*NURSING > SHADOW HEALTH > Comprehensive Assessment | self reflection Shadow Health Latest 2021 (All)
Comprehensive Assessment | self reflection Shadow Health Latest 2021
Document Content and Description Below
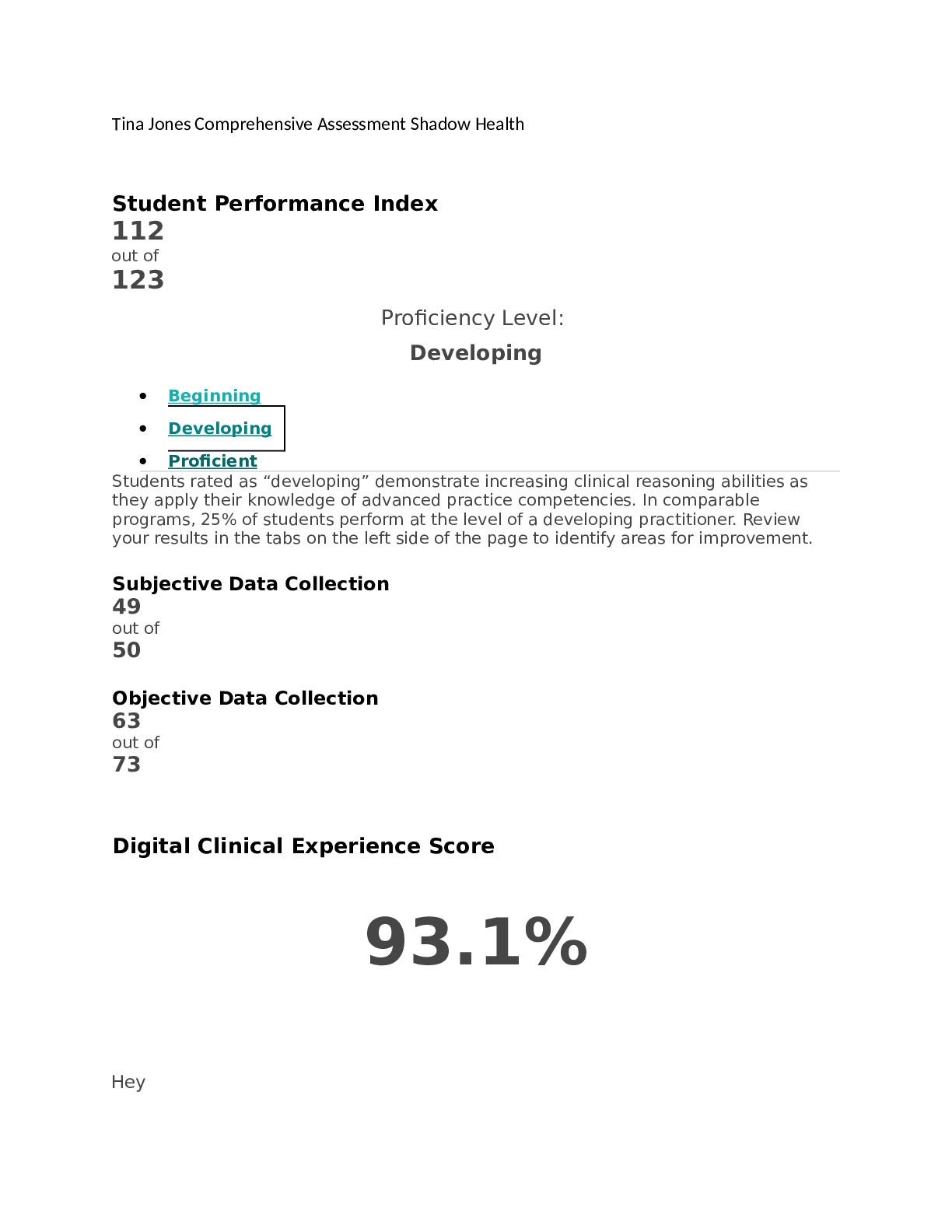
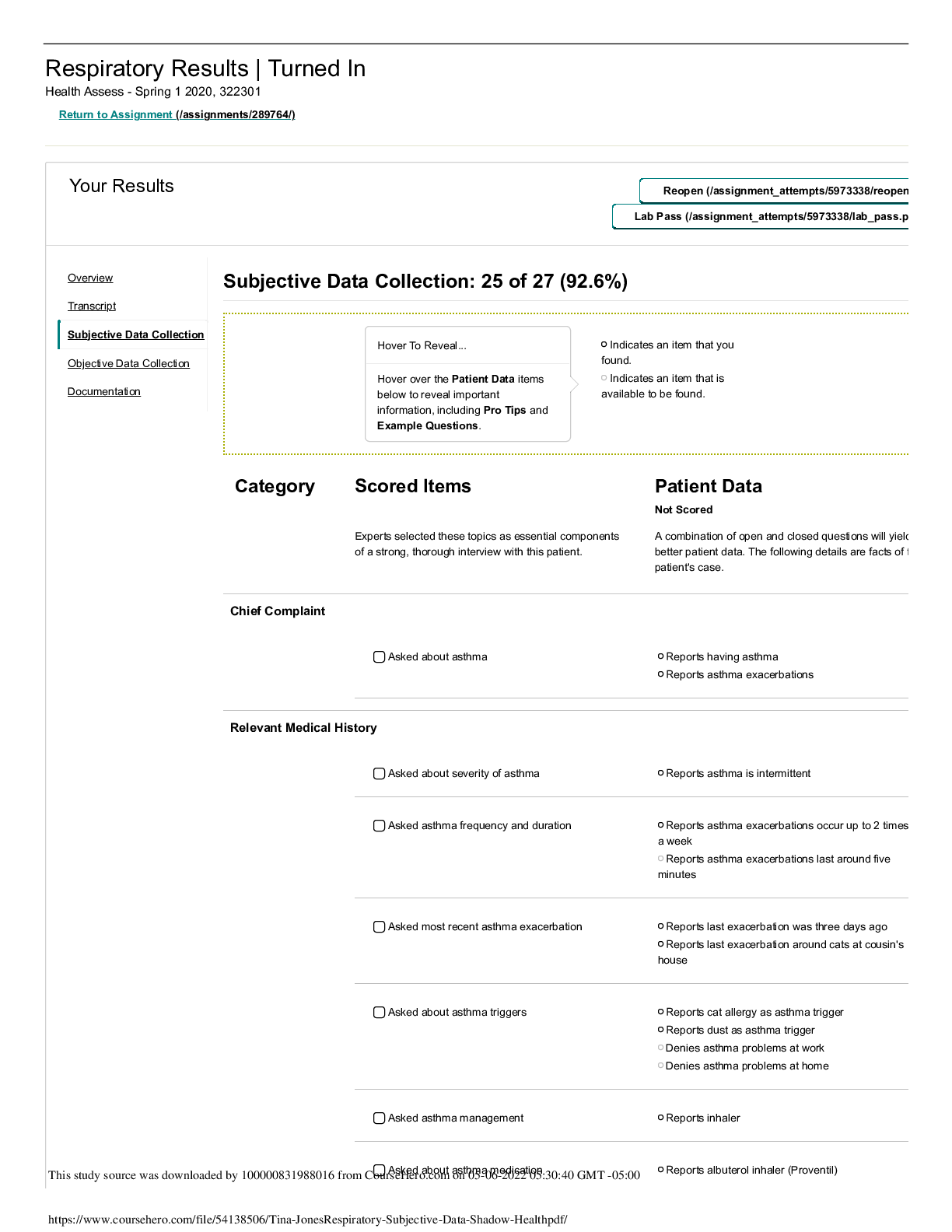
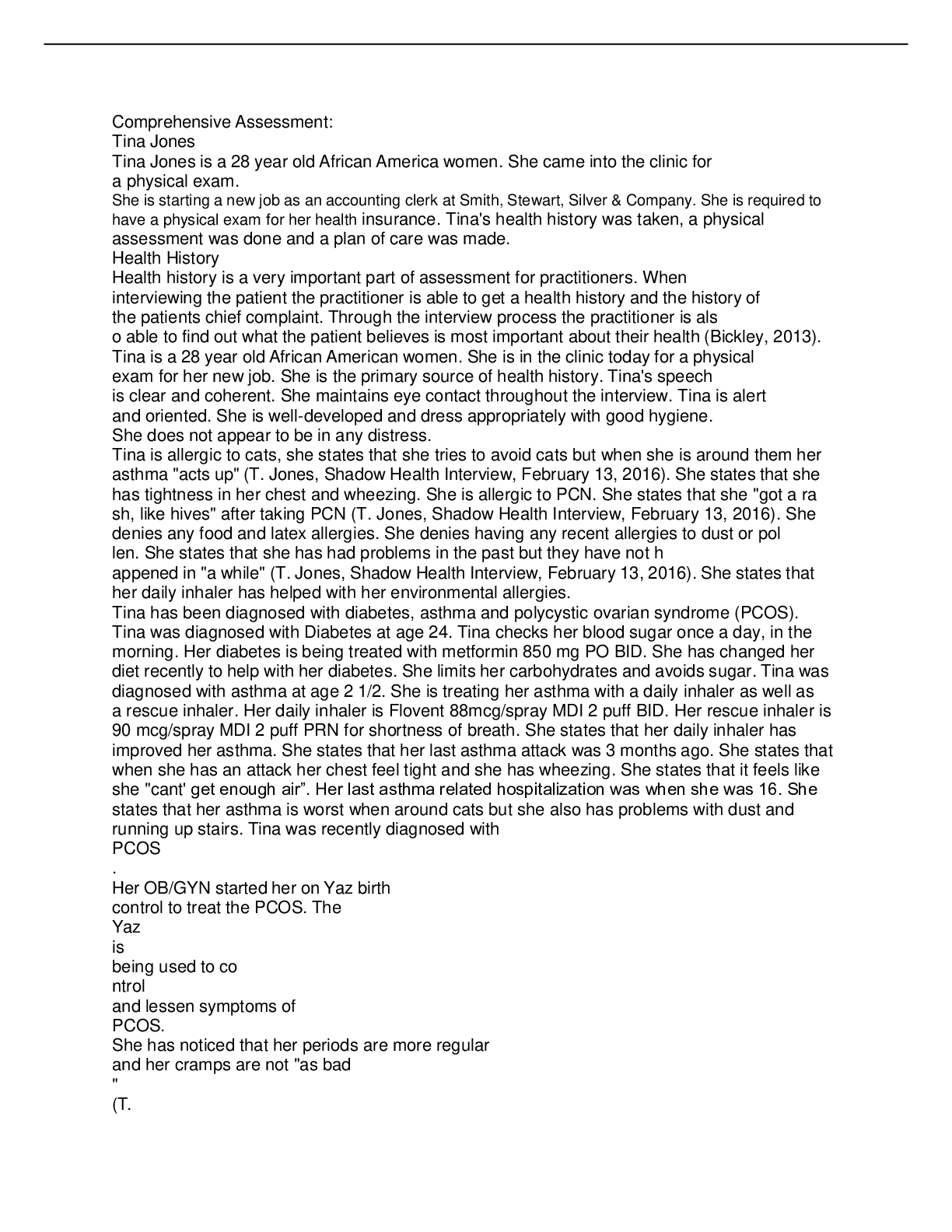
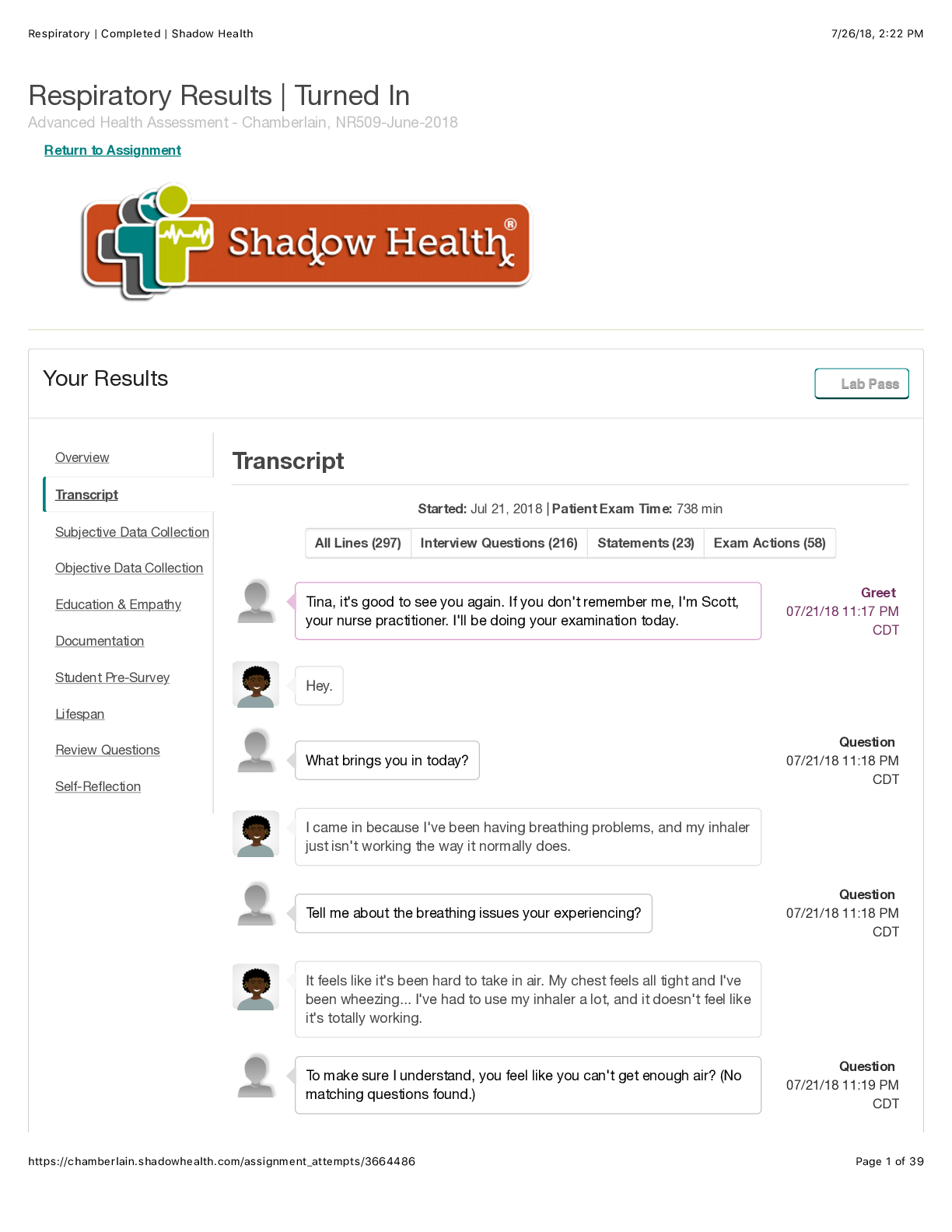
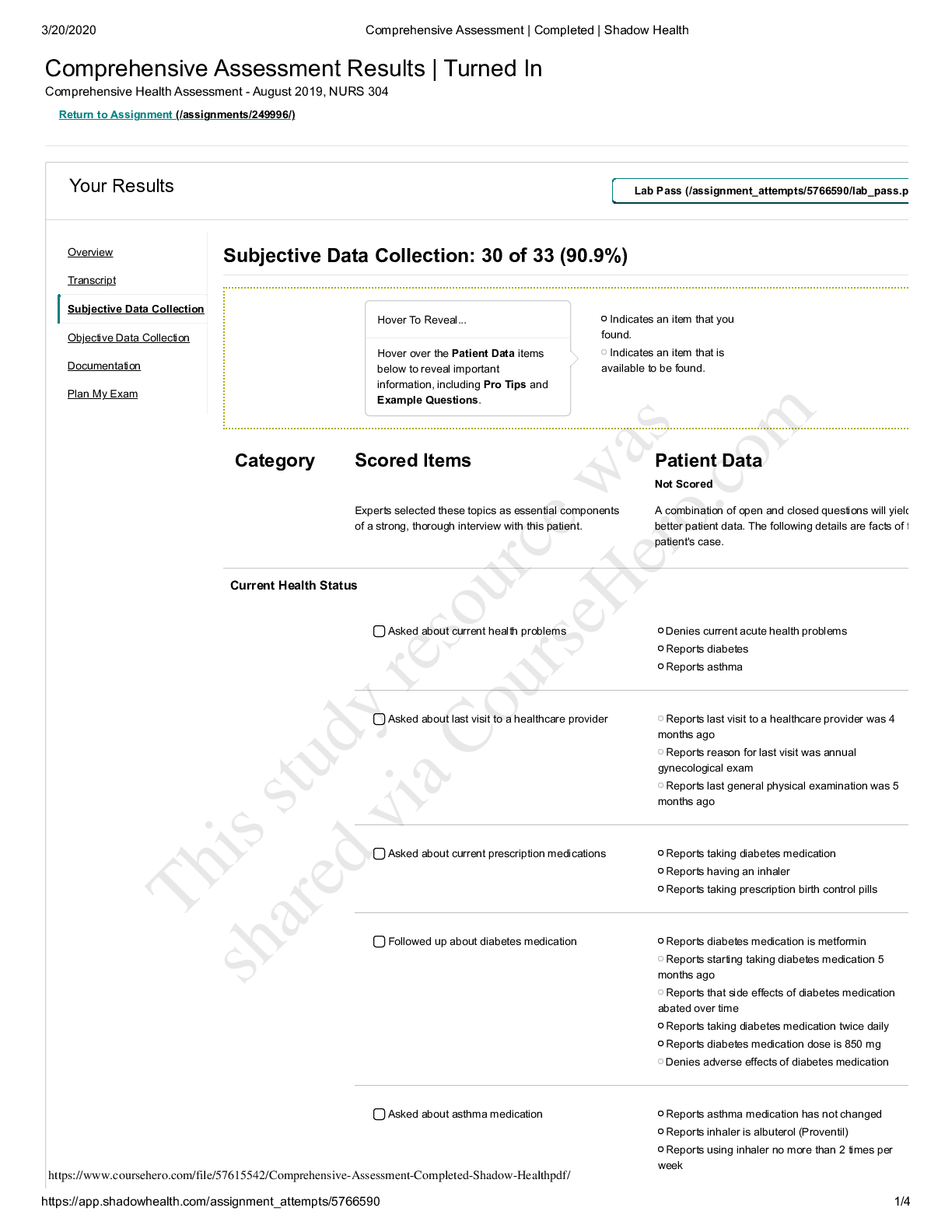
Comprehensive Assessment Results | Turned In Advanced Health Assessment - Chamberlain, NR509-April-2018 Return to Assignment Your Results LLaabb PPaassss Self-Reflection Activity Time: 20 min Exp... licitly describe the tasks you undertook to complete this exam. Student Response: A comprehensive assessment is a complete, all-encompassing, in-depth assessment that includes a complete health history and physical assessment. Components of the health history are the patient's personal history of illness, as well as their family medical history, including any current or prior treatments, surgeries, risk factors, and medications or supplements. In addition, it should include details of other aspects of health, such as the patient’s perception of their health, health beliefs, coping mechanisms, support systems, and functional status. The first question I asked was for Tina to verify her name and date of birth. This is a safety check that assures the assessment I am about to conduct, is on the right patient. It also helps me to determine if this patient is alert to self. Another important question that I started my interview process with was asking the patient the reason for her visit, and if she had any health concerns she would like to discuss. This helps focus the attention on the patient and what he or