus tachycardia: rate isless than 150 beats perminute rhythm rate QRS duration Pwave P-RintervalA "twisting" polymorphic ventricular tachycardia that is observed in situations where the QT interval has been prolonged What fataldisorderis associated with torsadesdepoints? torsades de pointes ventricular fibrillation List 3 examples of reentrant arrhythmias. Atria tachycardia atrial flutter atrial fibrillation supraventricular re-entrant tachycardia as in WolffParkinson-White syndrome ventricular tachycardia Describe the mechanism ofreentrant circuit tachyarrhythmia.A 17-year-old boy is referred to a cardiologist by a primary care physician for evaluation of recurrent spells of dizziness.Duringthe episodes, he feels intense anxiety with palpitations and breathlessness.Heis asymptomatic in between episodes; There is no h/o chest pain or syncope. Physical examination:No abnormalities detected Lab: EKG: Short PR interval; wideQRSwithaslurred upstroke. Blood: Normal; Chest X ray: Normal List 3 ECG findings in Wolff-Parkinson-White syndrome. Wolff-Parkinson-White syndrome short PRinterval wide QRS delta waveWhatisthenameofthe wide QRS wave with a slurred upstroke seenin Wolff-Parkinson-White syndrome? delta wave - widened QRS signifies pre-excitation What disorder is caused by an accessory atrioventricular connection leading to reentrant supraventricular tachycardia? Wolff-Parkinson-White syndrome Compare WolffParkinson-White syndrometolong QT syndrome.A46-year-old woman arrived in the ER complaining of sudden onset of palpitations, lightheadedness, and shortness of breath. These symptoms began approximately2hours previously. PE: BP 95/70 mm Hg HeartRate-averages 170 beats/min, regular Rest of her physical examination is unremarkable EKG: abnormal P waves; P-R intervalsarewithin normal limits; normal QRS complexes supraventricular tachycardia How can one use an ECG to differentiate between supraventricular and ventricular tachycardia? Ifthe QRS complexis narrow (<3smallboxes) - SVT. IftheQRS complexiswide(>3smallboxes)-VT.List 4 types of supraventricular tachycardias. atrial tachycardia atrial flutter atrial fibrillation AV node reentranttachycardia atrioventricular reentranttachycardia Describe the following ECG findings in supraventricular tachycardia: rhythm rate QRS duration Pwave P-RintervalA 44-year-old male complainsofoccasional palpitations, shortness of breath,dizzinessand chest discomfort. Physical examination:Pulse: Irregularly irregular JVP: absent "a" waves Heart sounds: variable intensity S1 with occasional S3 Lab: EKG: Variable ventricular rate(90-190); IrregularRR intervals. Blood:CK-MBnormal Chest Xray: Normal atrial fibrillation Describe the following ECG findingsin atrial flutter: rhythm rate QRS duration Pwave Pwaverate P-RintervalAtrialflutter(SVT)atrial rate 250-350/min Atrialfibrillation (SVT) atrial rate > 350/minand multifocal Describe thefollowing ECG findings in atrial fibrillation: rhythm rate QRS duration Pwave P-Rinterval Atrial tachycardia (SVT) atrial rate 150-250/minList 3 possible diagnoses ifQRS<120 ms. List 3 possible diagnoses ifQRS>120 ms. sinus arrhythmia supraventricular rhythm junctional tachycardia ventricular tachycardia supraventricularrhythm with additionalbundle branch block additional accessory AV pathway Describe thefollowing ECG findings in ventricular fibrillation: rhythm rate QRS duration Pwave Describe thefollowing ECG findingsin ventricular tachycardia: rhythm rate QRS duration PwaveA patient asks you He can modify his risk for cardiovascular disease by losing about his risk of weight and notsmoking cardiovascular disease. He is 50-years old and has diabetes,is overweight andsmokes cigarettes. Youadvise him that: Which of the following is true of the coronary arteries? The coronary arteries begin just above the aortic valve In the event of a coronary artery blockage,themuscle of the heart can receive blood from the: The right atrium receives bloodfromthe systemic circulationand the: Thevalvebetweenthe right atrium and the rightventricleisthe: Anastomoses that provide collateral circulation Coronary veins Tricuspidvalve Stroke volume depends on preload, afterload, and: Relaxationoftheheart is referred to as: Diastole The circumflex artery is a branch of the: Left coronary arteryMyocardial contractilityAn increase in peripheral vascular resistance: Decreases stroke volume The ventricles of the heart are innervated mainly by: Parasympathetic control of theheartisprovided by the: The resting membrane potential is determined primarily by the difference betweenthe intracellular potassium ion level and the Sympathetic nerve fibers Vagus nerve Extracellular potassium ionlevel The sodium-potassium pump functions to move: Potassium ions into the cell and sodium ions out of the cell Depolarization takes place when: Sodiumionsrushintothecell Toincreasecardiac output, you can: Increase both heart rate and stroke volume Themostimportant factor indetermining stroke volume in a healthy heartis: Preload The Starling law states that: Myocardialfiberscontractmoreforcefullywhentheyare stretchedThe activation of myocardial tissue more than one time bythe same impulse is called: Reentry Phase I of the action potential representsthe period of: Duringtheperiod between action potentials: The AV junction is formed bytheAVnode and the: Early rapid repolarization There is excessive sodium in the cell Bundle of His You are treating a patient who has a damagedSA nodethat isnolonger pacingthe heart. You would expect the patient's heart to: Which of the following cardiac pacemakers has an intrinsicrate of40to 60 beats per minute? Beat more slowly AV junction Acetylcholine affects the heart by: Decreasing heartrate The dominant pacemaker of the heart under normal conditions is the: SAnodeWhich of the following is a bipolar lead? Lead II In lead II ECG placement, the positive lead is located on the: Left leg Leads II and III are: Inferiorleads LeadIlooksattheheart from what view? Lateral A lead used for routinely monitoring dysrhythmias is: Lead II You are treating a 75- yearold woman who hasa historyofdiabetes and atherosclerosis. Her chief complaint is persistent heartburn. You suspect: Jugularvein distention in cardiac patients should be evaluated with the patient positioned: While assessing a patient you identify a carotid bruit.Thisleads youto believethatthe patient: This may be a cardiovascular problem With the head elevated 45 degrees Has atherosclerosis An ECG can help to determine: Whether there is ischemic cardiac muscleWhen preparing for a 12-lead ECG, locate the 4th intercostal space, just to the right of the sternum and place lead: V1 The first upward deflection on an ECG tracing is the: Pwave Aparamedicplaces10 leads: 4 on the limbs and 6onthechest.The paramedic ispreparing for viewinga: 12-lead ECG StandardECGpaperis divided into 1-mm blocks andmovespast thestylusof theECGat 25mmper second. Eachsmallblock represents: 0.04 second The PR interval representsthetime it takes an electrical impulse to: Each small square of graph paper represents _____ mV. 0.1 In a 12-lead ECG, leads V1 and V2 are: Septal leadsBe conducted through the atria and the AV nodeTheduration oftheQRS complex should be _____ second. While analyzing an ECG you cannot identify a Q wave. Thismeans: 0.08 to 0.10 The Q wave may not be visible in the lead you are viewing Deep and symmetrically inverted T waves may be indicativeof: The part of the ECG tracing that is most important for detecting life-threatening arrhythmias is the: Thetriplicatemethodof determiningheartrate is: WhenanalyzinganECG tracing,younoticethat the rhythm is highly irregular. The best methodto calculate the rate is the Cardiac ischemia QRS complex Accuratewhentheheartrateisnormalandgreaterthan 50 beats per minute Six-second count method The STsegment reflects the: Early repolarization of the ventriclesWhileevaluatinga22- yearoldfemalerunner who called 911 because shefell andtwistedher ankle, you apply an ECGmonitor.Her heart rateis46,Pwavesare normaland upright, the PR interval is 0.16 second, and the QRS complex looksnormal. Thereisa QRScomplex following eachPwave. The patient's ECG tracingreflects: Whileevaluatinga22- yearoldfemalerunner who called 911 because shefell andtwistedher ankle, you apply an ECGmonitor.Her heart rateis46,Pwavesare normaland upright, the PR interval is 0.16 second, and the QRS complex looksnormal. Thereisa QRScomplex following eachPwave. Treatment for this patient's heart rate should include: Sinus bradycardia No treatment at this time An undesirable side effect of atropine is: Increased myocardial oxygen demandIsoproterenol raises the heart rate by functioning asa: ECG analysis reveals that eachPwaveinthe tracing hasadifferent shape.The heartrateis 80beatsper minute. This is called: Whichofthefollowing may cause sinus bradycardia? Beta agonist Wandering pacemaker Intrinsic sinus nodedisease An ECG strip shows a regular rhythm with a QRScomplexof0.08,a rate of145, aPRinterval of0.12, andoneupright P wave before each QRS complex. You suspectthatthisrhythm is: Sinus tachycardia Atropineworksby inhibiting: ParasympatheticresponseYou are called to evaluate a 64-year-old womanwho complains of palpitations, weakness, and dizziness. Her heartrate is160beatsper minute, her blood pressure is 118/ 80 and her respiratoryrateis28. TheECGtracingshows narrowQRScomplexes and no identifiable P waves. The first recommended treatment for this patient is: Valsalva maneuver You are called to evaluatea64-year-old womanwhocomplains of palpitations, weakness, and dizziness. Her heart rate is160 beats perminute, her blood pressure is 118/ 80 and her respiratoryrate is28. TheECGtracingshows narrowQRScomplexes and no identifiable P waves.Thisrhythmis most likely: SVTWhich of the followinYou are called to evaluate a 64-yearold woman who complains of palpitations, weakness, and dizziness. Her heart rate is 160 beats per minute, her blood pressureis118/80and her respiratoryrate is 28. The ECG tracing shows narrow QRS complexes and no identifiable P waves. Which of the following drugs is a class I (recommended) drug for thispatient? AdenosineYou are called to evaluate a 64-year-old womanwho complains of palpitations, weakness, and dizziness. Her heartrate is160beatsper minute, her blood pressure is 118/ 80 and her respiratoryrateis28. TheECGtracingshows narrowQRScomplexes and no identifiable P waves. The patient beginsto developchest pain, and her blood pressure drops to 100/60.Thetreatmentof choiceforthispatientis now: Synchronous cardioversion first synchronous cardioversion for patients in PSVT should be at: 50JAtrial flutter is almost always caused by: Rapid reentry You see an irregular rhythmonthemonitor with arateof66to80,a normal PRinterval,and aPwavefor everyQRS. Theratespeeds upand slows down with the patient's respiratory rate. You suspect that this rhythmis: Sinus dysrhythmia You are treating a 70- yearold male patient with atrial fibrillation. The patient'sventricular heart rateis180beats per minute, the blood pressure is 90/60, and the patient complains of chestpain.The hallmark ofatrial fibrillationis: An irregularly irregular rhythm Vagal maneuvers for SVT include: Facial immersion in ice waterYou are treating a 70- yearold male patient with atrial fibrillation. The patient'sventricular heart rateis180beats per minute, the blood pressure is 90/60, and the patient complains of chest pain. You have determined that your atrial fibrillation patient is unstable and requires electrical therapy. You willperform_____ countershockwith _____ joules You are treating a 70- yearold male patient with atrial fibrillation. The patient'sventricular heart rateis180beats per minute, the blood pressure is 90/60, and the patient complains of chest pain. If this patient's atrial fibrillation has been present for more than 48 hours,conversionof this patient's rhythm may lead to: Synchronized; 100 Releaseofemboli Junctional escape rhythms: Occurwhen the SAnode fails tofireWhich of the following may be a lethal treatment for a patient with aventricular escape rhythm? Lidocaine Your patient has a regular bradycardic rhythm witha rateof40, noPwaves,anda QRS greaterthan0.12.Thisis: Ventricular escape rhythm Absolute bradycardia means that: Theheartrateislessthan60beatsperminute The intrinsic rate for a ventricularpacemakeris _____beatsperminute. 20 to40 An ECG strip shows a rhythmwitharateof45, a QRS of 0.08, and a P wavethatappearsafter the QRS. You suspect thatthisdysrhythmiais most likely: JunctionalYou are treating a patient who is complaining that his heart is "skippingbeats." OnECGevaluation,you see frequentPVCsthat are occurringingroups. The patient's blood pressureis 100systolic. Treatment for this patient: Should include oxygen and lidocaine Whichofthefollowing is true of ventricular tachycardia? Patients with pulseless ventricular tachycardia should be treated as though they have: Ventricular tachycardia is triggered by a PVC Ventricular fibrillation The most common arrhythmiainsudden cardiac arrestis: Ventricular fibrillation Synchronized cardioversion is acceptable for patients with ventricular tachycardia: Inallcases The treatment of choice for a symptomatic ventricular escape rhythm is: PacingDefibrillation ofpatients in asystole: Is notrecommendedWhich of the following is an absolute indication for unsynchronized cardioversion? Ventricular fibrillation You are treating a 65- year-old man who is complaining of chest pain and difficulty breathing. On ECG examination,you note thathisventricular heart rateis56,andthereare morePwavesthanQRS complexes. The PR interval is constant when aQRSfollowsaP wave. The QRS complexes are normal and narrow.You suspect this patient has what type ofheart block? Second-degree type II Demand pacemakers fire: Whenthepatient'sratedropsbelowapresetnumberYou are treating a 65- year-old man who is complaining of chest pain and difficulty breathing. On ECG examination,you note thathisventricular heart rateis56,andthereare morePwavesthanQRS complexes. The PR interval is constant when aQRSfollowsaP wave. The QRS complexes are normal andnarrow.This typeof heartblockis typically considered tobe a: You are treating a 65- year-old man who is complaining of chest pain and difficulty breathing. On ECG examination,you note thathisventricular heart rateis56,andthereare morePwavesthanQRS complexes. The PR interval is constant when aQRSfollowsaP wave. The QRS complexes are normal and narrow. The definitive treatment for this patientis: Serious arrhythmia regardless of signs and symptoms Transvenous pacemakerinsertionYou are treating a 65- year-old man who is complaining of chest pain and difficulty breathing. On ECG examination,you note thathisventricular heart rateis56,andthereare morePwavesthanQRS complexes. The PR interval is constant when aQRSfollowsaP wave. The QRS complexes are normal and narrow. Prehospital care for this patient consists of: Transcutaneous pacingYou are treating a 65- year-old man who is complaining of chest pain and difficulty breathing. On ECG examination,younote thathisventricularheart rateis56,andthereare morePwavesthanQRS complexes. The PR interval is constant when a QRS follows a P wave. The QRS complexes are normal andnarrow.Thistypeof block occurs when the impulse isnot conducted through the: AVnodeWhichofthefollowing isa classIintervention for all symptomatic bradycardias? How does atropine affect theventricular rate of third-degree heart block? Transcutaneous pacing Has no effect on the rate Identification of bundle branch blocksis: Helpful in identifying patients at risk for third-degree heart block Third-degree heart block tends to have: Regular but independent atrial and ventricular rhythms You are treating a 65- year-old man who is complaining of chest pain and difficulty breathing. On ECG examination,younote thathisventricularheart rateis56,andthereare morePwavesthanQRS complexes. The PR interval is constant when a QRS follows a P wave. The QRS complexes are normal andnarrow.Thistypeof block isusually associated with: Septal MIWhichofthefollowing is typicallyfoundonan ECG with a bundle- branch block? A notched QRS complex (rabbit ears) You are evaluating an ECG tracing thatshows wide QRS complexes that were produced by supraventricular activity. On MCL1 you see a QS pattern. You suspect: Arightaxisshiftofthe ECG isnotedwhenthe QRS deflectionis: Left bundle-branch block NegativeinleadI,negativeorpositiveinleadII,and positive in leadIII On ECG, pulseless electrical activity looks like: Whichofthefollowing isa correctablecause of PEA? You are treating a patient who is in PEA following home dialysis. Which of the following drugs may be indicated? Any electrical activity otherthan ventricularfibrillation or ventriculartachycardia Tension pneumothorax Sodium bicarbonate Emergency care for a bundle-branch block is: Aimedatthecauseoftheblockifitisidentifiable In a left bundle-branch block: A Q wave is seen instead of an R wave in MCL1Thefirstmedicationa paramedic should administerto a patient with angina is: Oxygen Wolff-Parkinson-White syndrome is of little clinical importance unless the patient: Is tachycardic Atherosclerosis is a disease characterized by: Progressivenarrowingofthelumenofmediumandlarge arteries Most myocardial infarctions arecaused by: Acute thrombotic occlusion Themajorityofacute myocardial infarctions involve the: Left ventricle Prinzmetalangina occurs when: Coronary arteriesspasm The three characteristics of WolffParkinson-White syndrome are a short PR interval,QRS widening, anda(n): Deltawave Wolff-Parkinson-White syndrome is a: Preexcitation syndromeAninferior-wallMIis usually caused by occlusion of the _____ artery. Right coronaryIftheleftventricleloses 25% ofitsmusclemass due to myocardial infarction: The most common cause of death followingmyocardial infarction is: The heart can still pump effectively Fatal dysrhythmia You are transporting a patient to a cardiac center after a suspected myocardial infarction. Thepatient'svitalsigns are stable.ECGshows sinus rhythm with elevatedST segments. The ST segment is elevated because the damaged muscleis: Constantly depolarized Chest painassociated with MI: Isconstant Ischemia caused by unstable angina: Responds well to treatment with antiplatelet agentsYou are transporting a patient to a cardiac center after a suspected myocardial infarction. Thepatient'svitalsigns are stable.ECGshows sinus rhythm with elevated ST segments. Whenyou analyzethe ECG, ST segment elevation is determined when theST segmentis elevated: By more than 1.0 mV in at least two leads You are transporting a patient to a cardiac center after a suspected myocardial infarction. Thepatient'svitalsigns are stable.ECGshows sinus rhythm with elevatedST segments. The patient's ST segment elevation is seeninleadsII,III,and aVF, leading you to suspect: Inferior-wall MIYou are transporting a patient to a cardiac center after a suspected myocardial infarction. Thepatient'svitalsigns are stable.ECGshows sinus rhythm with elevated ST segments. Fibrinolytic therapyfor this patient will be most effective if: You are transporting a patient to a cardiac center after a suspected myocardial infarction. Thepatient'svitalsigns are stable.ECGshows sinus rhythm with elevated ST segments. Fibrinolytic therapyis contraindicated forthis patient if he: A patient in left ventricular failure is expected to have: Thepositionofcomfort for a patient with left ventricular failure is usually: Administered within 12 hours after the onset of symptoms Had laser eye surgery 3 weeks ago Activation of the renin-angiotensin-aldosterone system Sitting with legsdependentSigns ofcardiac tamponade include: Muffledhearttones Treatment forapatient with left ventricular failure includes medicationsto: Reduce afterload Which of the following is most indicative of right ventricularinfarct? Cardiogenic shock is defined by shock symptoms after: Peripheral edema Hypovolemia and dysrhythmias have been corrected Ifapatientwithcardiac tamponade becomes hypotensivein the field, you should: Administer a fluid bolus Which of the following is true of abdominal aortic aneurysm(AAA)? Aneurysms are most commonly the result of: Atherosclerotic disease A drug that may improve the symptoms of cardiogenicshock patientsinthefieldis: Dopamine Right ventricularfailure most often results from: Leftventricular failureAAA may be asymptomatic as long as it is stableWhile assessing a patient, you note a pulsatile mass in the abdomen.Suddenly this mass is no longer palpable, and the patient's blood pressure begins to drop. You suspect that the: Patient's aneurysm hasruptured Patients usually describe thepainofan aortic dissectionas: You are called to the local airporttoevaluate a 40- year-old obese woman who is complaining of pain in her left lower leg. She hasjustcompleteda12- hourflight, and the pain developed as she got off theplane.Herlegis warm, swollen, and painful. You suspect: A compensatory mechanismofthe heart in the presence of chronic hypertensionis to: Ripping or tearing Deep-vein thrombosis Enlarge the muscle mass of the heart Dissections of the aorta are typicallyfound: In the ascending aortaMost new AEDs: Usewaveformsthataremoreeffectiveatlowerenergy settings You are treating a patient with blood pressure of200 over 140. The patient initially complained of headache and nausea. During your 3-hour transport, the patient began to seize and is now unresponsive to any stimulus. You suspect thepatienthas: Hypertensive encephalopathy You are treating a patient with blood pressure of200over 140. The patient initially complained of headache andnausea. During your 3-hour transport,thepatient began to seize and is now unresponsive to anystimulus.mentfor this condition includes: Labetalol The organ(s) most at risk in a hypertensive crisis include the: KidneysSecond and subsequent defibrillations for pediatric patients should occurat: .4J/kg Ifthepaddlepositions are switched (if the apex paddleisapplied to the sternum and the sternum paddletothe apex) during defibrillation: Defibrillation will occur as usual To help reduce impedance toelectrical current: Ifyouseetheoutlineof a smallboximplanted under skin in the left upper abdomen, you would suspect the patienthas a(n): Apply25poundsofpressurewiththepaddlesagainstthe chest wall Implantable cardioverter-defibrillator After deliveringfive Not deliver more shocks until a slower rate is restored for shocks, animplantable 30 seconds cardioverterdefibrillator will: Synchronous cardioversion delivers energy: 10 ms after the peak of the R wave Theinitialpediatric defibrillation should occur at: 2J/kgThesoundheardwhen the AV valves close during ventricular systole is: S1 The left anterior descending coronary artery mainly supplies blood to the: Septum Preloadisdefinedas: Ventricular end-diastolicvolume Pacemakers areusually set toarateof_____ beats per minute beginning with _____ amps. A blood pressure reading inanadultof 180/110 is considered: 70 to 80;50 Stage 3 hypertension The right coronary artery and the left anteriordescending artery supply most of the bloodto the: Right atrium andventricle The circumflex branch of the left coronary artery mainlysupplies blood to the: Leftatrium When performing CPR on an adult, you would compressthechesttoa depth of inches. 