*NURSING > SHADOW HEALTH > NR 509 Week 1 Assessment Tina Jones Shadow Health Latest 2021/2022 (All)
NR 509 Week 1 Assessment Tina Jones Shadow Health Latest 2021/2022
Document Content and Description Below
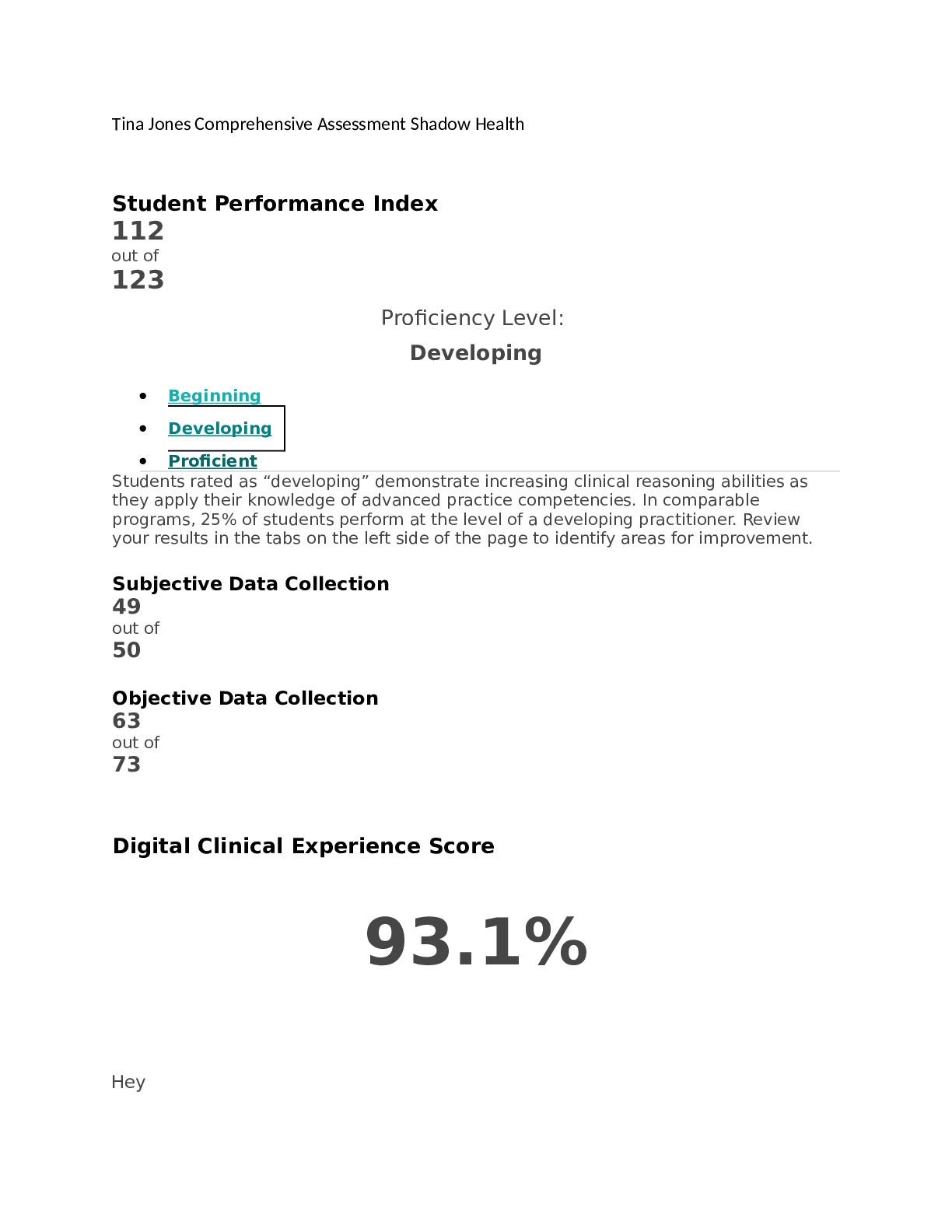
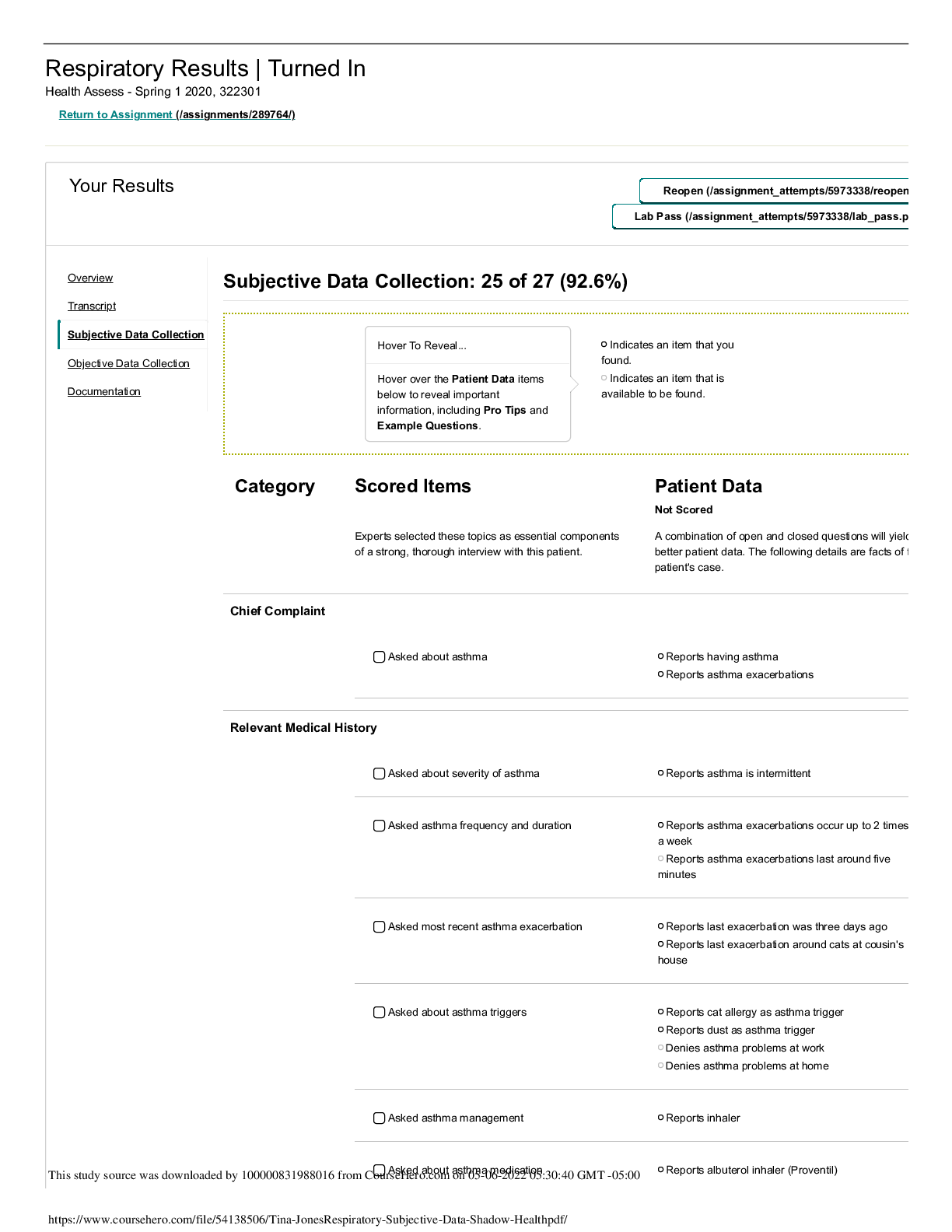
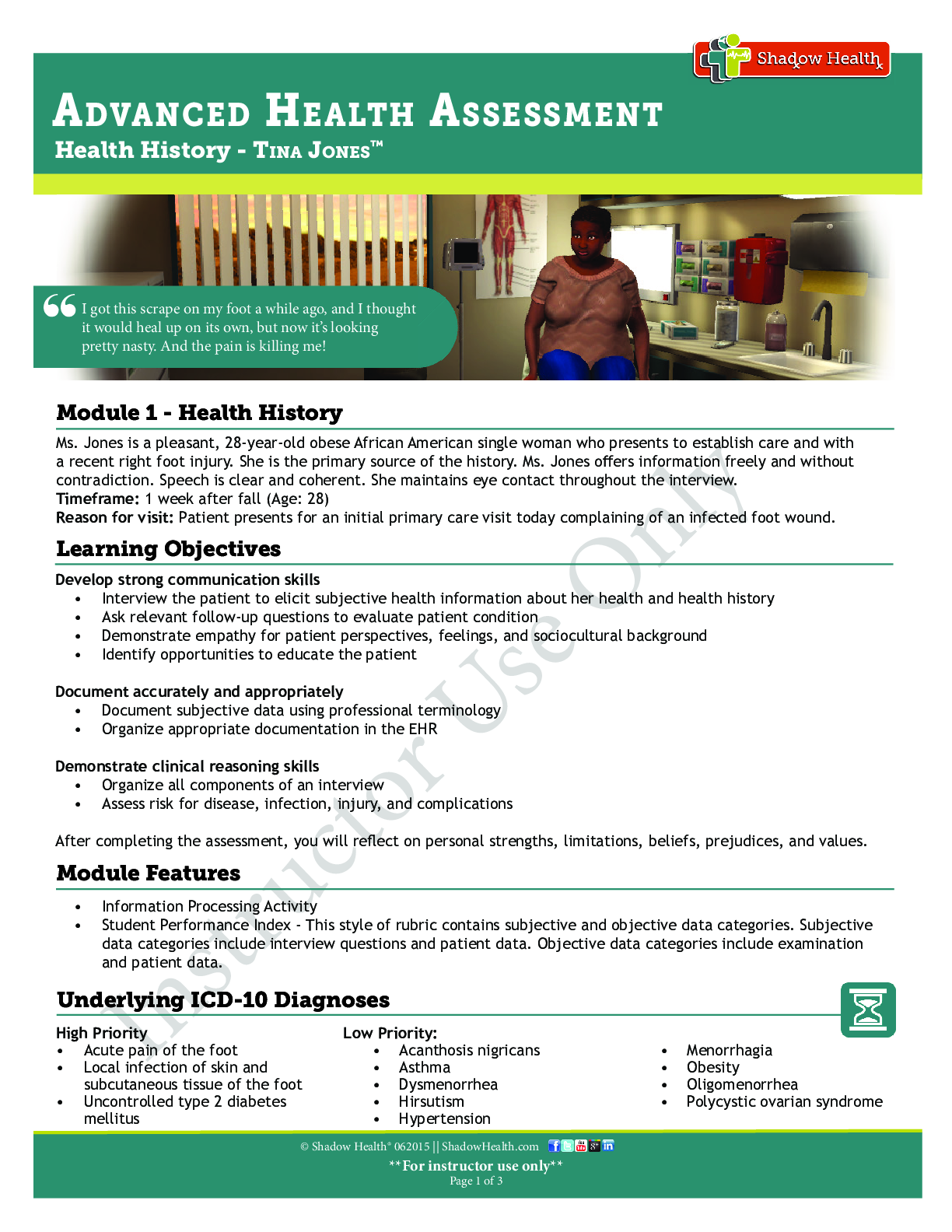
Document: Provider Notes Student Response Model Documentation Identifying Data & Reliability Tina Jones age: 28 African American female patient herself, seems reliable supervisor at Mid-America... n Copy & Ship Ms. Jones is a pleasant, 28-year-old obese African American single woman who presents to establish care and with a recent right foot injury. She is the primary source of the history. Ms. Jones offers information freely and without contradiction. Speech is clear and coherent. She maintains eye contact throughout the interview. General Survey Tina is a 28 year old African American female that appears healthy and stated age. Alert, oriented, and cooperative. No signs of distress. Ms. Jones is alert and oriented, seated upright on the examination table, and is in no apparent distress. She is wellnourished, well-developed, and dressed appropriately with good hygiene. Chief Complaint "I got this scrape on my foot a while ago...and the pain is killing me!" “I got this scrape on my foot a while ago, and I thought it