*NURSING > SHADOW HEALTH > Chamberlain College of Nursing NR 509 Gastrointestinal Documentation Shadow Health (All)
Chamberlain College of Nursing NR 509 Gastrointestinal Documentation Shadow Health
Document Content and Description Below
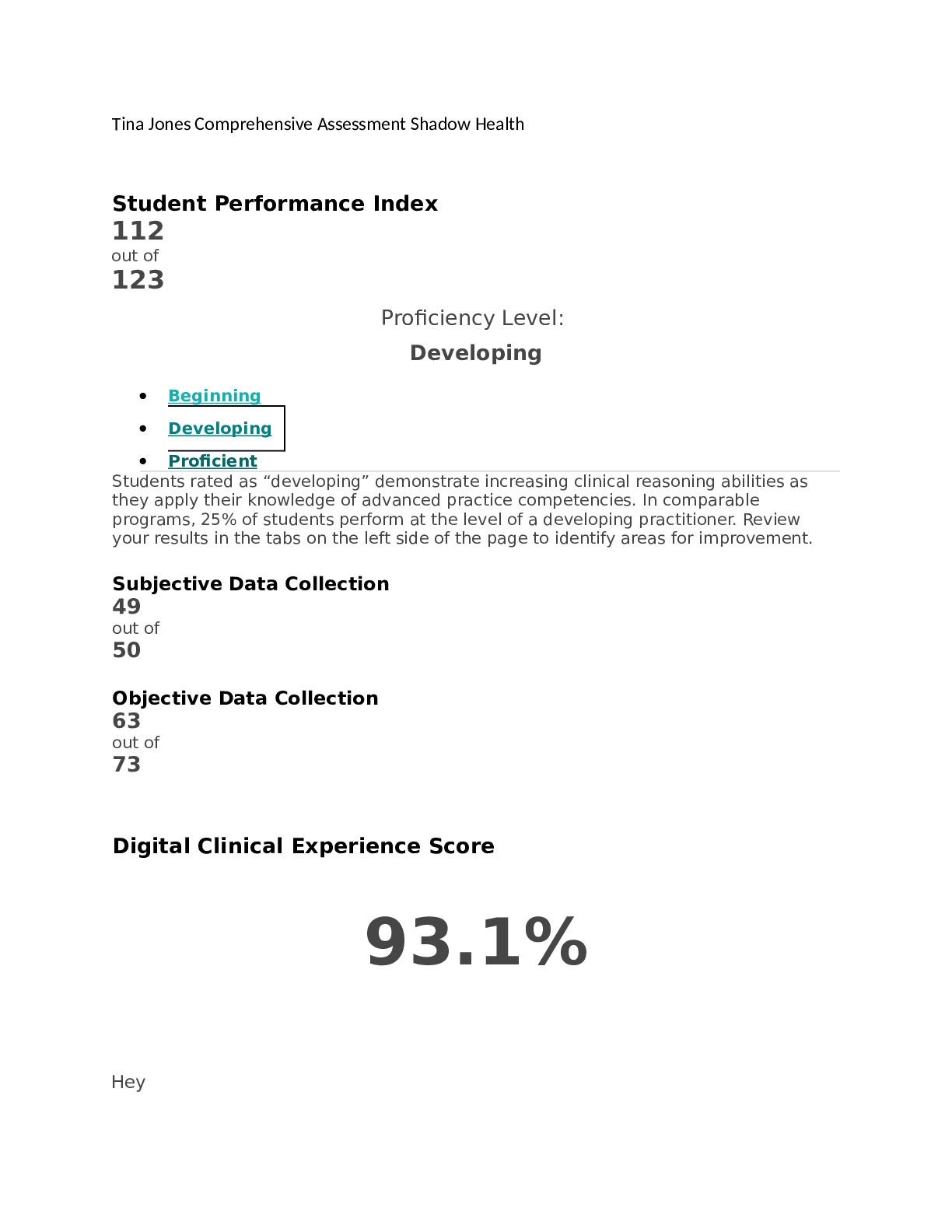
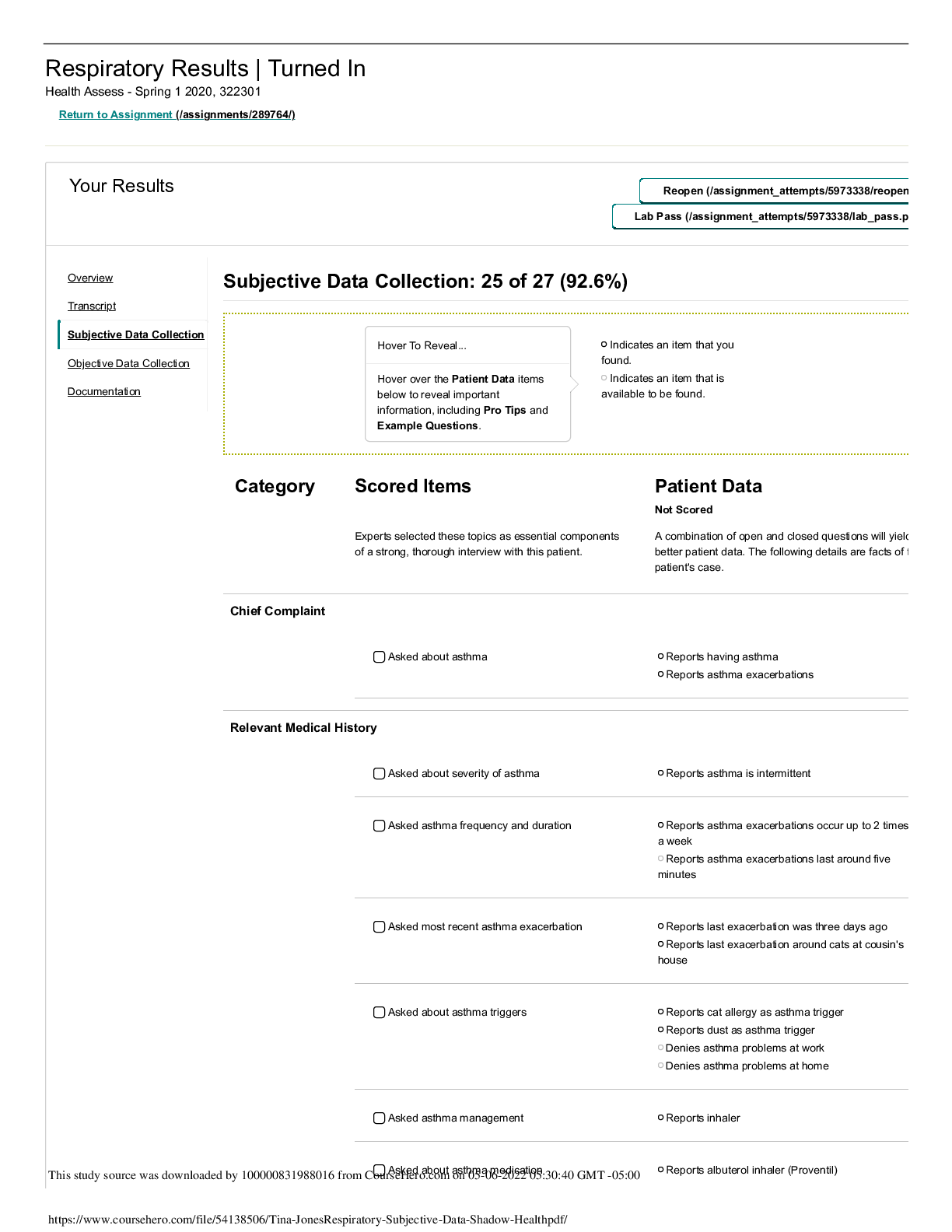
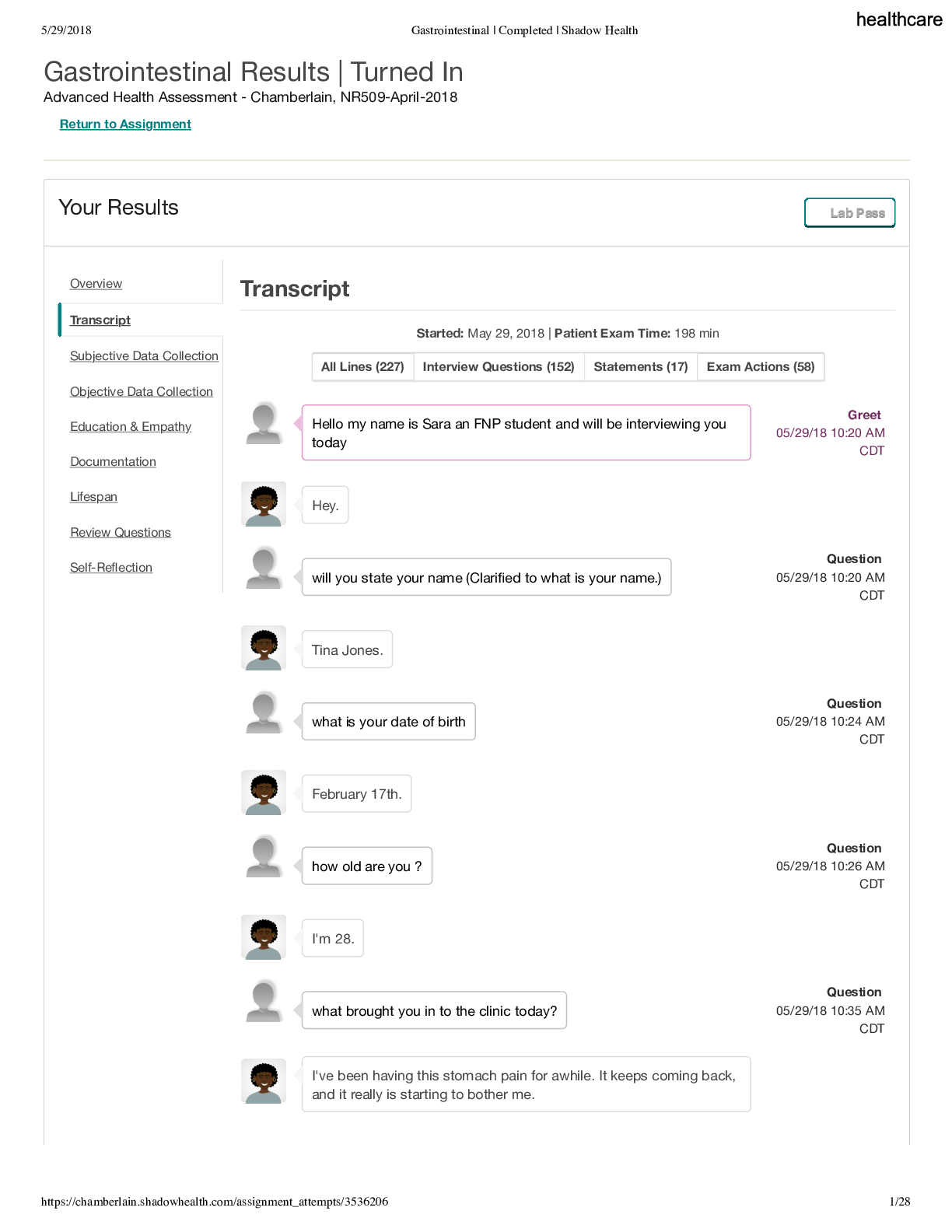
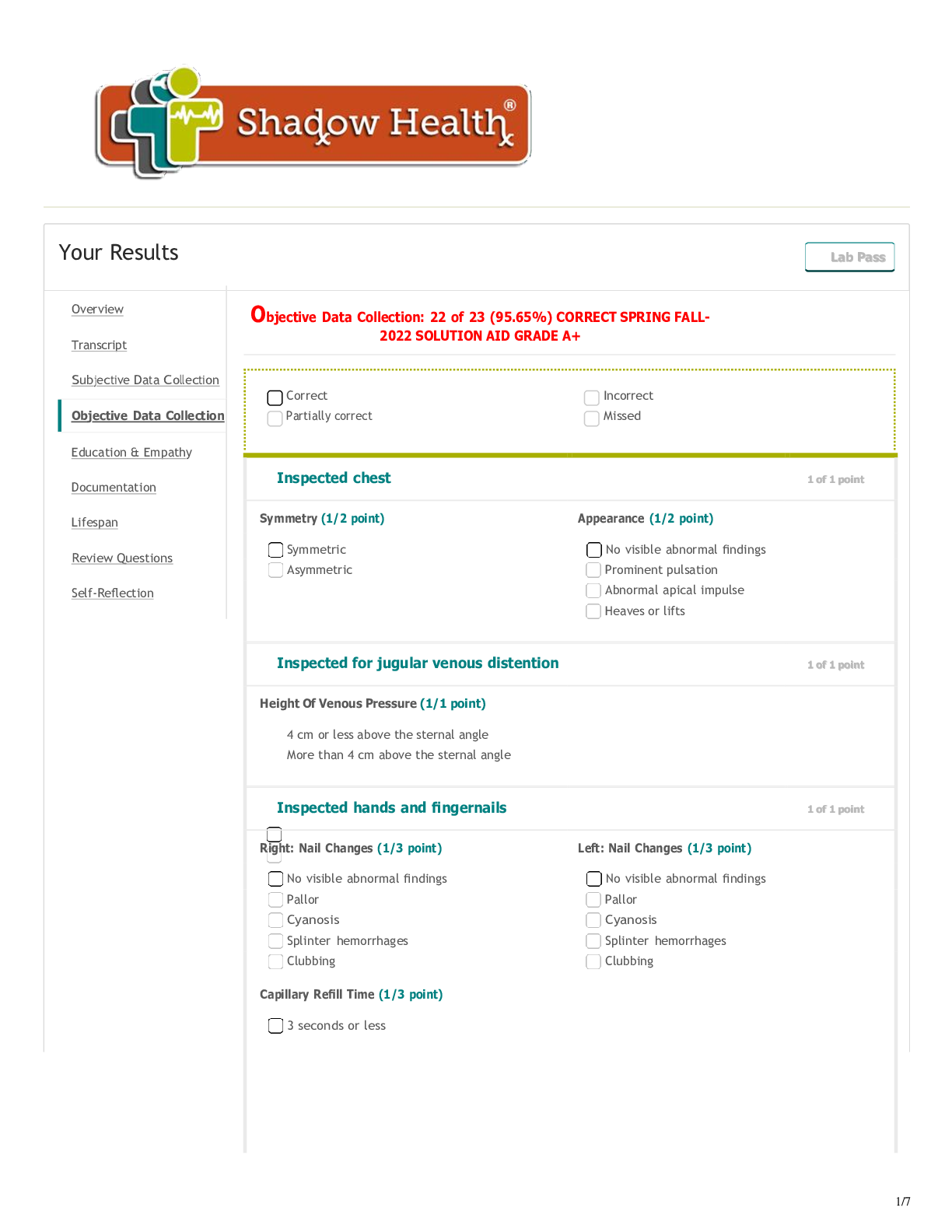
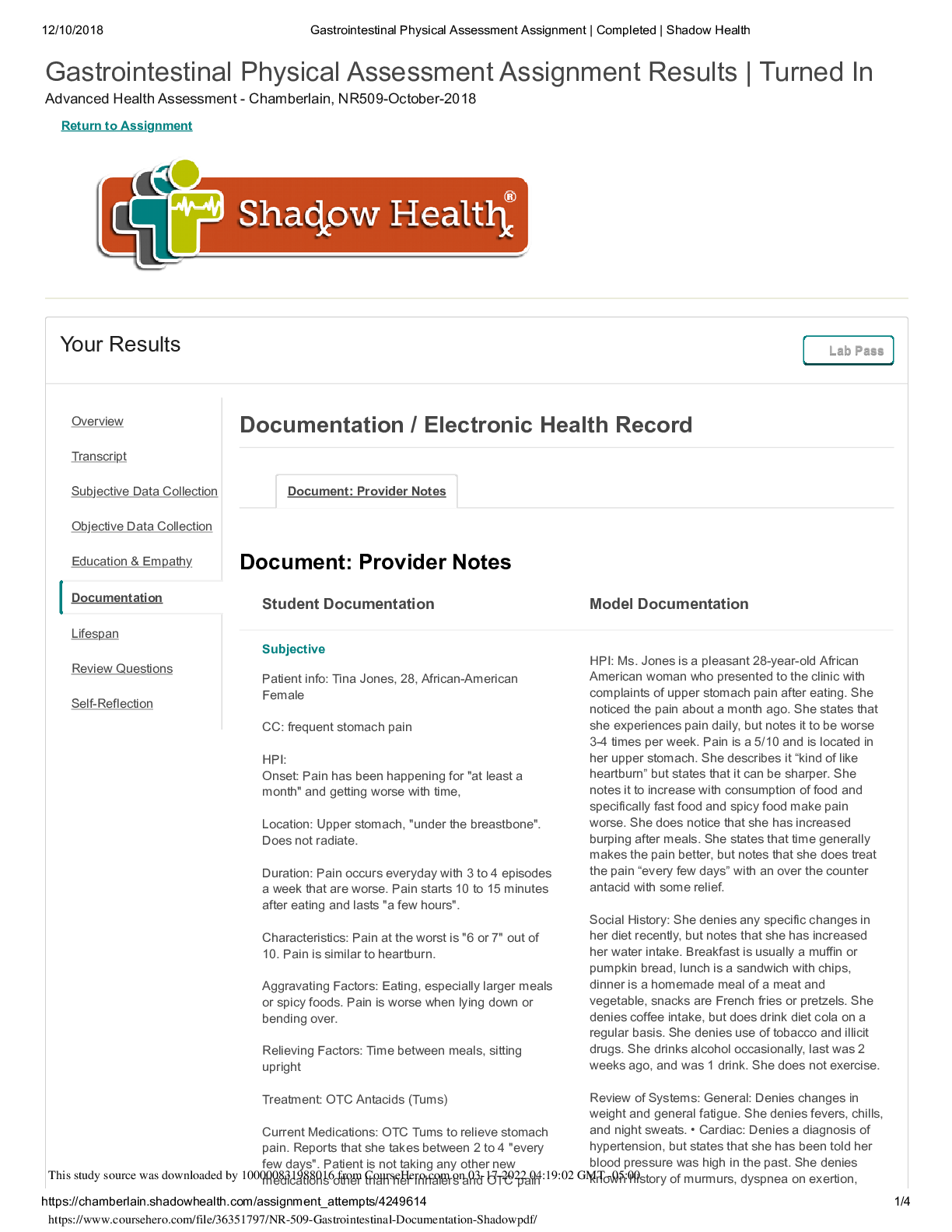
Gastrointestinal Physical Assessment Assignment Results | Turned In Advanced Health Assessment - Chamberlain, NR509-October-2018 Return to Assignment Your Results Lab Pass Document: Provider Notes... Document: Provider Notes Student Documentation Model Documentation Subjective Patient info: Tina Jones, 28, African-American Female CC: frequent stomach pain HPI: Onset: Pain has been happening for "at least a month" and getting worse with time, Location: Upper stomach, "under the breastbone". Does not radiate. Duration: Pain occurs everyday with 3 to 4 episodes a week that are worse. Pain starts 10 to 15 minutes after eating and lasts "a few hours". Characteristics: Pain at the worst is "6 or 7" out of 10. Pain is similar to heartburn. Aggravating Factors: Eating, especially larger meals or spicy foods. Pain is worse when lying down or bending over. Relieving Factors: Time between meals, sitting upright Treatment: OTC Antacids (Tums) Current Medications: OTC Tums to relieve stomach pain. Reports that she takes between 2 to 4 "every few days". Patient is not taking