11/2to2Each squareon ECG paper is __ mm in height and width. 1 An elevated STsegment suggests: Injury A depressedST segment suggests: Ischemia Twave inversion suggests: Ischemia The group of nerves that innervatestheatria and ventricles is known as the: The major neurotransmitterforthe parasympathetic system is: Cardiac plexus Acetylcholine Parasympathetic stimulationoftheheart causes: A decreased heart rate _____ seconds is/are measured in each large box on ECGgraph paper? 0.20 Norepinephrine's major effect is: VasoconstrictionAfter you administer nitroglycerine 0.4mg SL toa patientwithchest pain who has ST- segment elevation in leadsII,IIIandAVF,his blood pressure drops to 78/50 mmHg. You anticipated this side effect in this patient because his ECG changes indicate damage tothe: NormalSinus Rhythm Inferior wall which increases the dependence on preload Heart Rate: 60-100 bpm Regularity: Regular PRI: .12-.20 seconds QRS: <.12 seconds Which of the following homemedicineswould indicate that your patient has a strong risk factor forheart disease? MetforminNormal Sinus Heart Rate: <60 bpm Bradycardia Regularity: Regular PRI: .12-.20 seconds QRS: <.12 seconds Normal Sinus Heart Rate: >100 bpm Tachycardia Regularity: Regular PRI: .12-.20 seconds QRS: <.12 seconds Normal Sinus Heart Rate: 60-100 bpm; can be <60 Arrhythmia Regularity: Irregular PRI: .12-.20 seconds QRS: <.12 secondsPremature Atrial Contraction (PAC) Heart Rate: Depends on underlying rhythm Regularity: Interrupts the regularity of underlying rhythm P-Wave: can be flattened, notched, or unusual. May be hidden within the T wave PRI: measures between .12-.20 seconds and can be prolonged; can be differentfromothercomplexes QRS: <.12 seconds AtrialTachycardia(SVT) Regularity: R-R intervals are constant; Regular Rate: artial/ventricular rates are equal; heart rate is between 150- 250bpm. P-Wave: One P Wave in front of every QRS; may be flattened ornotched;becauseoftherapidrate,theP waves can be hidden within the T waves PRI: .12-.20 seconds and constant QRS: <.12 secondsAtrial Flutter Rhythm: Regular atrial rhythm; irregular ventricularrate Rate: 250- 350 bpm P-Wave: well defined P waves; "sawtooth" appearance PRI: Usually impossible to determine the PR in this arrhythmia. QRS: <.12 seconds Atrial Fibrillation (Uncontrolled) Regularity: Irregular; no pattern to it's irregularity Rate: Majority of time is >350 bpm P Waves: No P Waves Present PRI: Since no P Waves, no PRI can be determined QRS: Should be <.12 seconds Atrial Fibrillation Regularity: Irregular; no pattern to it's irregularity (controlled) Rate: <100 bpm P-Wave: Not present PRI: Since no P wave is present, PRI is not determinedQRS: <.12 secondsJunctional Rhythms -Occurs when the AV node takes over as the primary pacemakerintheheartratherthantheSAnode.AVnode takes over when is moves faster than SA node. Rate: 40-60 bpm; Accelerated Junctional: 60-100 bpm; Junctional Tachycardia: 100 bpm or greater P Wave: If before QRS, P wave will be inverted. P Wave can alsobe hiddenwithintheQRScomplex.PWaveisusually <.12 seconds QRS: <.12 seconds What are the four Supra-Ventricular Tachycardias(SVT)? FirstDegreeHeart Block Sinus Tachycardia (100-160 bpm) Atrial Tachycardia (150-250 bpm) Atrial Flutter (150-250 bpm) Junctional Tachycardia (100-180bpm) Regularity: depend on the rhythm Rate: Depend on underlying rhythm PWaves:UprightandUniform;eachPWave willbe followed by a QRS complex PRI: constant across entire strip, but always > .20 seconds. QRS: < .12 secondsSecondDegreeHeart Block(Wenckebach) Regularity: R-R Wave is irregular; R-R interval gets progressively shorterasPRIgetsprogressivelylonger Rate: Ventricular rate is slightly slower than normal; atrial rate isnormal P-Waves: upright and uniform; some pwavesarenot followed by the QRS complex PRI: gets progressively longer until one p wave is not followedbya QRScomplex;aftertheblockedbeat,cycle starts over QRS: < .12 seconds SecondDegreeHeart Block (Morbitz) Regularity: if conduction ratio is consistent, R-R interval will be constant and rhythm, regular. If conduction ratio varies, the R-R will be irregular Rate: atrial rate is usually normal; ventricular rate will be in bradycardia P Waves: upright and uniform; always be more P waves than QRS PRI: constant; might be longer than normal QRS: <.12 secondsPremature Ventricular Contraction (PVC) Regularity: Regular or Irregular Rate: Determined by underlying rhythm; but frequently do not produce apulse P-Waves:EctopicisnotprecededbyaP-Wave PRI: None QRS: Wide and Bizarre; measuring at least .12 seconds; T waveis often inopposite direction fromQRS. Ventricular Tachycardia Regularity: Usually regular Rate: Ventricular Rate: 150-250 bpm; if rate is <150 bpm, it's aslowVT;if exceeds250bpm,VentricularFlutter PWaves:NoneofQRSwillbeprecededbyPWaves PRI: no PRI QRS: wide and bizarre measuring at least .12 seconds; hard to tell between QRS and Twave VentricularFibrillation Regularity: chaotic Rate: cannot be determined P Waves: noPwavespresent PRI: no PRI QRS: no discernible QRS complexes3rdDegreeHeartBlock Regularity: Regular Rate: 40-60 bpm if junctional; 20-40 bpm if focus is ventricular. P Wave: upright and uniform; more p waves than QRS complexes PRI: no relationship between p waves and QRS complexes QRS: < .12 seconds if junctional; > .12 seconds if ventricular Bundle Branch Block (Left) Wide QRS (>.12 seconds) Left BundleBranch("M") Can deteriorate to a 3rd Degree HB Bundle Branch Block (Right) Asystole No electrical activity; only a straight lineWide QRS (>.12 seconds) Right Bundle Branch Block ("V") Can deteriorate to a 3rd Degree HBLead Placement Left: Smoke (Black) over Fire (Red) Right: Snow (White) over Grass (Green) Center: Chocolate (place a little off center for possible CPR) Sinus Tachycardia Etiology: Etiology/Clinical Signs -Physiologic demand foroxygen -Sympathomimetric Drugs -Fever -Pain Clinical Signs: -increased HR; increased oxygen demand SinusTachycardia Treatment Sinus Bradycardia Etiology/Clinical Signs SinusBradycardia Treatment -May resolve with treatment of underlying cause -Digoxin, Beta Blockers (-olol), Verapamil -Vagal Maneuver Etiology: -response to myocardial ischemia -vagal stimulation -electrolyte imbalance -drugs -increased intracranial pressure -highlytrainedathlete ClinicalSigns: -decreasedCOifbodycan'tcompensate;improved CO due to diastolic filling time -Atropine -Avoid Valsalva -Hold Rate Slowing Drugs (Digoxin, Beta Blockers)Sinus Bradycardia: 1. Airway Example: Your pt is 2. Oxygen pale, c/o dizziness and 3. ECG, BP, Oximetry fatigue; pulse 56, BP 4. IVAccess 86/60. How wouldyou 5. If s/s of perfusion, altered mental status, CP, follow protocol hypotension, signs of shock: according to ACLS? a. prepare for transcutaneous placing b. atropine 0.5mg IV while waiting for pacer (may repeat for total of 3mg IV) c. epi or dopamine drip while waiting pacer Atrial FlutterEtiology/ Etiology: Clinical Signs -occurs w/ heartdisease -CAD -Valve Disorders Clinical Signs: -may cause thrombus -"saw tooth" -250-400 bpm AtrialFlutterTreatment -Give anticoagulants (fastertheHR, moreriskfor thrombus) -treat underlying cause -digoxin (slows rate by enhancing AV block) -Quinidine (supresses atrial ectopic block) -Amiodarone -Calcium Channel Blockers (Cardizem)/Beta Blockers (- olol) -consider cardioversionAtrial Fibrillation Etiology: Etiology/Causes -Advanced Age -Valve Disorders -cardiomyopathy Causes: -chocolate (theobromine-stimulant) -sleep apnea -athletes -tall athletes -aging heart -men more thanwomen Atrial Fibrillation Treatment Amiodarone 1. Amiodarone 2. Calcium Channel Blockers, Beta Blockers, digoxin 3. Synchronized cardioversion ifunstable 4. radio frequency catheter ablation 5. anti-coagulation therapy 6. Cardizem Maycauseliver,lungdamage,andworseningof arrhythmias.PttoreportSOB,wheezing,jaundice, palpitations, lightheadedness Electrical Cardioversion Tx of choice if pt has a hemodynamically unstable tachydysrhythmia;unstableventriculartachycardiaw/a pulse; prevention of life-threatening dysrhythmias; cardioversion can be planned or emergent; proper cardioversion willcorrect Rhythmsfor cardioversion 1. A-Fib 2. A-Flutter 3. SVTpt dysrhythm iaw/ minimal discomfort and maximum safetyParoxysmal SVT Treatment 1. treat underlyingcause 2. adenosine, beta blockers, digoxin, quinidine, MS 3. Carotid/Vagal Maeuver 4. Synchronized cardioversion ifunstable Premature Ventricular 1. Hypoxia Contraction Etiology 2. Digoxin Toxicity 3. Mechanical Stimulation 4. Electrolyte Imbalance (potassium) 5. MI Premature Ventricular Contraction Clinical Signs 1. Depends onfrequency 2. short diastolic filling time, decreased cardiac output 3. sensation of palpitations, skipped beats 4. Bigeminy (pvc every other beat) 5. Trigeminy (pvc every 3rd beat) Premature Ventricular 1. treat impaired hemodynamics Contraction Treatment 2. antiarrythmics 3. oxygen 4. monitor for PVC on T-Wave PostCardioversionCare SameaswhenaptisinA-Fib Ifelective,digoxinisusuallywithheldfor48hrspriorto cardioversion to prevent dysrhythmias after procedure airway patency should be maintained and the patient state of consciousness should be evaluatedVentricular Arrythmias Etiology Same as PVC but also cardiomyopathy, myocardial irritability VentricularArrythmias Treatment 1. VT w/ a pulse: cardiovert 2. monitor moreclosely 3. prepare cardioversion (oxygen, lidocaine, treat cause) 4. VT w/o a pulse: defibrillate (call code)CardiacArrest VentricularAsystoleduetoVFib Etiology: trauma, overdose, MI Clinical Signs: asystole or VFib, no definable waves, Ventricular Asystole absence of VS TEA: trans-cutaneous pacemaker, epinephrine, atropine Ventricular Fib (Etiology, ClinicalSigns) 1. Same as VT,PVC 2. Surgical Manipulation of heart 3. Failed cardioversion 1. Same as cardiacarrest 2. EKG is disorganizedrhythm Ventricular Fib 1. IMMEDIATE DEFIBRILLATION X3 Treatment 2. CPR 3. SURVIVAL IS <10% FOR EVERY MINUTE THE PT REMAINS IN V-FIB SCREAM (acronym)for 1. Shock Q2min VFib and VTach 2. CPR after shock (compressions followed by resp 30:2) for 2min 3. Rhythm check after 2 min of CPR and shock again if indicated 4. Epinephrine or vasopressin 5. Antiarrythmic medications: Amiodarone/Lidocaine 6. Magnesium Sulfate Torsades De Pointes Treatment IVMagnesium1st Degree Heart Block Treatment Monitor; Observe for symptoms 2ndDegreeHeart Block Causes organic heart disease, MI, Dig Toxicity, Beta and Calcium Blockers 2ndDegreeHeart BlockTreatment Monitor HR, Atropine, Temp Pacemaker, Avoid meds that decrease conductivity 3rd Degree Heart Block Causes Organic Heart Disease, MI, Drugs, Electrolyte Imbalance, Excess Vagal Tone 3rd Degree Heart Block Signs & Symptoms Extreme Dizziness, Hypotension, Syncope, Decrease CO, Altered Mental Status 3rd Degree Heart Block Treatment Pacemaker (temporary or permanent) Loop diuretics: excessive diuresis, monitor for dehydration, output less furosemide, ethacrynic than 30ml/hr, hypotension, ototoxcity (irreversible w/ acid, bumetande, ethacrynicacid),hypokalemia,avoid inpregnancy, digoxin torsemide canincreasetoxicity, monitorBP, lithium,NSAIDsdecrease effect thiazide diuretics: assess for dehydration, report less that 30ml/hr, decrease hydrochlorothiazide, inK,increaseinglucose,avoidinpregnancyandlactation, chlorothiazide, no risk of hearing loss- alternate day can increase methyclothiazide, electrolyte imbalance thiazide-type diuretics, 1stDegreeHeartBlock Causes May be normal variant; inferior wall MI; drugs: verapamil or digoxinindapamide, chlorthalidone, metolazone- moderate diureticK-sparing diuretics: hyperkalemia, endocrine effects (impotence and irregular spironolactone, menstrual), no w/ kidney failure triamterene, amiloride, may take 12-48hr to work- less strong osmotic diuretics: mannitol ACE inhibitors: captopril (1hr before meal), enalapril, enalaprilat (only one for IV), fosinopril, lisinopril, ramipril, moexipril (1hr before meal): vasodilate, excrete water andsodium acute phase kidneyinjury,cerebraledema, preventkidney failurein shock,monitorforheartfailure,kidneyfailure, lithium excretion is increased usedin:heartfailure,HTN, MI,nephropathy.stopdiuretic 2-3days beforeACE,drycough,hyperkalmeia,rashand altertaste-report, angiodema, neutropenia,canincrease lithium levels, avoid use of NSAIDs ARBs: losartan, uses: HTN, prevent mortality following MI, stroke, valsartan, irbesartan, angiodema, fetal injury, given PO candesartan, olmesartan: dilate and excrete aldosterone hyperkalemia, hyponatremia, flulike manifestations-report, antagonists: dizziness, can cause lithium toxicity eplerenone, spironolactone: used w/ HTN, Heart failure Directrenininhibitors: aliskiren, HTN angiodema, hyperkalemia, diarrhea- dose related, decreases levels of furosemide, atorvastatin can increase levels,monitorforhypotensi on,avoidhighfatmealsmeds used forHTN nifedipine,verapamil, diltiazem, amlodipine, felodipine, nicardipine medsusedforcardiac dysrhythmias verapamil, diltiazem Nifedipein increased HR- can give beta blockerto fix, observe for swelling(cangivediuretic),acutetoxicity-monitorVS, admin.norepi, calcium,isoproterenol,lidocaine,ivfluids, gastric lavarge- slowling HR w/beta blockers, no grapefruit juice calcium channel blockers: nifedipine,verapamil, diltiazem, amlodipine, felodipine,nicardipine works on arteries, veins not affected verapamil, diltiazem OH and peripheral edema, constipation, cardiac suppression, dysrhtymias,acutetoxicity,increasedigoxin, don't use w/ beta blockers, avoid grapefruit juice alpha adrenergic start with low dose, first dose given at night, change blockers: prazosin, positions slowly, use carefully w/ antihypertensives. take doxazosin mesylate, med w/ food. terazosin: HTN, BPH centrally actingalpha drowsiness, dry mouth, rebound hypertension so taper. agonists: clonidine, dont use patch w/ scleroderma and lupus, use cautiously guanfacine HCL, w/ stroke, MI, DM, depression, renal failure. careful w/ medsusedforangina nefedipine, amlodipine, nicardipine, verapamil, diltiazemmethyldopa: migrain, prazosin and TCAs, ADHD, HTN, withdrawal, severe cancer painadrenergicagonists: epinephrine,dopamine,dobutamine,isoproterenol, terbutaline BetaBlockers: metoprolol and propranolol metoprolol, atenolol, metoprolol succinate, esmolo, propranolol, nadolol, carvedilol, labetalol: HTN, agnina, migrain, glaucoma bradycardia,cautiouslyindiabetes,decreasedcardiac outputmonitorandnotify,AVclock-baselineECG,OH, rebound myocardium excitation: taper off meds: monitor clients taking beta blockerconcurrently hypertensive crisis: nitroprusside, nitroglycerin, nicardipine, clevidipine, enalaprilat, esmolol HCl excessive hypotension, cyanide poisoning- increased for liver issues,reducebygivinglessthan5mcg/kg/minor thiosulfate, avoid prolonged use, protect from light, discard after24 hr cardiac glycosides: dysrhythmias, consume high Kfoods, .5-2 serum levels of digoxin: treatmentof digoxin, avoid use of quinidine, verapamil, thiazide, ACE heart failure and can increase digoxin levels, antacids decrease dysrhythmias Epinephrine: alpha 1, beta1 and2 dopamine: shock and heart failure vacoconstrict, increase HR, heart contraction, rate of conduction,bronchodilationhelpsw/slowsabsorptionof local anesthetics, manages superficial bleeding, decreased congestion of nasal mucosa, increased BP, treatment of AV block and cardiac arrest, asthma low dose: renal blood dilation moderate: beta 1: renal dilation, increase HR, myocardial contractility, increased rate of conduction propranolol avoidw/asthma,diabetes-monitorbloodglucoseb/cit masks signs of hypoglycemiahigh: all above and vasoconstriction dobutamine: beta 1 increased HR, myocardial contraction, rate of conduction: used w/ heartfailureInteractions of adrenergic agonists MAOIs with epi, TCAs with epi, general anesthetics w/epi, alphaand betaadrengergicblockersanddiureticsblock dopamine organic nitrates: use aspirin or acetaminophen to relive pain, OH, reflex nitroglycerin, nitro-time tachy, tolerance, can increase cranial pressure, avoid (capsules), nitrostat alcohol, careful w/ beta blocker, calcium channel, diuretic, (subling tablet), NO with viagraetc. nitorlingual (spray), nitro-bid (topical), nitrodur (transderm), nitrobid Iv, isosorbide dinitrate, isosorbide mononitrate- treat angina sublingual tabletand translingualspray sustainedrelease transdermal dobutamine adverse increased HR dopamine adverse dysrhythmias, necrosis epinephrine complications: hypertension, dysrhythmias,rapid onset, short duration treat acute attack, and prophylaxis of acute use at first sign, prior to activ ity known to cause pain, stored in cool, dark place slow onset, longduration long term prophylaxis against anginal attacks swalloww/o crushingorchewing-emptystomachw/ water slow onset, longduration long-term prophylaxis against attacks patches shouldn't be cut, rotate, no hair, remove w/soap and water, remove at nighttopical ointment slowonset,longduration long term phrophylaxis removepriordosebeforeapplyingnewdose,clean hairless area, coverw/saran, avoidtouching ointment, antianginal agent: ranolazine; lower cardiacO2demand monitorECGforQTprolonging,elevatedBP,avoiduse grapefruitjuice,HIVprotease,macrolideantibiotics, verapamil,quinidine,digoxin,simvastatin Class 1A-- decrease electrical conduction, automaticity, Procainamide, quinidine repolarization rate: used w/ supraventricular tachycardia, gluconate, quinidien ventricular tachycardia, atrial flutter, atrial fibrilation: sulfast, disopyramide Class 1B-- LIdocaine: mexiletine, tocainide decrease electrical conduction, automaticity, repolarization rate: short term use only for ventricular dysrhythmias HMG COA Reductase inhibitors:thestatins cholesterol absorption inhibitor: ezetimibedecreases LDL decrease LDL,increase HDL, hepatotoxic, myopathy, monitor CK, no grapefruit juice, erythromycin, ketoconazole, ezetimibe,gemfibrozil,fenofibrate hepatitis,myopathy,don'ttakew/bileacid,,fibratesif takenw/ statinmonitorformoreliverissues bile-acid sequestrants: increase fiber intake, oral fluids, take other meds 4hr Class 1C: propafenone, flecainide decrease electrical conduction, decrease excitability, increase rate or repolarlization: SVT IV usedforanginathatdoesn't respondtoothermeds, contorl BP or induce hypotension suring surgery, heart failure from acuteMI use glass IV bottle, start slow and titrate up,colesevelam HCL, before admin colestipol- decrease LDLdigoxin Decrease electrical conduction through AV node,Increase myocardial contraction used w/ H, atrial fibrillation and flutter, paroxysmalSVT Nicotinic acid, niacin: lowerLDL,raiseHDL fibrates: gemfibrozil, fenofibrate: increase HDL GIdistress-takew/food,facialflushing-takeaspirin30 minutes beforeeachdose, hyperglycemia, hepatotoxicity, hyperuricemia, GIdistress,gallstones,myopathy,heaptotoxicity,increases risk of bleeding w/ warfarin, use w/ statins increase myopathy class II medications: decreases HR, slow rate of conduction, decrease atrial propanolol ectopic stimulation: used w/ Atrial fibrillation, atrial flutter, hydrochloride, esmolol paroxysmal SVT, hypertension, angina hydrochloride, acebutolol hydrochloride class III meds: Amiodarone, Dofetilide, Ibutilide, Sotalol class IV meds: verapamil, diltiazem Decrease rate ofrepolarization, Decrease electrical conduction, Decreasecontractility, Decrease automaticity: used w/ Conversion of atrial fibrillation-oralroute, Recurrentventricularfibrillation, Recurrent ventricular tachycardia Decreaseforceofcontraction,Decreaseheartrate,Slow rateof conductionthroughtheSAandAVnodes:Atrial fibrillation and flutter, SVT,Hypertension, Angina pectoris procainamide: complications lupus- resolves w/disconinuation, controlsystems w/ NSAIDs, neutropenia and thrombocytopenia, cardiotoxicity, adenosine Decreaseelectricalconduction through AVnodeusedw/ Paroxysmal SVT, Wolff-Parkinson-White syndromeh y p o t e n s ion, pregnancy risk, contraindicated w/ hypersensitivity to procaine and quinidine, myastheniagravis,lidocaine complications Propafenone: complications Propranolol: complications amiodarone: complications verapamil: complications adenosine: complications Digoxin: complications CNS effects, give phenytoin to control seizures, respiratory arrest: contraindicated in stokes-adams, wolf-parkinson syndrome, severe heart block, liverand renal dysfunction, sinus bradycardiaand heart failure bradycardia,heartfailure,dizziness,weakness,monitorHR, chestpain edema.contraindicatedinclientsw/AVblock, severeheartfailure, severehypotension,andcardiogenic shock, use cautiously w/ heart, liver, kidney, failure. respiratoryorders, older clients hypotension, bradycardia, heart failure, fatigue, contraindicatedinAVclock,heartfailure,bradycardia, diabetes, liver,thyroid,respiratory,Wolff-parkinsonwhite pulmonarytoxicity,sinusbradycardiaandAVblock, monitor BP,HF,visualdisturbances,liverand thyroid dysfunction, phlebitiswithIVadmin,hypotension, bradycardia, contraindicated in patients w/ AVblock, pregnancy risk: av block, bradycardia, newborns and infants, HF,fluidand electrolyteimbalance bradycardia,hypotension,HF,constipation,pregnancyrisk, contraindicated in patients w/ IV form not used w/ tachycardia, sinusbradycardia,hypotension,dyspnea,flushingofface, monitor ECG- effectslast 1min orless. contraindicated in second and third degree heart block, AV block, atrial flutter, atrialfibrillation bradycardia, hypotension (therapeutic level: .5-.8) nausea, vomiting, dyrhythmias, hypokalemia, contraindicated:tachycardia,fibrillation, notuseAV block,bradycardia, renal disease, hypothyroidism, cardiomyopathyProcainamide: interactions lidocaine interactions propafenone interactions propranolol interactions amiodarone interactions Verapamilinteractions Adenosineinteractions digoxin interactions avoid antidysrhythmics, anticholinergic meds, antihypertneives, advisetotakeasprescribed, advisenot tocrush orchewsustained releasepreparations cimetidine, beta blockers, phenytoin, monitor client for CNS depression, IV admin is usually started w/loading dose, used for no more than 24hr mayslowmetabolismandcauseanincreaseinthelevels of digoxin, anticoagulants, and propranolol; quinidine and amiodarone increasetoxicity,monitorECG,bradycardia hypotension verapamil, dilitiazem have additive cardiosuprression effects, carefulw/diabetic patients; instruct clients to take apical pulse and notify