General Questions > EXAM > Exam (elaborations) NR507 COMPLETE PATHOPHYSIOLOGY FINAL EXAM STUDY GUIDE, LATEST 2022 UPDATE. (All)
Exam (elaborations) NR507 COMPLETE PATHOPHYSIOLOGY FINAL EXAM STUDY GUIDE, LATEST 2022 UPDATE.
Document Content and Description Below
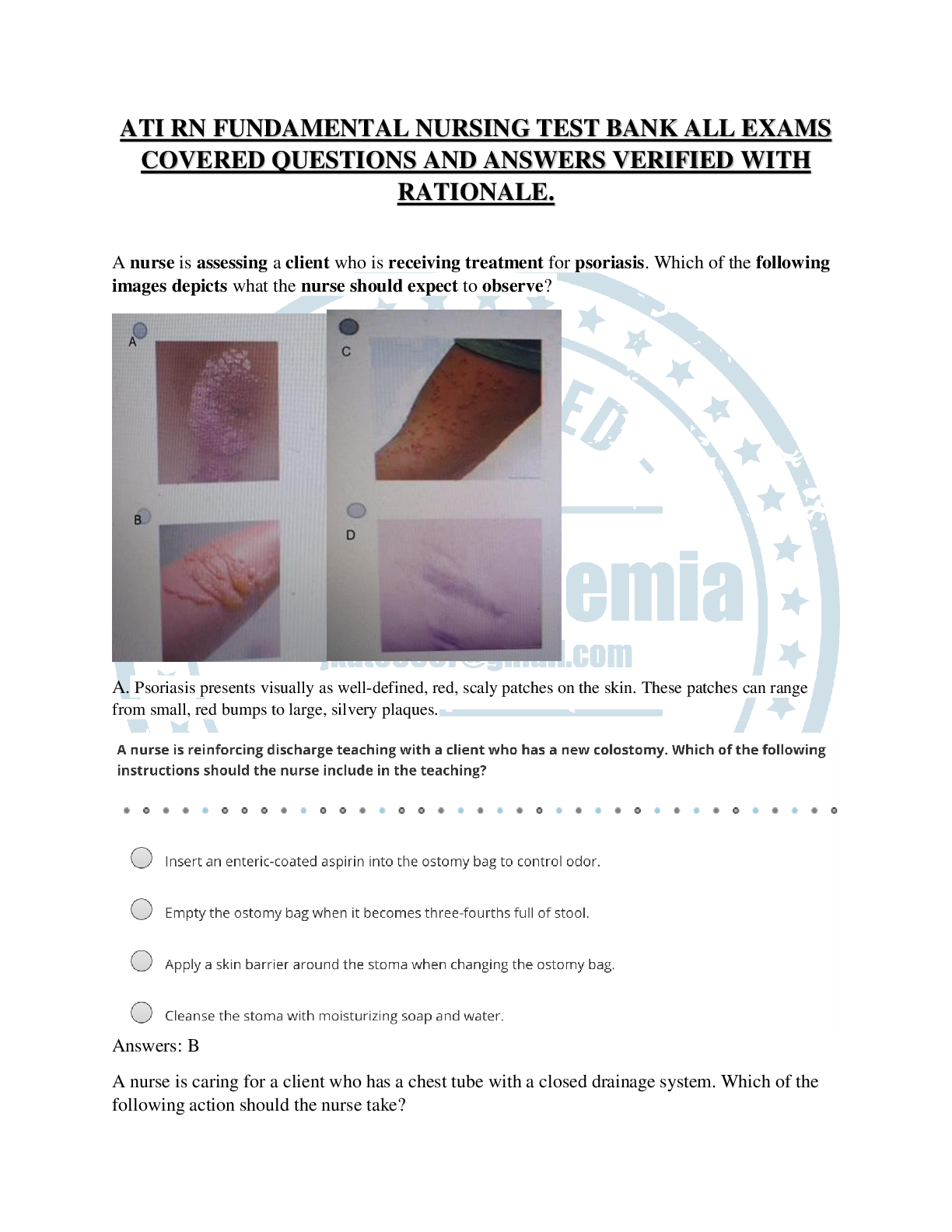
NR507 COMPLETE PATHOPHYSIOLOGY FINAL EXAM STUDY GUIDE REPRODUCTIVE Endometrial cycle and occurrence of ovulation Manifestation of female reproductive functioning is menstrual bleeding, which starts wi ... th menarche (1st period) and ends with menopause (cessation of menstrual flow for 1 year). Average age of menarche is 12 with a range of 9-17. Appears to be r/t body weight, especially body fat ratio. At first cycles are anovulatory and vary from 10-60 days or >. Then in adulthood range form 25-35 days. Length varies considerably. Cycle and regular ovulation are dependent on • The activity of gonadostat • Initial pituitary secretion of gonadotropin FSH • Estrogen positive feedback for the preovulatory FSH and LH surge, oocyte maturation, and corpus luteum formation and production of progesterone. The average menstrual cycle lasts 27 to 30 days and consists of three phases, which are named for ovarian and endometrial changes: the follicular/proliferative phase, the luteal/secretory phase, and the ischemic/menstrual phase. Phase 1-is the follicular phase in which begins on day one of one’s menstrual cycle. It lasts until about day 14. -In phase 1 the endometrium grows to form a lush lining inside of the uterus. Phase 2: Luteal phase-this is where the body secretes the hormones estrogen and progesterone. -These hormones work together to prepare the lining of the uterus for implantation. -This last for 12 days. Phase 3: Menstrual phase-The estrogen and progesterone start to decline and the endometrial lining begins to shed. This lasts for 3-5 days and the process restarts. Ovulation -Release of ovum -Present at the beginning of the luteal/secretory phase. -The ovarian follicle begins to transform into the corpus luteum. -Pulsatile secretion of the LH from the anterior pituitary stimulates the corpus luteum to secrete progesterone. -This will initiate the secretory phase of endometrial development. -Glands and blood vessels in the endometrium branch and curl through a functional layer, and the glands begin to secrete a thin glycogen-containing fluid= the secretory phase. *If conception occurs the nutrient-laden endometrium is ready for implantation. *The HCG hormone is secreted 3 days after fertilization by blastocytes and maintains the corpus luteum once implantation occurs at day 6 or 7. *HCG can be detected in maternal blood or urine about 8-10 days after ovulation. *Production of estrogen and progesterone continue until placenta can adequately maintain hormonal production. *Ovulatory cycles have a length of 24-26.5 days. *The primary ovarian follicle requires 10-12.5 days to develop. *The luteal phase appears at 14 days. Ovarian events of the menstrual cycle are controlled by gonadotropins. High FSH levels stimulate follicle and ovum maturation (follicular phase), then a surge of LH causes ovulation, which is followed by development of the corpus luteum (luteal phase). Ovarian hormones control the uterine (endometrial) events of the menstrual cycle. During the follicular/proliferative phase of the ovarian cycle, estrogen produced by the follicle causes the endometrium to proliferate (proliferative phase) and induces the LH surge and progesterone production in the