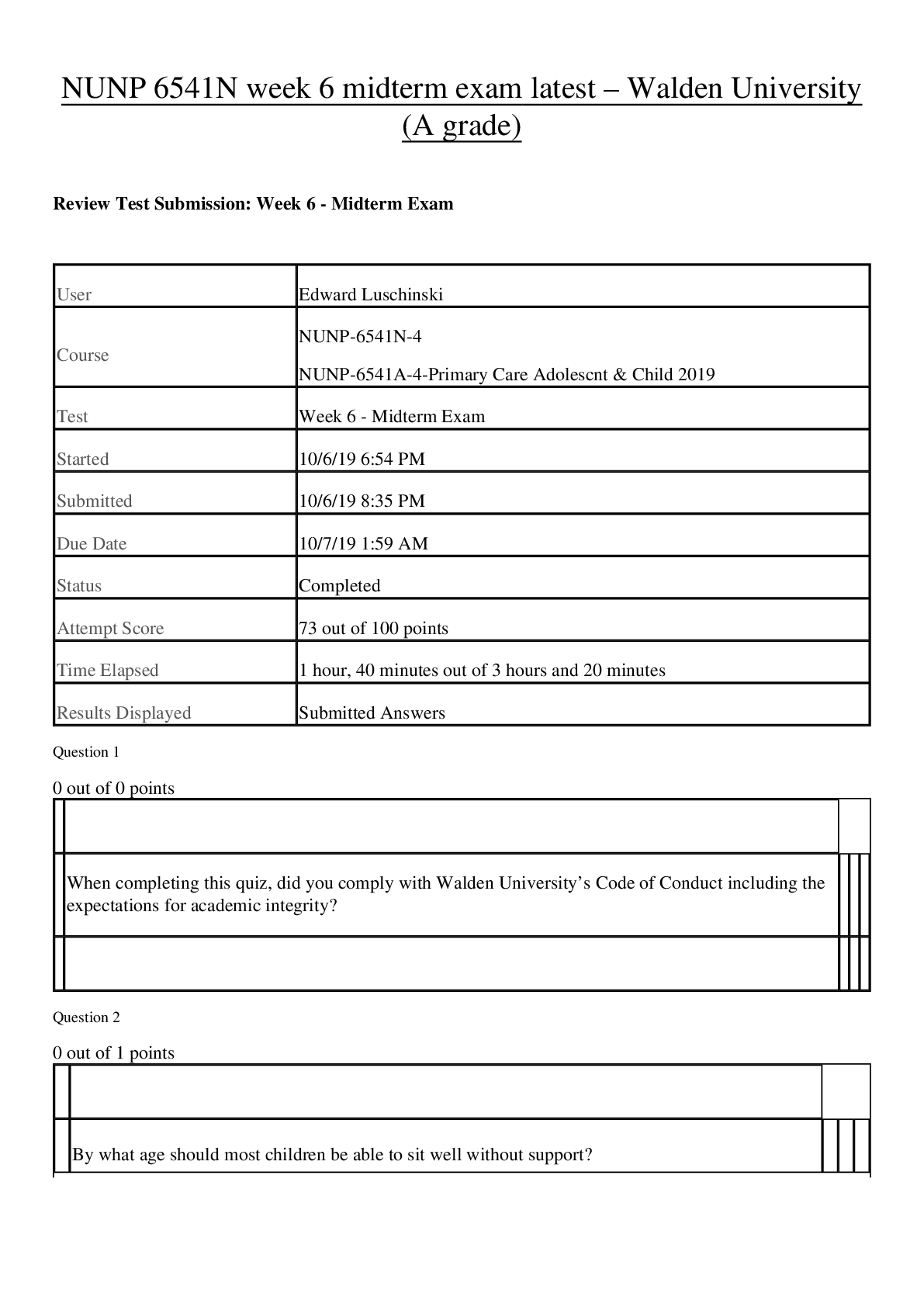
*NURSING > EXAM > NURS6560 / NURS 6560: Advanced Practice Care of Adults in Acute Care Settings II Midterm Exam Latest (All)
NURS6560 / NURS 6560: Advanced Practice Care of Adults in Acute Care Settings II Midterm Exam Latest Update Walden University
Document Content and Description Below
NURS 6560 Advanced Practice Care of Adults in Acute Care Settings II Mid Term Exam 1. A 22-year-old woman presents with a 3-year history of recurrent, unilateral, pulsating headaches with vomi... ting and photophobia. The headaches, which generally last 3 hours, can be aborted by resting in a dark room. She can usually tell that she is going to get a headache. She explains, "I see little 'squiggles' before my eyes for about 15 minutes. " Her physical examination is unremarkable. This presentation is most consistent with: A. tension-type headache. B. migraine without aura. C. migraine with aura. D. cluster headache. 2. A 44-year-old man has a long-standing history of moderate persistent asthma that is normally well controlled by fluticasone with salmeterol (Advair) via metered-dose inhaler, one puff twice a day, and the use of albuterol 1 to 2 times a week as needed for wheezing. Three days ago, he developed a sore throat, clear nasal discharge, body aches, and a dry cough. In the past 24 hours, he has had intermittent wheezing that necessitated the use of albuterol, two puffs every 3 hours, which produced partial relief. Your next most appropriate action is to obtain a: A. chest radiograph. B. measurement of oxygen saturation (SaO2). C. spirometry measurement. D. sputum smear for white blood cells (WBCs). 3. A 47-year-old woman experiences occasional migraine with aura and reports partial relief with zolmitriptan. You decide to add which of the following to augment the pain control by the triptan? A. lamotrigine B. gabapentin C. naproxen sodium D. magnesium 4. A 48-year-old woman presents with a monthly 4-day premenstrual migraine headache, poorly responsive to triptans and analgesics, and accompanied by vasomotor symptoms (hot flashes). The clinician considers prescribing all of the following except: A. continuous monophasic oral contraceptive. B. phasic combined oral contraceptive with a 7-day-per-month withdrawal period. C. low-dose estrogen patch use during the premenstrual week. D. triptan prophylaxis. 5. A 68-year-old woman presents with hypertension and BP of 152-158/92-96 mm Hg documented over 2 months on three different occasions. ECG and creatinine are normal, and she has no proteinuria. Clinical findings include the following: BMI 26.4 kg/m2; no S3, S4, or murmur; and point of maximal impulse at fifth intercostal space, mid-clavicular line. Which of the following represents the best intervention? A. Initiate therapy with metoprolol. B. Initiate therapy with hydrochlorothiazide. C. Initiate therapy with methyldopa. D. Continue to monitor BP, and start drug therapy if evidence of target organ damage. 6. A 68-year-old man presents with new onset of headaches. He describes the pain as bilateral frontal to occipital and most severe when he arises in the morning and when coughing. He feels much better by mid-afternoon. The history is most consistent with headache caused by: A. vascular compromise. B. increased intracranial pressure (ICP). C. brain tumor. D. tension-type with atypical geriatric presentation. 