Pediatric Gastroenteritis
UNFOLDING Reasoning
Harper Anderson, 5 months old
Primary Concept
Infection
Interrelated Concepts (In order of emphasis)
1. Inflammation
2. Perfusion
3. Fluid and Electrolyte Balance
4.
...
Pediatric Gastroenteritis
UNFOLDING Reasoning
Harper Anderson, 5 months old
Primary Concept
Infection
Interrelated Concepts (In order of emphasis)
1. Inflammation
2. Perfusion
3. Fluid and Electrolyte Balance
4. Acid-Base Balance
5. Thermoregulation
6. Clinical Judgment
7. Communication
8. Collaboration
© 2016 Keith Rischer/www.KeithRN.com
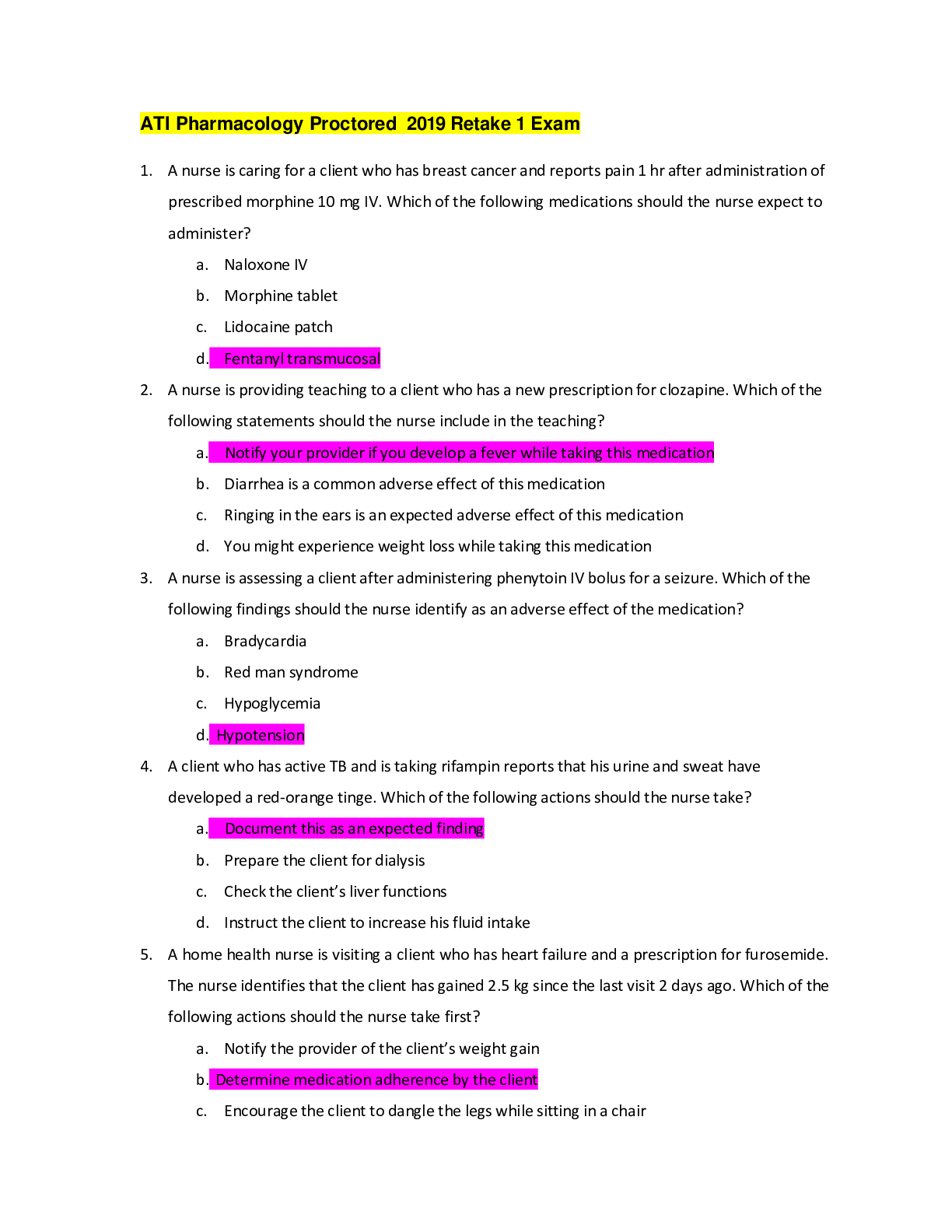
UNFOLDING Reasoning Case Study: STUDENT
Pediatric Gastroenteritis
History of Present Problem:
Harper Anderson is a 5-month-old female who was brought into the physician’s office for diarrhea and vomiting over the
past two days. She had two loose large loose stools the first day and now her mother reports that she has been less active,
is not interested in playing, and has been more sleepy today. She is unable to keep any feedings down today. She has had
four loose, watery stools and emesis x3 this morning. She has not had a wet diaper since yesterday evening. She is 25
inches (63.5 cm) in length and weighs 14 pounds, 2 ounces (6.4 kg). She weighed 15 pounds, 2 ounces (6.86 kg) at her
last office visit two weeks ago. Harper is a direct admit to the pediatric unit where you are the nurse responsible for her
care.