any other new medications other than her inhalers and OTC pain HPI: Ms. Jones is a pleasant 28-year-old African American woman who presented to the clinic with complaints of upper stomach pain after eating. She noticed the pain about a month ago. She states that she experiences pain daily, but notes it to be worse 3-4 times per week. Pain is a 5/10 and is located in her upper stomach. She describes it “kind of like heartburn” but states that it can be sharper. She notes it to increase with consumption of food and specifically fast food and spicy food make pain worse. She does notice that she has increased burping after meals. She states that time generally makes the pain better, but notes that she does treat the pain “every few days” with an over the counter antacid with some relief. Social History: She denies any specific changes in her diet recently, but notes that she has increased her water intake. Breakfast is usually a muffin or pumpkin bread, lunch is a sandwich with chips, dinner is a homemade meal of a meat and vegetable, snacks are French fries or pretzels. She denies coffee intake, but does drink diet cola on a regular basis. She denies use of tobacco and illicit drugs. She drinks alcohol occasionally, last was 2 weeks ago, and was 1 drink. She does not exercise. Review of Systems: General: Denies changes in weight and general fatigue. She denies fevers, chills, and night sweats. • Cardiac: Denies a diagnosis of hypertension, but states that she has been told her blood pressure was high in the past. She denies known history of murmurs, dyspnea on exertion, Overview Transcript Subjective Data Collection Objective Data Collection Education & Empathy Documentation Lifespan Review Questions Self-Reflection Documentation / Electronic Health Record This study source was downloaded by 100000831988016 from CourseHero.com on 03-17-2022 04:19:02 GMT -05:00 https://www.coursehero.com/file/36351797/NR-509-Gastrointestinal-Documentation-Shadowpdf/ 12/10/2018 Gastrointestinal Physical Assessment Assignment | Completed | Shadow Health https://chamberlain.shadowhealth.com/assignment_attempts/4249614 2/4 Student Documentation Model Documentation relievers for menstrual cramps that were discussed at a previous appointment. Allergies: Patient denies any new allergies other than her latex and penicillen allergy that were discussed at a previous appointment. PMHx: History of Asthma and Type II Diabetes that were discussed at a previous appointment. Hospitalized in the past, around age 16, for asthma, but no major hospitilizations or surgeries since. SociHx: Patient is a student with a strong family support system. She stated that her most recent meal was breakfast this morning. She typically eats three meals a day with snacks every so often. Her diet was described as high in carbohydrates iwth things like sandwhiches and pizza. Patient denies drinking coffee, but does drink diet soda frequently. She states that she consumes 6 to 8 glasses of water a day. Patient does not exercise. Patient does not