7. According to JNC-8, a 52-year-old well woman with a healthy BMI whose blood pressure is consistently 130-135/82-86 mm Hg is considered to have: A. normal blood pressure. B. hypertension requiring therapy with a CCB. C. hypertension requiring therapy with an alpha blocker. D. hypertension requiring therapy with a thiazide-type diuretic. 8. According to JNC-8 guidelines, a 67-year-old female with CKD should have a recommended blood pressure goal of A. <130/80 mm Hg B. <140/80 mm Hg C. <140/90 mm Hg D. <150/90 mm Hg 9. According to recommendations of the American Heart Association (AHA), which of the following antibiotics should be used for endocarditis prophylaxis in patients who are allergic to penicillin? A. erythromycin B. dicloxacillin C. azithromycin D. ofloxacin 10. According to the American Thoracic Society/Infectious Disease Society of American (ATS/IDSA) Consensus Guidelines on the Management of Community-Acquired Pneumonia in Adults, which of the following is the most appropriate antimicrobial for treatment of community-acquired pneumonia (CAP):A 42-year-old man with no comorbidity, no reported drug allergy, and no recent antimicrobial use? A. azithromycin B. cefpodoxime C. trimethoprim-sulfamethoxazole D. ciprofloxacin 11. According to the American Thoracic Society/Infectious Disease Society of American (ATS/IDSA) Consensus Guidelines on the Management of Community-Acquired Pneumonia in Adults, which of the following is the most appropriate antimicrobial for treatment of community-acquired pneumonia (CAP): A 69-year-old man with heart failure, prior myocardial infarction, and type 2 diabetes? A. respiratory fluoroquinolone B. amoxicillin with a beta-lactamase inhibitor C. cephalosporin D. beta-lactam plus macrolide 12. According to the American Thoracic Society/Infectious Disease Society of American (ATS/IDSA) Consensus Guidelines on the Management of Community-Acquired Pneumonia in Adults, which of the following is the most appropriate antimicrobial for treatment of community-acquired pneumonia (CAP): A 78-year-old woman with a history of COPD, hypertension and dyslipidemia who is taking lovastatin and a dihydropyridine calcium channel blocker? A. clindamycin B. high-dose amoxicillin with doxycycline C. clarithromycin D. ceftriaxone 13. According to the National Asthma Education and Prevention Program Expert Panel Report-3 (NAEPP EPR-3) guidelines, which of the following is not a risk for asthma death? A. hospitalization or an emergency department visit for asthma in the past month B. current use of systemic corticosteroids or recent withdrawal from systemic corticosteroids C. difficulty perceiving airflow obstruction or its severity D. rural residence 14. Acute cerebral hemorrhage is best identified with which of the following imaging techniques? A. transesophageal echocardiogram B. CT scan C. cerebral angiogram D. MR angiography 15. After inhaled corticosteroid is initiated, improvement in control is usually seen: A. on the first day of use. B. within 2 to 8 days. C. in about 3 to 4 weeks. D. in about 1 to 2 months. 16. After inhaled corticosteroid or leukotriene modifier therapy is initiated, clinical effects are seen: A. immediately. B. within the first week. C. in about 1 to 2 weeks. D. in about 1 to 2 months. 17. The anticipated effect on the lipid profile with high-dose omega-3 fatty acid use includes: A. increase in HDL. B. decrease in LDL. C. decrease in total cholesterol. D. decrease in triglycerides. 18. The anticipated effect on the lipid profile with plant stanol and sterol use includes: A. increase in HDL. B. decrease in LDL. C. decrease in select lipoprotein subfractions. D. decrease in triglycerides. 