providerof changes increase plasma levels, cholestyramine decreases levels of amiodarone,usecautiouslyw/diuretics,betablockers, verapamil, no grapefruit juice. may increase digoxinn toxicity- highlytoxic -lolmayincrease med, may potentiate carbamazapine and digoxin, maycauseheartfailure;maycauseOH-report edema orSOB methyxanthines block receptors, dipridamole uptake in inhibited,shorthalflife-soadversearemildandlastfor less than oneminute. antacids and metoclopramide decrease digoxin, amiodarone, quinidine,verapamil,diltiazem,propafenone, flecainide increase digoxin levers, cortico, diuretics, thiazides, amphotericin B may decrease Klevels-monitor HR- report isless than 60, eathigh K diet Endometiralinfection usually occurs with a prolonged rupture of membranes, not vacuumassisted births.Cervical lacerations are common complications from When a client is experiencing a wound evisceration... vacuum-assisted birth arerare butcan include perineal, vaginal, or cervicallacerations thenurseshouldinitiallystaywiththeclientandcallfor help. Next, the nurse should place saline-soaked gauze on theexposedbowelsto keeptheinternalorgansmoist.The nurseshouldthenplacetheclient inasupinepositionwith hishipsandkneesbenttorelievepressure fromtheopen wound.Last,thenurseshouldtaketheclient'svitalsigns to assess forchanges in hemodynamics. continuous passive motion (CPM)machine Turn oftheCPMmachineduringmealstopromote comfort and dietary intake. -The affected extremity should maintain neutral alignment. Correct method for walking upstairs with crutches 1. Holdtorailwithonehandandcrutcheswiththeother hand. 2. Pushdownonthestairrailandthecrutchesandstepup with the "unaffected"leg. 3. Ifnotallowedtoplaceweightonthe"affected"leg,hop up with the "unaffected" leg. 4. Bringthe"affected"legandthecrutchesupbesidethe "unaffected" leg. 5. Remember, the "unaffected" leg goes up first and the crutches Heparin is an anticoagulant that inhibits the conversation of prothrombintothrombin.Patientsonananticoagulant drugsuchasheparinareatanincreasedriskofbleeding. -Signs of bleeding: ecchymoses, tarry stools, mucosal bleeding, and pink/ red-tinged urine. Valproic acid can cause hepatic toxicity Intenstinal gas is a commonsideeffectof clientsfollowingacesareanbirthmove with the "affect ed" leg.Droplet precautions DROPLET: "SPIDERMAn" -Sepsis -Scarlet Fever -Strep -Pertussis -Pneumonia -Parvovirus -Influenza -Diphtheria -Epiglottitis -Rubella -Mumps -Adenovirus Management: Private room/mask -Aprivateroomaromwithotherclientswiththesame infectious disease. -Masks for providers and visitorsAirborne precautions: AIRBORNE: "My Chicken Hez TB" -Measles -Chicken pox -Herpes zoster -TB Management: neg. pressure room, private room, mask, n- 95 for TB. -A private room -Masksorrespiratoryprotectiondevicesforcaregivers and visitors. -An N95 or high-efficiency particulate air (HEPA) respirator is used if the client is known orsuspected to have TB. -Negative pressure airflow exchange in the room of at least six exchanges per hour.StageIpressure ulcer Stage II pressure ulcer Intact skin with an area of persistent, nonblanchable redness, typicallyoverabonyprominence,thatmayfeel warmerorcooler thantheadjacenttissue.Thetissueis swollenandhascongestion, withpossiblediscomfortat thesite.Withdarkerskin tones,theulcer may appearblue or purple. Partial-thickness skin loss involving the epidermis and the dermis. Theulcerisvisibleandsuperficialandmayappear asanabrasion, blister,orshallowcrater.Edemapersists, andtheulcermaybecome infected,possiblywithpainand scant drainage. Contact precautions CONTACT: "MRS WEE" -MRSA -RSV -Skininfections(herpes zoster,cutaneousdiphtheria, impetigo, pediculosis, scabies, and staph) -Wound infections -Enteric infections (C-Diff) -Eye infections(conjunctivitis) Management: gown, gloves, goggles, private room VRSA - contact and airborne precautions (private room, door closed, negative pressure) -Aprivateroomoraroomwithotherclientswiththesame infection. -Glovesand gownsworn bythecaregiversand visitors.StageIIIpressureulcer Stage IV pressure ulcer Full-thicknesstissuelosswithdamagetoornecrosisof subcutaneoustissue.Theulcermayextenddownto,but notthrough, underlyingfascia.Theulcerappearsasa deep craterwith orwithout undermining of adjacent tissue and without exposed muscle or bone. Drainage and infection arecommon. Full-thickness tissue loss with destruction, tissue necrosis, or damage tomuscle, bone, orsupportingstructures. There may be sinus tracts, deep pockets of infection, tunneling, undermining, eschar (black scab-like material), or slough (tan, yellow, or green scab-like material)GlasgowComaScore is calculated by using appropriate stimuli (a painful stimulus may be necessary)and then assessing theclientsresponse in threeareas. Eye opening (E) - The best eye response, with responses ranging from 4 to 1 4 = Eye opening occurs spontaneously. 3= Eyeopeningoccurssecondarytovoice. 2= Eye openingoccurssecondarytopain. 1 = Eye opening does not occur. Verbal (V) - The best verbal response, with responses ranging from 5 to 1 5= Conversationis coherent and oriented. 4 =Conversationisincoherent anddisoriented. 3 = Words are spoken, but inappropriately. 2= Sounds aremade, butno words. 1 = Vocalization does not occur. Motor (M) - The best motor response, with responses ranging from 6 to 1 6 = Commands arefollowed. 5 = Local reaction to pain occurs. 4 = There is a general withdrawal to pain. 3 = Decorticate posture (adduction of arms, flexion of elbows and wrists) is present. 2 = Decerebrate posture (abduction of arms, extension of elbows and wrists) ispresent. 1 = Motor response does not occur. Responses within each subscale are added, with the total score quantitatively describing the client's level of consciousness. E + V+ M = TotalGCSWhen verifying NG A good indication of appropriate placement is obtaining tube placement, the pH gastric contents with a pH between 0 and 4. of aspirated gastric fluid should Sodium 136-145 Potassium 3.5-5 Total Calcium 9.0-10.5 Magnesium 1.3-2.1 Phosphorus 3.0-4.5 BUN 10-20 Creatinine males 0.6-1.2 Creatinine females 0.5-1.1 Glucose 70-105 HcbA1c <6.5% WBC 5,000-10000 RBC men 4.7-6.1 million/mm3 RBC women 4.2-5.4 millin/mm3 Hemoglobin men 14-18 Hemoglobin women 12-16 Hematocrit men 42-52 Hematocrit women 37-47 Platelet 150,000-400,000 pH 7.35-7.45 pC02 35-45p02 80-100Normal INR= 0.7-1.8 (Therapeutic INR 2-3) Normal PTT= 30-40 seconds (Therapeutic PTT 1.5-2 x normal or control values) Digoxin 0.5-2.0 Lithium 0.8-1.4 Dilantin 10-20 Theophylline 10-20 LatexAllergies Notethatclientsallergic tobananas,apricots,cherries, grapes, kiwis, passion fruit, avocados, chestnuts, tomatoes, and/or peaches may experience latex allergies as well. H NCor0m3al PT= 2 111--1226.5 secondsCane Walking C-cane O-opposite A-affected L-leg Order of Assessment I-inspection P-palpation P-percussion A-auscultation Except with abdomen it is IAPP-inspect, auscultate, percuss and palpate.Arterial occlusion: 4 P's Pain Pulselessness or absent pulse Pallor Paresthesia Crutch walking Rememberthephase"stepup"whenpicturingaperson goingup stairswithcrutches.Thegoodleggoesupfirst followedbythe crutchesandthebadleg.Theopposite happensgoingdownthe stairs....OR"uptoheaven...down to hell" Angina Precipitating Exertion: physical activity and exercise Factors: 4 E's Eating Emotional distress Extreme temperatures: hot or cold weather Delegation RNsDONOTdelegatewhattheycanEAT--evaluate, assess, teachHeart Sounds:All PeopleEnjoythe Movies Aortic: 2nd right intercostal space Pulmonic: 2nd left intercostal space Erb's Point: 3rd left intercostal space Tricuspid: 4th left intercostal space Mitral or Apex: 5th left intercostal space Congestive Heart Failure Treatment: MADD DOG Morphine Aminophylline Digoxin Dopamine Diuretics Oxygen Gasses: Monitor arterial blood gasses Heart Murmur Causes: SPASM Stenosis of avalve Partial obstruction Aneurysms Septal defect Mitral regurgitationHypertension Care: DIURETIC Daily weight Intake and Output Urine output Response of bloodpressure Electrolytes Take pulse Ischemic episodes or TIAs Complications: CVA, CAD, CHR, CRF Shortness ofBreath (SOB) Causes: 4 As+4Ps Airway obstruction Angina Anxiety Asthma Pneumonia Pneumothorax Pulmonary Edema Pulmonary EmbolusCompartment Syndrome Signs and Symptoms: 5 P's Pain Pallor Pulse declined orabsent Pressure increased Paresthesia Shock Signs and Symptoms: CHORD ITEM Cold, clammy skin Hypotension Oliguria Rapid, shallow breathing Drowsiness, confusion Irritability Tachycardia Elevated or reduced central venous pressure StrokeSigns:FAST Face Arms Speech TimeMulti-organ damageHypoglycemia Signs: TIRED Tachycardia Irritability Restlessness Excessive hunger Depression and diaphoresis Hypocalcaemia Signs Convulsions and Symptoms:CATS Arrhythmias Tetany Stridor and spasms Hypokalemia Signs and Symptoms: 6L's Lethargy Leg cramps Limp muscles Low, shallow respirations Lethal cardiac dysrhythmias Lots of urine(polyuria)Traction Patient Care: TRACTION Temperature of extremity is assessed for signs of infection Ropeshangfreely Alignmentofbodyandinjuredarea Circulation check (5 P's) Typeandlocationoffracture Increasefluidintake Overhead trapeze No weights on bed or floor Hypertension Complications: The 4 C's Coronary artery disease (CAD) Congestive heart failure (CHF) Chronic renal failure (CRF) Cardiovascular accident (CVA): Brain attack or strokeLeukemiaSignsand Symptoms: ANT Anemia and decreased hemoglobin Neutropenia and increased risk of infection Thrombocytopenia and increased risk of bleeding Clients Who Require Dialysis: AEIOU (The Vowels) Acid base imbalance Electrolyte imbalances Intoxication Overload of fluids Uremic symptoms Cancer Early Warning Signs:CAUTION UP Change in bowel or bladder Alesionthatdoes notheal Unusual bleeding ordischarge Thickeningorlumpinbreastorelsewhere Indigestion ordifficulty swallowing Obviouschangesinwartormole Nagging cough or persistent hoarseness Unexplained weight loss Pernicious AnemiaAsthma Management: ASTHMA Adrenergics: Albuterol and other bronchodilators Steroids Theophylline Hydration: intravenous fluids Mask: oxygen therapy Antibiotics (for associated respiratory infections) Hypoxia: RAT (signs of early) BED (signs of late) Restlessness Anxiety Tachycardia and tachypnea Bradycardia Extreme restlessness DyspneaPneumothorax Signs: PTHORAX Pleuretic pain Trachea deviation Hyperresonance Onset sudden Reduced breath sounds (& dyspnea) Absent fremitus X-ray shows collapsedlung Transient incontinence Causes: DIAPERS Delirium Infection Atrophic urethra Pharmaceuticals and psychological Excess urine output Restricted mobility Stool impactionDealing with Constipation Constipation is difficult or infrequent passage of stools, which may be hard and dry. Causes include: irregular bowel habits, psychogenic factors, inactivity, chronic laxative use or abuse, obstruction, medications, and inadequate consumption of fiber and fluid. Encouraging exerciseand adiethighinfiberand promoting adequate fluid intake may help alleviate symptoms.Dealing with Dysphagia: Dysphagiaisan alterationin the client's ability to swallow. Causes include: Obstruction Inflammation Edema Certain neurological disorders Modifyingthetextureoffoodsandtheconsistencyof liquids may enable the client to achieve proper nutrition. Clients with dysphagia are at an increased risk of aspiration. Place the client in an upright orhigh-Fowler's position to facilitate swallowing. Provideoralcarepriortoeatingtoenhancetheclient's sense of taste. Allow adequate time for eating, utilize adaptive eating devices, and encourage small bites and thorough chewing. Avoid thin liquids and sticky foods.Dumping Syndrome Gastroesophageal Reflux Disease (GERD) DumpingSyndromeoccursasacomplicationofgastric surgeries that inhibit the ability of the pyloric sphincter to controlthe movementoffoodintothesmallintestine. This "dumping" results in nausea, distention, cramping pains, and diarrhea within 15 min aftereating. Weakness,dizziness,arapidheartbeat,and hypoglycemia may occur. Small, frequent meals are indicated. Consumptionofproteinandfatateachmealisindicated. Avoid concentrated sugars. Restrict lactose intake. Consumeliquids1hrbeforeoraftereatinginsteadofwith meals (a drydiet) GERD leads to indigestion and heartburn from the backflow ofacidicgastricjuicesontothemucosaofthe loweresophagus. Encourage weight loss for overweight clients. Avoid largemealsandbedtimesnacks. Avoidtriggerfoodssuchascitrusfruitsandjuices,spicy foods, and carbonatedbeverages. Avoid items that reduce lower esophageal sphincter (LES) pressure, such as alcohol, caffeine, chocolate, fatty foods, peppermint and spearmint flavorsand cigarette smoking.PepticUlcerDisease (PUD) PUDischaracterizedbyanerosionofthemucosallayerof the stomach orduodenum. This may be caused by a bacterial infection with Helicobacterpyloriorthechronicuseofnon-steroidal antiinflammatorydrugs(NSAIDs),suchasaspirinand ibuprofen. Avoid eating frequent meals and snacks, as they promote increased gastric acidsecretion. Avoid alcohol, cigarette smoking, aspirin and other NSAIDs, coffee, black pepper, spicy foods, and caffeine. Lactose intolerance Lactoseintoleranceresultsfromaninadequatesupplyof lactase, the enzyme that digests lactose. Symptomsincludedistention,cramps,flatus,anddiarrhea. Clientsshouldbeencouragedtoavoidorlimittheirintake offoodshighinlactosesuchas:milk,sourcream,cheese, cream soups,coffeecreamer, chocolate,icecream,and puddings.Diverticulosisand Diverticulitis: Cholecystitis Acute Renal Failure (ARF): Pre-End Stage Renal Disease (pre-ESRD):A highfiber diet may prevent diverticulo sis and diverticuliti s by producing stools that are easily passed and thus decreasing pressure within the colon. During acute diverticuli tis, a lowfiber diet is prescribe d in order to reduce bowel stimulati on. Avoid foods with seeds or husks. Clients require instruction regarding diet adjustment based on the need for an acute intervention or preventive approach. Cholecystitis is characterized by inflammation of the gallbladder.Thegallbladderstoresandreleasesbilethat aids in the digestion of fats. Fatintake should be limited to reduce stimulation of the gallbladder. Otherfoodsthatmaycauseproblemsincludecoffee, broccoli, cauliflower, Brussels sprouts, cabbage, onions, legumes, and highly seasoned foods. Otherwise, the dietis individualized to the client's needs and tolerance. ARF is an abrupt, rapid decline in renal function. It is usually caused by trauma, sepsis, poor perfusion, or medications.ARF cancausehyponatremia,hyperkalemia, hypocalcemia, and hyperphosphatemia. Diet therapy for ARF is dependent upon the phase of ARF and its underlying cause. Pre-ESRD,ordiminishedrenalreserve/renalinsufficiency,is a predialysis condition characterized by an increase inserum creatinine. Goals of nutritional therapy for pre-ESRD are to: Help preserve remaining renal function by limiting the intake of proteinand phosphorus. Controlbloodglucoselevels andhypertension,whichare both risk factors. Proteinrestriction is keyforclients with pre-ESRD. Slows the progressionof renaldisease. Toolittleproteinresultsinbreakdownofbodyprotein,so protein intakemustbe carefullydetermined. Restricting phosphorus intake slows the progression of renal disease. Highlevelsofphosphoruscontributetocalciumand phosphorus deposits in the kidneys. Dietary recommendations for pre-ESRD:Limit meatintake. Limit dairy products to ½ cup per day. Limit high-phosphorus foods (peanut butter, dried peas and beans,bran,cola,chocolate,beer,somewhole grains). Restrict sodium intake to maintain blood pressure.End Stage Renal Disease (ESRD): End Stage Renal Disease (ESRD): ESRD, or chronic renal failure, occurs when the glomerular filtration rate(GFR)islessthan25mL/min,theserum creatininelevelsteadily rises,ordialysisortransplantation is required. The goal of nutritionaltherapyis to maintain appropriate fluid status,bloodpressure,andbloodchemistries. Ahigh-protein,low-phosphorus,low-potassium,low- sodium, fluidrestricteddietisrecommended. Calcium and vitamin D are nutrients of concern. Proteinneedsincreaseoncedialysisisbegunbecause protein and amino acids are lost in the dialysate. Fiftypercentofproteinintakeshouldcomefrombiologic sources (eggs, milk, meat, fish, poultry, soy). Adequatecalories(35cal/kgofbodyweight)shouldbe consumed to maintainbodyproteinstores. Phosphorus mustbe restricted. The high protein requirement leads to an increase in phosphorus intake. Phosphate binders must be taken with all meals and snacks. Caution clients to use vitamin and mineral supplements ONLYwhen recommended by their provider.Nephrotic Syndrome Nephrotic syndrome results in serum proteins leaking into the urine. The goals of nutritional therapy are to minimize edema, replace lost nutrients, and minimize permanent renal damage. Dietary recommendations indicate sufficient protein and low-sodium intake. Vitamin D deficiency occurs because the kidneys are unable to convertit to its active form. Thisaltersthemetabolism ofcalcium, phosphorus, and magnesium and leads to hyperphosphatemia, hypocalcemia, andhypermagnesemia. Calciumsupplementswilllikelyberequiredbecausefoods highin phosphorus(whicharerestricted)arealsohighin calcium. Potassium intake is dependent upon the client's laboratory values, which shouldbe closelymonitored. Sodiumandfluidallowancesare determinedbyblood pressure, weight,serumelectrolytelevels,andurine output. Achieving a well-balanced diet based on the above guidelines is adifficulttask. The NationalRenalDiet providesclientswith alistofappropriatefoodchoices.Nephrolithiasis (Kidney Stones) Prioritization Increasing fluidconsumptionistheprimaryinterventionfor the treatment and prevention of the formation of renal calculi. Excessiveintakeofprotein,sodium,calcium,and oxalates(rhubarb, spinach, beets)mayincreasetheriskof stone formation. Prioritization includes clinical care coordination such as clinicaldecisionmaking,prioritysetting,organizational skills,useofresources,timemanagement,andevaluation of care. Clinical decisions are made by completing a thorough assessment which will help you make good judgments later whenyouseea changingclinicalcondition.Apoorinitial assessment canleadto missedfindingslateron. Priority setting refers to addressing problems and prioritizing care.Itiscriticalforefficientcare.TheRNuses his/herknowledgeof pathophysiologywhenprioritizing interventions with multiple clients. Orders of prioritization: 1. Treatfirstanyimmediate threatsto a patient'ssurvivalor safety. Ex. obstructed airway, loss of consciousness, psychological episode or anxiety attack. ABC's. 2. Next, treat actual problems. Ex. nausea, full bowel or bladder, comfortmeasures. 3. Then, treat relativelyurgent actual orpotentialproblemsVariant angina (Prinzmetal's angina) Due to a coronary artery spasm, oftening occurring during periods of rest. Unstable angina Occurs with exercise or emotional stress, but it increases in occurrence, severity, and duration over time. Stable angina Occurswithexerciseoremotionalstressandisrelievedby rest or nitroglycerin (Nitrostat). that the patient or family does not recognize. Ex. Monitoring for post-op complications, anticipating teachingneedsofa patientthatmaybeunawareofside effects of meds. 4. Lastly, treat actual or potential problems where help may be needed in the future. Ex Teaching for self-care in the home. Herearesomegreatprinciplestohelpyouasyou prioritize: Systemic before local Acute before chronic Actualbefore potential Listen don't assume Recognize first then apply clinical knowledge Maslow's Hierarchy of Needs: PrioritizeaccordingtoMaslowwithphysiologicaland safety issues before psychologicalesteem issues.Addison's disease Decreased aldosterone and renin Hypothyroidism Decreased triiodothyronine (T3) and thyroxine Cushing's disease Elevated cortisol Diabetes Insipidus (DI) Decreased urine specific gravity Diabetesmelitus Elevated glycosylated hemoglobin (HbA1c) Angle-closure glaucoma Rapid onsetofelevatedIOP maculardegeneration Centrallossofvision Open-angle galucoma Loss of peripheral vision Retinaldetachment Sudden loss of vision without pain electrolyte imbalance manifestations: hypocakelmia--> flat T waves on ECG hypercalcemia--> decreased deep tendon reflexes (DTRs) hypocalcemia--> tetany hyperkalemia--> tall peaked T waves on ECG Syndrome of InappropriateSecretion of Antidiuretic Hormone Increased urine osmolality Cataract ProgressiveandpainlesslossofvisionBelow-the-knee amputation Position: The client should be placed in the prone position severaltimesadaytopreventhipflexioncontractions. Hepatitisdisease transmissions Heart Failure Hepatitis A-->Ingestions ocontaminated food/water HepatitisB-->Unprotectedsexualcontact Nonviral Hepatits--> Drug toxicity Symptoms:Shortnessofbreath,fatigue,jugularvein distention, and an S3aresigns/symptoms ofheartfailure resulting from the decreased pumping ability of the heart and increased fluidvolume. Hypovolemicshock position: Supine with legs elevated (shock position) Decerebrate Decorticate Common disease's manifestations Cholecystitis--> Murphy's sign Pancreatitis--> Turner's sign Peptic Ulcer Disease--> Upper epigastric pain 1-2 hours after meals Appendicits--> Pain at McBurney's pointLefthomonymous hemianopsia haslosttheleftvisualfieldofbotheyes.Theyareunable tovisualize anything tothe leftof midlineof the body. Troponin I A positive Troponin I indicates damage to cardiac tissues andlevelarenolongerevidentinthebloodafter7days. Hyperglycemia -Testurinesforketonesandreportifoutsidetheexpected reference range Chesttube -Continuous bubling in the waterseal champers indicates anairleak. Ifthisis observed, thenurseshouldattempt to located the source of the air leak and intervene accordingly(tightentheconnections, replacedrainage system) dialysis fistula client teaching: avoid lifting heavy objects with access-site arm,avoid carryingobjectsthatcompresstheextremity, avoid sleeping on top of the extremity with the access device, perform hand exercises that promote fistula maturation, check the access site at intervals following dialysis, apply light pressure if bleeding, notify the provider if the site continues to bleed after 30 min following dialysis. Synchronized cardioversion is the electrical management of choice foratrial fibrillation, supra ventricular tachycardia (SVT) and ventricular tachycardia with a pulse. Myoglobin istheearliestmarkerofinjurytocardiacorskeletalmuscle and levels no longer evident after 24 hr. Chronic renal failure Diet: low-protein, low-potassium, and high-carbohydrate, as well as low-sodium and low-phosphate Compartment syndrome Symptoms: Pulselessness (late sign), Increased pain unrelieved with elevation or by pain medicationCleft lip: nursing care plan (postoperative) —"CLEFT LIP" Crying, minimize Logan bow Elbow restraints Feed with Brechtfeeder