smoke. Patient drinks alcohol infrequently. Last menstrual period was 3 weeks ago. Patient is not currently sexually active. FamHx: Patient notes that an uncle passed away from Colon cancer. Patient denies any family history of GERD, IBD, gallbladder issues, or bladder disease. Mother has high cholesterol and high blood pressure. Father had high blood pressure and high cholesterol, along with Type II diabetes. Sister has asthma. Brother is obese. ROS: General: Patient denies any fever, chills, or fatigue. No changes in weight. Respiratory: Patient denies any sore throat, coughing, or shortness of breath. Cardiovascular: Patient denies any chest pain, chest heaviness, or heart palpitations. Gastro: Patient notes increased burping. Patient denies any past history of gastro issues. Patient has a bowel movement every two days, with a normal consistency for her. No blood or mucus in stool. No pain during movements. Genitourinary: Patient notes increased amounts of urination, especially at night. Color is yellow or clear. No pain during urination. No blood in urine. Can control her bladder. Mental: Patient notes some increased stress due to school and work, but is handling it. She has some anxiety, but no more than usual. orthopnea, paroxysmal nocturnal dyspnea, or edema. • Respiratory: She denies shortness of breath, wheezing, cough, sputum, hemoptysis, pneumonia, bronchitis, emphysema, tuberculosis. She has a history of asthma, last hospitalization was age 16, last chest XR was age 16. • Gastrointestinal: