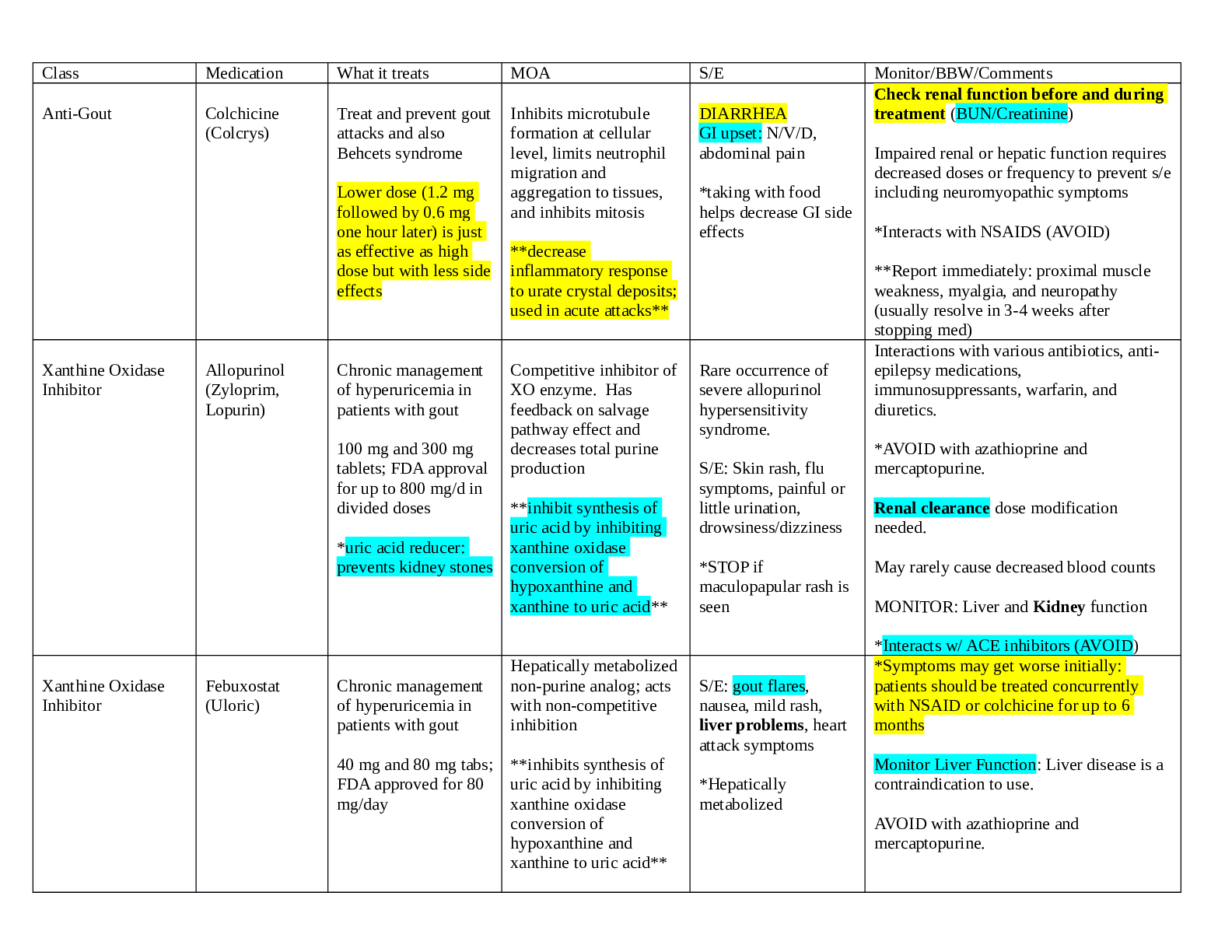
Class Medication What it treats MOA S/E Monitor/BBW/Comments
Anti-Gout Colchicine
(Colcrys)
Treat and prevent gout
attacks and also
Behcets syndrome
Lower dose (1.2 mg
followed by 0.6 mg
one hour later) is just
...
