*NURSING > SHADOW HEALTH > NUR 516 Focused Exam_ Abdominal Pain _ Documentation Latest 2021 Rated A (All)
NUR 516 Focused Exam_ Abdominal Pain _ Documentation Latest 2021 Rated A
Document Content and Description Below
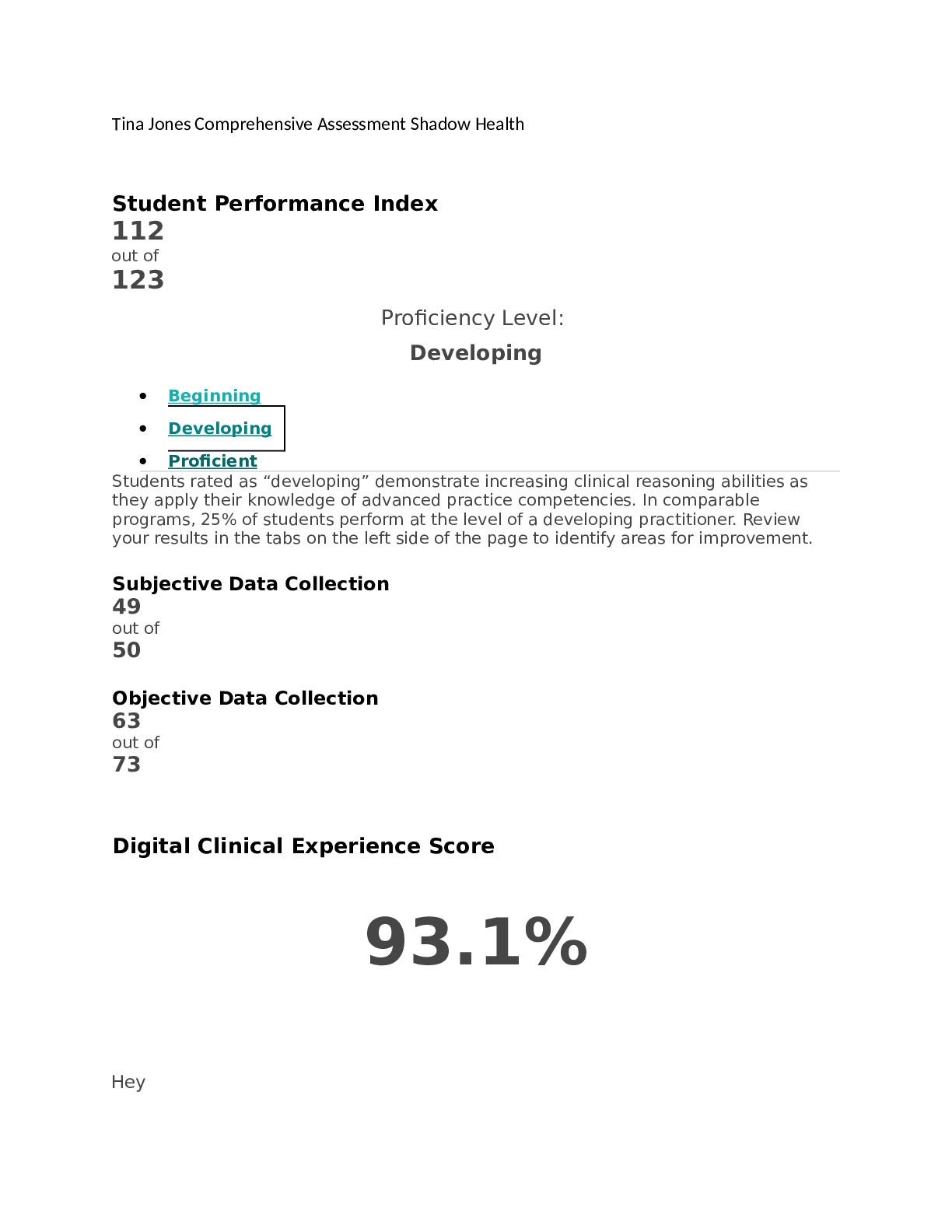
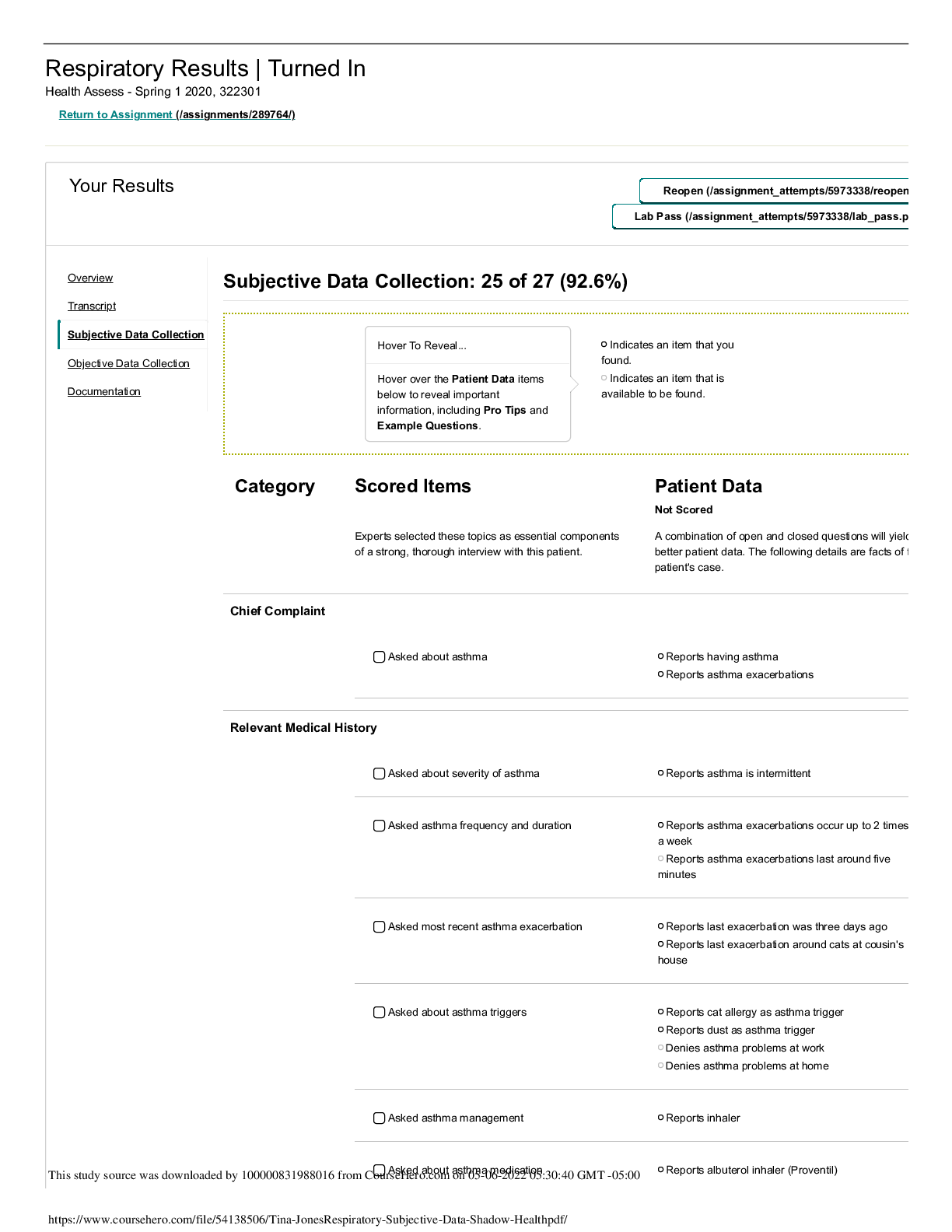
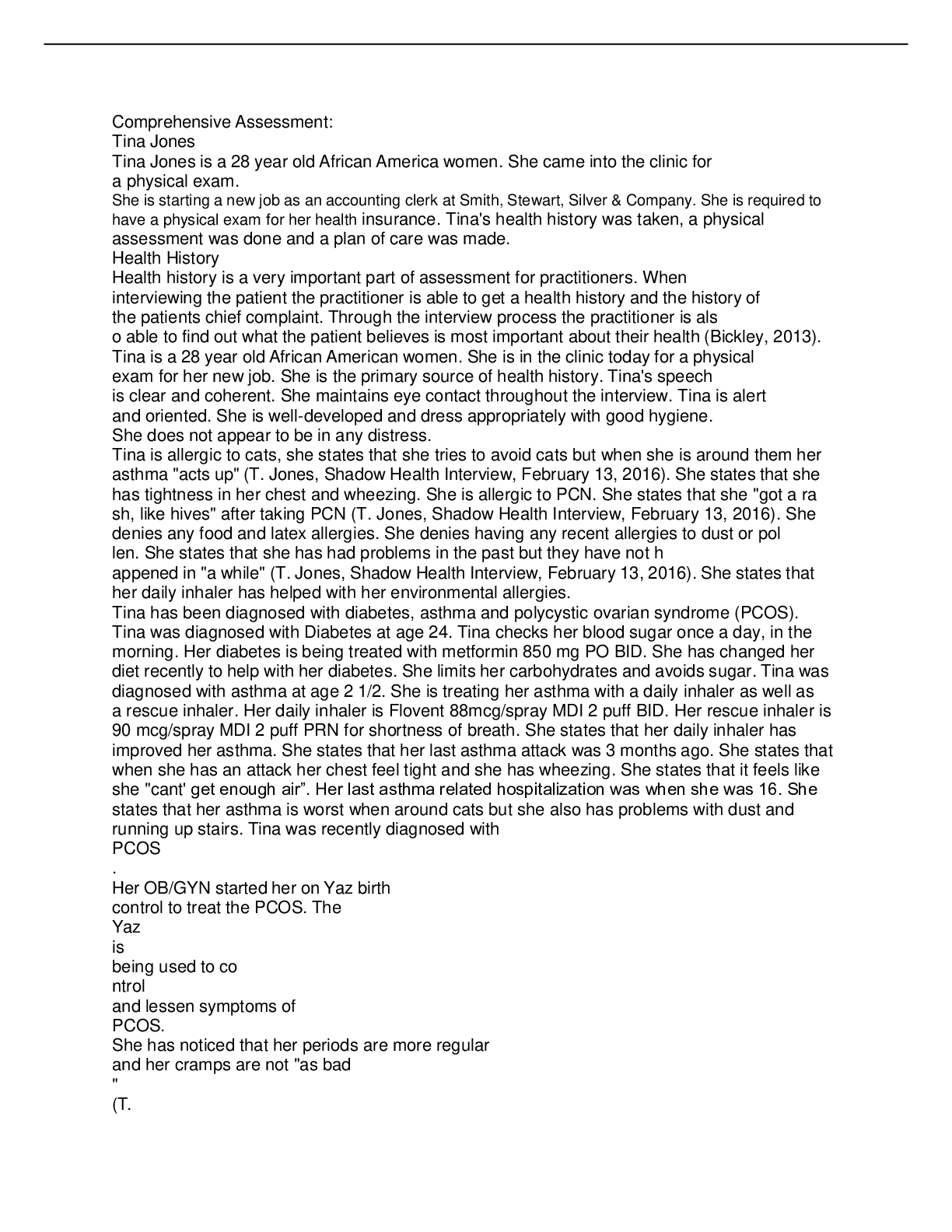
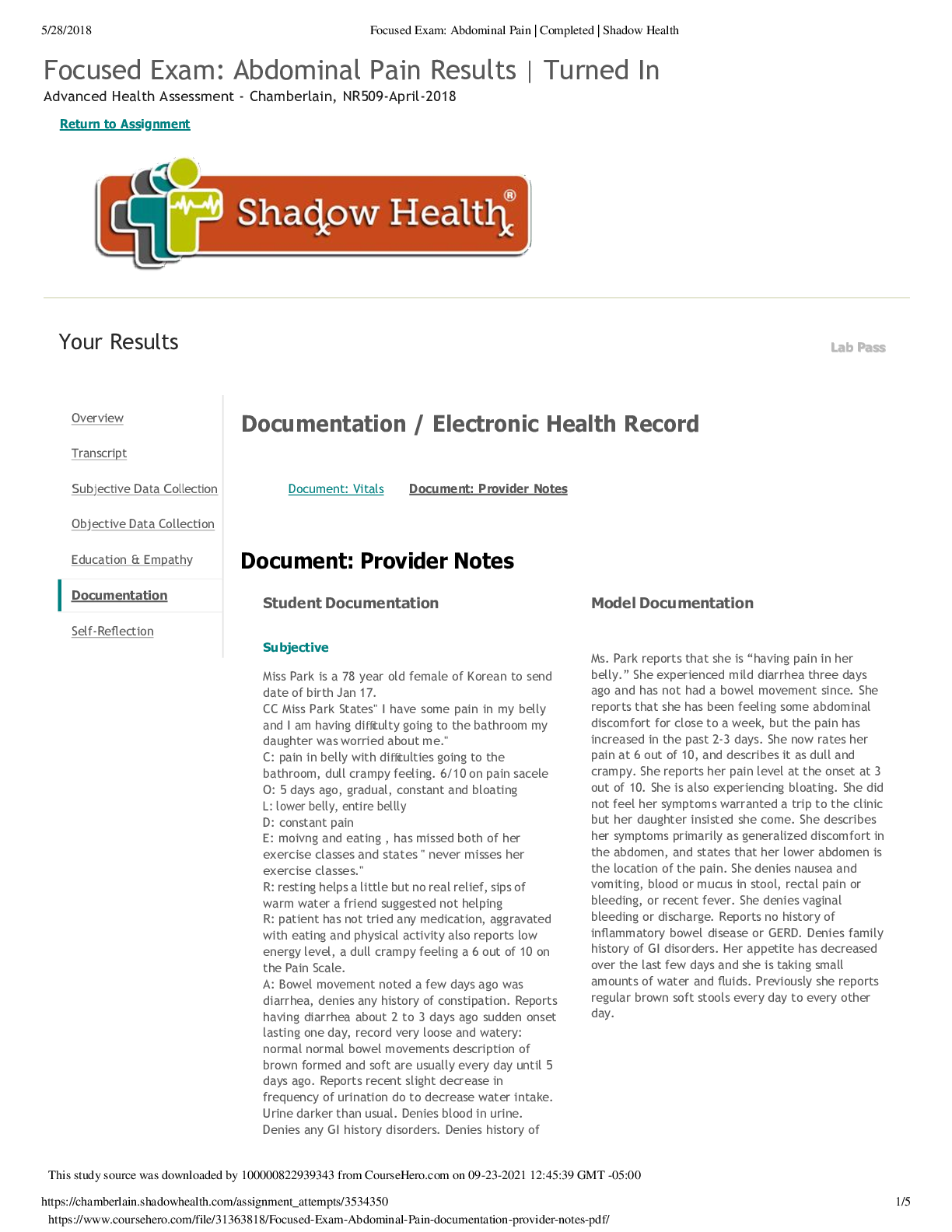
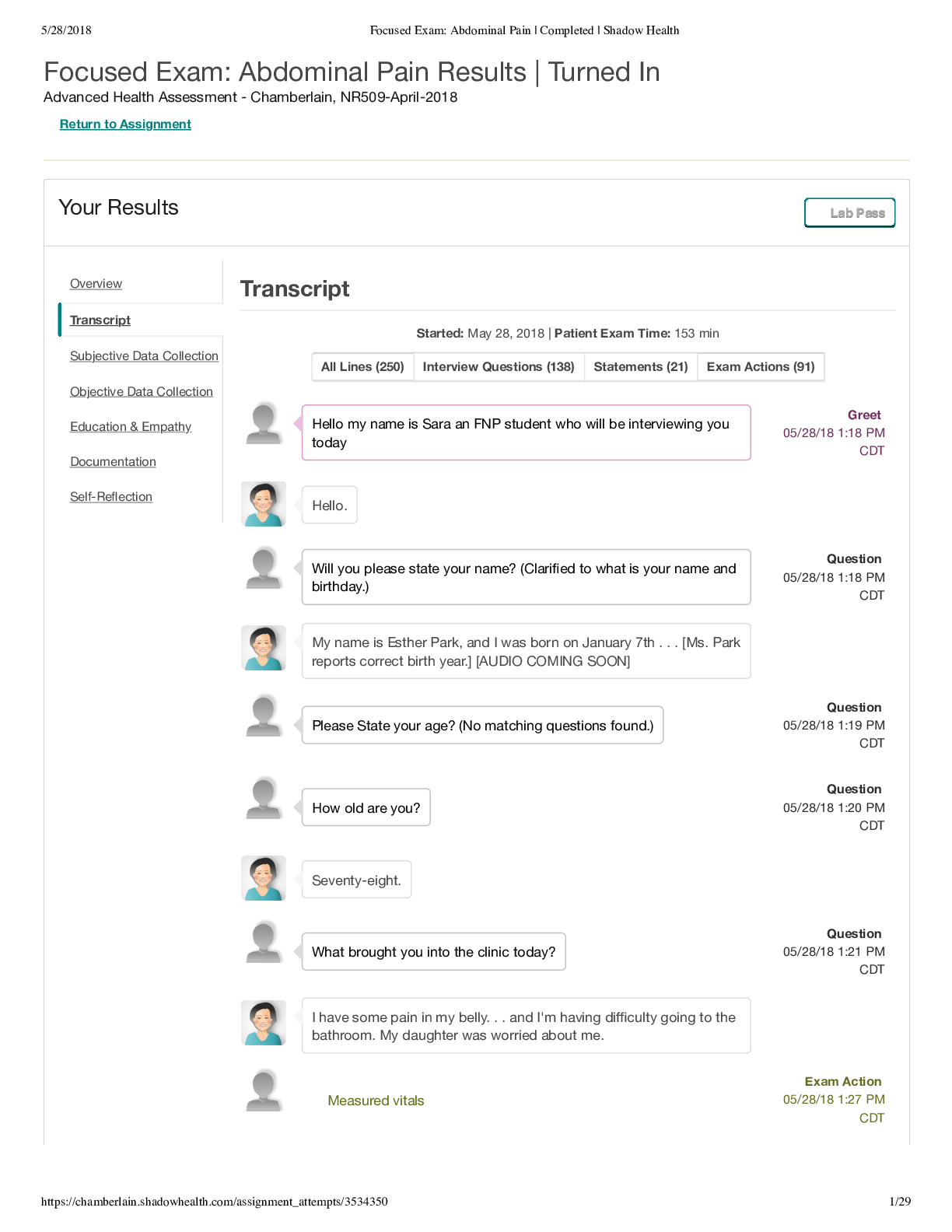
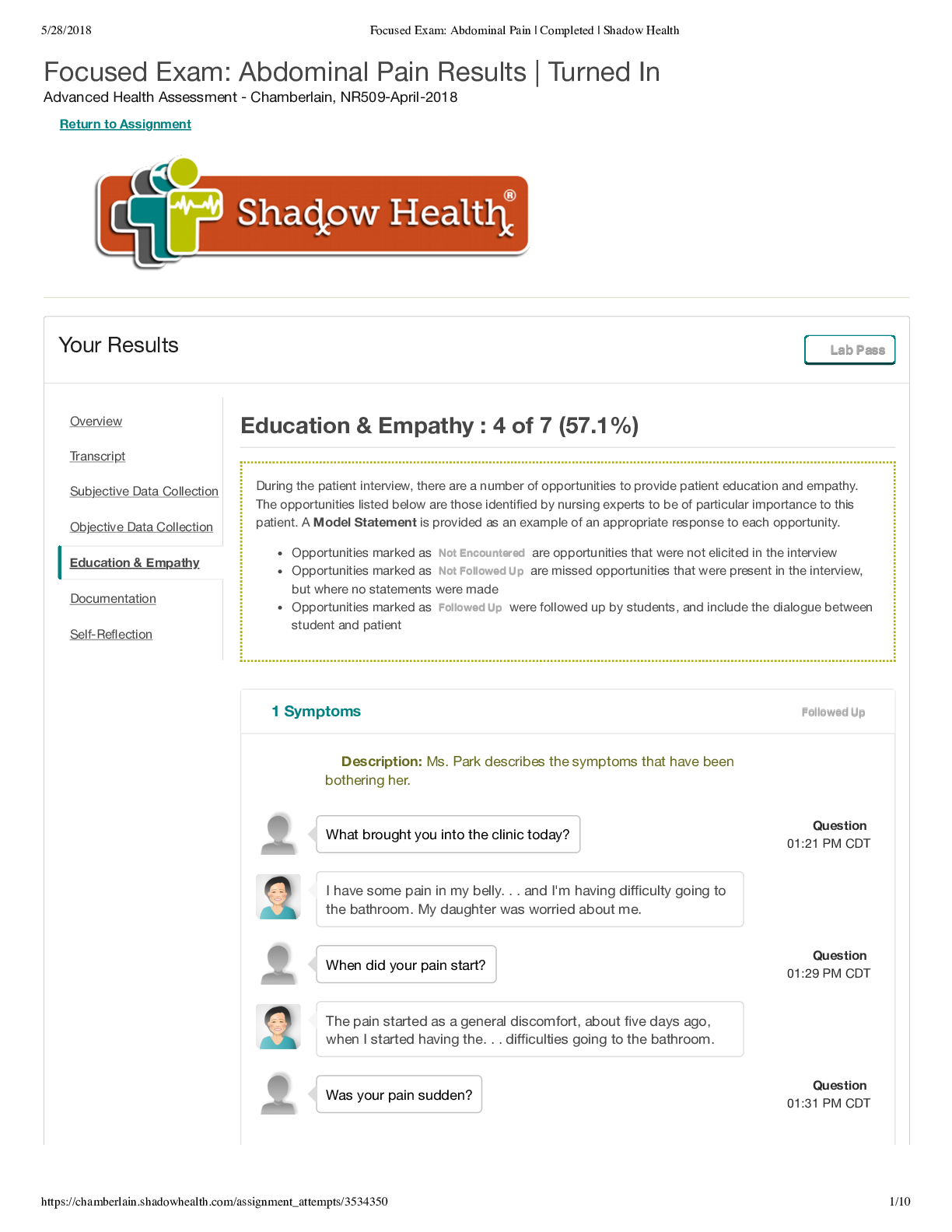
Focused Exam: Abdominal Pain Results | Turned In Advanced Health Assessment - September 2019, 2019SEP NUR-516-NG001 Return to Assignment Your Results Lab Pass Document: Vitals Document: Provider N... otes Document: Provider Notes Student Documentation Model Documentation Subjective Ms. Park is a 78 year old Korean female. HPI: Miss Park states that she has "pain in her belly...and I'm having