would heal up on its own, but now it's looking pretty nasty. And the pain is killing me!” History Of Present Illness First noticed scrape on right foot two days ago. Tripped and fell down steps, scraped foot on the edge of the step. Sharp, throbbing pain rated a 7 on 0- 10 scale. White drainage. Unable to bear weight on right foot and has missed two days of work. No chills or fever noted. Reports temperature of 102 last night. Ms. Jones reports that a week ago she tripped while walking on concrete stairs outside, twisting her right ankle and scraping the ball of her foot. She sought care in a local emergency department where she had x-rays that were negative; she was treated with tramadol for pain. She has been cleansing the site twice a day. She has been applying antibiotic ointment and a bandage. She reports that ankle swelling and pain have resolved but that the bottom of the foot is increasingly painful. The pain is described as “throbbing” and “sharp” with weight bearing. She states her ankle “ached” but is resolved. Pain is rated 7 out of 10 after a recent dose of tramadol. Pain is rated 9 with weight bearing. She reports that over the past two days the ball of the Student Response Model Documentation foot has become swollen and increasingly red; yesterday she noted discharge oozing from the wound. She denies any odor from the wound. Her shoes feel tight. She has been wearing slip-ons. She reports fever of 102 last night. She denies recent illness. Reports a 10-pound, unintentional weight loss over the month and increased appetite. Denies change in diet or level of activity. Medications Tramadol 50 mg tablet, 2 tablets by mouth three times a day as needed for pain Proventil 90 mcg/spray MDI, 2 puffs by mouth as needed for asthma No vitamins or herbal supplements Advil as needed for menstrual cramps Acetaminophen 500-1000 mg PO prn (headaches) • Ibuprofen 600 mg PO TID prn (menstrual cramps) • Tramadol 50 mg PO BID prn (foot pain) • Albuterol 90 mcg/spray MDI 2 puffs Q4H prn (Wheezing: “when around cats,” last use three days ago) Allergies Allergic to penicillin, develops rash, hives. Allergic to cats, develops itchy eyes, shortness of breath. No food allergies. No seasonal allergies. No latex allergy. Penicillin: rash • Denies food and latex allergies • Allergic to cats and dust. When she is exposed to allergens she states that she has runny nose, itchy and swollen eyes, and increased asthma symptoms. Medical History Chickenpox in second or third grade. No measles, mumps, pertussis. Strep once a year as a child but not since high school. No rheumatic fever, scarlet fever, or polio. Diagnosed with asthma at age 2. Diagnosed with diabetes a few years ago. Hospitalized several times as a child for asthma attacks, last time was age 16. Gravida 0/Para 0/Abortion 0. Recent weight loss of 10 pounds. No excessive bruising. No fever or sweats. No broken bones. No burns. No eczema or psoriasis. Darkening of skin on neck reported. Excessive dryness on arms and legs. Excessive thirst. Wakes up 2-3 times a night to urinate. Asthma diagnosed at age 2 1/2. She uses her albuterol inhaler when she is around cats and dust. She uses her inhaler 2 to 3 times per week. She was exposed to cats three days ago and had to use her inhaler once with positive relief of symptoms. She was last hospitalized for asthma “in high school”. Never intubated. Type 2 diabetes, diagnosed at age 24. She previously took metformin, but she stopped three years ago, stating that the pills made her gassy and “it was overwhelming, taking pills and checking my sugar.” She doesn't monitor her blood sugar. Last blood glucose was elevated last week in the emergency room. No surgeries. OB/GYN: Menarche, age 11. First sexual encounter at age 18, sex with [Show More]
Last updated: 2 years ago
Preview 1 out of 97 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$15.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Mar 10, 2022
Number of pages
97
Written in
Additional information
This document has been written for:
Uploaded
Mar 10, 2022
Downloads
3
Views
756