Class Medication What it treats MOA S/E Monitor/BBW/Comments
Anti-Gout Colchicine
(Colcrys)
Treat and prevent gout
attacks and also
Behcets syndrome
Lower dose (1.2 mg
followed by 0.6 mg
one hour later) is just
as effective as high
dose but with less side
effects
Inhibits microtubule
formation at cellular
level, limits neutrophil
migration and
aggregation to tissues,
and inhibits mitosis
**decrease
inflammatory response
to urate crystal deposits;
used in acute attacks**
DIARRHEA
GI upset: N/V/D,
abdominal pain
*taking with food
helps decrease GI side
effects
Check renal function before and during
treatment (BUN/Creatinine)
Impaired renal or hepatic function requires
decreased doses or frequency to prevent s/e
including neuromyopathic symptoms
*Interacts with NSAIDS (AVOID)
**Report immediately: proximal muscle
weakness, myalgia, and neuropathy
(usually resolve in 3-4 weeks after
stopping med)
Xanthine Oxidase
Inhibitor
Allopurinol
(Zyloprim,
Lopurin)
Chronic management
of hyperuricemia in
patients with gout
100 mg and 300 mg
tablets; FDA approval
for up to 800 mg/d in
divided doses
*uric acid reducer:
prevents kidney stones
Competitive inhibitor of
XO enzyme. Has
feedback on salvage
pathway effect and
decreases total purine
production
**inhibit synthesis of
uric acid by inhibiting
xanthine oxidase
conversion of
hypoxanthine and
xanthine to uric acid**
Rare occurrence of
severe allopurinol
hypersensitivity
syndrome.
S/E: Skin rash, flu
symptoms, painful or
little urination,
drowsiness/dizziness
*STOP if
maculopapular rash is
seen
Interactions with various antibiotics, antiepilepsy medications,
immunosuppressants, warfarin, and
diuretics.
*AVOID with azathioprine and
mercaptopurine.
Renal clearance dose modification
needed.
May rarely cause decreased blood counts
MONITOR: Liver and Kidney function
*Interacts w/ ACE inhibitors (AVOID)
Xanthine Oxidase
Inhibitor
Febuxostat
(Uloric)
Chronic management
of hyperuricemia in
patients with gout
40 mg and 80 mg tabs;
FDA approved for 80
mg/day
Hepatically metabolized
non-purine analog; acts
with non-competitive
inhibition
**inhibits synthesis of
uric acid by inhibiting
xanthine oxidase
conversion of
hypoxanthine and
xanthine to uric acid**
S/E: gout flares,
nausea, mild rash,
liver problems, heart
attack symptoms
*Hepatically
metabolized
*Symptoms may get worse initially:
patients should be treated concurrently
with NSAID or colchicine for up to 6
months
Monitor Liver Function: Liver disease is a
contraindication to use.
AVOID with azathioprine and
mercaptopurine.
Class Medication What it treats MOA S/E Monitor/BBW/Comments
Uricosuric Agent Probenecid
(Benemid,
Probalan)
Chronic management
of hyperuricemia in
patients with gout
500 mg tablets: FDA
approval for BID
dosing for a total dose
of 2,000 mg/day or
less
*Uric acid reducer
Blocks the transport of
acidic media across
transporters in the
kidneys
**inhibit renal tubular
reabsorption of urate
and therefore increase
excretion of uric acid via
the kidneys and decrease
serum uric acid**
S/e: frequent
urination, N/V,
headache, dizziness,
skin rash
NOT used in acute
attacks
*ENCOURAGE FLUIDS r/t risk of stone
development and possible development of
nephrolithiasis
*monitor CBC for blood dycrasias
Monitor BUN/Creatinine clearance
*do not take aspirin or salicylates
Take medication with food or milk to
decrease GI s/e
Corticosteroid Prednisone Acute gouty arthritis
RA, lupus, asthma,
allergies
Variable dosing: 35
mg/d and 0.5 mg/kg
daily dosing over 5-10
days
Inhibits gene
transcription for COX-2,
cytokines, cell adhesion
molecules, and inducible
nitric oxide synthase.