Teach feeding techniques; two months of age (average age at repair) Liquid (sterile water), rinse after feeding Impaired feeding (nosucking) Position—never onabdomen Complication of severe preeclampsia—"HELLP" syndrome Hemolysis Elevated Liverenzymes Low Platelet count Constantbubblingina water seal chamber (of a chest tube) is an indication of anairleak atropine blocksthecardiacmuscarinicreceptorsandinhibitsthe parasympathetic nervous system. The blockage of parasympathetic activity resultsinanincreased heartrate. Whentheheartrateincreases, cardiacoutputwillalso increase.IUD: potentialproblems with use—"PAINS" Period (menstrual: late, spotting, bleeding) Abdominal pain, dyspareunia Infection (abnormalvaginaldischarge) Not feeling well,feverorchills String missing Dystocia: general aspects (maternal) —"4P's" Powers Passageway Passenger Psych Infections during pregnancy—"TORCH" Toxoplasmosis Other (hepatitis B, syphilis, group B beta strep) Rubella Cytomegalovirus Herpes simplex virusOralcontraceptives: Signs of potential problems—"ACHES" Abdominalpain(possibleliverorgallbladderproblem) Chest pain or shortness of breath (possible pulmonary embolus) Headache (possible hypertension, brain attack) Eye problems (possible hypertension or vascular accident) Severe leg pain (possible thromboembolic process) Newborn assessment components—"APGAR" Appearance Pulse Grimace Activity Respiratory effort Obstetric (maternity) history—"GTPAL" Gravida Term Preterm Abortions (SAB, TAB) Living childrenVEAL CHOP-which relatestofetalheart rate. Variable decels => Cordcompression (usuallyachange in mother's positionhelps) Earlydecels=>Headcompression(decelsmirrorthe contractions;thisisnotasignoffetalproblems) Accelerations => O2 (baby is well oxygenated-this is good) Latedecels=>Placentaluteroinsufficiency(thisisbadand means there is decreased perfusion of blood/oxygen/nutrients to the baby). Nine-point Postpartum B- Breasts Assessment...BUBBLEHE U- Uterus R B- Bladder B- Bowel function L- Lochia E- Episiotomy H- Hemorrhoids E- Emotional Status R- Respiratory System Preterm infant: Anticipated problems —"TRIES" Temperature regulation (poor) Resistance to infections (poor) Immature liver Elimination problems (necrotizing enterocolitis [NEC]) Sensory-perceptualfunctions(retinopathyofprematurity [ROP])Considerations for the pregnant client Admittance ofa pregnant client to amedical-surgicalunit: You may have a pregnant client admitted with a diagnosisunrelatedtoherpregnancyand,therefore,shemaybe admittedtoa generalmedical-surgicalfloor.Amnemonic toassistyouin performingimportantassessmentelements forthese clients is FETUS. * F: Document fetal heart tones every shift. To assess fetal hearttones, useahandheldDopplerultrasoundandplace itinanarea correspondingtouterineheight.Forexample, foraclientwho'sless than20weeks'pregnant,themost likelyareatofindfetalhearttones isatthepubichairline orthesymphysispubis.Foraclientwhose pregnancyis moreadvanced,suchasat24weeks,thefetalheartrate can most probably be heard midline between the symphysis pubis and the umbilicus. As the pregnancy advancesinweeks, fetalhearttonescanbeheardcloser to and possiblyabove the umbilicus. * E:Provideemotionalsupport.Pregnantwomenwhoare experiencingunexpectedmedicalconditionsareatahigh level of anxiety related to how the current medical problemmayaffectthe fetus.Youshouldtakeextracareto alleviateandreduceyourclient's anxietybyexplainingall medicationsandtreatments.Additionally, bepreparedto listenforfetalhearttonesanytimetheclientrequestsit to furtherreduce herworryofthe fetus'wellbeing. * T:Measurematernaltemperature.Becauseyourclient's corebody temperatureishigherthanyoucandetectthroughoralortympanicthermometers,bealerttothe presenceofa fever.Ahighmaternaltemperaturecanlead tofetaltachycardiaand distress.Anorderforantipyretics onadmissiontoensuretheirquick availabilitywillbea prudent request you should make to the admitting physician. * U: Ask about uterine activity or contractions. Make it a normal part of your routine to ask about any type of uterinepain,tightening, ordiscomfortthroughoutyour shift.Beawarethatearly contractionsoftenpresentas lowerbackpain.Don'tattribute complaintsoflowerback paintothehospitalbed.Ifyourclient reportsanyunusual activity,takecaretosoftlypalpatethelower abdomenfor periodsofgreaterthan2minuteswhileconversing with her.Watchforsubtlechangesoffacialexpressionwhile simultaneously detecting a change in uterine tone. If contractionsaresuspected,yourclientwillneedtobe monitored withcontinuousfetalmonitoringinthelabor and deliveryunit. * S:Assessforthepresenceofandchangesinsensations offetal movement.After20weeks'gestation,allwomen shouldbeableto reportfeelingthefetusmove.Thisisan importantassessmentto performanddocumentatleast everyshift,easilyaccomplishedby asking"Howoftenare youfeelingthebabymove?"Byaskingthisas anopen- ended question, you'll receive more information about the quantityoffetalmovement suchas, "Ihaven'tfeltthe baby move as much as usual today."Admittance of a postpartum client to a medical-surgicalunit There are times when a woman may be hospitalized during thepostpartumperiodforamedicalcondition. Whenthis occurs,she'llmostlikelybeplacedonageneralmedical- surgical unit.Heradmissionwillcauseyoutoask:"What's normalduringthe weeksfollowingthebirthofababy?" * Breasts. Within thefirst24 hourspostpartum, colostrum appears andisfollowedbybreastmilkwithinthefirst72 hours.Breast engorgementismostlikelytooccuraround day4postpartum.The engorgedbreastwillappearfull, taut,andevenshiny.Althoughthisis normal,itmaybe very uncomfortableforyourclient.Incontrast,a womanwith mastitiswillusuallyrunafeverhigherthan100°F,report feeling "ill," and have one breast that's affected (firm, inflamed, swollen, and exquisitelytenderto touch). Ifyour clientisbreastfeeding hernewborn,she'llrequireabreast pump.Dependingonthe medicationsordered,themilk mayneedtobedisposedofandnot usedforthebaby. * Lochia. Sometimes women will experience lochia (vaginal discharge)untilthetimeoftheir6-weekpostpartumvisit. Immediatelyafterdelivery,thelochiaisredandheavy enoughto requireapadchangeevery1to2hours.By7 days postpartum, the lochia should be lighter in color (pink tored)andamount,requiringa padchangeevery4hours. Lochia that becomes heavier, has a foul odor, and is accompanied by pelvic pain isn't a normal finding and requires immediateintervention.* Perinealcare.Forthefirst2weeksfollowingdelivery, clientswill needtoperformperinealhygieneastaught duringtheimmediate postpartumperiod. Thismayinclude perinealwaterrinsesfollowing eliminationusingwarm waterormedicinalrinses,useofsitzbaths, andcomfort medications to the perinealand analarea. * Cesareansection.Ifyourclientdeliveredherbabyvia cesarean section,continuedassessmentofthesurgical incisioniswarranted forthefirst2to3weekspostpartum. Redness and warmth around the incision, excessive bruising around the incision,orincisional drainage requires immediateintervention.Ifthesurgeonused staplesto close the incision, they're usually removed approximately 5 days post-delivery. Placenta Previa(PP) versus Abruptio Placenta (AP) Remember,thehospitalizedpostpartumclientislikelyto bevery emotional.Notonlywillshebeexperiencingthe normalhormonal fluctuationsofthepostpartumperiod, she'll may also be distraught leaving her newborn at home and feeling thatshe'smissing bonding time with herchild. Visitation between the mother and her infant may be very limited to minimize theinfant'sriskofinfection, butvisits should be arranged if at all possible. Problem: PP--> Lowimplantation of the placenta AP--> Premature separation of the placenta Incidence:PP-->Itoccursinapproximately5inevery1000 pregnancies AP-->Itoccursinabout10%ofpregnanciesandisthe most common cause of perinataldeath Risk factors: PP--> increased parity, advanced maternal age, past cesarean births,pastuterinecurettage,multiplegestation, AP-->highparity, advanced maternalage,ashortumbilical cord,chronichypertensive disease,pregnancy-induced hypertension, direct trauma, vasoconstriction from cigarette use, thrombic conditions thatlead to thrombosis such as autoimmune antibodies Bleeding: PP--> Always present AP--> May or may not be present Color of blood in bleeding episodes: PP-->Brightred AP-->Darkred Pain during bleeding: PP--> Painless AP--> Sharp, stabbingpain Management: PP-->Placethewomanimmediatelyonbedrestinaside- lyon position. Weight perineal pads. NEVER attempt a pelvicorrectal examinationbecauseitmayinitiate massive blood loss. AP--> Fluid replacement. Oxygen by mask. Monitor FHR. Keep thewomaninalateralposition.DONOTperformany vaginalor pelvicexaminationsorgiveenema.PregnancyCommon Thyroid Levo thyro xine (Syn thro id,Levo thro id) Medications Lio thyro nien(Cytomel) Liotrix ( Thyrolar) Thyroid ( ThryoidUSP) Antithyroid Medications (hyperthyroidism) Thyroid-Radioactive Iodine (hyperthyroidism) Antithyroid medications areusedto block (anti)the thyroid hormones. Antithyroid medications block (anti) the conversionof T4intoT3.UsedtotreatclientswithGraves Disease, thyro toxicosis. Antithryoid medications are prescribedforclientswhohavean overactivethyroidor hyperthyroidism. Inhyperthyroidism....... everything is HIGHHHHHHH(HYPERRRRRRRRR) Clients that are prescribed this medication need to take radioactivity precautions. Common Antithyroid Medications: Propylthiouracil (PTU) Athighdoses,thyroidradioactiveiodinedestroysthyroid cells.This drugisusedforclientswhohavethyroidcancer and an over active thyroid (hyperthyroidism). must be terminated because the fetus cannot obtain adequateoxygenandnutrients.Ifbirthdoesnotseem imminent, cesarean birth is method of choice for delivery.Thyroid- NonRadioactive Iodine (hyperthyroidism) Oral Hypoglycemic Agents ForInsuline Overdose Thismedicationcreatesahighlevelofiodinethatwill reduce iodine uptake bythe thyroid gland. Itinhibits the thyroidhormone productionandblocksthereleaseof thyroid hormones into the bloodstream. Thismedicationtastesnasty;hasametallictaste!Clients aretodrink thismedicationthroughastrawtoprevent toothdiscoloration. Radioactivityprecautionsarenot necessaryduetothisdrugis nonradioactive. These medications promote insulin release from the pancreas. Clientswhoareprescribedoralhypoglycemic agentsdonotproduce enoughinsulintolowertheirblood glucose(bloodsugar)levels. Prescribedforclientswith type 2 DiabetesMellitus. Common Oral HypoglycemicAgents: glipizide(Glucotrol,GlucotrolXL).Seetheformof glucose in the drug name? chlorpropamide ( Diab ines).See the form ofDiabetes in the drug name? glyburide ( Diab inese,Micronase). See the form of Diabetes in the drug name? metforminHC1 ( Gluco phage). See the form of glucose in the drug name? Common medication for insulin overdose: Gluc agon (see the form of glucose in the drug name?) Glucagon (or glucose) isneeded toincrease blood glucoseorblood sugar.Posterior Pituitary Hormones/Antidiuretic Hormone This medication promotes the reabsorption of water within the kidneys; causes vaso constriction due to the contraction of vascularsmooth muscle. Common Posterior Pituitary Hormones/Antidiruetic Hormones: desmopressin(DDAVP,stimate) vaso pressin (Pitressin synthetic) (See the form of vasoin the drug name, for vaso constriction) Anterior Pituitary Hormons/Growth Hormones These medications stimulate growth. Areused to treat growth hormonedeficiencies. Use cautiously in clients who have Diabetes Mellitus since these medicationscausehyperglycemiabecauseofthe decreased use of glucose. Common Anterior Pituitary Hormones/GrowthHormone Agents: somatropin somatrem(Protropin) Anticonvulsants The anticonvulsants are medications used for the treatment of epilepticseizures.Thesemedssuppresstherapidand firing ofneurons in the brainthatstartaseizure. Drugs for all types of seizures, except petit mal: CaPhe like cafe in French CA rbamazepinePHE nytoin/Phenobarbital Drugs forpetitmalseizures: ValEt Val proic Acid Ethosuximide Phenytoin: adverse effects P - interactions H irsutism Enlargedgums N ystagmus Yellow-browning of skin T eratogenicity O steomalacia InterferencewithBmetabolism(henceanemia) N europathies:vertigo,ataxia,headache Allanti-epilepticdrugscanberememberedbythis mnemonic: Dr.BHAISAB's New PC.D...Deoxybarbiturates B ...Barbiturates H....Hydantoin A ... Aliphatic carbacids I ....Iminostilbenes S....Succinimides B ... Benzodiazepines (BZD's) N....Newerdrugs P....Phenyltriazines C ...Cyclic gabaanaloguesAntiparkinsonian Opthalmic Anantiparkinson,orantiparkinsonianmedicationsareused forclients diagnosed withParkinson'sDisease. These medications increase dopamine activity orreduce acetylcholineactivityinthebrain.Theydonothaltthe progression of the disease. These medications offer symptomatic relief. Anti-Parkinsonian Drugs include: A Cat Does Like Milk! A nticholinergicAgents COMTInhibitors (catechol-O-methyltransferase);An enzyme involvedindegradingneurotransmitters. D opamine Agonists L evodopa M AO-B Inhibitors Ophthalmic medications are drugs used forthe eye. These medications are typically prescribed for clients who have Glaucoma, MacularDegeneration. Otherophthalmic medications are used to treat allergic conjunctivitis, inflammatorydisorders, dyesto visualize the eye, and to treat infections orviruses. Beta-Adrenergic Blocking Agents Prescribedforclientswhohaveopen-angleglaucoma. These agents decrease the production of aqueous humor. Block beta 1and beta 2 receptors. Common Beta-Adrenergic Ophthalmic Blocking Agents:betaxolos(Betoptic)(seetheformofbetainthedrug names?)See opticinBetoptic?Opthalmicmedication. levobetaxolol(Betaxon)(seetheformofbetainthe drug names?) levobunolol(Betagan)(seetheformofbetainthedrug name?) timolol(Betimol)(seetheformofbetainthedrugname?) Prostaglandin Analogs First line treatment forglaucoma. Fewer side effects and just as effective as the beta-adrenergic Ophthalmic blocking agents. These drugs lower IOP by facilitating aqueous humor outflow by relaxingthe ciliarymuscle. Common Prostaglandin Analogs: latanoprost (Xalatan ) (seethe suffix atan in this drug and the drug below,they are the same) Travoprost(travatan )(seethe suffixatanin this drugand the drug above; they are the same) Alpha2-Adrenergic Agonists These drugs lower IOP by reducing aqueous humor productionandbyincreasingoutflow. Alsodelaysoptic nerve degeneration and protects retinal neurons fromdeath. Common Alpha2-Adrenergic Agonists: Brimonidine(Alphagan)(seethesimilaritieswithidinein the name of the drug) Apraclonidine (Iop idine )(see the similarities withidine in both of the names of the drug) Direct Acting Cholinergic Agonist/Muscarinic Agonist (parasympathomimetic agent) These drugs stimulate the cholinergic receptors in the eye, constricts the pupil(miosis), and contraction of the ciliary muscle. IOP is reduced by the tension generated by contractingtheciliarymuscle andpromoteswideningof the spaces within the trabecular meshwork, thereby facilitating outflowof aqueous humor. Common Direct Acting Cholinergic AgonistAgents: Pilocarpine Key points of ophthalmic medications: · Cyloplegicsaredrugsthatcauseparalysisoftheciliary muscle...plegic-like paraplegic,paralysis · Mydriatics are drugs that dilate the pupil. · Drugtherapyforglaucomaisdirectedatreducing elevated IOP,byincreasingaqueoushumoroutflowor decreasing aqueous humor production.· Oculus Dexter: OD (right eye) · Oculus Sinister: OS (left eye) · Oculus Uterque: OU (both eyes) Remember BAD POCC: Ophthalmic Medication Classes for treatment of Glaucoma B-betaadrenergicblockingagents A - Alpha-AdrenergicAgonists D-DirectActingCholinergicAgonists P - ProstaglandinAnalogs O -Osmotic Agents C -Carbonic AnhydraseInhibitors C -Cholinesterase Inhibitor; An indirect acting Cholinergic Agonist RememberBADPOCCforkeypointsorsideeffectsof Opthalmic Medications: B -Blurred vision A-Angleclosureglaucoma(medicationsareusedforthis kind of glaucoma) D -Dry eyesTaking in phase 24-48 hours after birth: dependent, passive; focuses on own needs; excited,talkative Taking hold phase focusesonmaternalroleandcareofthenewborn; eager to learn; may develop blues Lettinggophase Focuses on family and individual roles Cephalopelvic disproportion Whenthefetushasaheadsize,shapeorpositionthat does not allow for passage through the pelvis. Hyperemesis Gravidarum HELLP syndrome Severe morning sickness with unrelenting, excessive nausea or vomiting that prevents adequate intake of food and fluids A variant of gestational hypertension where hematologic conditions coexist with severe preeclampsia and hepatic dysfunction. Mild preeclampsia Hypertension beginning after the 20th week of pregnancy with1to2+ proteinuriaandaweightgainofmorethan2kg per week in the second and third trimesters. Eclampsia Severe preeclampsia symptoms with seizure activity or coma Gestational hypertension Hypertension beginning after the 20th week of pregnancy with no proteinuria. Gestational diabetes mellitus Impairedtolerancetoglucosewiththefirstonsetor recognition during pregnancy P-Photophobia O-Ocularpressure(usedtotreatOPfromglaucoma) C-CanCausesystemiceffects C -Ciliary muscleconstrictionRegularity The amount of consistency in the frequency and intensity of contractions. Station The relationship ofthe presenting parttothematernal ischial spines that measures the degree of descent of the fetus. Presentation Transverse lie Includes cephalic, breech and shoulder. The longaxis of the fetus is at aright angle to the mother's long axis. This is incompatible with avaginaldelivery ifthe fetus remains in this position missing birthcontrol pills... Intheeventofaclientmissingadosethenurseshould instructthe clientthatifonepillismissedtotakeassoon aspossible.Iftwoor threepillsaremissedtheclient should follow the manufacturer's instructions and use an alternative form ofcontraception. pediatric carbon cord--> 14-22 dioxide premature 1 week --> 14-27 pediatric acetaminophen levels >200 mcg/ml Frequency Theamountoftimefromthebeginningofonecontraction to the beginning of the next contraction Longitudinal lie Thefetallongaxisisparalleltothemother'slongaxis.The fetus is either in a breech or vertex presentation Duration Theamountoftimeelapsedfromthebeginningofone contraction to the end of the same contraction. Intensity The strength of the uterine contraction.newborn --> 13-22 infant, child --> 20-28pediatric Digoxin toxic concentration > 2.5 ng/ml pediatricchloridelevel Cord --> 96-104 Newborn --> 97-110 Child --> 98-106 pediatric creatinine cord --> 0.6-1.2 level newborn --> 0.3-1.0 infant 0.2-0.4 child --> 0.3-0.7 adolescent --> 0.5-1.0 pediatricGlucose (Serum) Newborn, 1 day --> 40 to 60 Newborn, > 1 day --> 50 to 90 Child --> 60 to 100 pediatric Hematocrit 1 day --> 48-69% levels 2 day--> 48-75% 3 day --> 44-72 % 2 month --> 28-42 % 6- 12 year --> 37-49% 12- 18 year Male --> 37-49% 12-18 year Female --> 36-46% Antigout Medications - What isgout? Goutisatypeofarthritis.Inhealthypeoplethebody breaksdowndietarypurinesand producesuricacid.The uric acid dissolves and is excreted via the kidneys. In individuals Conjugated direct Bilirubin level 0.0-0.2 mg/dlaffectedwith goutthebody either produces too muchuricacid orisunableto excrete enoughuric acid and it builds up. High uric acid levels results in urate crystals which can now collect in joints or tissues. This causessevere pain, inflammation andswelling. Treatmentis both lifestyle adjustment and medication.Medications First Line: NSAIDs and prednisone (Deltasone) Purpose: Used as a first line defense to treat the pain and inflammation of gout attacks. Colchicine (Colgout): Purpose: Treat the inflammation and pain associated with gout. Justlike NSAIDs, these meds can leadto GI distress and should be taken with foods. HINT: The word gout is right in the name Colgout. Allopurinol (Zyloprim): Purpose: This is the only medical preventative treatment forgout. Allopurinal preventsuricacidproduction.Thiscanbean effectivemeansof preventinggoutattackswhendiet alone is noteffective. HINT: Examine the name allopurinol and you can see the word PURINE in the middle of the name. Note: There are many drug and food interactions associated with allopurinol: Potentialseriousinteractionswiththeuseofsaliscylates, loop diuretics,phenylbutazaminesandalcoholandAnti-reabsorptives Whatisanati-reabsorptive? Boneisalivingorgan whichiscontinuallybeingremoved (resorbed) and rebuilt. Osteoporosis develops when there is more resorption than rebuilding. Antiresorptive medications are designed to slow bone removal and or improve bone mass. Treating and preventing osteoporosis can involve lifestyle changes and sometimes medication. Lifestyle change includes diet and exercise, and fall prevention. Prevention and treatment of osteoporosis involve medications that work by preventing bone breakdown or promote new bone formation. Medications Bisphosphonates prevent the loss of bone mass potential fordrug interactions with Warfarin (Coumadin). Teach client with gout to avoid the following: · Anchovies, sardine in oil, fish roe, herring · Yeast · Organ meat (liver, kidneys, sweetbreads) · Legumes (dried beans and peas) · Meathextracts (gravies and consommé) · Mushrooms, spinach, asparagus, cauliflowerAlendronate (Fosamax) Monthlyusedtotreatandpreventosteoporosisin menopausal women. Facts:ThebenefitsofFosamaxcanevenbeseeninelderly women over75years of age. Hint: Fosamax has been associated with severe esophagitis andulcers oftheesophagus.Shouldbeavoidedinclients with history of gastric ulcers. Risedronate (Actonel): This is a newer drug and less likely to cause esophageal irritation Hint: Teach clients taking either drug to take on an empty stomach withatleast8ounces(240ml)ofwater,while sittingorstanding. Thisminimizesthechancesofthepill being lodged in the esophagus. Clients should also remain uprightforatleast30minutesaftertaking thesepillsto avoid refluxin to the esophagus. Forthoseclientswhocannottoleratetheesophagusside effectsof Fosamax, estrogen, etidronate (Didronel), and calcitonin are possible alternatives. Teriparatide (Forteo): It acts like parathyroid hormone and stimulates osteoblasts,thusincreasingtheiractivity. Promotes bone formation. Facts:Thisdrugisassociatedwithariskofbonetumorsso is only used when the benefits outweigh the risks.Antirheumatics What is rheumatoid arthritis? Rheumatoidarthritis(RA)isachronicdiseasethatresultsin inflammationofthejointsandsurroundingtissues.RA affectsthe liningofthejointsandthepainfulswellingcan resultinboneerosion andjointdeformities.Itisthesmall jointsinhandsand feetaremost often affected. Treatment is designed to provide symptom relief and some delayin progressionofthe disorderbutnotacure. Medications Disease-modifying Antirheumatic drugs (DMARDs), glucocorticoids, and non-steroidal anti-inflammatory drugs (NSAIDs) may be used individuallyorin combination to manage this chronic disorder. The major categories of antirhematics are: DMARDsI - MajorNonbiologic DMARDs · Cytotoxic medications: Methotrexate (Rheumatrex), leflunomide (Arava) · Antimalarialagents:Hydroxychloroquine(Plaquenil) · Anti-inflammatory medication: Sulfasalazine (Azulfidine) · Tetracycline antibiotic: Minocycline (Minocin) DMARDs II - MajorBiologic DMARDs · Etanercept (Enbrel)· Infliximab (Remicade) · Adalimumab (Humira) · Rituximab (Rituxan) · Abatacept (Orencia) DMARDs III - Minor nonbiologic and biologic DMARDs · Gold salts: Aurothioglucose (Solganal) · Penicillamine (Cuprimine,Depen) · Cytotoxic medications: Azathioprine (Imuran), cyclosporine (Sandimmune, Gengraf, Neoral) · Glucocorticoids: · Prednisone (Deltasone), prednisolone (Prelone) ● NSAIDs Hints: DMARDsslowjointdegenerationandprogressionof rheumatoid arthritis. GlucocorticoidsandNSAIDsprovidesymptomrelieffrom inflammation and pain. Rheumatrex(methotrexate)isthemostcommonlyused DMARD. ThisisbecauseithasbeenshowntoworkaswellAntineoplastics Antineoplastics are used combat cancerous cells. Therearemanykindsofanti-cancerdrugswithavarietyof actions. Butinsimpletermsthiscategoryofdrugsattack cellsthat multiply and divide. This veryaction which can kill cancercellscanalsodothesame tohealthydividingcells. Thisisespeciallytrueofcellsthatneeda steadysupplyof new cells such asskin, hairand nails. There are over 90 different kinds of chemotherapy agents and differentdrugs cause differentside effects Chemotherapy is associated with a variety of side effects: § Nausea andvomiting § Diarrhea and or constipation §Alopecia § Anorexia § Fatigue andexhaustion orbetterthananyothersinglemedicine.Itisalsorelatively inexpensive and generally safe. Methotrexate has many food and drug interactions especiallyaffectdigoxinandphenytoin.Verydifficultto absorb and should be taken on an empty stomach. Taking folic acid helps reduce some of the side effects. Methotrexate's biggest advantage could be that it has been shown tobe safeto take forlong periods of time and can even be used in children.