19. Antiepileptic drugs useful for preventing migraine headaches include all of the following except: A. divalproex. B. valproate. C. lamotrigine. D. topiramate. 20. Aortic stenosis in a 15-year-old male is most likely: A. a sequela of rheumatic fever. B. a result of a congenital defect. C. calcific in nature. D. found with atrial septal defect. 21. Assessing vision and visual fields involves testing cranial nerve (CN): A. I. B. II. C. III. D. IV. 22. Celeste is a 9-year-old girl with moderate persistent asthma. She is not taking a prescribed inhaled corticosteroid but is using albuterol PRN to relieve her cough and wheeze. According to her mother, she currently uses about six albuterol doses per day, in particular for cough and wheeze after active play. You consider that: A. albuterol use can continue at this level. B. excessive albuterol use is a risk factor for asthma death. C. she should also use salmeterol (Serevent) to reduce her albuterol use. D. active play should be limited to avoid triggering cough and wheeze. 23. The cornerstone of moderate persistent asthma drug therapy is the use of: A. oral theophylline. B. mast cell stabilizers. C. short-acting beta2-agonists. D. inhaled corticosteroids. 24. A diagnosis of pneumonia is confirmed by: A. sputum culture. B. sputum Gram stain C. bronchoalveolar lavage. D. chest radiograph. 25. For patients with documented coronary heart disease, the American Heart Association advises intake of approximately ____ of eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) per day, preferably from oily fish. A. 500 mg B. 1 g C. 2 g D. 4 g 26. In a person with a well-documented history of systemic cutaneous reaction without airway impingement following penicillin use, the use of which of the following cephalosporins is most likely to result in an allergic response? A. cephalexin B. cefprozil C. ceftriaxone D. cefpodoxime 27. In counseling a patient who experience migraines, you recommend all of the following lifestyle changes to minimize the risk of triggering a headache except: A. avoiding eating within 1-2 hours of AM awakening. B. limiting exposure to cigarette smoke. C. avoiding strenuous physical activities. D. implementing strategies to reduce stress. 28. Indicators that a headache can be the presenting symptom of a serious illness and may require neuroimaging include all of the following except: A. headaches that occur periodically in clusters. B. increasing frequency and severity of headaches. C. headache causing confusion, dizziness, and/or lack of coordination. D. headache causing awakening from sleep 29. An innocent heart murmur has which of the following characteristics? A. occurs late in systole B. has localized area of auscultation C. becomes softer when the patient moves from supine to standing position D. frequently obliterates the second heart sound (S2) 30. In patients with heart failure, the point of maximum impulse: A. remains unchanged near the fourth intercostal space. B. remains unchanged near the fifth intercostal space. C. shifts lower on the mid-clavicular line. D. shifts laterally by one or more intercostal spaces 31. In performing a cardiac examination in a person with MVP, you expect to find: A. an early- to mid-systolic, crescendo−decrescendo murmur. B. a pansystolic murmur. C. a low-pitched, diastolic rumble. D. a mid- to late-systolic murmur. 