Creates multi-level
suppression of
inflammation
High BP, weight gain,
muscle weakness,
insomnia, systemic
immunosuppressant,
potential for decreased
wound healing and
increased infectious
risk, acute
development of
hyperglycemia,
increased intra-ocular
pressure, mood
changes, peripheral
edema, easy bruising
Adrenal Suppression
occurs with longterm therapy
MONITOR BLOOD SUGARS r/t causing
hyperglycemia
Patient may need vitamin supplements
(vitamin D, calcium, bisphosphonate) to
help prevent osteoporosis
After 6 months worry about osteoporosis
Report black/tarry stools and abdominal
pain
Adrenal suppression w/ long-term therapy
(malaise, myalgia, fever, HTN)
Tapering is necessary to prevent
withdrawal symptoms
If dose exceeds 1 gram, prescribe a PPI
(omeprazole)
**Do not take with active infections: may
worsen fungal infections
Class Med What it treats
MOA S/E Monitor/BBW/Comments
NSAID Naproxen
(Aleve,
Naprosyn,
Anaprox)
Indomethacin
(Indocin)
Sulindac
(Clinoril)
Aspirin
Mild to moderate pain
(375-500 mg BID)
Acute gouty arthritis
(50 mg. TID)
Acute gouty arthritis
(150-200 mg BID)
Mild to moderate
pain. (350-650 mg. q
4 hours; 500 mg q 6
hours)
RA (500 mg q 4-6 hrs;
1000 mg q 4-6. Hrs;
1950 mg bid
Heart attacks
prevention w/. 81,
162, or. 325 mg daily
Variably selective
inhibitors of the COX-1
& COX-2 isoenzymes,
leading to decreased
prostaglandin formation
and inflammatory tissue
response
**Inhibit COX activity
and prostaglandin
synthesis
S/E: may impair
renal/liver function,
N/V, rash
*Indomethacin is
associated with
depression and
psychosis
*BBW increased risk of CV events (MI,
stroke, thrombus, CV disease) and GI
bleed (increased risk for elderly and w/
increased dose)
*Drug interactions w/ Warfarin (increased
bleeding)
Encourage fluids (renally excreted)
Monitor: CBC annually when pt is on long
term aspirin therapy: if high dose-also
check salicylate level and urine pH.
Prescribe H2 blocker (ranitidine) if taking
aspirin and pt c/o heartburn
*Early sign of aspirin toxicity is tinnitus
*Avoid aspirin 1 week prior to surgery: can
cause thrombosis w/ Coumadin and
Heparin
Cautious use in CHF, HTN, PUD, Renal
dysfunction, advanced age
AVOID IN PREGNANCY
*1st line treatment for pain, especially
inflammatory pain
Analgesic and
Antipyretic
Acetaminophen
(Tylenol)
Mild to moderate pain
(< 3g/day in elderly or
with liver issues
<4 g/d)
*max dose is now 2
g/d. (was 4 g/d)
Highly selective cox-2;
inhibit central and.
Peripheral prostaglandin
synthesis
Serious s/e:
hypersensitivity rxs,
kidney damage,
anemia,
thrombocytopenia,
angioedema, SJS, and
liver damage
Metabolized by the
liver
*Toxic to liver in large doses
*do not give to patients’ w/ liver
disease/alcoholics
*In overdose, contact poison control; if
ingestion is more than 150 mg/kg or
unknown, obrtain serum acetaminophen
level (>300mg/mL liver damage has
occurred)
*tx Gastric lavage w/in 4 hours and oral nacetylcysteine is specific antidote
Class Medication What it treats MOA S/E Monitor/BBW/Comments
Biguanides Metformin DM2
*also lowers
cholesterol,
triglycerides, and can
aid in weight loss
*1st line for adults and
children >10
Decrease hepatic
glucose production,
decrease intestinal
absorption of glucose,
and improve insulin
sensitivity by increasing
peripheral glucose
uptake and utilization
S/e: N/V/D
*Diarrhea is BIG s/e
Take with food to decrease GI s/e
MONITOR renal function (serum
creatinine initially, then annually
C/I: renal disease or dysfunction, metabolic
acidosis (Can cause lactic acidosis)
*hold 48 hrs after radiological studies
*can reduce B12 and reduce TSH
Sulfonylureas *RIDES
Glimepiride,
chlorpropamide,
glipizide,
glyburide
DM2
(Drug recommended
for older adults w/
DM2, is 3rd generation
Sulfonylureas)
Decrease BG by
stimulating insulin
release from pancreatic
beta cells
Hypoglycemia, weight
gain, GI upset,
hemolytic anemia,
agranulocytosis,
leukopenia,
thrombocytopenia
*glipizide causes
diarrhea
MONITOR: CBC if c/o fever/sore throat
Take with food except glipizide. (don’t.
take with food)
*This class is usually added to metformin
for additive therapy (Step 2 therapy b/c
significant risk of hypoglycemia)
C/I: sulfa allergy, hypersensitivity type I,
infections/trauma
Alpha-Glucosidase
Inhibitors
Acarbose,
miglitol
DM2
(50-100 mg taken @
1
st bite of each meal.