she needs or hopes to get out of the visit, and also helps guide the interview. Other questions were based on the components of the health history mentioned earlier. For example, I asked Tina how she felt she was doing, to get insight to her perception of health, which can help identify areas of that Tina may need further education on. In addition, I asked Tina what her medical history was, what (if any) medications (OTC, prescribed or supplements) she was currently taking and the reason for taking them, and the dose and frequency. Aside from Tina’s health I asked questions about her personal life, such as who she lived with, what her new job would be, relationship status, and what she enjoyed doing for fun. Again, helping to develop a relationship with the patient, but also providing me with insight to her functional status, support systems, and so on. Other questions asked pertained to risk factors or unhealthy/unsafe behaviors. For example, asking Tina is she currently smoked, or used illicit drugs, or had unprotected sex helps determine if she partakes in unhealthy/unsafe behaviors. Once subjective data was collected, I performed the comprehensive physical assessment, which according to Jensen (2015) should be a complete head-to-toe examination. Head/Neck: I examined the patients head/face for general appearance, symmetry, expression, etc. I assessed her skin, hair, and scalp. I estimated her eyes for equality, pupil response, eye movements, and vision; her ears, nose, mouth, and throat. I palpated her lymph nodes and carotids. I tested her neck strength and ROM. Chest: I examined the patient's chest, in the following sequence, first anteriorly, then posteriorly. First I inspected the pt position and