granulosa layer. During the luteal/secretory phase, estrogen maintains the thickened endometrium, and progesterone causes it to develop blood vessels and secretory glands (secretory phase). As the corpus luteum degenerates, production of both hormones drops sharply, and the “starved” endometrium degenerates and sloughs off, causing menstruation, the ischemic/menstrual phase. Cyclic changes in hormone levels also cause thinning and thickening of the vaginal epithelium, thinning and thickening of cervical secretions, and changes in basal body temperature. Uterine Prolapse descent of cervix or entire uterus into vaginal canal. In severe cases the uterus falls completely through the vagina and protrudes from the introitus. Symptoms of other pelvic floor disorders may also be present. Tx depends on severity of symptoms and physical condition of woman. First line treatment is often a pessary- removable mechanical device that holds uterus in position. The pelvic fascia may be strengthened through kegels or by estrogen therapy in menopausal women. Healthy BMI, preventing constipation, and treating chronic cough may also help. Surgical repair with or without hysterectomy is the last resort. Page-771 fig 25.11 -Dropping of the cervix or the entire uterus into the vaginal canal. -In severe cases the uterus completely through the vagina and protrudes from the introitus. -Symptoms of other pelvic floor disorders may also be present. Symptoms: urinary-sensation of incomplete emptying of bladder, incontinence,frequency,bladder splinting to accomplish voiding. Bowel-constipation or feeling of rectal fullness, difficult defecation, stool or flatus incontinence. *Pain or bulging includes pelvic pressure, low back pain, and vagina, bladder or rectum bulging. *Sexual-decreased sensation, lubrication or arousal. -Dyspareunia Treatment: -Depends on age and severity. -Isometric exercise-strengthen the pubococcygeal muscle. KEGELS* -Estrogen-to improve tone and vascularity of fascial support POSTMENOPAUSAL* -Pessary—a removable device to hold pelvic organs in place. -Weight loss -Stool softeners to avoid constipation -tx of lung and cough conditions PCOS Polycystic ovary syndrome (PCOS) is a difficult syndrome to diagnose because several factors are involved. It is a syndrome in which at least two of the following are present: oligo-ovulation or anovulation, elevated levels of androgens, or clinical signs of hyperandrogenism and polycystic ovaries. Prolonged anovulation leads to infertility, menstrual bleeding disorders, hirsutism, acne, endometrial hyperplasia, cardiovascular disease, and diabetes mellitus in women with hyperinsulinemia. Presenting s/s: obesity, menstrual disturbance, oligomenorrhea, amenorrhea, regular menstruation, hyperandrogenism, infertility or they could be asymptomatic. Diagnosis of PCOS is based on evidence of androgen excess, chronic anovulation, and inappropriate gonadotropin secretion. Tests for impaired glucose tolerance are recommended. As stated, polycystic ovaries do noT have to be present and, conversely, their presence alone does not establish the diagnosis. Goals of treatment include reversing signs and symptoms of androgen excess, instituting cyclic menstruation, restoring fertility, and ameliorating any associated metabolic or endocrine, or both, disturbances. *Most common cause of anovulation and ovulatory dysfunction in women. *Leading cause of infertility and most common endocrine disturbance. *Mostly common in younger women *Usually has two/three