Few people can
tolerate more than 300
mg/day)
Inhibits absorption of
carbs, decreases amount
of glucose available for
absorption
s/e: flatulence,
diarrhea, abdominal
pain (decrease dose if
s/e occur)
Monitor serum creatinine and serum
electrolytes
C/I: IBD
Take with first bite of each meal
*used as adjuvant medication
Thiazolidinediones
(TZD)
*GLITAZONES
Rosiglitazone
(Avandia)
Pioglitazone
(Actos)
DM2
Off label use to tx
PCOS
Decrease insulin
resistance and improve
insulin sensitivity
S/e: WATER
RETENTION, edema,
heart failure
*BBW: bone fracture
possible
BBW: cardiotoxicity, bladder cancer
C/I: Class 3 or 4 HF
Actos can cause bladder cancer if taken >1
yr
*Can cause bone fractures
Monitor Weight
Watch carefully in patients with decreased
ventricular function
*Do not initiate when ALD> 2.5 the upper
limit of normal.
Use back up birth control w/ Pioglitazone
Meglitinides *GLINIDES
Repaglinide
Nateglinide
DM2 Close ATP-dependent
potassium channels in
the beta cell membrane
by binding at specific
receptor sites which
depolarizes the beta cell
and leads to an opening
of the calcium channels
which increases the
secretion of insulin.
AKA: Stimulates
pancrease to produce
more insulin
S/e: hypoglycemia
(less likely b/c shorter
½ life), weight gain
*take at start of meal and do NOT take if
meal is not eaten
*do NOT take at bedtime
Dipeptidyl
Peptidase-4
Inhibitors (DPPD-4)
*GLIPTINS
Sitagliptin,
alogliptin,
linagliptin,
sitagliptin
DM2 Blocks DPP4 by
increasing incretin
levels. Increase incretin
levels (GLP-1 and GIP)
which inhibits glucagon
release, which increases
insulin secretion,
decreases gastric
emptying, and decreases
BG
NO major s/e
NO hypoglycemia, no
weight gain
ADVANTAGE of this
drug is LOW risk of
hypoglycemia
Gliptin and metformin are best for
patients w/ high cholesterol
Administration of gliptin w/ ACE inhibitor
increase risk of angioedema
Monitor renal function
Digoxin has increased concentration when
given with a gliptin
Caution use in renal disease
Glucagon-like
Peptide Agonists.
(GLP-1 Agonists)
*TIDES
Exenatide
(Byetta),
liraglutide
(Victoza),
Trulicity
DM2
*adjunct therapy w/
metformin or
sulfonylureas or both
*reduces blood
pressure
*reduces triglycerides
Acts on the incretin
system and binds to
GLP-1 receptors.
GLP-1 agonists mimic
GLP-1 hormone and
bind to GLP-1 receptors
to slow gastric emptying
and stimulate insulin
release.
*increase insulin
secretion from beta cells
and suppress glucagon
release from the alpha
cells and slows gastric
emptying
Has lower risk. Of
causing hypoglycemia
S/e: GI, weight loss
Byetta: Administer 60 min before meal
BID at lease 6 hours apart
Avoid concurrent use w/ digoxin,
lovastatin, and warfarin (monitor digoxin
and INR levels)
C/I: GI disease
Cautious use in patients with renal
impairment or end-stage disease
*monitor renal function, thyroid, and
pancreas
Selective Sodium
Glucose Cotransporter Inhibitors
(SGLT-2)
*FLOZINS
Canagliflozin
(Invokana),
Dapagliflozin
(Farxiga),
Emagliflozin
(Jardiance)
DM2
(used alone or in
combination w/
metformin or other
diabetic meds)
Inhibition of SGLT-2 to
prevent reabsorption of
glucose and facilitate
glucose excretion in
urine. Lowers the
threshold for glucosuria
and spills sugar into the
urine at 140 instead of
180, thus there is less
reabsorption of sugar
into the body
s/e: yeast infections,
UTIs, increased
urination, kidney
problems-renal
insufficiency,
hypoglycemia,
hyperkalemia, GI
upset, fatigue, urinary
discomfort, and
weight loss
Increase LDL
C/I in patients w/ kidney disease or on
dialysis
BBW: Necrotizing fasciitis of the perineum
*Do not take canagliflozin w/ primizide
*Monitor patients on digoxin
Canagliflozin can increase effects of ACE
inhibitors and ARBs.