appearance, to see if the patient appeared comfortable. Noting for any signs of respiratory distress. Then I examined the patient's chest for symmetry, size, shape, and muscle use. Next, I auscultated the patient's heart and lung sounds. After auscultation, I palpated PMI, and tactile fremitus anteriorly, and palpated posteriorly for tactile fremitus, symmetry, and expansion and palpated for CVA tenderness; Last, I percussed all lung fields. Abdomen: I examined the patient's abdomen in the following order: inspection, auscultation, percussion, and palpation to include the general appearance of ( scars, masses striae, etc.) symmetry, shape, and size. Overview Transcript Subjective Data Collection Objective Data Collection Documentation Plan My Exam Self-Reflection This study source was downloaded by 100000831988016 from CourseHero.com on 03-14-2022 06:32:59 GMT -05:00 https://www.coursehero.com/file/31663874/Comprehensive-Assessment-self-reflection-pdf/ 6/12/2018 Comprehensive Assessment | Completed | Shadow Health https://chamberlain.shadowhealth.com/assignment_attempts/3569767 2/5 Auscultation was performed of the patient's abdominal arteries, and bowel sounds. Bowel sounds were auscultated first starting at the RLQ and moving in a clockwise fashion (RLQ, RUQ, LUQ, LLQ). As were percussion, and palpation. During the assessment, the patient was told everything that was going to be done before doing it and was assessed for signs of discomfort. Upper Extremities: I examined the patient's extremities, first the upper extremities, then the lower extremities. This included general appearance (skin condition, cuts, scrapes, edema). For the upper extremities, I examined the patients ROM and strength starting at the