States that in general her appetite is unchanged, although she does note that she will occasionally experience loss of appetite in anticipation of the pain associated with eating. Denies nausea, vomiting, diarrhea, and constipation. Bowel movements are daily and generally brown in color. Denies any change in stool color, consistency, or frequency. Denies blood in stool, dark stools, or maroon stools. No blood in emesis. No known jaundice, problems with liver or spleen. This study source was downloaded by 100000831988016 from CourseHero.com on 03-17-2022 04:19:02 GMT -05:00 https://www.coursehero.com/file/36351797/NR-509-Gastrointestinal-Documentation-Shadowpdf/ 12/10/2018 Gastrointestinal Physical Assessment Assignment | Completed | Shadow Health https://chamberlain.shadowhealth.com/assignment_attempts/4249614 3/4 Student Documentation Model Documentation Objective Tina Jones was a pleasant, 28 year old African American female. She was obese, but in no signs of visual distress. She was alert and oriented. She maintained eye contact and answered questions fully and correctly. She was dressed well and seemed to have good hygiene. Abdominal: Visua; inspection found skin turgor had no tenting. Abdomen was symmetric, protuberant, with striae and excessive hair growth around the belly button. Bowel sounds in all quadrants were normoactive. Patient did not react to CVA percussion. Spleen was tympanic. Liver was between 6 and 12 cm. No abdominal tenderness. No palpable masses in the abdomen. Liver