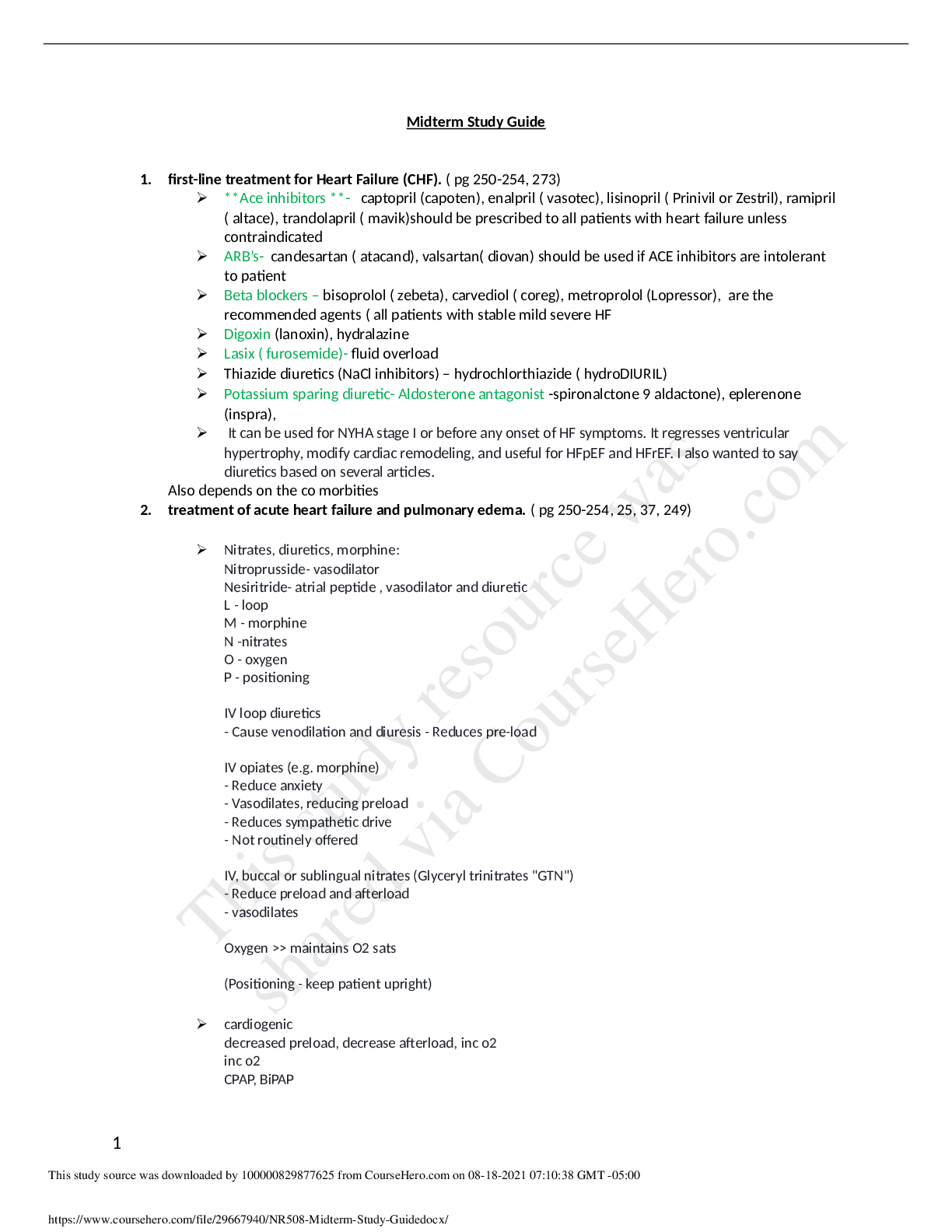
Midterm Study Guide
1. first-line treatment for Heart Failure (CHF). ( pg 250-254, 273)
**Ace inhibitors **- captopril (capoten), enalpril ( vasotec), lisinopril ( Prinivil or Zestril), ramipril
( altace), trandolap
...