shoulders and moving distally to till I reached the hands. I also assessed peripheral pulses, sensation to soft touch and pain, and hand movements. When at the hands, I examined the patient's fingernails, checked capillary refill, position sense of a finger, stereognosis, graphesthesia, and DTRs. Lower Extremities: Similar to the upper extremities, I examined ROM starting proximally at the hip and moved distally to the ankles. To do this, the patient was instructed to do the range of motion exercises. During range of motion, the joints and muscles are palpated, and strength was tested. This can help identify things such as arthritis, pain, tenderness, swelling, deformity or any other abnormalities. I also assessed peripheral pulses, sensation to soft touch and pain, and leg movements. When at the feet, I examined the patient's toenails, checked capillary refills, position sense of random toes, monofilaments, and Deep tendon reflexes. Body: I examined the patient's spine while standing and her balance. Once the examination was completed I was open for questions and to call the office if she had any questions or concerns. Explain the clinical reasoning behind your decisions and tasks. Student Response: Student Response: I started this exam by first collecting the health history from the patient, which is subjective data. Subjective data provides insight to the patient and can provide context to how any current problems may be related. Also, personal data collection helps to guide the physical assessment and the nursing process. "The nurse's role in collecting subjective data is to use it to improve the patient's health status and to determine the cause of the patient's current symptoms" (Jensen, 2015). For