of the following: irregular ovulation, elevated levels of androgens (testosterone), and the appearance of polycystic ovaries on ultrasound. *Polycystic ovaries do not need to be present to dx POS. *Thyroid dysfunction, hyperprolactinemia, and congenital adrenal hyperplasia must be ruled out first. *Associated with metabolic dysfunction, dyslipidemia, insulin resistance, and obesity. *Strong genetic component and possibly differentially inherited. *Difficult to diagnose as symptoms may change over time. *80% of women have one or more of the symptoms with normal ovaries. *More prominent sx as we age. *May be associated with Cushing’s syndrome, acromegaly, premature ovarian failure, obesity, congenital adrenal hyperplasia, thyroid disease and androgen producing adrenal tumors. Pathophysiology: *Underlying cause is unknown *Genetic involvement suggested because of steroid and androgen biosynthesis. *No single factor accounts for abnormalities of pcos. ***A HYPERANDROGENIC STATE IS A CARDINAL GEATURE IN THE PATHOGENSIS OF PCOS*** -3 X LIKELY TO HAVE INSULIN RESISTENCE. *Insulin stimulates androgen secretion by the ovarian stroma and reduces the serum sex hormone-binding globulin. * Free testosterone levels increase *Excessive androgens affect follicular growth and insulin affects follicular decline by suppressing apoptosis Decreased intraovarian receptors for estrogen receptor -a- or insulin like growth factor 1, increased leptin levels, or direct infrared redaction select ovarian cells. *Intrauterine and early child enviroment contribute to childhood development. *Weight gain aggravates symptoms and women will have an increased leptin level. *Leptin levels are increased in thin women as well *Leptin influences the hypothalamic pulsatility of GNRH and interaction with HPO. *Dysfunction in ovarian follicle development results from inappropriate gondatropin secretes and triggers the beginning of anovulation. *FSH is low and LH are high. *Persistent LH elevation causes an increase in androgens *DHEA (in adrenal glands and testosterone). And Androstenedione and dhea in the ovary. *Characterized by excessive levels of androgen and estrogen. -increased androgen contributes to a premature follicular failure (anovulation). -Persistent anovulation causes the pearly white smooth capsules (polycystic ovaries). -Thickening of the tunica, increased cortical stromal thickening, and hyperplasia. -**Women with PCOS 3 x greater of developing uterine cancer. Clinical Manifestations: *Appear within 2 years of puberty. *May not present until normal menstrual function or pregnancy. *Obese *Anovulation, hyperandrogenism, insulin resistance *infertility, hirsutism, acne, dysfunctional bleeding. *More likely to experience sleep apnea. Evaluation and Treatment: *dx is made based on androgen excess, chronic anovulation, and sonographic evidence of polycystic ovaries. *Must have 2 -3 of these. *Impaired glucose tolerance test is recommended *Goals are to suppress androgen, instituting menstruation, restore fertility, and reduce endocrine disturbance. **FIRST LINE TREATMENT= COMBINED ORAL CONTRACEPTIVES** -This helps to initiate regular menses. -Lifestyle modifications= exercise and weight loss. --Insulin resistance= metformin -If pregnancy is not desired- progesterone therapy is important to oppose estrogen effects on the endometrium to help monthly bleeding. **FOR OBESE WOMEN LIFESTYLE MODIFICATIONS ARE FIRST LINE** -CLOMIPHENE CITRATE CAN BE USED TO FACILITATE OVULATION* Testicular cancer & Risk factors Highly treatable, usually curable cancer most often develops in young and middle aged men. Rare, but most common form of cancer between young men 15-35. More common on R side than left. Germ cell tumors arising from male gametes: seminomans and nonseminomas. Seminomas are most common, least aggressive. Nonseminomas include embryonal carcinomas, teratomas, and choriocarcinomas, most aggressive but rare. Neoplasm cause is unknown. Genetic predisposition is suggested d/t incidence in brothers, identical twins and close male relatives. Risk factors: cryptochordism- neoplasms develop more commonly in contralateral testis. Abnormal testicular development, HIV and AIDS, Klinefelter syndrome, and hx of testicular cancer. Symptoms that require evaluation for Breast Cancer Clinical manifestation Pathophysiology Chest pain Metastasis to lung Dilated blood vessels Obstruction of venous return by fast growing tumor Dimpling of skin Can occur with invasion of dermal lymphatics because of retraction of cooper ligament Edeme of arm Local inflammation of lymphatic obstruction Hemorrhage Erosion of blood vessels Local pain Local obstruction by tumor Nipple/areolar eczema Paget disease Nipple discharge in a nonlactating woman Spontaneous and intermittent d/c caused by tumor obstruction Nipple retraction Shortening of mammary ducts Pitting of the skin Obstruction of subq lymphatics, resulting in fluid accumulation Reddened skin, local tenderness, warmth Inflammation Skin retraction Involvement of suspensory ligaments Ulceration Tumor necrosis Signs of premenstrual dysphoric disorder (PMDD) • The cyclic recurrence (in the luteal phase of the menstrual cycle) of distressing physical, physical, psychologic, or behavioral changes that impair interpersonal relationships or interfere with usual activities. • Neurotransmitters, GABA, and noradrenaline may have mediating or moderating roles on symptom manifestation. These neurotransmitters have demonstrated interactions with estrogen and progesterone and all of these are neuroactive with known mood and behavior effects, including negative mood, irritability, aggression, and impulse control. • Symptoms usually appear a week before menstruation and end a few days after your period starts. When this happens, some women have trouble functioning at home, at work and in relationships during this time. • Women show symptoms of irritability, nervousness, anger, insomnia, anxiety, paranoia, trouble sleeping, N&V, headaches, fainting. - - - - - - - - -- - - - - - - - - - - - - - - -- - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - adrenocorticotropic hormone from the pituitary gland. As a result, the adrenocorticotropic hormone levels start to fall. This is called a negative feedback loop. Stress, both physical and psychological, also stimulates adrenocorticotropic hormone production and hence increases cortisol levels. **The effects of too much adrenocorticotropic hormone are mainly due to the increase in cortisol levels which result. Higher than normal levels of adrenocorticotropic hormone may be due to: Cushing's disease – this is the most common cause of increased adrenocorticotropic hormone. It is caused by a non-cancerous tumour called an adenoma located in the pituitary gland, which produces excess amounts of adrenocorticotropic hormone. (Please note, Cushing’s disease is just one of the numerous causes of Cushing’s syndrome). A tumour, outside the pituitary gland, producing adrenocorticotropic hormone (also called ectopic