Midterm Study Guide
1. first-line treatment for Heart Failure (CHF). ( pg 250-254, 273)
**Ace inhibitors **- captopril (capoten), enalpril ( vasotec), lisinopril ( Prinivil or Zestril), ramipril
( altace), trandolapril ( mavik)should be prescribed to all patients with heart failure unless
contraindicated
ARB’s- candesartan ( atacand), valsartan( diovan) should be used if ACE inhibitors are intolerant
to patient
Beta blockers – bisoprolol ( zebeta), carvediol ( coreg), metroprolol (Lopressor), are the
recommended agents ( all patients with stable mild severe HF
Digoxin (lanoxin), hydralazine
Lasix ( furosemide)- fluid overload
Thiazide diuretics (NaCl inhibitors) – hydrochlorthiazide ( hydroDIURIL)
Potassium sparing diuretic- Aldosterone antagonist -spironalctone 9 aldactone), eplerenone
(inspra),
It can be used for NYHA stage I or before any onset of HF symptoms. It regresses ventricular
hypertrophy, modify cardiac remodeling, and useful for HFpEF and HFrEF. I also wanted to say
diuretics based on several articles.
Also depends on the co morbities
2. treatment of acute heart failure and pulmonary edema. ( pg 250-254, 25, 37, 249)
Nitrates, diuretics, morphine:
Nitroprusside- vasodilator
Nesiritride- atrial peptide , vasodilator and diuretic
L - loop
M - morphine
N -nitrates
O - oxygen
P - positioning
IV loop diuretics
- Cause venodilation and diuresis - Reduces pre-load
IV opiates (e.g. morphine)
- Reduce anxiety
- Vasodilates, reducing preload
- Reduces sympathetic drive
- Not routinely offered
IV, buccal or sublingual nitrates (Glyceryl trinitrates "GTN")
- Reduce preload and afterload
- vasodilates
Oxygen >> maintains O2 sats
(Positioning - keep patient upright)
cardiogenic
decreased preload, decrease afterload, inc o2
inc o2
CPAP, BiPAP
dec preload
nitroglycerin, loop diuretics (furosemide, bumetanide)
2
dec afterload
nitroprusside, ACEi/ARB
noncardiogenic
treat underlying cause, mechanical ventilation
3. side effects of ACE inhibitors and mechanism of action of ACE inhibitors. (pg. 279, 274-275)
side effects- cough (change to an ARB) Angioedema, rash, diaphoresis, angioedema, cough,
abdominal pain, leukopenia, myalgia, headache, renal insufficiency. INCREASES creatinine,
hyperkalemia, hypotension. Teratogen (fetal renal malformations)
MOA- inhibits angiotensin converting enzyme, interfering with conversion of angiotension I to
angiotensin II. ACE inhibitors inhibit the breakdown of bradykinin a potent and naturally occurring
vasodilator by blocking the enzyme kininase II. This is thought to be the cause of the cough
commonly experienced by patients who take this class of drugs.
Uses: HTN, Chronic HF, Prevention of renal failure in diabetes
4. which antihypertensive medication classes are contraindicated in patients with asthma. (pg. 261)
Beta blockers- such as metoprolol (Toprol), carvedilol ( coreg), nadolol (corgard), penbutolol (
levatol), pindolol ( visken), atenolol ( tenormin),
Propranolol (Non-selective beta blocker)
5. mechanism of action of Digoxin. ( pg 248-255, 274t)
increases intracellular concentration of calcium which increases force of myocardial contraction
decreases activation of sympathetic nervous system
improved quality of life but no decrease in mortality
directly inhibits the Na+/K+ ATPase location in the plasma membrane, which leads to indirect
inhibition of Na+Ca2+, increase in cardiac contractility
6. uses and the mechanism of action of Penicillin. (pg. 672-673, 674)
PCN’s inhibit bacterial cell wall synthesis
Penicillins, which are bactericidal against susceptible organisms, disrupt synthesis of the bacterial
cell wall and compete for and bind to specific enzyme proteins that catalyze transpeptidation and
cross-linking. The enzymes to which they bind are called penicillin-binding proteins (PBPs). They
consist of transpeptidases, transglycosylases, and D-alanine carboxykinase and are implicated in the
final phases of building and reshaping of the bacterial cell wall while it is growing and dividing.
This action interferes with the biosynthesis of mucopeptides and prevents linkage of structural
components of the cell wall. After the penicillin molecules bind and inhibit the transpeptidase
enzymes, susceptible bacteria are no longer able to lay protein cross-links across the peptidoglycan
backbone of the cell wall. In addition to being structurally weak, this formation is thought to
catalyze the activation of autolytic enzymes in the cell wall that cause progressive bacterial lysis
[Show More]