§ Mouth sores § Easy bruising Medications Fluorouracil (5-fluorouracil, 5-FU) Warning - Hazardous drug! 5-FUisoneoftheoldestchemotherapydrugsandisused against a variety of cancers. Followingaresomeofthemostcommonandimportantill effects: · Soreness of the mouth, difficulty swallowing · Diarrhea · Stomach pain · Lowplatelets · Anemia · Sensitive skin (to sun exposure) · Excessive tear formation from the eyes Nursing Hints: Be aware of the importance of leucovorin rescue with fluorouracil therapy, if prescribed.Oral hypoglycemics What is diabetes? Diabetesisadisorderthataffectsglucose metabolism. Type 1 diabetes: Theclient eithermakesno insulinornot enough insulin. Type2diabetes:Theclientmakesenoughinsulinatleast earlyinthe diseasebutisunabletotransportglucosefrom the blood into the cells. Inbothcases,theindividualisunabletometabolize glucose.The purposeoforalhypoglycemicsistoassist with glucose metabolism. Medications There are four classes of hypoglycemic drugs: · The best treatment for extravasation is prevention. · Extravasation can cause pain, reddening, or irritation on thearmwiththeinfusionneedle.Inseverecasesincan leadtotissuenecrosisandevenlossofanextremity. · Check infusion site frequently · Stop infusion immediately if suspected · Slowlyaspirate back blood back from the arm · Elevatearmandrestinelevatedposition · Checkinstitutionpoliciesonhowtoremovecatheter· Sulfonylureas Tolbutamide (Orin ase); glyburide; Micronase Stimulates insulinproduction Associated with weight gain · Biguanide: Metformin o First line drug in type 2 diabetes o Reducesthe production ofglucose withinthe liver o Associated with modest weight loss o Less likelyto cause hypoglycemia. o Significant lipid-loweringactivity. · Thiazolidinediones o Reverses insulinresistance o Increases glucose uptake and decreasedglucose production o Associated with severeliverdamage · Alpha-glucosidaseinhibitors. o Acarbose (Precose)oReducestheabsorptionofdietaryglucose oAssociatedwithflatulenceanddiarrhea Hints: Nomatterwhichclasstheclientwillbetakingthereis always the risk of hypoglycemia Be suretoteachclienthowtorecognizeearlysignsand symptoms of hypoglycemia as wellas appropriate interventions.MentalStatusExam Allclients should have a Mental Status Exam, which includes: Level of consciousness Physical appearance Behavior Cognitive and intellectual abilities ThenurseconductstheMSEaspartofhisorherroutine and ongoing assessment of the client. Changes in Mental Statusshould beinvestigatedfurtherandtheprovider notified. There are two types of mental health hospitalizations: Voluntary commitment and involuntary or civil commitment. Involuntary commitment is against the client's will. Despite that, unless proven otherwise, clients arestill considered competent and have the right to refuse treatment.ECT Themostcommontypeofbrainstimulation therapyis electronconvulsive therapy or ECT. ECT is generally performed for major depressive disorders, schizophrenia oracutemanicdisorders.Mostclientsreceivetherapy threetimesaweekfortwotothreeweeks.PriortoECT, carefullyscreentheclientforanyhomemedicationuse. Lithium,MAOIsandallseizurethresholdmedications should be discontinued twoweeks priortoECT. After therapy,reorienttheclientasshorttermmemorylossis common. Use the following * If the client is anxious or depressed - use open-ended, communication tips supportive statements when answering *Iftheclientissuicidal-usedirect,yesornoquestionsto questions on NCLEX: assess suicide risk * If the client is panicked - use gentle guidance and direction * If the client is confused - provide reality orientation * If the client has delusions / hallucinations / paranoia - acknowledge these, but don't reinforce * If the client has obsessive / compulsive behavior - communicate AFTER the compulsive behavior * If the client has a personality or cognitive disorder - be calm and matter-of-fact Anxiety disorders Anxietydisordersarecommonmentalhealthdisorders. GeneralizedAnxietyDisorder,PanicDisorder,Phobias, Obsessive CompulsiveDisorder,andPosttraumaticstress disorder (PTSD) are all considered types of anxiety disorders.Assesstheclientfor riskfactors,triggersand responses.TCAs TCAs:TricyclicAntidepressants. Amitriptyline (Elavil)isan example. Anticholinergic effects and orthostatic hypotension may occur. Depressive disorders Bipolar disorders A classic symptom of depression is change in sleep patterns, indecisiveness, decreased concentration, or changeinbody weight.Anyclientwhoshowsthesesigns orsymptoms should be asked ifthey have suicidalideation. Teach clients to never discontinue anti-depressants suddenly. Bipolar disorders are mood disorders with periods of depression andmania.Clientshaveahighriskforinjury during the manic phase related to decreased sleep, feelings of grandiosity and impulsivity. Hospitalization is oftenrequiredandnursesshould provideforclientsafety. violent clients For the aggressive or violent client, setting boundaries and limits on behavior are important. The nurse should maintain a calm approach anduseshort,simplesentences. SSRI's SSRIs: Selective Serotonin Reuptake Inhibitors. These medicationsincludeCitalopram(Celexa),Fluoxetine (Prozac),orSertraline(Zoloft).Theclientshouldavoid using St. John's Wort with these medications, and should eat a healthy diet while on these medications. abuse There are several different types of abuse, including physical,sexual,oremotional.Abusetendstobecyclic, following a pattern on tension building, battering and honeymoon phase. When test questions appear related to abuse, look forthe phase to determine the correct response.Atypical antidepressants Atypical antidepressants. Bupropion (Wellbutrin) is the most common example. Appetite suppression is a common side-effect. Headacheanddrymouthmaybesevereand client should notify the provider if this occurs. Atypical antidepressants should not be used with clients with seizure disorders. Antagonists In order to understand how antagonist drugs work, you need to understand howagonist drugs produce therapeuticeffects.Agonistsaresimplydrugsthatallow the body's neurotransmitters, hormones, and other regulators to perform the jobs they are supposed to perform. Morphine sulfate, codeine, and meperidine (Demerol) are opioids agonists that act on the mu receptorstoproduceanalgesia,respiratory depression, euphoria,andsedation.Thesedrugsalsoworkon kappa receptors, resulting in pain control, sedation and decreased GI motility. Antagonists, on the otherhand, are drugsthat preventthebodyfromperformingafunction that it would normally perform. To quote William Shakespeare&theUSArmy, thesedrugclassesallowthe body'sfunctions"tobeornottobe...all thattheycanbe". Common uses of antagonists: SNRI's Serotonin Norepinephrine Reuptake Inhibitors. Common SNRIs include Venlafaxine (Effexor) and Duloxetine (Cymbalta). Adverse effects may include nausea, weight gain, and sexual dysfunction. MAOIs MAOIs: Monoamine Oxidase Inhibitors. Phenelzine (Nardil) is an example. Hypertensive crisis may occur with tyramine food ingestion, so care must be taken to avoid these substances.Educatethe clienttoavoidallmedications until discussed with provider.· Treatmentof opioidsoverdose,reversalofeffectsof opioids, or reversalof respiratory depression in an infant · Example: a post-operative client receiving morphine sulfate for pain control experiences respiratory depression and is treated with naloxone (Narcan) Nursing Interventions for antagonists: · Monitor for side/adverse effects · Tachycardia and tachypnea · Abstinence syndrome in clients who are physically dependent on opioids agonists · Monitor for symptoms to include cramping, hypertension, and vomiting · Administer naloxone by IV, IM or subcutaneous routes, not orally · Bepreparedtoaddressclient'spainbecausenaloxone will immediatelystoptheanalgesiaeffectoftheopioidthe client had taken · When used for respiratory depression, monitor for return to normal respiratoryrate(16-20/minforadults;40-60/min fornewborns)Antidotes Bronchodilators Antidotesareagentsgiventocounteracttheeffectsof poisoning related to toxicity of certain drugs or substances. Antidotes are extremelyvaluable, however most drugs do not haveaspecific antidote. Atropine-->is the antidote formuscarinic agnostic and cholinesterase inhibitors: Bethanechol (Urecholine), Neostigmine (Prostigmin) Phyosostigmine (Antillirium)--> is the antidote for anticholinergic drugs,atropine. DigoxinimmuneFab(Digibind)-->istheantidotefor digoxin, digitoxin VitaminK-->istheantidoteforWarfarin(Coumadin) Protaminesulfate-->istheantidoteforHeparin Glucagon-->istheantidoteforinsulin-induced hypoglycemia Acetylcysteine(Mucomyst)-->istheantidotefor acetaminophen (tylenol) Bronchodilators are used to treat the symptoms of asthma thatresultfrominflammationofthebronchialpassages, buttheydonottreattheinflammation.Therefore,most clients with asthma take an inhaled glucocorticoid concurrentlytoprovide thebestoutcomes.Thetwomost common classes of bronchodilators are beta2- adrenergicagonists and methylxanthines. Beta2-adrenergic agonists : actupon the beta2-receptors in the bronchial smooth muscle to provide bronchodilationandrelievespasmofthebronchialtubes,inhibitreleaseof histamines and increase motility of bronchial cilia. These short-acting preparations provide short-term relief during an asthma exacerbation, while the long-acting preparations provide longterm control of asthma symptoms. Thegenericnamesfortheinhaledformofthesedrugsend in"terol"=" TakingEasesRespiratorydistressorLabored breathing" · Albu terol (Proventil,Ventolin) · Formo terol (Foradil Aerolizer) · Salme terol(Serevent) Thebrandnamesofsomedrugsinthisclassprovideahint aswell becausetheycontainthewords "vent"or"breth " referring to ventilation or breathing: · Albuterol (Pro vent il, Vent olin) · Salmeterol(Serevent) · Terbutaline(Brethine) Nursing interventions and client education: · Short-acting inhaled preparations of albuterol (Proventil, Ventolin) can cause systemic effects of tachycardia, angina, andtremors. · Monitorclient's pulse rate before,during, and afternebulizer or inhaler treatments · Long-acting inhaled preparations can increase the risk of severe asthma orasthma-related death ifusedincorrectly —mainly if used without concurrent inhaled glucocorticoid use · Oralpreparationscancauseanginapectorisor tachydysrhythmiaswithexcessiveuse · Instruct clients to report chest pain or changes in heart rate/rhythm to primarycare provider · Clientshouldbetaughtproperprocedurewhenusing metered dose inhaler(MDI) and spacer · Iftakingbeta2-agonistandinhaledglucocorticoid concurrently, take the beta2-agonist first to promote bronchodilation which will enhance absorption of the glucocorticoid · Advise client not to exceed prescribed doses · Adviseclienttoobserveforsignsofimpendingasthma attacks and keep log of frequency and intensity of attacks · Instructtonotifyprimarycareproviderifthereisan increase in frequencyorintensityofasthma attacks Methylxanthines:causebronchialsmoothmuscle relaxationresultinginbronchodilation. Theophylline (Theolair) is the prototype medication and is used for long-term controlofchronic asthmaACE inhibitors ACE inhibitors block the production ofangiotensin II which resultsinvasodilation,sodiumandwaterexcretion,and potassium retention. Drugs in this class are used for treating heartfailure,hypertension,myocardialinfarction, anddiabeticor nondiabeticnephropathy.Clientstaking captopril(Capoten) shouldbeinstructedtotake medat least1 hourbeforemeals;all otherACEinhibitorsarenot affected by food. The generic names of ACE inhibitors end in "pril": · Capto pril(Capoten) · Enala pril(Vasotec) · Fosino pril(Monopril) Nursing interventions: · Monitor serum levels for toxicity at levels >20 mcg/mL · Mild toxicity can cause GI distress and restlessness · Moderate to severe toxicity can cause dysrhythmias and seizures · Educatedclientregardingpotentialmedicationandfood interactions that can affect serum theophylline levels · Caffeine, cimetidine (Tagamet), and ciprofloxacin (Cipro) can increase levels · Phenobarbital and phenytoin can decrease levels· Lisino pril(Prinivil) · Rami pril (Altace) Side/adverse effects include: · Orthostatic hypotension with first dose · InstructclienttomonitorBPforatleast2hoursafterfirst dose · Cough, rashoralteredordistorted taste(dysgeusia) · Instruct client to notify health care provider · Angioedema · Treated with epinephrine and symptoms will resolve once medication isstopped · Neutropeniaisrarebutserious withcaptopril(Capoten) · Instruct client to report signs of infection Hyperkalemiacanbelife-threatening Monitor potassium levels to maintain normal range of 3.5- 5.0 mEq/L Medication/food interactions: · Concurrent use with diuretics can lead to first-dose orthostatic hypotensionVasodilators ... · Concurrent use with other antihypertensives can lead to increase effect resultingin hypotension · Concurrent use with potassium supplements or potassium-sparing diuretics increases the risk of hyperkalemia · Concurrentusewithlithiumcanincreaseserumlithium levels, leading to lithium toxicity · Concurrent use with NSAIDs can decrease the therapeutic effectsofthe ACEinhibitor Blood Transfusion - Typesofreactionsand onset Acute hemolytic -immediate Febrile-30minto6hraftertransfusion Mild allergic - During or up to 24 hr after transfusion Anaphylactic - immediate Blood Transfusion - Circulatory overload: Potential Complications Administer oxygen. Monitor vitalsigns. Slow the infusionrate. Blood Transfusion Reaction - Medications Antipyretics (acetaminophen [Tylenol]) - febrile Antihistamines (diphenhydramine [Benadryl]) - mild allergic Antihistamines, corticosteroids, vasopressors - anaphylacticAdminister diuretics as prescribed. Notify the provider immediatelyBlood Transfusion - Sepsis and septic shock Maintain patent airway. Administer oxygen. Administerantibiotics as prescribed. Obtainbloodsamplesforculture. Administervasopressorsinlatephase. Elevate client'sfeet. Assessfordisseminated intravascularcoagulation. Digoxin -Take apical Digoxin-Instructtheclientnottotakemedicationwithin2 pulse for 1 min, and hr of eating, and teach client how monitor laboratory to take an apical pulse for 1 min. levels for signsof toxicity. Sodium polystyrene- Sodium polystyrene - Monitor for hypokalemia, and Instruct the client to restrict sodium intake. take a mild laxative if constipated, andteach how to take blood pressure Epoetin alfa - Instruct Epoetin alfa - Administer by subcutaneous route, and the client about having monitor forhypertension. blood tests twicea week and how to take blood pressure. Ferrous sulfate - Ferrous sulfate - Administer following dialysis and with a Instruct the client to stool softener take medicationwith food and that stools willbe dark in color.Aluminum hydroxide Aluminum hydroxide gel - Instruct the client to report gel - Avoid constipation to the provider and to take administering ifclient 2 hr before or after receiving digoxin. has gastrointestinal disorders; administer astool softener withthis medication Furosemide - Monitor intake and output and blood pressure. Furosemide - Instruct the client to weigh selfeach morning and to notify providerof light - headedness, excess thirst, and unusual coughing Asthma - Combination agents (bronchodilator and anti-inflammatory) Ifprescribed separatelyforinhalationadministrationatthe same time, administerthe bronchodilator first in order to increase the absorption of the anti-inflammatoryagent Ipratropium and albuterol (Combivent) Fluticasone and salmeterol(Advair)ASTHMA- Encourage the client to drink plenty of fluids to promote hydration. Encourage client to avoid persons with respiratory infections. Use good mouthcare. Encouragetheclientto take prednisone with food. Do not stop the use of this type of medication suddenly. Adviseclienttousethis medication to prevent asthma, not for the onset of an attack. Short-acting beta2 Provide rapid relief of acute agonists, suchas symptoms and prevent exercise-induced asthma. albuterol (Proventil, Ventolin) Anticholinergic medications, such as ipratropium (Atrovent), block the parasympathetic nervous system. This allows forthe sympathetic nervous system effects of increased bronchodilation and decreased pulmonary secretions. These medications are long-acting and used to prevent bronchospasmsIpratropium -Advise the clienttosuckon hard candiestohelp relieve dry mouth; increase fluid intake; and report headache, blurred vision, orpalpitations, which may indicate toxicity of ipratropium. Methylxanthines, such as theophylline(Theo- 24), require close monitoring of serum medication levelsduetoanarrow therapeuticrange. Short-acting beta2 agonists, such as albuterol (Proventil, Ventolin), provide rapid relief of acute symptoms andprevent exerciseinduced asthma. Ipratropium - Observe the client fordry mouth. Monitor the client's heart rate Use only when other treatments are ineffective. Theophylline - Monitor the client's serum levels for toxicity. Side effects will include tachycardia, nausea,anddiarrhea Albuterol - Watch the client for tremors and tachycardia. Salmeterol - Asthma Salmeterol-Adviseclienttousetopreventanasthma attack and not at the onset of an attackCombination agents (bronchodilator and anti-inflammatory) Ifprescribed separatelyforinhalationadministrationatthe same time, administerthe bronchodilator first in order to increase the absorption of the anti-inflammatoryagent Ipratropium and albuterol (Combivent) Fluticasone and salmeterol(Advair) Nursing Interventions/Client Education Advise the client to report black, tarry stools. Observe the client for fluid retention and weight gain. This can be common. Watch the client for decreased immune function. Monitor the client's throat and mouth for aphthous lesions (cold sores). Monitor for hyperglycemia. Omalizumab can cause anaphylaxis. Nontunneled percutaneous central catheter: Insertionlocation-subclavianvein,jugularvein;tipinthe distal third of the superior venacava Description - 15 to 20 cm inlengthwithoneto three lumens Indications -administrationofblood,long-term administration ofchemotherapeutic agents, antibiotics, and total parenteral nutrition Lengthofuse-shortterm use onlyPeripherally inserted centralcatheter Description-40to65 cm with single or multiple lumens Insertionlocation-basilicorcephalicveinatleastone finger's breadth below or above the antecubitalfossa; the cathetershould be advanced until the tip is positioned in the lower one-third of the superior vena cava. Lengthofuse-upto12 months Peripherally inserted central catheter- PICC Indications -administrationofblood,long-term administration ofchemotherapeutic agents, antibiotics, and total parenteral nutrition Tunneled percutaneous central catheter Insertionlocation-Aportionofthecatheterliesina subcutaneous tunnel separating the point where the catheter enters the vein from where it enters the skin with a cuff. For long-termuse. Indications-Frequent and long-termneedfor vascular access Tissue granulatesintothecufftoprovideamechanicalbarrierto organisms and an anchoring for the catheter. Implantedport:a1year or more. Description - Port is comprised of a small reservoircoveredbya thickseptum. Indications - Long-term (ayear or more) need forvascular access; commonly used for chemotherapy.Abone marrow Biopsyiscommonlyperformedtodiagnosecausesof blood disorders, suchas anemia or thrombocytopenia, orto rule-outdiseases, such as leukemia and other cancers, and infection Apply local anesthetic to skin if indicated. Palpateskintolocate the portbodyseptum to ensure proper insertion oftheneedle Cleantheskinwithalcoholforatleast3. Apply local anesthetic to skin if indicated. Palpateskintolocatetheportbodyseptum to ensureproperinsertionoftheneedle. secondsandallowtodrypriortoinsertionof the needle. Access with a noncoring (Huber) needle. Occlusionisablockage in the access device that impedesflow. Nursing Actions Flushthelineatleastevery12hr(3mLforperipheral,10 mLfor central lines) to maintain patency Infiltrationand Extravasation Infiltration is fluid leaking into surrounding subcutaneous tissue, andextravasation is unintentional infiltration of a vesicant medication that causes tissue damageA bonemarrow Intra Pre Administer sedativemedication. Ensure that the client has signed the informed consent form. Assist with theprocedure. Apply pressure to the biopsy site. Positiontheclientina prone or side-lying position. Place a sterile dressing over the biopsy site. A bone marrow - Post Potential Complications: Monitorforevidenceof infectionandbleeding. Bleeding and infection Applyicetothebiopsy site. Administer mild analgesics; avoid aspirin or medications that affect clotting Client Education:A bone marrow: Explain the procedure to be performed: use of local anesthesia, sensation of pressureor brief pain. Reportexcessive bleedingandevidenceofinfectionto the