difficulty going to the bathroom". She states that the the pain began about 5 days ago when she started having trouble going to the bathroom. Her current pain level is 6/10. The pain is low in her belly. She describes the pain as dull, crampy and constant. Her pain increases when she moves around alot or eats. Ms. Park has tried rest and taking small sips of warm water to ease the pain but she has gotten no relief. She denies recent fever or chills but states that she has low energy. Social History: Ms Park has two children. She has lived with her daughter for several years since her husband passed. Ms. Park denies a history of smoking cigarettes. She also denies the use of recreational drugs. Ms Park consumes one glass of dry white wine per week. Ms. Park's normal diet includes toast for breakfast, soup for lunch and fish or chicken with rice for dinner. She has not eaten much in the last few days. Ms Park states that she had a little chicken broth for dinner last night and toast this morning for breakfast. She usually drinks two glasses of water per day and does not drink any caffeinated beverages. Ms. Park reports that she is “having pain in her belly.” She experienced mild diarrhea three days ago and has not had a bowel movement since. She reports that she has been feeling some abdominal discomfort for close to a week, but the pain has increased in the past 2-3 days. She now rates her pain at 6 out of 10, and describes it as dull and crampy. She reports her pain level at the onset at 3 out of 10. She is also experiencing bloating. She did not feel her symptoms warranted a trip to the clinic but her daughter insisted she come. She describes her symptoms primarily as generalized discomfort in