32. Intervention for patients with MVP often includes advice about which of the following? A. restricted activity because of low cardiac output B. control of fluid intake to minimize risk of volume overload C. routine use of beta-adrenergic antagonists to control palpitations D. encouragement of a regular program of aerobic activity 33. In the treatment of asthma, leukotriene modifiers should be used as: A. long-acting bronchodilators. B. an inflammatory inhibitor. C. a rescue drug. D. intervention in acute inflammation. 34. Leukotriene modifiers and ICS are interchangeable clinically because both groups of medications have equivalent anti-inflammatory effect. A. True B. False 35. The mechanism of action of triptans is as a(n): A. selective serotonin receptor agonist. B. dopamine antagonist. C. vasoconstrictor. D. inhibitor of leukotriene synthesis. 36. The mechanism of transmission of Legionella species is primarily via: A. respiratory droplet. B. inhalation of aerosolized contaminated water. C. contact with a contaminated surface. D. hematogenous spread. 37. The most common causative organism of bronchiolitis is: A. Hemophilus influenzae. B. parainfluenza virus. C. respiratory syncytial virus. D. coxsackievirus. 38. Of the following individuals, who is most likely to have a physiological split S2 heart sound? A. a 19-year-old healthy athlete B. a 49-year-old with well-controlled hypertension C. a 68-year-old with stable heart failure D. a 78-year-old with cardiomyopathy 39. Of the following patients, who is in greatest need of endocarditis prophylaxis when planning dental work? A. a 22-year-old woman with MVP with trace mitral regurgitation noted on echocardiogram B. a 54-year-old woman with a prosthetic aortic valve C. a 66-year-old man with cardiomyopathy D. a 58-year-old woman who had a three-vessel coronary artery bypass graft with drug-eluting stents 1 year ago 40. The patient you are evaluating is having a severe asthma flare. You have assessed that his condition is appropriate for office treatment. You expect to find the following on physical examination: A. tripod posture B. inspiratory crackles C. increased vocal fremitus D. hyperresonance on thoracic percussion 41. Poorly controlled asthma in children can lead to: A. attenuated lung development. B. chronic tracheitis. C. sleep apnea. D. alveolar destruction. 42. Prophylactic treatment for migraine headaches includes the use of: A. amitriptyline. B. ergot derivative. C. naproxen sodium. D. clonidine. 43. Risk factors for cluster headaches include all of the following except: A. over 65 years of age. B. heavy alcohol use. C. heavy tobacco use. D. male gender. 44. Signs and symptoms consistent with endocarditis include all of the following except: A. bradycardia. B. Osler's nodes. C. hematuria. D. petechiae. 45. Untreated hypothyroidism can result in which of the following changes in the lipid profile? A. increased HDL and decreased triglycerides B. increased LDL and total cholesterol C. increased LDL, total cholesterol, and triglycerides D. decreased LDL and HDL 46. Upon detection of a suspected pathologic cardiac murmur, the next step in obtaining a diagnostic procedure usually includes a: A. Ventilation perfusion scan. B. echocardiogram. C. pulmonary artery angiography. D. cardiac CT scan. 47. The use of neuroleptics such as prochlorperazine (Compazine) and promethazine (Phenergan) in migraine therapy should be limited to less than three times per week because of their: A. addictive potential. B. extrapyramidal movement risk. C. ability to cause rebound headache. D. sedative effect. 