provider. Checkthebiopsysitedaily.Itshouldbeclean,dryand intact. If there are sutures, return in 7 to 10 days for removal.Repaglinide should not be taken just before bedtime; Repaglinide causes a rapid, short-lived release of insulin. The client should take this medication within 30 min before each mealso thatinsulin is available when food is digested Repaglinide is not taken upon awakening in the morning Pramlintide delaysoral Pramlintideshouldnotbemixedinasyringewithanytype medication absorption, of insulin so oralmedications should be taken 1 to 2 hr after pramlintide injection Pramlintidecancause hypoglycemia, especially when the clientalsotakesinsulin, so it is important to eat a mealafterinjectingthis medication. Insulinlispro Insulinlisprohasapeakeffectaround30minto2.5hr following administration Regular insulin Regularinsulinhasapeakeffectaround1to5hrfollowing administration NPH NPHinsulinhasapeakeffectaround6to14hrfollowing administration. Insulinglargine Insulin glargine, a long-acting insulin, does not have a peak effect time, but is fairly stableineffectaftermetabolizedUnused medication in the open pramlintide vial should be discarded after28 day' Unused medication in the open pramlintide vial should be discarded after28 dayExenatide Thenurseshouldmonitordailybloodglucosetestingby the client, periodic HbA1c tests, and periodic kidney function testing. Exenatide should be used cautiously in clients who have any renal impairment. Acarbose can cause liver toxicity when taken longterm. Liver function tests should be monitored periodically while the client takes this medication Exenatide isprescribed Exenatide improves insulin secretion by the pancreas, along with anoral decreases secretion ofglucagon, antidiabetic medication, and slows gastricemptying such as metformin or a sulfonylurea medication, forclients who have type2 diabetes mellitusto improve diabetes control. Exenatide A/E: GI effects, such as nausea and vomiting Hypoglycemia, especially when taken concurrently with a sulfonylurea medication,such as glipizide Pancreatitis manifested by acute abdominal pain and possibly severe vomitingExenatide Teach the client that exenatide should not be given within 1 hr of oral antibiotics, acetaminophen,oranoralcontraceptive duetoitsability to slow gastricemptying Instruct client how to injectexenatide subcutaneously. Adviseclienttowithholdexenatideandnotifytheprovider for severe abdominal pain. Teach the client how to recognize and treat hypoglycemia. Teach client to take exenatide within 60 min beforethemorningand evening meal but not following the meal. Type1diabetesmellitus is an autoimmune dysfunction involving the destructionofbeta cells, which produceinsulininthe islets of Langerhans of the pancreas. Type 1 diabetes mellitus usuallyoccurs at ayoung age, and there are no successfulinterventions to prevent the disease. Immunesystemcells and antibodies are present in circulation and may also be triggered by certain genetic tissue types or viral infections.Diabetic Screening: risk factors - obesity, hypertension, inactivity, hyperlipidemia, cigarette smoking, genetic history, elevated C-reactive protein(CRP), ADA-recommendsscreeningaclientwhohasaBMI greater than 24andagegreaterthan45years,orifachildis overweight and has additional risk factors. ethnic group, and women who have delivered infants weighingmore than 9 lb Rapid-acting diuretics, Morphinedecreasessympatheticnervoussystemresponse such asfurosemide and anxiety andpromotes (Lasix) and bumetanide mild vasodilation. (Bumex), promotefluid excretion. Risk Factors: Obesity, physical inactivity, high triglycerides (greater than 250 mg/dL), and hypertensionmay lead to the development of Pancreatitisand Cushing's syndrome aresecondarycauses of diabetes. insulinresistanceand type 2diabetes.Vision and hearing Tissue deterioration secondary to aging may impact the deficits mayinterfere client's ability to prepare food, with theunderstanding care for of teaching, reading of self, perform ADLs, perform foot/wound care, and materials, perform glucose monitoring. and preparation of medications. Vasodilators (nitroglycerin, sodium nitroprusside)decrease preload and afterload. Inotropic agents, such as digoxin (Lanoxin) and dobutamine (Dobutrex),improvecardiacoutput. Older adult clients may A fixed income may mean that there are limited funds for not be able to drive to buying diabetic supplies, wound care the provider's office, supplies, insulin, and medications. This may result in grocery store, or complications. pharmacy. Assess support systems available for older adult clients. Hyperglycemia -blood olydipsia (excessive thirst) due to dehydration glucose levelusually Loss of skin turgor, skin warm and dry greater than 250 mg/dL. Dry mucous membranes Polyuria (excessurine Weakness and malaise production and Rapid weak pulse and hypotension frequency) from osmotic diuresisPolyphagia (excessive hunger and eating) causedfrominabilityof cellstoreceiveglucose (cells are starving); Client maydisplay weight loss. Metabolic acidosis. KussmaulrespirationsOther: acetone/fruity breath odor; headache, nausea, vomiting, abdominal pain, inability to concentrate, decreased level of consciousness, and seizures leading to coma. Rapid-acting insulin Onset is rapid, 10 to 30 min depending on which insulin is Lispro insulin administered. (Humalog), aspart Administerinconjunctionwithintermediate-orlong-acting insulin (Novolog), insulin to provideglycemic glulisine insulin (Apidra). control between meals and at night. Administer before meals to control postprandial risein blood glucose. Short-acting insulin U-500 is reserved for the client who has insulin resistance Regularinsulin (Humulin and is never administered IV. R, Novolin R). U-100 is prescribed for most clients and may be Administer 30 to 60 min administered IV before meals to control postprandial hyperglycemia. Available in two concentrations.Intermediate-acting Administer NPH insulin subcutaneous only and as the only insulin insulin to mixwith NPH insulin(Humulin short-acting insulin. N), detemirinsulin (Levemir). Administered for glycemic control between meals and at night. Long-acting insulin Glargine insulin forms microprecipitates that dissolves Glargine insulin (Lantus) slowly over 24 hr and maintains a Administered once steady blood sugar level with no peaks or troughs. daily, anytimeduring the day but always at the same time each day. Diabetic neuropathy Monitor blood glucose levels to keep within an acceptable Caused from damage range to slowprogression. to sensory nerve fibers ■ Provide footcare. resulting innumbness and pain. Is progressive,may affect every aspect of the body, and can lead to ischemiaand infection. Diabetic nephropathy Nursing Actions Damage to the kidneys Monitor hydration and kidney function (I&O, serum from prolonged creatinine).elevated blood glucose Report an hourly output of less than 30 mL/hr. levels anddehydrationDKA Reduced or missed dose of insulin (insufficient dosing of Lack of sufficient insulin insulin or error in dosage) related toundiagnosed or untreated type 1 diabetes mellitusor nonadherence to a diabetic regimen Any conditionthat ◻ Increasedhormoneproduction(e.g.,cortisol,glucagon, increases carbohydrate epinephrine) stimulates the liver to metabolism, suchas produce glucose and decreases the effect of insulin. physical oremotional stress, illness, infection (No. 1 cause of DKA), surgery, or trauma that requires an increased need for insulin Hypothyroidism Theolderadultisatrisk for alteredmetabolism of medication due to decreased kidney and liver functionbecauseofthe aging process. Condition in which there is an inadequate amount of circulating thyroidhormones triiodothyronine (T3) and thyroxine (T4), causing a decrease in metabolic rate that affects all body systems. The older adult may have visional alterations; yellowing of lens, decreased depth perception, cataracts, whichcanaffectabilitytoreadinformationandattendto medication administration.Hypothyroidism isalso classified by age of onset. Cretinism-Cretinismisastateofseverehypothyroidism found in infants. When infants do not produce normal amounts of thyroid hormones, central nervous system developmentand skeletal maturation are altered, resulting in retardation ofcognitive development, physicalgrowth, orboth. Juvenile hypothyroidism Adult hypothyroidism: - Juvenile Because olderadult clients who have hypothyroidism may hypothyroidism is most have manifestations that mimic the aging often caused by chronic process, hypothyroidism is often undiagnosed in older autoimmune adult clients, which can lead to potentially thyroiditis andaffects serious adverse effects from medications (sedatives, the growth and sexual opiates, anesthetics) maturation of the child. Clinical manifestations are similar toadult hypothyroidism, and the treatment reverses most of the clinical manifestations of the disease.Laboratory Tests - Theexpected referencerangefor T3is70to205ng/dL,andtheexpected referencerangeforT4is4to12mcg/dL.) Hypothyroidism - S/S: Early findings Early findings; Fatigue, lethargy, irritabilily Fatigue, lethargy, Intolerance to cold irritabilily Constipation Intolerance to cold Weight gain without an increase in caloric intake Constipation ; Pale skin Weight gain without an Thin, brittle fingernails increase; incaloric Depression intake; Thinning hair Pale skin; Joint and/or muscle pain Thin, brittle fingernails; Depression; Thinning hair; Joint and/ormuscle pain; Hypothyroidism: - Late Dry, flaky skin; findings: Swelling in face, hands, and feet(myxedema[non-pitting, Bradycardia, mucinous edema]); hypotension, Decreased acuity of taste and smell; dysrhythmias; Hoarse, raspy speech; Slow thoughtprocess Abnormalmenstrualperiods(menorrhagia/amenorrhea) and speech; and decreased libido; Hypoventilation, pleural effusion Thickening of the skin; Thinning of hair on the eyebrows;Radioactiveiodine(131 I) is administered orally 24 hrpriortoathyroid scan. The thyroid absorbs theradiation, which resultsin destruction ofcells that produce thyroidhormone Client Education: Do not use same toilet as others for 2 weeks, sit down to Advise the client that urinate, and flush toilet three times. the effects ofthe Take a laxative 2 to 3 days after treatment to rid the body therapy may not be of stool contaminated with evident for 6 to 8 radiation. weeks. Advise the client to take medication asdirected. Advise female clients to avoid becoming pregnant for 6 months. Wear clothing that is washable, washclothing separate from clothing of others, and run the washingmachinefora full cycleafterwashing contaminated clothing. Advisetheclienttoavoidinfantsorsmallchildrenfor2to 4 days afterthe procedure. Avoid contamination from saliva, do not share a toothbrush, and use disposable food service items (paperplates).Teach the client that thyroid replacement therapy is usually lifelong. - Therapeutic Use Levothyroxine replaces T4 andisusedasthyroid hormone replacement therapy. Replacement of T4alsoraisesT3levels, because some T4 is converted intoT3. Nursing Care: Adverseeffectsinclude cardiac effects, chest pain, hypertension,and palpitations, especially in older adults Teach theclienttotake levothyroxine on an empty stomach,usually 1 hrbefore breakfast. Adverse effectsareessentiallythesame as manifestations of hyperthyroidism: cardiac symptoms, suchashypertensionandanginapectoris;insomnia, anxiety; weightloss;heatintolerance; increasedbodytemperature;tremors;andmenstrual irregularities Thenurseshouldmonitorthyroidfunctiontests:T3,T4,and TSH Teachtheclient thatthyroid replacement therapyis usually lifelong. Monitorforadverseeffectsthatindicatethatthedosage needs to bereduced.TPN provides a nutritionally complete solution.Itcanbeused whencaloricneedsare very high, when the anticipated duration of therapy is greaterthan7days,or when thesolutiontobe administered is hypertonic (composed of greater than 10% dextrose). PPN can provide a nutritionally complete solution. However, it is administered into a peripheral vein,resultinginalimitednutritionalvalue.Itisindicated forclients who require short-term nutritional support with fewercalories per day. The solution must be isotonic and contain no more than10%dextrose and5%aminoacids Itcanonlybe administered in a central vein. Identify three complicationsofTPN Related Content 1 - Infection and sepsis Monitor for manifestations of fever, chills, increased WBCs, and redness around catheterinsertionsite. 2 - Hyperglycemia 3 - Hypoglycemia Administer slidingscale insulin or planforinsulintobe added tothe TPN solution. Informtheproviderandplantogive additional dextrose. Monitor frequent blood glucose. Monitor blood glucoseDiagnostic Procedures LaboratoryTests: Cerebrospinalfluidanalysis. DiagnosticProcedures:MRIofthebrainandspine MS is an autoimmune Plaque damages the disorder characterized myelin sheath and interferes with impulse transmission by the between the CNS and the body. development ofplaque in the white matter of the centralnervous system. Medication-MS Immunosuppressive agents such as azathioprine (Imuran) and cyclosporine (Sandimmune) - Long-term effects include increased risk forinfection, hypertension, and kidneydysfunction. Corticosteroids suchas Antispasmodicssuchasdantrolene(Dantrium),tizanidine prednisone -Increased (Zanaflex), baclofen (Lioresal)and risk forinfection, diazepam (Valium) are used to treat muscle spasticity. hypervolemia, hypernatremia, hypokalemia, GI Hypoglycemia - S/S Weight gain greater than 1 kg/day Inform the provider and anticipate adecreaseintheconcentration, rate of administration or volume of lipid emulsion. Monitortheclient'sintakeof oral nutrientsCorticosteroids such as prednisone Report increased weakness and jaundice to provider.Avoidstoppingbaclofenabruptly. bleeding, and personality changes.Beta-blockerssuchas primidone (Mysoline) and clonazepam (Klonopin)areusedfor tremors ... Immunomodulators Anticonvulsants such as carbamazepine (Tegretol) are such as interferon beta used for paresthesia. (Betaseron) are used to prevent and treat relapses Stool softeners such as Anticholinergics such as propantheline are used for docusate sodium bladder dysfunction. (Colace) are usedfor constipation Amyotrophic lateral This results in sclerosis (ALS) is a progressive paralysis and muscle wasting that eventually degenerative causes respiratory paralysis and death. neurological disorderof Cognitive function is not usually affected the upper and lower motor neuronsthat results indeterioration and death of the motor neurons. Death usuallyoccurs Physical AssessmentFindings: due to respiratory Muscle weakness - usually begins in one part of the body failure within 3 to 5 Muscle atrophy; years of the initial Dysphagia ;manifestations. The Dysarthria; cause of ALS is Hyperreflexia of deep tendon reflexes; unknown, and there is no cure.Laboratory Tests - Increased creatine kinase (CK-BB) level Musclebiopsy-Reductioninnumberofmotorunitsof peripheral nerves and atrophic muscle fibers Diagnostic Procedures Electromyogram (EMG) - Reduction in number of functioning motor units of peripheral nerves ALS - Medication : Riluzole (Rilutek) is a glutamate antagonist that can slow the deterioration of motor neurons by decreasing the release of glutamicacid Baclofen (Lioresal), dantrolene sodium (Dantrium), diazepam (Valium) ■ Antispasmodics are used to decrease spasticity. Complications: ALS: Nursing Actions - Assess respiratory status routinely and Pneumonia canbe administer antimicrobialtherapy caused byrespiratory as indicated. muscle weaknessand paralysis contributingto ineffective airway exchange. Complications: ALS: Respiratoryfailure may necessitate mechanical ventilation. Nursing Considerations: Monitorliverfunctiontests-hepatotoxicrisk. Assess fordizziness, vertigo, and somnolence.Nur sing Acti ons - Asse ss resp irato ry stat us and be pre pare d to pro vide vent ilato ry sup port as nee ded per the clie nt's adv anc e dire ctiv es.Myasthenia gravis (MG) It is characterized by periods of exacerbation and is aprogressive remission. Muscle weakness improves with rest and autoimmune disease worsens with increasedactivity. that producessevere muscular weakness. Myastheniagravis(MG) Itis caused by antibodies that interfere with the transmission of acetylcholine at the neuromuscular junction Assessment: Myasthenia Subjective Data: gravis Progressive muscle weakness; Risk factorsassociated Diplopia; with rheumatoid Difficulty chewing and swallowing; arthritis, scleroderma, Respiratory dysfunction; and systemiclupus Bowel and bladder dysfunction; erythematosus Poor posture; Fatigue after exertion Objective Data: PhysicalAssessment Findings; Impaired respiratory status (difficulty managing secretions, decreased respiratory effort); Decreased swallowing ability Decreased muscle strength, especiallyofthe face, eyes, and proximalportion ofmajormuscle groups Incontinence Drooping eyelids - unilateral or bilateralTensilon testing: Baseline assessmentof the cranial muscle strength isdone. Medication inhibits the breakdown of acetylcholine, making it available for use at the neuromuscularjunction. Edrophonium (Tensilon) is administered MG - Atropine Haveatropineavailable,whichistheantidotefor edrophonium (bradycardia,sweating, and abdominal cramps). Therapeutic Procedures This is usually done several times Plasmapheresis over a period of days and may continue on a regular basis removes circulating for some clients. antibodies from the plasma. Monitor for the possible ■ ClientEducation-Instructtheclientthattheprocedure complications of will typically last 2 to 5 hr. hypovolemia, hypokalemia, and hypocalcemia. Electromyography Shows the neuromuscular transmission characteristics ofMG. Surgical Interventions Thymectomy - removal of the thymus glandisdonetoattainbettercontrolorcomplete remission. Maytakemonthstoyearstoseeresultsduetothelifeof the circulating Tcells.Decrease in amplitude of the muscle is demonstrated over a series ofconsecutive muscle contractionsComplications: The manifestations of both can be very similar (muscle weakness, respiratoryfailure). The client's highest risk forinjury is due to respiratory compromise and failure. Complications: MG, such as infection, or is taking inadequate amounts of ● Myasthenic crisisand cholinesterase inhibitor. cholinergic crisis; Cholinergic crisis occurs when the client has taken too Myasthenic crisis occurs much cholinesterase inhibitor. when the client is experiencing astressor that causesan exacerbation of MYASTHENIC CRISIS Undermedication: Respiratory muscle weakness - mechanical ventilation Myasthenic findings (weakness, incontinence, fatigue) › Hypertension; › Temporary decrease of findings with administration ofTensilon; CHOLINERGIC CRISIS: Cholinergic manifestations - hypersecretions (nausea, Overmedication diarrhea, Muscle twitching to the respiratory secretions) and hypermotility (abdominal point ofrespiratory cramps) muscle weaknessmechanical ventilation › Cholinergic manifestations - hypersecretions (nausea, diarrhea,respiratory secretions) and hypermotility (abdominal cramps)Hypotension › Manifestations decrease with the administration of an › Tensilon has no anticholinergic positive effect on medication, such asatropine. manifestations, and can actually worsen findings (more anticholinesterase - more cholinergic manifestations). MIXED CRISIS: › Manifestations include dyspnea, dysphagia, dysarthria, › Clients may restlessness, apprehension, salivation, and lacrimation. experience mixedcrisis when myasthenic crisis is overtreated with anticholinesterase drugs. Provide small,frequent, Have the client sit upright when eating, and use thickener high-calorie mealsand in liquids asnecessary. schedule at times when medication ispeaking. MS - Nursing Care: Use energy conservation measures. Allow for periods of Assess and intervene as rest. needed to maintain a Assess swallowing to prevent aspiration. Keep oxygen, patent airway (muscle endotracheal intubation,suctioning weakness of diaphragm, equipment, and a bag valve mask available at the client's respiratory, and bedside. intercostal muscles).Apply a lubricating eye Encourage the client to wear a medical identification drop during theday wristband or necklace at all times. and ointment at night if Administer medications as prescribed and at specified the client is unable to times completely closehis eyes. The client may also need to patch or tape his eyes shut at night to prevent damage to the cornea. Leukopenia is a total Leukocytosis- WBC count ofgreaterthan 10,000/mm3. It WBC count of less than may indicate an inflammatory 4,500/mm3. It may response to a pathogen or a disease process indicate acompromised inflammatory response or viralinfection. Neutropenia isa A client who has neutropenia is at an increased risk for neutrophil count of less infection. than 2,000/mm3. Neutropenia occursin clients who are immunocompromised, are undergoing chemotherapy, orhave a process that reduces the production ofneutrophils.During the test, various Ifanallergenisnotattracted,thisisconsideredanegative radiolabeled allergens result. If a client's IgE is attracted to an allergen, the are exposed tothe amount is measure on a scale of 0 to 5, with client's blood, and the thehighernumberindicatingahigherlevelfrom sensitivity. amount of the client's immunoglobulin E (IgE) that is attracted to each specific allergen is measured according to standardized values. AIDS - Nursing Care: ◯ Assess skin integrity (rashes, open areas, bruising). ◯ Assess the client's pain status. ◯ Monitor vital signs (especially temperature). ◯Assesslungsounds/respiratorystatus(diminishedlung sounds). ◯Assessneurologicalstatus(confusion,dementia,visual changes). Assess riskfactors (sexual practices,IV drug use). ◯ Monitorfluid intake/urinary output. ◯ Obtain daily weights to monitor weight loss. ◯ Monitornutritional intake. ◯ Monitorelectrolytes. Systemic lupus In autoimmune disorders, small antigens may bond with erythematosus (SLE) is healthy tissue. The body then produces an autoimmune disorder antibodies that attack the healthy tissue. This may be in which an atypical triggered by toxins, medications, bacteria, immune and/or viruses.response results in chronic inflammation and destruction of healthy tissue.Subjective Data:SLE Butterfly Rash › ◯ Fatigue/malaise ◯ Alopecia ◯ Blurred vision ◯ Malaise ◯ Pleuritic pain ◯ Anorexia/weightloss ◯ Depression ◯ Joint pain, swelling, Raynaud's Syndrome tenderness Objective Data - SLE ■ Fever(alsoamajor symptom of exacerbation) ■ Anemia ■ Lymphadenopathy ■ Pericarditis(presence ofa cardiac friction rub or pleuralfrictionrub) ■ Raynaud'sphenomenon(arteriolarvasospasmin response tocold/stress) ■ Findingsconsistentwithorganinvolvement(kidney, heart, lungs, and vasculature) ■ Butterfly rash onface