Monitor renal function and potassium
levels frequently
Amyline Agonist Pramlintide
(Symlin)
DM1 and DM2
Synthetic analogue of
human amylin:
Acts on glucagon
secretion, slowing
emptying and
suppression of appetite
Decreases BG after
meals
S/e: increased risk of
hypoglycemia w/
insulin
C/I: hypoglycemia unawareness, and
confirmed gastroparesis
BBW: increased risk of hypoglycemia
when used in combination with insulin
*Give immediately prior to each meal
Rapid Acting Insulin Lispro
Aspart
Novolog
Humalog
DM 1 & DM2
RAI: Onset: 15 min
Peak: 1 hours
Duration: 3-5 hours
SAI: Onset: 30 min
Peak: 2-3 hours
Duration: 4-6 hours
IAI: Onset: 1 hours
Peak: 4-10 hours
Duration: 10-16 hours
LAI: Onset: 1 hour
Peak: none
Duration: up to 24
hours
Insulin binds to a
glycoprotein receptor on
the surface of the cell.
**Insulin increase
peripheral glucose
uptake by skeletal
muscle and fat
S/E: hypoglycemia,
hypokalemia
*when switching from NPH to Glargine,
decrease dose by 20% to avoid
hypoglycemia
* Newer premixed insulins work better to
decrease hgb A1C than long-acting insulins
*when mixing insulin, mix clear to cloudy
Short Acting Insulin Regular
Humalin R
Novalin R
Intermediate Acting
Insulin
NPH (QD or
BID dosing)
Long Acting Insulin Glargine
Detemir
Levemir
Thyroid
Replacement
Levothyroxine
(Synthroid,
Hypothyroidism (high
TSH, low TH)
Synthetic T4 hormone,
also to prevent recurring
S/e: hyperthyroid s/s
Increased HR,
CI: recent MI
Levoxyl, T4),
Liothyronine
(Cytomel T3)
thyroid cancer. increased O2 demand
on the heart, A-flutter,
A-fib, chest pain,
tremors, nervousness,
insomnia, irritability,
N/V/D, weight loss,
menstrual irregularity,
heat intolerance
Elderly: monitor for tachycardia and
angina
Take 30 min before food on empty stomach
Do not take OTC thyroid preps
Labs to monitor: Free T4/TSH every 4-8
weeks after starting then at 6 months then
at 12 months
Long term use and high doses associated
with decreased bone density
Thyroid replacement during pregnancy
requires dose increases and monitoring
*teach pt to HOLD if pulse >100
Do not change brands-would need dose
adjustments and lab monitoring
Antithyroid Agents Propylthiouracil
(PTU)
Hyperthyroidism Inhibits TH synthesis.
Works in thyroid and
peripherally
S/e: agranulocytosis
(report fever/sore
throat-CBC),
vasculitis, temporary
alopecia, aplastic
anemia
BBW for PTU: liver failure-report
headache, malaise, weakness, yellowing of
skin or eyes
Monitor CBC w/ diff, liver function-prior
to treatment
Safer in pregnancy
Monitor lithium and warfarin levels closely
Antithyroid Agents Methimazole Hyperthyroidism
Toxic Goiter
Thyroid synthesis
inhibitor
ONLY works in the
thyroid
s/e: agranulocytosis,
vasculitis,
hepatotoxicity,
pancreatitis, jaundice,
pruitis, dark urine,
acholic stools,
abdominal pain,
fatigue, fever
(report and stop
immediately if s/s
agranulocytosis)
*Preferred in all patients w/ Graves disease
except in 1st trimester b/c it is teratogenic
(aplasia cutis) NOT SAFE IN
PREGNANCY
*May have to take for 6-12 months before
in an euthyroid state
*Started in higher doses (10-20 mg daily)
to restored euthyroidism followed by
maintenance 5-10mg daily
*may need a beta blocker to decrease
cardiac rate
*monitor T3/T4 after 4 weeks of starting
treatment then every 4-8 weeks until
euthyroid state then every 3-4 months
*CBC w/diff (fever/sore throat/rash)
ACE Inhibitors
“prils”
Captopril-short
½ life
Lisinopril
HTN
Diabetic patients with
Works on RAAS to
decrease AgII and
Aldosterone, facilitates
S/E: dry hacking
cough, hypotension
Monitor renal function, LFTs, and
electrolytes (check K+ levels prior to
starting and w/in 1 week)
Enalapril
Wuinapril
Ramipril
