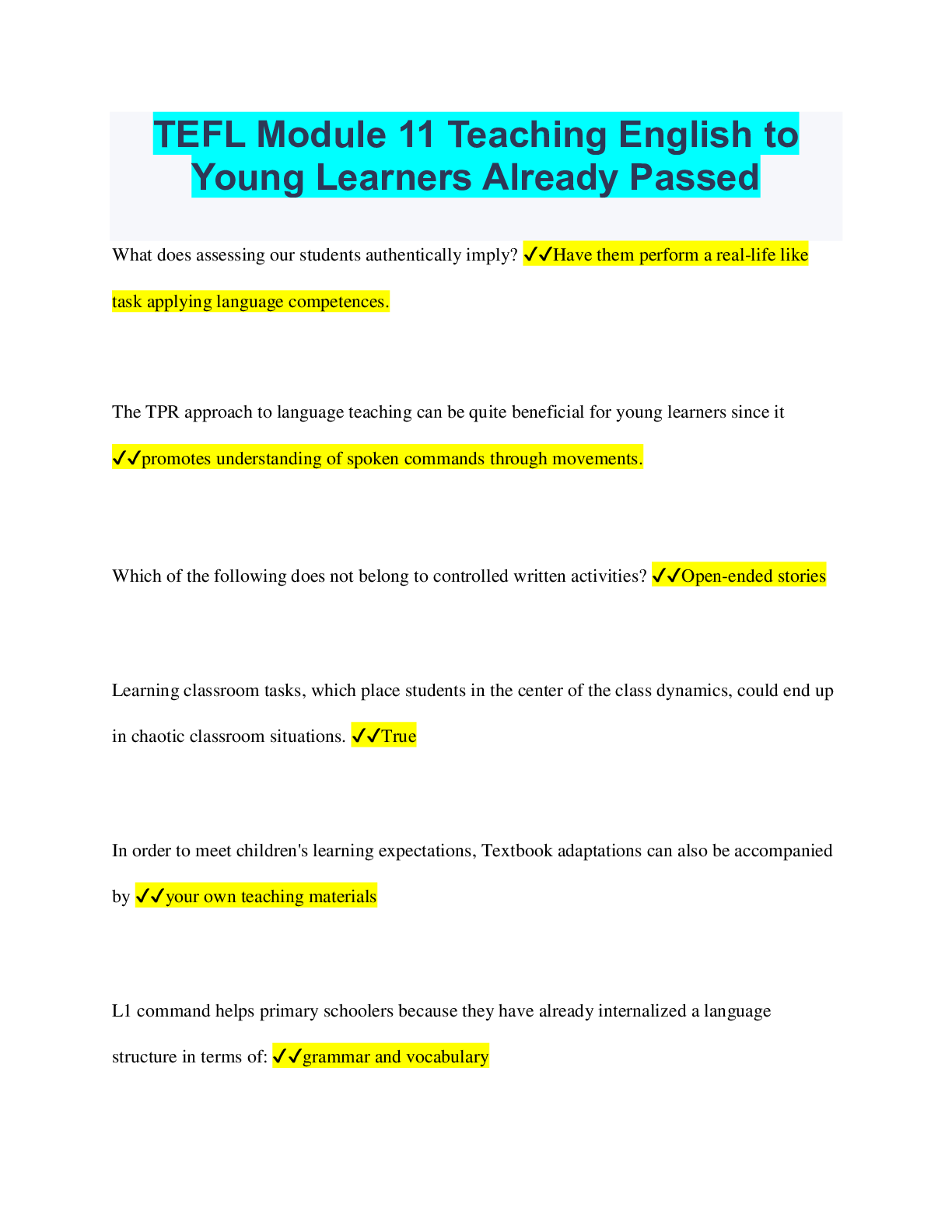
Health Care > QUESTIONS & ANSWERS > RHIA & RHIT Final Quiz 4.1 2022 COMPLETE SOLUTION (All)
RHIA & RHIT Final Quiz 4.1 2022 COMPLETE SOLUTION
Document Content and Description Below
RHIA & RHIT Final Quiz 4.1 2022 COMPLETE SOLUTION A four-digit code that describes a classification of a product or service provided to a patient is a - ✔✔revenue code State Medicaid programs ... are required to offer medical assistance for - ✔✔individuals with qualified financial need. Based on CMS's DRG system, other systems have been developed for payment purposes. The one that classifies the non-Medicare population, such as HIV patients, neonates, and pediatric patients, is known as - ✔✔APR-DRGs. Which of the following best describes the situation of a provider who agrees to accept assignment for Medicare Part B services? - ✔✔The provider cannot bill the patients for the balance between the MPFS amount and the total charges. Terminally ill patients with life expectancies of ______ may opt to receive hospice services. - ✔✔6 months or less ICD-10-PCS procedure codes are used on which of the following forms to report services provided to a patient? - ✔✔UB-04 This is the amount collected by the facility for the services it bills. - ✔✔reimbursement The Centers for Medicare and Medicaid Services (CMS) will make an adjustment to the MS-DRG payment for certain conditions that the patient was not admitted with, but were acquired during the hospital stay. Therefore, hospitals are required to report an indicator for each diagnosis. This indicator is referred to as - ✔✔present on admission. ____ is knowingly making false statements or representation of material facts to obtain a benefit or payment for which no entitlement would otherwise exist. - ✔✔fraud A HIPPS (Health Insurance Prospective Payment System) code is a five-character alphanumeric code. A HIPPS code is used by home health agencies (HHA) and ____. - ✔✔skilled nursing facilities (SNFs) and inpatient rehabilitation facilities (IRFs) A patient is being cared for in his or her home by a qualified agency participating in Medicare. The dataentry software used to conduct all patient assessments is known as - ✔✔HAVEN Commercial insurance plans usually reimburse health care providers under some type of __________ payment system, whereas the federal Medicare program uses some type of _________ payment system. - ✔✔retrospective, prospective Under APCs, payment status indicator "C" means - ✔✔inpatient procedures/services. The following services are excluded under the Hospital Outpatient Prospective Payment System (OPPS) Ambulatory Payment Classification (APC) methodology. - ✔✔durable