48. When prescribing a fibrate, the NP expects to see which of the following changes in lipid profile? A. marked decrease in LDL level B. increase in HDL level C. no effect on triglyceride level D. increase in very low-density lipoprotein (VLDL) level 49. Which of the following best describes asthma? A. intermittent airway inflammation with occasional bronchospasm B. a disease of bronchospasm that leads to airway inflammation C. chronic airway inflammation with superimposed bronchospasm D. relatively fixed airway constriction 50. Which of the following best describes patient presentation during a myoclonic seizure? A. blank staring lasting 3 to 50 seconds, accompanied by impaired level of consciousness B. awake state with abnormal motor behavior lasting seconds C. rigid extension of arms and legs, followed by sudden jerking movements with loss of consciousness D. brief, jerking contractions of arms, legs, trunk, or all of these 51. Which of the following best describes patient presentation during an absence (petit mal) seizure? A. blank staring lasting 3 to 50 seconds, accompanied by impaired level of consciousness B. awake state with abnormal motor behavior lasting seconds C. rigid extension of arms and legs, followed by sudden jerking movements with loss of consciousness D. abrupt muscle contraction with autonomic signs 52. Which of the following best describes patient presentation during a tonic-clonic (grand mal) seizure? A. blank staring lasting 3 to 50 seconds, accompanied by impaired level of consciousness B. awake state with abnormal motor behavior lasting seconds C. rigid extension of arms and legs, followed by sudden jerking movements with loss of consciousness D. abrupt muscle contraction with autonomic signs 53. Which of the following daily doses has the lowest lipid-lowering effect? A. simvastatin 10 mg B. rosuvastatin 5 mg C. atorvastatin 10 mg D. pravastatin 40 mg 54. Which of the following is an example of moderate-intensity statin therapy? A. fluvastatin 10 mg B. atorvastatin 10 mg C. simvastatin 10 mg D. pravastatin 20 mg 55. Which of the following is associated with the highest risk of ischemic heart disease? A. presence of microalbuminuria plus heavy alcohol intake B. absence of microalbuminuria plus use of a thiazolidinedione C. absence of microalbuminuria plus chronic physical inactivity D. presence of microalbuminuria plus cigarette smoking 56. Which of the following is inconsistent with the presentation of asthma that is not well controlled? A. a troublesome nocturnal cough at least 2 nights per week B. need for albuterol to relieve shortness of breath at least twice a week C. morning sputum production D. two or more exacerbations/year requiring oral corticosteroids 57. Which of the following is most likely to appear on a chest radiograph of a person during an acute severe asthma attack? A. hyperinflation B. atelectasis C. consolidation D. Kerley B signs 58. Which of the following is true regarding the use of systemic corticosteroids in the treatment of asthma? A. Frequent short bursts are preferred over daily inhaled corticosteroids. B. The oral corticosteroid should be started at day 3-4 of the asthma flare for optimal effect. C. The oral route is preferred over parenteral therapy. D. The adult dose to treat an asthma flare should not exceed the equivalent of prednisone 40 mg daily. 59. Which of the following medications is an alpha/beta-adrenergic antagonist? A. atenolol B. metoprolol C. propranolo D. carvedilol 60. Which of the following most accurately describes sputum analysis in the evaluation of the person with community-acquired pneumonia? sputum Gram stain and culture is A. Gram stain is routinely advised. B. Antimicrobial therapy should not be initiated until sputum specimen for culture has been obtained. C. Sputum analysis is not recommended in the majority of patients with community-acquired pneumonia. D. If required, chest physical therapy can be used to facilitate sputum production. 