cardiovascular disease
(HTN)
Reduce adverse
effects of diabetes on
the kidneys-slow the
onset of diabetic
neuropathy in patients
w/ microalbuminuria
and DM1
breakdown of
bradykinin to decrease
bp and protect kidneys
*Act on AT1 and AT2
receptors by decreasing
AgII production
Rare/Serious S/e:
angioedema-increased
risk when coadministered with
gliptins
Drug interactions: may increase lithium
levels leading to lithium toxicity
Avoid NSAIDS-reduce effect r/t increased
sodium retention
Alcohol increases hypotension
Take 1 hour apart from antacids-inhibits
absorption
Decrease ACE dose in creatinine >2.5
C/I: Bilateral renal artery stenosis,
pregnancy, and angioedema
If dry hacking cough develops, switch to
ARB
Discontinue diuretics 2-3 days before
starting on an ACE inhibitor if potassium
depleting r/t risk of hyperkalemia
Angiotensin receptor
blockers (ARBs)
“sartins”
Losartan
Valsartan
HTN Block binding of
angiotensin II to the AT1
receptor on cell
membrane
Similar s/e profile of
ACE inhibitors
C/I: bilateral renal artery stenosis,
pregnancy, angioedema, hyperkalemia
Monitor renal/hepatic function, and
electrolytes (K+ level prior to starting and
1 week after)
Does NOT increase bradykinin so no dry,
hacking cough
Avoid NSAIDS
Give antacids 1 hour apart
Calcium Channel
Blocker (CCB)
Amlodipine
Felodipine
Amlodipine is used
for HF and chest pain;
also good for LV
Mainly affect arterial
vascular smooth muscle
and lower blood
S/e: hypotension with
beta blocker &
amlodipine
CCBs first line treatment for African
Americans
Dihydropyridines
“Pine”
Isradipine
Nifedipine
Nicardipine
Nimodipine
nitrendipine
failure & HTN pressure by causing
vasodilation
Block the influx of
calcium
Reduce afterload
significantly and reduce
the force of contraction
Do not work on heart,
only work on
vasculature
Amlodipine increases
blood flow to the heart
to relieve angina
PERIPHERIAL
EDEMA
Reflex tachycardia
Photosensitivity,
dizziness, headache,
hypotension, syncope,
peripheral edema,
palpitations, flushing,
optic neuritis,
bradycardia,
constipation
Can worsen proteinuria in patients with
peripheral neuropathy
Can increase edema of hands and feet
No grapefruit juice-increases amlodipine
levels
Check TSH and Free T4 with Amlodipine
Report any eye problems to provider
immediately (optic neuritis)
Check TSH every 6 months if patient has
hypo/hyperthyroidism
Do not give nifedipine in angina (reflux
tachycardia)
Calcium Channel
Blocker (CCB)
Nondihydropyridine
s
Diltiazem
Verapamil
Hypertension
Angina
Arrhythmias
Esophageal disorders
Verapamil can treat
migraines
Verapamil decreases
workload-do not give in
HF: use for angina: also
used to tx SVT
Diltiazem: decrease
workload and HR, and
causes vasodilation:
used for arrhythmias
S/E Verapamil:
bradycardia, heart
block, constipation
S/E: hypotension,
dizziness, headache,
syncope, can worsen
or lead to HF
Do not take verapamil with statins (risk of
myalgia) or in patient’s w/ HF (can worsen
HF)
Do not give with beta blocker; give with
ACE inhibitor to decrease proteinuria in
DM patients
C/I unstable angina r/t risk of tachycardia
Avoid use after Mi, avoid in patients with
peripheral edema; hepatic impairment,
pregnancy category c; avoid in lactation
Monitor LFT prior to starting therapy and
during therapy
Change positions slowly, avoid exercise in
hot weather
Cardiac Glycoside Digoxin HF and A-fib, Aflutter, slows HR
Strong, highly selective
inhibitor of sodiumpotassium-adenosine
S/E: Gi (N/V/D),
anorexia, fatigue,
disorientation,
Crosses placenta and BBB
C/I: renal impairment and AV blocks;
triphosphatase system
Increase cardiac output
and causes ventricles to
empty more completely.