Systemic manifestations ◻ Rubor, pallor, and cyanosis of hands/feet ◻ Hypertension and (vasculitis/vasospasm, Raynaud'sphenomenon) edema (renal ◻ Arthralgias, myalgias, and polyarthritis (joint and compromise) connective tissue involvement) ◻ Urine output(renal ◻ Changesinmentalstatusthatindicateneurologic compromise) involvement (psychoses, paresis, seizures) ◻ Diminished breath ◻ BUN,serumcreatinine,andurinaryoutputforrenalsounds (pleural involvement effusion) ◻ Tachycardiaand sharp inspiratorychest pain (pericarditis)Objective Data - SLE ◯ PhysicalAssessment Findings Anemia Lymphadenopathy Raynaud's phenomenon (arteriolar Fever (also a major vasospasm in response to cold/stress) manifestation Findings consistent with organ of exacerbation) involvement (kidney, heart,lungs Pericarditis (cardiacor and vasculature) pleural friction Butterfly rash onface rub may be present) Medications: ◯ NSAIDs Nursing Considerations - Monitor forfluid retention, hypertension, and renaldysfunction. ◯ Corticosteroids (prednisone ■ ClientEducation-Donotstoptakingsteroidsor decrease the doseabruptly. [Deltasone]) ■ Immunosuppressant ◯Immunosuppressantagents-methotrexateand azathioprine (Imuran) agents -methotrexate and azathioprine (Imuran) ■◯ ClientEducation: ■ Avoid UVand sun Avoid crowds and individuals who are sick, because illness can precipitate anexacerbation. exposure. ■ Use mildprotein ■ Educateclientofchildbearingageregardingrisksof shampoo and avoid pregnancywith lupus and harsh hair treatments. treatment medications. ■ Use steroidcreams for skinrash. ■ Reportperipheral and periorbitaledema promptly / signs of infection related to immunosuppression. Rheumatoid arthritis- The inflammation can extend to the cartilage, RA is an autoimmune bone,tendons,andligamentsthatsurroundthejoint.Joint disease that is deformity and bone erosion may result precipitated by WBCs fromthesechanges,decreasingthejoint'srangeofmotion attacking synovial and function. tissue. The WBCs cause the synovial tissue to become inflamedand thickened. Chemotherapy : They interfere with the life Pathophysiology ofthe cycle of rapidly proliferating cells, such as those found in Problem; hair follicles, resulting in hair loss Alopecia occurs as an adverse effect ofchemotherapy medications.S/S Pain at rest and with ● Objective Data movement ◯ Morningstiffness ◯ Pleuritic pain (pain ◯ Joint swelling and deformity ■ Jointswelling,warmth,and erythema. ■ Finger,hands,wrists,knees,andfootjointsaregenerally upon inspiration) affected. ◯ Xerostomia(dry interphalangeal and metacarpophalangeal joints. mouth) ■ Jointsmaybecomedeformed merelybycompleting ◯ Anorexia/weightloss ◯ Fatigue ◯ Paresthesias ◯ Recent ADLs. ■ Ulnardeviation,swanneck,andboutonnièredeformities are common in the fingers. illness/stressor ◯ Joint pain ◯ Lack of function Client Education: Use a soft hair brush or wide-tooth comb for grooming. Wearhats,turbans,and wigs. Avoid the use of damaging hair-care measures, such as electric rollers and curlingirons,hairdye, andpermanentwaves. Avoidsunexposure.Useadiaperrashointmentorcream for itching. Alopecia is temporary, and hair will return when chemotherapy isdiscontinued Corticosteroids They are not given for long-term therapy (prednisone) arestrong due to significant adverse effects (osteoporosis, anti-inflammatory hyperglycemia, immunosuppression,cataracts). medications thatmaybe given for acute exacerbationsor advanced forms of the disease.Nursing Care: ◯Apply heat orcold to the affectedareasas Monitor the client for indications of fatigue. ◯ Teach the client measures to ■ Maximize functionalactivity indicated based on ■ Minimize pain client response. ■ Monitor skinclosely ■ Morningstiffness(hot ■ Conserveenergy(spaceoutactivities,takerestperiods, shower) ask for additional assistance ■ Pain inhands/fingers when needed) (heated paraffin) ■ Promote copingstrategies ■ Edema (coldtherapy) ■ Encourage routinehealthscreenings Disease modifying anti- Relief of symptoms may not occur rheumatic drugs for severalweeks. (DMARDs) ■ Antimalarialagent-hydroxychloroquine(Plaquenil) ■ DMARDs workin a ■ Antibiotic - minocycline(Minocin) variety of ways to slow ■ Sulfonamide - sulfasalazine (Azulfidine) the progression ofRA and suppress the immune system's reaction to RA that causes pain and inflammation Sjögren's syndrome NSG CARE: (triad of symptoms - dry eyes, dry mouth, and Provide the client with eye drops and artificial saliva, and dry vagina) ◯ Caused by obstruction ofsecretory recommendvaginallubricants as needed. ■ Provide fluids withmeals. ducts and glands■Plasmapheresis: Total joint arthroplasty - RA ■ Removescirculating ■ Surgicalrepairandreplacementofajointmaybedone antibodies from plasma, for a severely deformed joint that has decreasing attackson not responded to medication therapy. the client'stissues ◯ May be done for a severe, life-threatening exacerbation Nursing Interventions: Discuss the impact of alopecia on self-image. Encouragetheclientto express feelings. ... Recommend use of information from the American Cancer Society on managing alopecia. Provide referral to a cancer support group. Nausea and vomiting/anorexia ■ Many of the medications used for chemotherapy are emetogenic (induce vomiting) orcause anorexia as well as an altered taste in the mouth. ■ Serotoninblockers,suchasondansetron(Zofran),have been found to be effective and are often administeredwithcorticosteroids, phenothiazines,and antihistamines. ■ Nursing Actions ◻ Administerantiemeticmedicationsattimesthatare appropriateforachemotherapeutic agent (prior to treatment, during treatment, after treatment). ◻Administer antiemetic medication s forseveral days after each treatment as needed. ◻ Remove vomiting cues, such as odor and suppliesassociated with nausea. ◻ Implement nonpharmacological methods to reduce nausea (visual imagery, relaxation, acupuncture, distraction). ◻ Perform calorie counts to determine intake. Provide liquid nutritional supplementsas needed. Add protein powders to food or tube feedings. ◻ Administer megestrol (Megace) to increase the appetite if prescribed. ◻ Assess for findings of dehydration or fluid and electrolyte imbalance. ◻ Perform mouth care prior to serving meals to enhance the client's appetite Encourage the use of plastic eating utensils, sucking on hard candy, and avoiding red meats to prevent or reduce the sensation of metallic tasteInstruct the client to Alopecia is an adverse effect of certain chemotherapeutic avoid the useof medications related to their interference damaging hair-care with the life cycle of rapidly proliferating cells. measures, suchas ■ electric rollers Nursing Actions and curling irons, hair ◻ dye, andpermanent Discuss the impact of alopecia on self-image. Discuss waves. Use of a soft hair options such as hats, turbans, and wigs brush orwide-tooth to deal with hair loss. comb for grooming is ◻ preferred. Recommend soliciting information from the American ◻ Cancer Society regarding products Suggest that the client for clients experiencing alopecia. cut her hair short before ◻ treatment todecrease Inform client that hair loss occurs 7 to 10 days after weight on the hair treatment begins (select agents). follicle. Encourage client to select hairpiece before treatment ◻ starts. After hair loss, the client ◻ should protect the Reinforce that alopecia is temporary, and hair should scalp from sun return when chemotherapy exposure and usea is discontinued diaper rash ointment/cream for itching. ... Mucositis (stomatitis) is inflammation of tissues in the mouth, such as the gums, tongue, roofand floor of the mouth, and inside the lips and cheeks. ■N u rs i n g A ct io n s ◻ E x a m i n e t h e cl ie n t' s m o u t h s e v eral times a day, and inquire about the presence of oral lesions.◻ Documentthelocationandsizeoflesionsthatarepresent. Lesions should be cultured and reported to theprovider. ◻ Avoid using glycerin-based mouthwashes ormouth swabs. Nonalcoholic, anesthetic mouthwashes are recommended. ◻ Administer a topical anesthetic prior to meals. ◻ Discourage consumption of salty, acidic, or spicy foods. ◻ Offer oral hygiene before and after each meal. Use lubricating or moisturizing agents to counteract drymouth. ■ Client Education ◻ Encourage the client to rinse mouth with a solution of half 0.9% sodium chloride and half peroxide at least twice a day, and to brush teeth using a soft-bristled toothbrush. ◻ Instruct client to take medications to control infection as prescribed (nystatin [Mycostatin], acyclovir [Zovirax]). ◻ Encourage the client to eat soft, bland foods and supplements that are high in calories(mashed potatoes, scrambled eggs, cooked cereal, milk shakes, ice cream, frozen yogurt, bananas, and breakfast mixes)... Anemia and thrombocytopenia occur secondary to bone marrow suppression (myelosuppression). ■ Nursing Actions for Anemia ◻ Monitor for fatigue, pallor, dizziness, and shortness of breath. ◻ Help the client manage anemia-related fatigue by scheduling activities with rest periods in betweenandusingenergysavingmeasures(sittingduring showers and ADLs). ◻ Administererythropoietic medications such as epoetin alfa (Epogen) and antianemic medications such as ferrous sulfate (Feosol) as prescribed. ◻ MonitorHgb values to determine response to medications. Be prepared to administer blood if prescribed. ... Nursing Actions for Thrombocytopenia ◻ Monitor for petechiae, ecchymosis, bleeding of the gums, nosebleeds, and occult orfrank bloodinstools, urine,orvomitus. ◻ Institutebleeding precautions(avoidIVsandinjections, apply pressure forapproximately 10 min after blood is obtained, handle client gently and avoid trauma).◻ A d m i n i s t e r t h r o m b o p o i e t i c m e d i c a t i o ns such as oprelvekin (Interleukin 11,Neumega) to stimulate platelet production. Monitor platelet count,Pacemaker Fixed rate (asynchronous) - Fires at a constant rate without regard for the heart's electrical activity. and be prepared to administer platelets if the count falls below 30,000/mm 3 . ■ Client Education ◻ Instruct the client and family how to manage active bleeding. ◻ Instructthe client aboutmeasures to prevent bleeding (use electric razor andsoft-bristled toothbrush, avoid blowing nose vigorously, ensure that dentures fit appropriately). ◻ Instruct the client to avoid the use of NSAIDs. ◻ Teach the client to prevent injury when ambulating (wear closed-toes shoes, remove tripping hazards in the home) and apply cold if injury occursDemand mode (synchronous)-Detects the heart's electrical impulses andfiresata preset rate only iftheheart'sintrinsic rate isbelowacertain level. Pacemaker response modes include the following: Pacemakeractivityis **inhibited/does not fire. Pacemakeractivityis **triggered/fires when intrinsic activity is sensed. Can overpace a **tachydysrhythmia and/or deliver an electrical shock. Permanent pacemaker:Incision using a local anesthetic and IV sedation. The pacemaker battery will last about 10 years. The pacemaker pulse generator must be replaced when this occurs. The pacemaker may be reprogrammed externally after procedure. POST-OP: Makesureallequipmentisgroundedwithathree-pronged plug. Maintaintheclient's safety. Wear gloves when handling pacemaker leads. Ensure that allelectrical equipment has grounded connections. Remove any electrical equipment that is damaged.Foratemporary pacemaker Unattached pacemaker wires can cause cardiac arrhythmiasorventricularfibrillation, even when not attached to pacemaker generator. Secure thepacemaker Provide the client with a pacemaker identification card battery pack. Take care including the manufacturer's when moving the client, name, modelnumber, mode of function, rate parameters, and ensure that and expected batterylife. there is enough wire slack. ◻ For apermanent pacemaker Insulate pacemaker terminals andleads with nonconductive material when not in use (rubber gloves). Keep spare generator, leads, and batteries at the client's bedside. Permanentpacemaker discharge teaching Carry a pacemaker identification card at all times. Permanentpacemaker teaching:Permanent pacemaker teaching: Take pulse daily at the same time. Notifytheproviderifheartrateislessthanfivebeats below the pacemaker rate. Prevent wire dislodgement (wear sling whenoutofbed, donot raisearmabove shoulder for 1 to 2 weeks). Permanent pacemaker teaching: Report signs of dizziness, fainting, fatigue, weakness, chest pain, hiccupping, or palpitations. For clients with pacemaker-defibrillators, when the device delivers a shock, anyone touching theclientwillfeelaslightelectricalimpulse,butthe impulse will not harm the person. Permanent pacemaker teaching: Avoid direct blows or injury to the generator site. Resumesexual activityasdesired,avoidingpositionsthat put stress on the incision site. Follow activity restrictions as prescribed, including no contact sports or heavy liftingfor 2 months. Permanent pacemaker teaching: Never place items that generate a magnetic fielddirectlyoverthe pacemakergenerator.These items can affect function and settings. This includes garage door openers, burglar alarms , strong magne ts, genera tors and other power trans mitter s,and large stereo speak ers.Permanent pacemaker teaching: Inform other providers anddentistsaboutthe pacemaker. Some tests, such as magnetic resonance imagingand therapeutic diathermy (heattherapy), maybe contraindicated. Pacemakers will set off airport security detectors, and officials should be notified. The airport security device should not affect pacemaker functioning. Airport security personnel should notplacewanddetectiondevicesdirectlyoverthe pacemaker. Macular degeneration, Risk Factors: often called age- Dry macular degeneration: Female related macular Short body stature degeneration (AMD),is Diet lacking carotene and vitamin A the central loss of vision that affects the macula of the eye. There is nocure Loss of central vision: Blindness: Anophthalmoscopeisusedtoexaminethebackpartof the eyeball (fundus), including the retina, optic disc, macula, and blood vessels. Consume foods high in antioxidants, carotene, vitamin E, and B12. Provider may prescribe dailysupplement highin carotene + vitamin E.Acataractisanopacity in the lens of an eye that impairsvision. Therearethreetypesof cataracts: CataractsTeach clients to wear sunglasses while outside. Assessment: Decreased visual acuity (prescription changes, reduced night vision) A subcapsular cataract - back of the lens. A nuclear cataract - center (nucleus) of the lens. Acorticalcataract-lenscortexandextendsfromthe outside of the lens to the center. Educate clients to wear protective eyewear while performing hazardous activities, such as welding and yard work. Encourage annual eye examinations and good eye health, in adults > 40 yr. Blurred vision; Diplopia - doublevision Glareandlightsensitivity-photosensitivity; Halo aroundlights Cycloplegic mydriatic (Atropine 1% ophthalmic solution) This medication prevents pupil constriction forprolonged periods of time and relaxes muscles in theeye. Dilatestheeyepreoperativelyandforvisualizationofthe eye's internal structures.Surgical Interventions: Surgical removal of the lens; The posterior capsule is retained. A replacement; or intraocular lens is inserted. Asmallincision is made, and the lens is either removed in one piece, or in several pieces, after being broken up using soundwaves. Replacement lenses can correct refractive errors, resulting in improved vision. Postoperative-Client Education: Wear sunglasses while outsideorinbrightlylit areas. Reportsignsof infection: Clientshouldreportincludeyelloworgreendrainage, increased redness or pain, reduction invisualacuity, increased tearproduction, and photophobia. Avoid activities that Head hyperflexion; increase IOP. Restrictive clothing, such as tight shirt collars; Bending over at the Sexual intercourse waist Sneezing; Coughing; Straining; Limit activities. Avoid rapid, jerky movements, such as vacuuming. Avoid tilting the head Avoid driving and operating machinery. back to wash hair. Avoid sports. Limit cookingandhousekeeping.Open-angle glaucoma ■ Headache ■ Mild eyepain ■ Lossofperipheral vision ■ Decreased accommodation ■ Elevated IOP (greater than 21 mmHg) ... Complications: Infection; Client Education Clients should immediately report any sudden change in visual acuityoran increase in pain. Bleeding: Bleedingisapotential risk several days following surgery. Open-angle glaucoma- The aqueous humor outflow is decreased due to most common form of blockages in the eye's drainage glaucoma. Open-angle system (Canal of Schlemm and trabecular meshwork), refers to theangle causing a rise in IOP. between the iris and sclera. Angle-closure IOP rises suddenly. With angle-closure glaucoma - less glaucoma, the angle between the iris and the sclera common form of suddenly closes, causing a corresponding glaucoma. increase in IOP.Angle-closure glaucoma ■ Rapidonsetof elevatedIOP; ■ Decreasedorblurred vision; ■ Seeing halosaround lights; Pupils are nonreactive to light ■ Severe pain andnausea; ■ Photophobia; ■ Medications Prescribed eye medication is beneficial if used every 12 hr. The priority intervention Instill one drop in each eye twice daily. for treating glaucoma is Wait10to15mininbetweeneyedropsifmorethanoneis drug therapy. prescribed by theprovider. Client teachingshould include the following: Avoid touching the tip ■ Once eyedropis instilled, applypressureusingthe of the application punctal occlusion technique (placing bottle to theeye. pressure on the inner corner of the eye). ■ Always washhands before and after use. Pilocarpine (Isopto Carpine - ophthalmic solution) Prednisolone acetate (Pred Forte Pilocarpine is a miotic, which constricts the pupil and allows forbettercirculation of the aqueous humor. Miotics can cause blurred vision. ophthalmic solution) ■ Prednisoloneacetateisanocularsteroidusedto decrease inflammation. Timolol (Timoptic- Beta-blockers (timolol) and carbonic anhydrase inhibitorsophthalmic solution) (acetazolamide) decrease IOPby and acetazolamide reducing aqueous humor production. (Diamox - oral medication)... Nursing Considerations ◻ Always ask clients whether they are allergic to sulfa. Acetazolamide is a sulfa-based medication IVmannitol(Osmitrol) ■ IVmannitolisan osmotic Acetazolamide (Diamox - oralmedication) Diuretic used in the emergency treatment forangle- closure glaucoma to quickly decreaseIOP. Acetazolamide is administered preoperatively to reduce IOP, to dilate pupils, and to create eye paralysis to prevent lens movement. Gonioscopy Laser trabeculectomy, ◻ Gonioscopy isused iridotomy, or the placement of a shunt are procedures to determine the used to improve drainage angle of the the flow of the aqueous humor by opening a channel out anterior chamber of the of the anterior chamber of the eye. eyes. Diagnostic Procedures Tonometry ■ Visualassessments Toetry is used to measure IOP. ◻ Decrease invisual IOP, expected reference range is 10 to 21 mm Hg) is acuity andperipheral elevated with glaucoma w/ angle-closure. vision Laser trabeculectomy - Clients should report if any changes occur, such as lid Post OP swelling, decreased vision, bleeding or Clients should not lie on discharge, a sharp, sudden pain in the eye and/or flashes the operative side and of light or floating shapes. should reportsevere pain ornausea , possible hemorrhage.Limit activities. Avoidtiltingheadback to washhair. Limit cookingand housekeeping. Avoid rapid, jerky movements, such as vacuuming. Avoid driving and operating machinery. Avoid sports. Report pain withnausea/vomiting -indications of increased IOPorhemorrhage. ◻ Finalbestvisionisnotexpecteduntil4to6weeksafter surgery Blindness is a potential consequence of undiagnosed and untreatedglaucoma. Care after Discharge: Setupservicessuchascommunityoutreach programs, meals on wheels, and servicesforthe blind. Encourage adults 40 or older to have an annual examination, including a measurementofIOP. Retinal Detachment : Blurred vision worsening as detachment increases. Painlesschangeinvision(floaterscausedbybloodcellsin the vitreous and flashes oflight as the vitreous humorpulls on theretina). Photopsia ( recurrent flashes of light). With progression ofdetachment, painless vision loss that may be described as veil, curtain or cobweb that eliminates part of the visualfield.Cervical Tongs Blood donation: universal donorand universal recipient? Profile of the patient with polycythemia Vera:natureof thecondition, how the patient appears? Cervicaltongsareappliedafterdrillingholesintheclient's skull under local anesthesia. Weights are attached to the tongs, which exertpulling pressure onthelongitudinalaxisofthecervicalspine. Serialx-raysofthe cervicalspine aretaken, with weights being addedgraduallyuntilthex-rayrevealsthatthe vertebralcolumn is realigned. Afterthat,weightsmaybereducedgraduallytoapoint that maintainsalignment. TheclientwithcervicaltongsisplacedonaStrykerframe or RotoRestbed. Thenurseensures thatweightshangfreely,and the amountof weightmatches thecurrentprescription. Thenursealsoinspectstheintegrityandpositionofthe ropesand pulleys.Thenursedoesnotremovetheweights to administercare. -O negative universal donor. -AB universal recipient. Bone marrow abnormality, excessive production of RBC, WBC and platelets Looks erythemic. Characteristics ofthe patient with agranulocytosis, including primary risk for thepatient? InfectionRisks for the patient -Risk forinfection. with leukemia. Why is -ineffective coping, related to diagnosis and disease there a risk for process. hemorrhage forsome -Thrombocytopenia inducedhemorrhage. leukemia patients? Characteristics of DIC (disseminated intravascular coagulation)? Overstimulation of clotting in anticlotting process. Characteristics and Carries oxygen from the lungs to the cells and functions of Carbon Dioxide carries away from the cells to the lungs. hemoglobin with reference to oxygen and carbon dioxide? Characteristics ofthe spleen including its locationinthebody? Priority nursing a concernforthepatient with immuno suppressionrelatedto chemotherapy? Priority nursingconcern for the patient with severely decreased platelet count? Therapeutic communication between the nurse and the spouse of a dying patient?Foundinthe leftupper quadrant. Servesa reservoirfor blood(upto 500cc), forms lymphocytes monocytes and plasma cells, destroys wornout RBC, removes bacteria from phagocytosi s. Prevent infection, handwashing. Hemorrhage OPEN ENDED QUESTIONS,LISTENCancer antigen important in the diagnosis of gynecologic cancer? CA-125 The relationship betweencancerand heredity? Therecanbeapredispositioninfamilyforspecifictypesof cancer (ex: other family members have history of cancer, go get checked out.Do notwaituntilithitsyou) Characteristics of Transducer emits hundreds of thousand sound waves at ultrasound as