was palpable. Spleen not palpable. Kidneys not palpable. Cardiovascular: S1 and S2 were audible with no extra sounds. Abdominal, Renal, Iliac, Femoral arteries all had no bruit. Respiratory: Symmetrical chest. Ausculatation found clear breath sounds present in all areas with no adventitious sounds. General: Ms. Jones is a pleasant, obese 28-year-old African American woman in no acute distress. She is alert and oriented. She maintains eye contact throughout interview and examination. • Abdominal: Abdomen is soft and protuberant without scars or skin lesions; skin is warm and dry, without tenting. Bowel sounds present and normoactive in all quadrants. No tenderness to light or deep palpation. Tympanic throughout. Liver is 7 cm at the MCL and 1 cm below the right costal margin. Spleen and bilateral kidneys are not palpable. No CVA tenderness. • Cardiovascular: Regular rate and rhythm, S1 and S2 present, no murmurs, rubs, gallops, clicks, precordial movements. No bruits with auscultation over abdominal aorta. No femoral, iliac, or renal bruits. • Respiratory: Chest is symmetrical with respirations. Lung sounds clear to auscultation anteriorly and posteriorly without wheezes, crackles, or cough. [Show More]
Last updated: 2 years ago
Preview 1 out of 4 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$13.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Mar 17, 2022
Number of pages
4
Written in
Additional information
This document has been written for:
Uploaded
Mar 17, 2022
Downloads
0
Views
115