example, When asking about Tina's medical history I wanted to know if she had any conditions, and if so how long has she had them, the severity of any illness, symptoms, aggravating factors, and if she was currently receiving treatment for it. I also inquired about any allergies, what happens with exposure, the severity of allergies, and how allergies are/have been treated. Other questions I asked included a social history, such as if she smokes and for how long. This helps me to identify any personal risk behaviors Tina may participate in or any environmental risk factors that she may expose herself to. After conversing with the patient, I started to collect my objective data through physical assessment. Before performing the physical assessment, I made sure that the patient was comfortable and that her room temperature was adequate. Also, before starting the nursing comprehensive assessment, I organized my physical assessment from head to toe, instead of systems. This helps the assessment go more smoothly. For purposes of explanation, I will do it based on systems. Of note, The physical assessment is done using four techniques: inspection, palpation, percussion, and auscultation. During the assessment, the patient was told everything that was going to be done before doing it and was assessed for signs of discomfort. Once the assessment was complete, I made sure that the patient was comfortable and had everything she needed, and all of her questions were answered. Neuro- I asked Tina questions to inquire about any risk factors that she may have of developing a neurological condition, such as head trauma and any signs or symptoms of neurological or neuromuscular complications. During subjective data collection an informal neurological assessment was being performed, such as assessing the patient's speech, alertness, etc. Obtaining subjective is important because it provides insight to the patient, and to any potential or current risk factors they may have towards developing or worsening neurological disorders. It also allows for an informal neurological assessment of LOC, speech, general knowledge, etc. This can be helpful in things like determining safety hazards/risks, and when providing education. The cerebellar function was tested by having the patient do a finger-to-nose test and heel-to-shin test. Performing this test not only tests for possible cerebellar lesions/dysfunction but may also help identify safety hazards (such as being a fall risk, or needing assistance at home for an unsteady gait). Sensory function was tested to check for sensory deficits, perception so the patientsclinical situation should be considered when testing it. For example, Tina has diabetes and is more likely to have the peripheral sensory loss. Peripheral sensory from diabetic neuropathy is usually distal, whereas someone with the sensory loss caused by spinal trauma will have sensory loss specific to the area of the skin that is supplied by nerves from the affected spinal root (Jensen, 2015). Testing This study source was downloaded by 100000831988016 from CourseHero.com on 03-14-2022 06:32:59 GMT -05:00 https://www.coursehero.com/file/31663874/Comprehensive-Assessment-self-reflection-pdf/ 6/12/2018 Comprehensive Assessment | Completed | Shadow Health https://chamberlain.shadowhealth.com/assignment_attempts/3569767 3/5 sensory loss can help identify educational points, for example, Tina had a sensory loss on the balls of