the abdomen, and states that her lower abdomen is the location of the pain. She denies nausea and vomiting, blood or mucus in stool, rectal pain or bleeding, or recent fever. She denies vaginal bleeding or discharge. Reports no history of inflammatory bowel disease or GERD. Denies family history of GI disorders. Her appetite has decreased over the last few days and she is taking small amounts of water and fluids. Previously she reports regular brown soft stools every day to every other day. Overview Transcript Subjective Data Collection Objective Data Collection Education & Empathy Documentation Self-Reflection Documentation / Electronic Health Record This study source was downloaded by 100000831988016 from CourseHero.com on 03-19-2022 14:27:51 GMT -05:00 https://www.coursehero.com/file/50721353/Focused-Exam-Abdominal-Pain-Documentationpdf/ Student Documentation Model Documentation Ms. Park usually does water aerobics and pilates but the pain this week has made her skip her classes. PMI: Ms. Park was diagnosed with hypertension at the age of 54. She does not monitor her blood pressure at home and only gets a check annually during her physical. Surgeries: Ms. Park has had two surgeries in her life. A C-section at the age of 40 and a cholecystectomy at the age of 42. Medications: Accupril 10mg q Daily. She takes it in the morning with her breakfast. Allergies: Ms Park has an allergy to latex which causes a rash. Family History: Ms. Park states that her father had occasional heartburn but no one else in her family has stomach issues. She denies family history of colon cancer, liver disease, cholecystitis, irritable bowel syndrome, kidney problems or bladder issues but she nites that her extended