adrenocorticotropic hormone tumour). Addison's disease (although cortisol levels are low, adrenocorticotropic hormone levels are raised). Congenital adrenal hyperplasia (a genetic disorder with inadequate production of cortisol, aldosterone or both). Bartholin glands (pg 772) Also called greater vestibular or vulvovaginal glands. In response to sexual stimulation Bartholin glands secrete mucus to lubricate inner labial surfaces and enhance viability and motility of sperm. It also facilitates coitus (sexual intercourse). Gonococcal disease (pg 920-922) Gonorrhea is caused by gonococci (species of Neisseria gonorrhoeae) Risk factors include: Transient or urban residence, sexual activity at a young age, drug use, prostitution, and previous case of gonorrheal or concurrent STI. Females have a higher risk of contracting than men Transmitted through sexual, oral or anal intercourse. Pregnant women can transmit to fetus. Glomerulonephritis- Inflammation of the glomerular filtration membrane (epithelium, podocytes, endothelium and basement membrane). Messangelial expansion leads to leaking and loss of negative charge thus causing hematuria (casts and proteinuria). Severe glomerulonephritis -> edema, hypertension, impaired renal function causing decreased glomerular filtration (due to decreased blood flow)-> decreased GFR ultimately causing renal failure. Small patent ductus arteriosus (PDA)- ***Picture--PDA with left to right shunt*** In fetal circulation a PDA allows blood to shunt from PA to aorta. Then at birth when the placenta is removed and lungs expand, the PDA constricts within the first few hours of life. Full closure occurs within 15hrs to 2 weeks after birth. Defect of the PDA accounts for 5-10% of all congenital cardiac defects and is most prevalent in preemies. Failure of PDA closure=persistent patency of ductus arteriosus. IN PDA: At birth pulmonary circulation = systemic circulation (minimal shunting) Later Pulmonary vascular resistance decreases and reverse fetal shunting occurs (left to right or aorta to PA) pulmonary blood flow increases increasing pulmonary venous return to the LA and LV increased work of Left heart leading to increased Right heart ventricular pressure increased pulmonary vascular pressure. Clinical manifestations- Infant has an audible continuous machine like murmur best heard at the left upper sternal border throughout systole and diastole. Small PDA is generally asymptomatic. Diagnosis through CXR, Echo and presence of machine like continuous murmur. Asymptomatic PDA or small PDA with no murmur- closure of PDA by 2 yrs old is recommended via surgical ligation and division or a prostaglandin inhibitor if unable to undergo surgery. Risk factors for hypertension- (HTN= >120/>80) Primary HTN= no known cause (95%) Secondary HTN= cause r/t underlying disease Risk factors are both genetic and environmental in primary HTN: Family history, advancing age, gender (men < 55, women >70), black, high Na+ intake, glucose intolerance, smoking, obesity, high alcohol use, low dietary intake of K+, Ca+ and Mag. Loss of language and/or comprehension-such as terms-aphasia, etc. –(Data Processing Deficits) Agnosia- Deficit of pattern recognition- one sense fails to recognize form/nature of objects but the others may maintain ability to recognize. Agnosia may be auditory, visual or tactile. Example: Person may be able to look at a pin and say “pin” but is unable to do the same when touching it. Agnosia is most common in CVA but can also be found in other