her feet, so following up by asking her if she performs daily feet assessments is important (Jensen, 2015). Respiratory: To assess the patient's respiratory system I asked questions regarding her respiratory status, and history. By inquiring if she has ever had a respiratory disease, it helps identify the potential for developing subsequent respiratory conditions. Tina, has asthma, which is a chronic respiratory disease in which the upper airway is overly sensitive to different environmental stimuli and allergens. This is one reason why I asked Tina if she had any allergies and what reactions she has had in the past to the allergens. Cats and dust are two of her allergies that trigger her asthma. I also asked Tina about her lifestyle choices and environment. For example, I asked her if she has ever used or smoked tobacco, because smoking poses many risks to a person's health. Smoke inhalation can irritate air passageways, and trigger asthma exacerbations. It can also lead to other respiratory conditions, such as lung cancer. Asking questions such as these, helps to identify current and potential risk factors the patient has that can have a negative impact on her health status. It also helps to identify nursing interventions and education that that can potentially benefit the patient and promote health. For the objective portion of the examination, I inspected her general appearance and position, noting [Show More]
Last updated: 2 years ago
Preview 1 out of 5 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$12.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Mar 14, 2022
Number of pages
5
Written in
Additional information
This document has been written for:
Uploaded
Mar 14, 2022
Downloads
0
Views
179