Digoxin reduces the
ventricular rate
hallucinations, visual
disturbances
Toxicity S/S: GI,
visual disturbances
(yellow vision/green
halos), atrial
arrhythmias, AV
blocks, PVCs
pregnancy category C
Not 1st line
Cautious use and monitor electrolyte
abnormalities (K+, Ca+, and Mg) b/c will
worsen toxicity
Cautious use in elderly r/t renal function
and protein levels (require slower
digitalization and careful monitoring)
Toxicity levels > 2mg/mL (elderly at
increased risk for toxicity)
Monitor renal function and digoxin levels
Eat high potassium diet-milk 1 hour later;
high fiber may decrease absorption
Take at same time each day; report s/s
toxicity and worsening HF and to check
pulse
Do not take w/ verapamil, amiodarone,
erythromycin, epinephrine
Hypokalemia leads to dig toxicity
Antiarrhythmics
Class I: Sodium
channel blockers
1a:
procainamide
and Quinidine
1b: lidocaine
SVT and ventricular
arrhythmias
1a: lengthens the
duration of the action
potential and reduces the
duration of the action
potential
1a S/e: N/V, increased
HR, widened QRS,
prolonged PR & QT,
lupus like syndrome,
hypotension,
Procainamide has a short ½ life and it
needs to be dosed every 3-4 hours
1a drugs: Monitor for CHF if administered
after MI/ACS (Difficulty breathing,
1c: flecainide,
propanfenone
bradycardia
1b S/e: drowsiness,
confusion, CV
depression
1c S/e: may
exacerbate
arrhythmias,
malignant
arrhythmias, dizziness,
fatigue
peripheral edema, JVD)
With procainamide, there is a chance of
systemic lupus erythematosus development
Monitor CBC and ANA
Procainamide may lead to drug induced
fever
Antiarrhythmics
Class II: Beta
receptor blocker
“olol”
Propranolol
Metoprolol
Hypertension Blocks beta-receptors in
the heart causing
decreased HR,
decreased force of
contraction, and
decreased rate of AV
conduction
s/e: bradycardia,
lethargy, GI
disturbances, CHF,
hypotension,
depression
Contraindicated in asthma
Antiarrhythmics
Class III: Potassium
channel blocker
Amiodarone
Sotalol
SVT s/e: N/V, taste
disturbances,
bradycardia, heart
blocks, dysrhythmias,
prolonged QT,
hepatitis,
hypo/hyperthyroidism,
interstitial lung
disease, pulmonary
fibrosis Blue colored
skin, optic neuropathy,
eye problems
No grapefruit juice (metabolism issues)
Not used in pregnancy
Monitor chest x-ray, pulmonary function
every 3-6 months
Inhibits enzyme that converts T4T3
Monitor TSH every 6 months
Skip missed doses
Antiarrhythmics
Class IV: Calcium
channel blocker
Verapamil
Diltiazem
Nifedipine
Cardizem
See above See above
Peripherial edema
Facial flushing
See above
Nitrates Glyceryl
trinitrate
Nitroglycerin
Angina
Acute MI
Severe HTN
Coronary artery
spasms
Reduce preload and
after-load
Plasma volume
expansion in the
depletion of intercellular
s/e: orthostatic
hypotension,
bradycardia, syncope,
flushing, and headache
(ha common and will
decrease over time)
Do not take with erectile dysfunction meds
(causes profound hypotension)
Nitrate tolerance with continuous exposure
and they lose effectiveness; All regimens
should be tailored to provide 10-12 hours
self-hydro pro-factors nitrate free interval to decrease tolerance
C/I: head trauma or cerebral hemorrhage
Peripheral
vasodilators
Hydralazine
Minoxidil
Severe refractory
HTN
Peripheral vasodilation
through a direct
relaxation of vascular
smooth muscles
Adverse reaction:
rebound HTN,
dizziness, tachycardia
ETOH and nitrates may potentiate
orthostatic hyotension
Cautious use in CV disease and pulmonary
HTN
In people with intolerance to ACEIs and
ARBs who have significant kidney
dysfunction, the use of combined
hydralazine and isosorbide nitrate is
effective alternative that has been shown to
reduce mortality in people with moderate
heart failure, especially African Americans
Do not give diuretics with Lithium (lithium