family is still in Korea so she cannot be certain. ROS: HEENT: Ms. Park denies any dizziness. She states but she has no problems with her vision. She did state that her hearing is not as good as it used to be but she feels that she still hears pretty well. Ms. Park does not have any sinus problems and state that she hasn't "gad a cold or any congestion all year". She denies any pain in her mouth or teeth. Ms. Park notes that she had a root canal 1 year ago. Cardiac: Ms. Park was diagnosed with hypertension at the age of 54. Respiratory: Ms. Park denies any breathing problems or shortness of breath. Gastrointestinal: Ms. Park denies a history of GERD, ulcers, appendicitis or hernia. She states that she has not had any digestive or gastrointestinal issues until now. She had her gall bladder removed 26 years ago. Ms Park has not had a normal bowel movement in almost five days. She notes that her last bowel movement was diarrhea. Ms. Park states that she is normally regular having one bowel movement a day. She denies vomiting recently but states that she feels bloated. Gynecological: Ms. Park went through menopause at the age of 54. Urinary: Ms. Park denies any issues with her kidneys, problems urinating for incontinence. She knows that her urine has been where's my mom's house a bit darker than usual and that she has not been urinating as often. Musculoskeletal: Ms. Park denies any pain in her [Show More]
Last updated: 2 years ago
Preview 1 out of 4 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$11.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Mar 19, 2022
Number of pages
4
Written in
Additional information
This document has been written for:
Uploaded
Mar 19, 2022
Downloads
0
Views
99