medical equipment APCs are groups of services that the OPPS will reimburse. Which one of the following services is not included in APCs? - ✔✔organ transplantation CMS assigns one _______________ to each APC and each ______________ code. - ✔✔payment status indicator, HCPCS/CPT This is the difference between what is charged and what is paid. - ✔✔contractual allowance When the third-party payer returns a claim due to missing, inaccurate, or invalid information, this is called a - ✔✔rejected claim. Health plans that use ____________ reimbursement methods issue lump-sum payments to providers to compensate them for all the health care services delivered to a patient over a specific period of time for a particular reason. - ✔✔episode of care (EOC) The category "Commercial payers" includes private health insurance companies and - ✔✔employerbased group health insurers. ____ are errors in medical care that are clearly identifiable, preventable, and serious in their consequences for patients. - ✔✔Never events or sentinel events In a hospital, a document that contains a computer-generated list of procedures, services, and supplies, along with their revenue codes and charges for each item, is known as a(n) - ✔✔chargemaster The Correct Coding Initiative (CCI) edits contain a listing of codes under two columns titled "comprehensive codes" and "component codes." According to the CCI edits, when a provider bills Medicare for a procedure that appears in both columns for the same beneficiary on the same date of service, - ✔✔code only the comprehensive code. The _______________ is a statement sent to the provider to explain payments made by third-party payers. - ✔✔remittance advice This document is published by the Office of Inspector General (OIG) every year. It details the OIG's focus for Medicare fraud and abuse for that year. It gives health care providers an indication of general and specific areas that are targeted for review. It can be found on the Internet on CMS's website. - ✔✔the OIG's Work Plan Of the following, which is a hospital-acquired c [Show More]
Last updated: 3 years ago
Preview 1 out of 5 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Also available in bundle (1)
Click Below to Access Bundle(s)
.png)
[SOLVED] RHIA BUNDLED EXAMS QUESTIONS AND ANSWERS WITH COMPLETE AND VERIFIED SOLUTIONS
[SOLVED] RHIA BUNDLED EXAMS QUESTIONS AND ANSWERS WITH COMPLETE AND VERIFIED SOLUTIONS
By Nutmegs 2 years ago
$20
15
Reviews( 0 )
$7.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
May 25, 2022
Number of pages
5
Written in
All
Additional information
This document has been written for:
Uploaded
May 25, 2022
Downloads
0
Views
163








.png)