Personal/Social History:
Harper’s mother Nicole is 21 years old. She is a single mother and this is her first child. Nicole is not currently working
and lives with her parents. Though she has strong social support from her parents, she feels consistently overwhelmed as a
new mother.
Past Medical History (PMH):
∙ Healthy full-term infant that weighed 6 pounds 10 ounces (3.0 kg) at birth.
∙ No current health problems. Mom is no longer breast feeding and Harper is on formula.
∙ Mother had no complications with pregnancy.
∙ Has not had any immunizations from birth, including rotavirus
RELEVANT Data from Present Problem: Clinical Significance:
1. Diarrhea and vomiting over the
past two days
2. Less active, not interested in
playing
3. Unable to keep any feedings today
4. Four loose, watery stools and
emesis x3 this morning
5. No wet diaper since yesterday
evening
6. Today's weight is 14lb, 2oz. Last
office visit, 2 weeks ago, weight
was 15lb, 2oz.
The patient is presenting with signs of dehydration and
infection
RELEVANT Data from Social History: Clinical Significance:
1. Mother is 21 years old, single, and
this is her first child
2. Mother is not working and lives
with parents
3. Even with support, the mother is
consistently overwhelmed as a new
mother
Mother is young and single, this is where a support system must be
established. Mother is not working, lives with her parents, but is
constantly overwhelmed as a new mother, there may be a financial
stressor and mother may be experiencing postpartum
depression/blues.
Patient Care Begins:
Current VS: Pain Assessment – FLACC Behavioral Pain Scale
T: 102.2 F/39.0 C (axillary) Face: 1
P: 158 Legs: 0
R: 38 Activity: 1
BP: 62/42 Cry: 1
O2 sat: 95% RA Consolability: 2/Total score: 5/10
© 2016 Keith Rischer/www.KeithRN.com
FLACC Behavioral Pain Scale
0 1 2
Face Relaxed or smile Occasional grimace,
frown, withdrawn
Frequent frown, clenched jaw, quivering chin
Legs Relaxed Uneasy, restless, tense Kicking or legs drawn up
Activity Lying quietly,
moves easily
Squirming, tense Arched, rigid, or jerking
Cry No cry (awake
or asleep)
Moans, whimpers.
Occasional complaints
Crying, sobs, screams, frequent complaints
Consolability Content or
relaxed
Easy to console, distractible Difficult to console or comfort
Each of the five categories is scored from 0-2, resulting in a total of 0-10
What VS data are RELEVANT and must be recognized as clinically significant to the nurse?
RELEVANT VS Data: Clinical Significance:
1. Temperature: 102.2F
2. BP: 62/42
An elevation in temperature indicates infection and a low BP indicates
dehydration. Rest of Vital signs are WNL.
Current Assessment:
GENERAL
APPEARANCE:
Irritable when awake, alternates with lethargy once quiet, when awake and
crying, tears are not present
RESP: Breath sounds clear with equal aeration bilaterally, non-labored
CARDIAC: Skin is pale, cool to touch, cap refill 3–4 seconds in both hands, brachial
pulses palpable bilaterally
NEURO: Lethargic, does not maintain eye contact with mom or caregiver
GI: Abdomen soft with hyperactive BS x4 quadrants, no apparent tenderness
to palpation
GU: 5 mL dark amber, cloudy urine noted in urine collection bag-sent to lab
SKIN: Anterior fontanel depressed, eyes slightly sunken, lips and tongue are dry with no
shiny saliva present, when skin over abd. is pinched, remains tented for 2–3
seconds
What assessment data are RELEVANT that must be recognized as clinically significant by the nurse?
RELEVANT Assessment Data: Clinical Significance:
1. Alternates with lethargy
once quiet
2. Tears are not present when
crying
3. Skin is pale, cool to touch,
cap refill is 3-4 sec in both
hands
4. Hyperactive BS x4
Quadrants
5. 5 mL dark amber, cloudy
urine
6. Anterior fontanel depressed,
eyes slightly sunken, lips and
tongue are dry, skin is
tented for 2-3 seconds
When the patient is lethargic once quiet, and has dark amber and
cloudy urine, it is a sign of infection.
Tears not being present when crying, Skin pale, cool to touch,
capillary refill that is late, tented skin, dry lips and tongue, sunken
eyes, all indicate dehydration. Hyperact
[Show More]




.png)



 Chamberlain College Of Nursing (100 Correct Q & A.png)