61. Which of the following statements is false regarding the use of omalizumab (Xolair)? A. Its use is recommended for patients with mild persistent asthma to prevent asthma flares. B. The medication selectively binds to IgE to reduce exacerbations. C. Labeled indication is for patients with poorly controlled asthma with frequent exacerbations. D. Special evaluation is required prior to its use and ongoing monitoring is needed during use. 62. Which pneumococcal vaccine offers protection against the greatest number of serotypes? A. Pneumovax B. Prevnar C. PCV7 D. LAIV 63. With migraine, which of the following statements is true? A. Migraine with aura is the most common form. B. Most migraineurs are in ongoing healthcare for the condition. C. The condition is equally common in men and women. D. The pain is typically described as pulsating. 64. With the use of a lipid-lowering resin, which of the following enzymes should be periodically monitored? A. ALP B. LDH C. AST D. No particular monitoring is recommended. 65. With the use of ezetimibe (Zetia), the NP expects to see: A. a marked increase in HDL cholesterol. B. a reduction in LDL cholesterol. C. a significant reduction in triglyceride levels. D. increased rhabdomyolysis when the drug is used in conjunction with HMG-CoA reductase inhibitor. 66. You are examining an 85-year-old woman and find a grade 3/6 crescendo−decrescendo systolic murmur with radiation to the neck. This is most likely caused by: A. aortic stenosis B. aortic regurgitation. C. anemia. D. mitral stenosis. 67. You examine a 29-year-old woman who has a sudden onset of right-sided facial asymmetry. She is unable to close her right eyelid tightly, frown, or smile on the affected side. Her examination is otherwise unremarkable. This presentation likely represents paralysis of CN: A. III. B. IV. C. VII. D. VIII. 68. You examine an 82-year-old woman who has a history of heart failure (HF). She is in the office because of increasing shortness of breath. When auscultating her heart, you note a tachycardia with a rate of 104 bpm and a single extra heart sound early in diastole. This sound most likely represents: A. summation gallop. B. S3. C. opening snap. D. S4. 69. You perform an extraocular movement test on a middle-aged patient. He is unable to move his eyes upward and inward. This indicates a possibility of paralysis of CN: A. II. B. III. C. V. D. VI. 70. You see a 34-year-old man with moderate persistent asthma who has a severe asthma flare and a regimen of oral prednisone is being considered. Which of the following is true? A. A taper is needed for prednisone therapy lasting longer than 4 days. B. A taper is not needed if the prednisone regimen is for 7 days or less. C. A taper is not needed regardless of duration of prednisone therapy. D. A taper is needed if the patient is taking concomitant inhaled corticosteroids [Show More]
Last updated: 2 years ago
Preview 1 out of 7 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$12.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Nov 09, 2020
Number of pages
7
Written in
Additional information
This document has been written for:
Uploaded
Nov 09, 2020
Downloads
1
Views
110













 – Chamberlain College of Nursing.png)