toxicity risk greatly increased)
Thiazide Diuretics HCTZ Edema in CHF/liver
cirrhosis, or kidney
disorders
HTN
HCTZ-deplete body
sodium and reduce fluid
volume
Vision problems, dry
mouth, thirst, N/V,
drowsiness, restless,
dizziness, tachycardia,
muscle pain/weakness,
red/blistering-peeling
skin
NSAIDS can decrease diuretic effect
Loop Diuretics Furosemide
(Lasix)
Edema in CHF, liver
disease, or kidney
disorders such as
nephrotic syndrome
Inhibit Na-K-Cl
cotransporter in the loop
of Henle by binding to
the chloride transport
channel, thus these
electrolytes to be losses
in urine
S/e: increased
urination, thirst,
muscle cramps,
itching/rash,
weakness, dizziness,
diarrhea
Monitor serum potassium
NSAIDS can decrease diuretic effect
Caution w/ digoxin
Potassium sparing
diuretics
Spironolactone
(Aldactone)
1
st line therapy for
HTN
s/e: hyperkalemia,
headache, dizziness,
thirst, muscle cramps,
N/V/D, stomach
cramps
NSAIDS can decrease diuretic effect
Use of both potassium-sparing diuretics
and ACE inhibitors can cause
hyperkalemia
HMG COA
inhibitors
Statins
Lovastatin
Simvastatin
Rosuvastatin
High cholesterol Blocks HMG-CoA
reductase, which block
the pathway for
synthesizing cholesterol
in the liver
S/e: liver damage,
rhabdomyolysis, DM,
neuropathy, sexual
dysfunction
Before starting on statin get baseline liver
function and creatine
Ezetimibe (Ezetrol) is an adjunct to diet
and statins to reduce total
cholesterol/LDL/triglycerides
Take in evening, report any muscle
weakness/tenderness
Avoid grapefruit juice
Pt should report muscle cramps/weakness
and/or dark colored urine immediately:
check CPK
Do not give to people w/ 1st or 2nd degree
relatives w/ history of muscle issues when
started on statins
Bile Acid Resins Cholestyramine
Colesevelam
Questran
High Cholesterol Exchanges chloride ions
for bile acids so that
they can’t be reabsorbed
in GI tract
S/e: constipation,
abdominal pain,
bloating, N/V/D,
weight loss, flatulence,
heartburn
Fibric Acid
Derivatives
Fenofibrate
(Tricor)
Gemfibrozil
(Lopid)
High Cholesterol;
mainly high
triglycerides
Increase lipolysis of
triglycerides
S/e: GI upset (N/V/D),
inflammation of liver,
back pain, flatulence,
headache, abdominal
pain, bloating
Not 1st line treatment
Lopid: Minimal effect on LDL, raises HDL
Tricor: lowers LDL
Interacts w/ statins and other anti-lipid
drugs (cause increase risk of
rhabdomyolysis)
Niacin (B3) Nicotinic acid High Cholesterol Decrease production of
LDL/triglycerides/total
cholesterol, increase
HDL
S/e: Headache,
flushing, pruritis d/t
vasodilation
ER: less flusing
Take w/ food and avoid alcohol!!
Prior to giving Niacin, give 325 mg ASA
30 min before to help with flushing
Monitor creatinine and LFTs
Anticoagulant Warfarin Prevention of
thrombosis and
thromboembolisms
Inhibits vitamin K
epoxide reductase
enzyme that recycles
oxidized vitamin K after
it has participated in the
carboxylation of several
blood clot blood
coagulation proteins
S/e: severe bleeding,
red or brown urine,
black or bloody stool,
severe headache or
stomach pain, joint
pain
Can be reversed w/ vitamin K
Avoid vitamin K rich foods (kale, spinach)
C/I in pregnancy, hepatic dysfunction,
bleeding
Monitor INR: therapeutic 2-3
CHF:
1
st line therapy: treat w/ ACE (or ARBs) and diuretic first (coreg and losartan); or use hydralazine/nitrates in African Americans. Add
BB especially those w/o A-fib then add beta blocker if not working to help with heart failure
2
nd line therapy: digoxin
3
rd line therapy: diuretics
Systolic HTN: treat w/ diruteic and CCB
MI: treat with BB (ACE systolic)
Angina (BB)
Tachycardia (BB)
DM2 and proteinuria (ACE)
DM2 (ACE)
ACE and ARBs help in treating diabetic neuropathy
Protein restriction helps slow diabetic neuropathy
[Show More]


.png)





.png)