a high frequency wherever there is a density, it converts the diagnostic tool.What sound waves back and creates an image. does it do and how does it work? Nursing diagnosis for the patient who has experienced surgery for cancer involving the removalofbreast,limb, or surgerythatresultsin an ileostomy or a colostomy. Howbestto addressthis concern? Nursing care for a patient with a radioactive implant? Disturbed body image related to surgical removals Keepdistance as much as possible, minimize time in room (implant doesnotmakeurineorstoolradioactive) An accessory organ of digestion,thelargest glandularorganinthe body? LiverRisk forthe patient with peptic ulcer disease? Perforation(peritonitis,death) Therapeutic Educate them about nursing care postoperatively. Monitor communication to closely, give painmedications reassure a patient who is about to undergo surgery? Teaching apatient Do not each 3 hours before bed, sit two hours after meals, about lifestylechanges smallfrequentmeals,reduceintakeofcaffeineandalcohol to assist the patient with preferably to zero the managementof GRED (Gastroesophageal Reflux Disease). Treatment for an ulcer caused by Heliobacter Pylori? Antibiotic therapy Characteristics of Jaundice? Nursing assessment prior to the administration of contrastmedium? Characteristics of the 4 major types of cirrhosis? Characteristics of Crohn's Disease? Inflammation of segments of the GI tract, malabsorption, diarrhea frequentlyYellow, discoloration ofthe skin, mucous membranes, and sclerae oftheeyes, causedbybilirubin.Lookatliverand bilirubin test Allergies to iodine,shellfish Alcoholic, postnecrotic, biliary,lanexAppropriate foodsfor the patient newly recovered fromacute pancreatitis? Low fat, high complex carbs Teaching apatient Restandexercise,autoimmunediseasefortherestofyour about hernewly life diagnosed rheumatoid arthritis? Teaching apatient Degenerative disorder, exercise must be joint sparing about hernewly (swimming) diagnosed osteoarthritis? Favored alternative supplement forpatient with a chronic musculoskeletal disorder? Characteristics ofpain? Glucosamine Subjective (whatever and wherever the patient says it is), pain often occurs when there is tissue damage. Chronic: long last pain over six Characteristics ofthe electromyogram? Needleelectrodeintotheskeletalmusclessothat electrical activity can be heard Mostcommon types of hepatitis in the united states? Hepatitis A Medications that are contraindicated forthe patient withCirrhosis? Tylenolmonths acute: less than six months Whatarethefivevital signs? BP,Temp,Resp.,Pulse,PainMedicationtoreverse the effects of an opiate? Narcan Appropriate nursing measures to prevent/treat constipation? Appropriate nursing response to the patient's complaintof pain? Describetheprocessof withdrawal form an opiate agonist? Fluids, high fiber, DSS (Colace), stool softeners Believe what the patient says Pain medications (opioid direct), takes about 2 days for symptomstopeakandabout5-7daystodisappear Compareandcontrast the use of acetaminophen and aspirinforthepatient with arthritis? Aspirin-upsides:anti inflammatory downside: GI upset Tylenolupside: analgesic downside: non anti inflammatory,less irritatingtothestomachbutinhigh doses ishepatotoxic Ifitisaautoimmune,thinkaboutNSAIDSbecausethereis no inflammation process Patient teachingabout Gradually drop the dose so the patient does not go how a patient who has through withdrawals Restrictions on the use of digoxin? Hold ifthe apicalpulseislessthan60bpm pain scale tobe used with children? Wongbakerfacesscalebeen receivingopioids for a few months should discontinue the medication.Characteristics of patient controlled analgesia? Allows patient to control, inject whenever pain comes, it locks you out what is the difference -Objective is what you observe between objective -Subjective is what the patient tells you symptoms and subjective symptoms? Characteristics of TranscutaneousElectric Nerve Stimulation? Electrical current that is attached to your body that stimulates a nervelocallythat blocks transmission ofpain sensation using gate theory Preferred route of administration of differenttypesofpain relievers for different types ofpain? IV (opioid agonist), PO Characteristics of tuberculosisincluding it mode of transmission and infective potential? Droplet nuclei, isolation, negative pressure, spores forming phase, not highly contagious but you should take appropriate precautions Characteristics of empyema? Pusinthepleuralspaceofthethoraciccavity Characteristics of orthopnea? Sitorstandtobreathdeeply(placeonchairfacingbackor lean over table) Possibleeffectsof unrelieved pain? Anxiety, slows recovery, reduces trustSigns and symptoms of Decreased breath sounds, airhunger(gasping), unequal the sudden rise and fall of the chest development of a pneumothorax?Best time to teach the Prior to surgery (this is when you informs hat there will be patient about the use of additional medication if needed) a PCA(Patient Controlled Analgesia.) Uses andcharacteristics of conscious sedation? Itdecompressedthecentralnervoussystem.Sedated sufficiently so that thereis no anxiety, no apprehension of fear, and little or no pain Teaching for a patient Cleanfromleaststeriletomoststerile,handhygiene,keep who will do daily sterile technique, teach signs of infection (pus, dead skin dressing changesat cells, erythema, inflammation, heat home? Frequency ofnursing Every 15 minutesx4 assessments fornew Every 30 minutesx4 post-operative Every hour x4 patients? who has the authority to sign the informed consentfor surgery? Patient, advanced directive (designated person), if no one isavailable andisemergenttodosurgerythephysicians can sign Counseling thepatient Talk to them preoperatively and explain that we're going to who is afraid of pain observe you and do our utmost to keep you safe and associated withan makesurethatanypainistreatedquickly,donotbeafraid upcoming surgery? to ask Patient teaching about the useoftheincentive spirometer? Characteristicsof informed consent? The physician informs the patient about the procedure being donePriorto surgery, inhale slowly andkeep itbetweenthe parameters to inflate your lungs fully to prevent complications especiallypneumoniaFirst priority for the nurse in admitting the patienttoamed-surg bed after transfer from the PACU? ABC's Why does the nurse To know what can cause adverse reactions and what may take a complete interfere with postoperativemedications medication history, including the use of supplements, when admitting a patient for surgery? Circumstances that If the patient is sedated, major tranquilizers, major pain could prevent from medication validly signinghis informed consent document? The four types of General(IVimmediatelybefore surgery), regional(epidural anesthesia. Whenand or spinal) conscious sedation(30 minutes prior to how are they procedure) local(immediately before procedure) administered? Measures to encouraging peristalsis in a postoperative patient? Firstsignsand symptoms of hemorrhage? Nursing intervention after a wound evisceration?Early ambulation Increase pulse, increase respiration, decrease BP, pallorto ashy greyskin, decreased urineoutput, brightred blood, upper GIcoffee ground emesis,lower GIblacktarry stool Wound opensand intestines comeout, coverwith warm normal salineAbnormal early postoperative signs? Respiratory distress, urinary retention, bright red bleeding or emesis, signs of shock Routine of offering postoperative analgesiato a patient in her second postop day? Continue with every 4 hours around the clock Administration ofIM Must correctly demonstrate it back to you, give analgesia analgesia to a patient attest 30 minutes before exercises postoperatively before controlled deep breathing and coughing? Signs of a pulmonary embolus? Howtosplintapatient for deepbreathingand coughing who has an incisioninhislowerleft abdomen? Teaching ofcontrolled beep breathing and coughing? Sense of impending dume, extremely restless, sudden sharppain inchest, respiratorydistress, petechiae in upper part ofchest Hug a pillow over the whole low abdomen 2-3deepbreathsthencoughfromasdeepdownas possible Priority nursing problemsforapatient with a new ileostomy? Excoriationofskin(impairedskinintegrity),disturbed body image Idealtime todopre-op teaching ifpossible? 1-2 days before surgeryPatient teaching for a NPO after midnight, down the esophagus into stomach patient who is about to and into duodenum. No pain during procedure. Will undergo an carefully monitor before food or drinks. Make sure gag esophagogastrodueden reflexes are active oscopy? Special assessment required forapatient after agastrectom? A nursing measure to prevent or minimized dumping syndrome? First priority for the patient aftercompleting barium swallow examination? Nursingeducationfora patient who is undergoing astooltest for ova and parasites? The most serious complication of a hernia? Concernedaboutperniciousanemia(vitaminB12takenin form of ability to metabolize which is injection or sublingual) and dumping syndrome (rapid gastric emptying) Six smallmeals Immediate access torestroom Once a day for three consecutive days Strangulationitoccludedbloodsupplyandobstructs intestinal flow Therapeutic Listen, open needed questions, encourage to express communication feelings between a nurse and a patient who is expressing that he does not think he will ever adjust to his newcolostomy?Whatistheimportance of bowel sound assessment forapatient who has had an abdominalsurgery? Peristalsis has returned in ALL four quadrants Primary nursing goal for a patient with an immunodeficiency disease? Acriticalnursing goal for a post-operative liver transplant patient who is receiving Imuran? Nursing procedure after giving a clinic patient an injection of penicillin? Thepurposeofgiving cyclosporine to a patientafterakidney transplant? Preventinfection Preventinfection Wait 20-30 minutes to see if there is an allergic reaction To prevent tissuerejection Emergency medication for a patient experiencing an anaphylactic reaction? Epinephrine Signs of an anaphylactic reaction? Respiratorydistress, hives, swellingaround eyes, swelling of lips, swelling of tongueThefirstevidenceina patient's historyofa possible immunodeficiency disease? Recent history of repeated infections Priority nursingaction Two lisenced nurses check the blood and the chart, then before administeringa check once entered the room blood transfusion to a patient? What is the average 10-14 years length of time between Contaminated blood transfusion or dirty needle 1-2 years infection with HIV (the Human Immunodeficiency Virus) and the onset of AIDS (Acquired Immune Deficiency Syndrome)? Laboratory findingthat indicates progression for HIVinfectiontothe onset ofAIDS? Patient education regarding the use of condoms in the prevention of sexually acquired diseases? CD4 count less than or equal to 200 Demonstrate how to use and give them information SignsofaKaposi's sarcoma lesion? Purple,irregularborders,notulceratedlesions,alloverthe bodyIs the HIV positive patient contagious beforeacquiringfullblown AIDS? YesDTAP contraindication Hxofinconsolable crying NewbornCarSeat Safety Snug harness across axillary. Not across abdomen or neck. Nursing measuresto Lift patient, reposition patient, use othermethods for pain assist the patient with before medication comfort and pain control? Nursing measures to assist a patient to prevent post-operative pulmonary complications? Fontella Closing on Newborn (Anterior and Posterior) Deep breathing, coughing, incentive spirometer Anterior: 12-18 months Posterior: 1-2 months Cholecystitis (inflammation of gallbladder)Diet Moro Reflex (one of many reflexespresent at birth) Position for suppository or enema administration. -Increase fruits, vegetables, whole grains. Ex: Melon -Avoid greasy/fatty foods -Startled(armsoutsideways,palmsup,thumbflexed). Ex: strike surface nextto newborn. -Sim's/leftlateral/Rt.kneetochest Varicella contraindication Corticosteroids Besttimetoperform bladder scan. ImmediateaftervoidHep B contraindication Baker's yeast MMR contraindication -Pregnancy, recent blood transfusion.... Anorexia Nervosa Electrolytes increasing: Sodium, Potassium, Chloride, BUN, Liver function, Cholesterol. Bulimia Therapeutic Nursing Care offer small and frequent meals Venturi Mask Ensure reservoir bag 2/3 full during inspiration and Thoracentesisposition expiration. sitting position, arms raised and resting overbed table. Ileostomy what pt expect on appearance. Ileostomy care and education -Initial drainage: dark green, odorless. -Some initialbleeding normal -Pink or red stoma color normal -Initial swelling; decreases 2-3 weeks later *-Empty pouch: 1/3 to 1/2 full. -Clean pouch 1-2 times daily. -Pouch change every 4-6 weeks. -Wafer size 1/8 to 1/4 larger than stoma -Avoid high fiber foods to prevent blockage. 89% oxygen postoperative: what to do... Change oxygen to another finger Non-Rebreather Mask Ensure two "flaps" open during exhalation/close during inhalation. Delirium (occurs quickly) Simple orientation and low stimuli environmentChlorpromazine (med -Severe Spasms/Tremors for psychoses) Tx:benzotropine(Cogentin),diphenhydramine(Benadryl). -Adverse Effects and given treatmentContraction StressTest -Brush palm across nipple for 2-3min to release natural (CST). oxytocin that produce contractions. Description, Purpose, -Determine how fetus will tolerate stress of labor. normal range. -3 contractions, 10 min period, duration 40-60 secs. What is most likely to happen during variable deceleration? Whatismostlikelyto happenduringearly deceleration? Cord compression Fetal Head Compression Cystic Fibrosis -DNA mutant gene identification. (Respiratory Disorder) -Open capsule sprinkle on food (Enzyme: Pancrease). -Diagnostic Test -Possible Medication Administration Levothyroxine -Thyroid hormone; treats hypothyroidism. (Synthroid) -Cardiac pts; aggrevates tachy and anxiety -What is it? -Take in the morning, on empty stomach -What patientsshould use this medication with caution? -Best way to take? Levothyroxine (Synthroid) -Signs ofToxicity *Cardiac: anxiety, chest pain, tachy, htn. Buck's Traction -Immobilization -Goal -Follow RXorders: type of traction, weights, whether it can-Following conservative be removed. measurements -Reposition every 2 hrs, provide pin care, neuro checks -Skin integrity/NeuroOrientation Phase Introduce,Discussconfidentiality, Setgoals Working Phase ProblemSolve TerminalPhase Evaluation (evaluate goals, experience, feelings) Chadwick'sSign Purplish vulva during pregnancy Patient is having a hysterectomy and states, "Icanpossibly plan apregnancy". What needs to be reinforced? Outcome Vaginal Flush Complications Preterm Labor: Ruptured membranes, signs of infection SucralfateforPUD coatsstomachtopreventformationofulcerandaidswith healing existing ulcers 17 year old having an emergency surgery. Whattypeofconsentis best tointervene? Verbal Insulins notto mix garglarine and determis Malfunctioning IV machine markasdefectedandgetnewone Ferrous Sulfate(Feosol) -Treats iron deficiency -Purpose -GI distress: nausea, constipation, heartburn. -Reporting symptoms -Take on empty stomach, drink with straw and rinse to -Administration prevent staining. -How to monitor - Increase Hgb of 2g/dL, Hct effectiveness Amputation -Patient education Apply prosthetic beforeambulating.What is the best recommendation for a newly diagnosed diabetic 2patientsthat lives independently? Circumcision post op care: cleaning TBprecautionsandcare Refer to supportgroup -Change diaper every 4 hrs. -Clean penis with each change. -Applypetroleumjellyforatleast24hrsaftercircumcision (prevent adhering). -Fan fold diaper (prevent pressure). -Avoid wrapping penis (impairs circulation) -Washing: trickle warm water over penis. -Do not clean yellowish mucus that appears by day 2. -Do not use moistened towelettes. -Healing: a couple of weeks. -private room/negative pressure -N95 masks -ptwearmaskwhentransportedoutofroomorinany public place. -Medications:maybetakingupto4medsatatime;upto 6-12 months -Test exposed familymembers -Sputumcultureevery2-3weeks;3negativesresultsin noninfectious. MRSAContact Precautions -keep distance within 3 ft of client -Private roomorshare with someone with similarinfection (wound Vaginal discharge during early pregnancy Leukorrheainf ecti on, herpes simplex) -double bag dressinggauze. -PPE: Gloves and Gowns.Contraindication During Alcohol Withdrawal Delirium,accompanied byhallucinations. Interaction between SSRI (e.g.fluoxetine) and St.John's Worts Diabetic FootCare Hypertension and Increased HR; may be life-threatening. -Nailcare: Podiatrist, cut nail straight across. -Wear Clean Cotton Socks/Closed Shoes -Do not soak feet or wear ointments Patient education for Amniocentesis. Indications ofFluid Volume Depletion (Hypovolemia) -Position: supine or rolled towel under right hip -Continue breathing normally when inserting needle -Rest 30 mins after procedure. -Increase fluids for next 24 hrs. -Thready pulse/Hypotensive -Tachy -Increased Respiration -Cool, Clammy, Diaphoretic -Decreased Urine Output -Thirst Used Opioidoverdose Naloxone (Narcan) Drawing up Insulin? Regular vs.NPH First Regular (clear), then NPH (cloudy) Metformin most commonsideeffect Renal(kidney)failureType Stomas: -Single (one stoma); brought through onto anterior abd Appearance wall. -Single -Loop (two openings); proximal (active) and distal -Loop (inactive). -Divided -Divided (two separate stomas); proximal(digestive) and -Double-Barrel distal (secretesmucus). -Double-Barrel (distal and proximal sutured together are both brought up onto abd wall).PriorityforPanic Disorder Breathing Technique NewbornWaterand Room Temp Water: 120F or lower Room:97.9-99 F Educationonmedsfor Kidney Disease 1.Digoxin (Lanoxin) 2.Sodium plystyrene (Kayexalate) 3.Epoetin alfa (Epogen) 4.Ferrous sulfate (Feosol) 5.Aluminumhydroxide gel (Amphojel) 6.Furosemide (Lasix) 1. Take within 2 hrs of meal, monitor signs of toxicity, apical pulse for 1 min. 2. Monitorhypokalemia, restrict sodium intake. 3. blood twice a week, monitor HTN. 4. administer following dialysis with stool softner, take with food. 5. avoidptswithGIdisorders,take2hrsbeforeorafter Digoxin. 6. Monitor I&O, bp, weight. Report thirst, cough. Bathing Newborn Bathe from cleanest to dirtiest technique -Eyes -Face -Head -Chest -Arms -Legs -Groin (last) Documentation for Ostomy Care (Stool) Amount Consistency ColorNewbornreflexshown on day 1 hear voiceDementiaLiving Coordination HomehealthAgency>AssistedLiving>NursingHome Need forSterile Gloves Inserting Catheter Immunization is recommended for postexposure protection Hep A (fecal route) Arthroplasty pt -Do not bend at waist. education -Use abductor pillow in between legs. -How to avoid -Perform Continuous PassiveMotion contractures, -Ice pack dislocations; prevent DVT's. -Non-pharmalogical treatment COPD -High Fowler position -conservative -Increase fluids to liquify mucous measurements -Albuterol -Rapid relief med Discomforts During -Nausea Pregnancy -Fatigue -Backache -Constipation -Varicose Veins -Hemoroids -HeartburnAcute Mania Interventions -Decrease stimuli and one to one observation if necessary. -Nasal stuffiness -Dyspnea -Leg Cramps -Edema lowerextremitiesReinforcing Teaching About Oppositional Defiant Disorder Osteoarthritis What to do before bolus feeding or administration of medication What to do when pt complains of cramping during tube feeding? Ideallocation for drainage bag of catheters Ventilator Alarms -Low Pressure -High Pressure Glasgow Coma Scale (head injuries) (eyes,verbal,motor) Setclearlimitsonunacceptablebehaviorsandbe consistent. Reward system foracceptable behavior. Alternate: Heat Therapy for Pain and Cold Therapy for Inflammation -Useassistive devices (raisedtoilettohelpnotstraining) Check for residuals (60 mLsyringe) Decrease infusion rate Hang on bedframe below level of the bladder. -Low: disconnection -High: suction for possible secretions, kinks. highestnumber15,good. lowest number 3, severe. Pressure Ulcer -Bed every 2hr, chair every hour. Strategies -Apply barrier cream and moisture absorbing pad. -Reposition time (bed/chair) -Incontinent Pt. BulimiaPlanofCare when meal planning closelymonitortheclientduringandaftermealsto prevent purgingTrueLaborvsFalse Labor Abdominal Discomfort true:lowbackandabdominal false: abd and groin Types of Decelerations: -early: head compression <120 fhr -late: uteroplacental insufficiency -early -variable: cord compression -late -variable NursingInterventions duringlateorvariable deceleration left lateral position, oxygen, c-section NormalFetalHR 120-160 Contraindicated Immunizations During Pregnancy -Varicella -Zoster -MMR How to calculate due date: LMP 8/2/15 -subtract 8-3=5 -add 7 + 2= 9 May9,2016 HowtomeasureFundal Height topofsymphysispubistotopoffundus HPV vaccination doses 3doses Immunization: booster every 10years DTPNursing CareforBoggy Uterus Askpttovoid;ifstillboggymassagetopoffunduswith fingers and reassess every 15 mins. NursingCarefor Engorgement Apply moist heat for 5 min before breastfeeding. Icecompressesafterfeedingtoreducediscomfortand swelling.BUN/Creatinine normal values (forkidneyfunction) 7-20/0.8-1.4 WBC normal values (forinfection) 4,000-10,000 Sodium 136-144 Potassium 3.5-5.5 Chloride 96-106 Whatiswrongwiththe script? gentamicin50mgpo every 4 hours #30 Drug name: Gentamicin (capital G) Be ready to administer ____ for Magnesium sulfate toxicity Calcium gluconate Sign of mag sulfate 1. Absent deep tendon reflexes toxicity (4) 2.Resp rate < 12 3. Urine output <30 Anemia lab RBC 4.20-4.87 Narcotic antidote Naloxone (narcan) NursingCarefor Mastitis Continue breastfeeding and take antibiotics as prescribed.4.Mag levels above 8 Understanding Rh. Administration of antibodyandtime. Stroke eating precautions Mother Rhnegative. Fetus Rh positive. Rhogam at 28 weeks, then 72 hrs after birth. -check gag reflex -thickened fluids/puree -Sit upright/flexed neckforwardAdverse effect of ACE inhibitor (pril's) ACE inhibitors, such as captopril, increase potassium levels (hyperkalemia) Dehydration S&S (hypovolemia) Urine Specific Normal Values and Significance -pulse; weak and thready. hypotension -tachy -confused -decreased urine output -skinandmucousmembranesdry Urine Specificityincreased Decreased hypervolemia. Increased hypovolemia. 1.001-1.029 JVD.Whatsideof heart? RightFundamentals of Nursing 23 sets Picmonic $8.05 $5.99 STUDY GUIDE YOU MIGHT ALSO LIKE... [Show More]
Last updated: 2 years ago
Preview 1 out of 450 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$17.50
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Oct 22, 2020
Number of pages
450
Written in
Additional information
This document has been written for:
Uploaded
Oct 22, 2020
Downloads
4
Views
533





 – Concorde career College.png)