neurological issues. Dysphagia- Impairment of comprehension or production of language, comprehension or use of symbols in either written or verbal language is impaired. Aphasia- Complete loss of comprehension or production of language. Chronic inflammatory joint disease Commonly called arthritis Characterized by damage/destruction of synovial membrane/articular cartilage and systemic signs of inflammation (fever, leukocytosis, malaise, anorexia, hyperfibrinogenemia. Can be infectious or non-infectious. Noninfectious – Gout, rheumatoid arthritis (RA) and ankylosing spondylitis (AS) Infectious- caused by bacteria, virus and fungi (Lymes, TB, ), gonococcus, staph, strep, haemophilus influenza, parovirus B19, rubella, hep C, HIV • Rheumatoid arthritis (RA) is a chronic, systemic inflammatory autoimmune disease distinguished by joint swelling and tenderness and destruction of synovial joints, leading to disability and premature death. Cytokines (interleukins, B Cells and matrix metalloproteinases) contribute to joint damage. Attack begins at synovial membrane and spreads to cartilage, joints, ligaments, and tendons causing pain, joint deformity and loss of function. Most common joints are fingers, feet, wrists, elbows, ankles and knees. Other symptoms include fever, malaise, rash, lymph node/spleen enlargement and Raynaud’s phenomenon. *Risk factors include: age, genetic factors and inflammatory mediator **Chemokines are thought to be responsible for inflammation by attracting T cells. Diagnosis- Presence of serum RF (rheumatoid factor) in addition to physical findings.** Pathophysiology- In inflammation--Arginine (amino acid) modified by enzymes to become citrulline (Citrullination) to change structure and function. T and B cells attack the Citrullinated proteins because they are seen as antigens, causing bony erosion, interlueukins breakdown cartilage and bone and a pannus (thick abnormal layer of granulation tissue) is formed. Synovial swelling and hyperplastic thickening (due to abnormal proliferation and increase in cell size) contribute to damage. Treatment—early aggressive treatment of RA can prevent disability and joint destruction. Treated with disease modifying antirheumatic drugs (DMARDs) (methotrexate, cyclosporine, hydroxychloroquine), NSAIDs, glucocorticoids, steroid injections, PT, OT, assistive devices and surgery to treat deformities. • Ankylosing spondylitis (AS) is the most common of a group of inflammatory arthropathies known as spondyloarthropathies. It is a chronic inflammatory joint disease characterized by stiffening and fusion (ankylosis) of the spine and sacroiliac joints. Exact cause is unknown but strong association with: HLA-B27 in the endoplasmic reticulum (ER) causing misfolded proteins to accumulate stress response in ER increased interleukins and inflammatory cytokines. Most common signs and symptoms: Early- low back pain and stiffness typically in early 20s. Later- pain progresses, often worse after prolonged rest, and alleviated by physical activity. Early morning stiffness, and difficulty sitting up and twisting spine. Pain and loss of motion due to inflammation and reflex muscle spasm. Causes lumbar lordosis and kyphosis- thus Tspine is rounded and head and neck are bent forward. Other manifestations- peripheral joint involvement, uveitis, fibrotic changes in lungs, cardiomegaly, aortic incompetence, amyloidosis, and Achilles tendonitis. Symptoms: fatigue, wt loss, low grade fever, hypochromic anemia and increased sed rate. Diagnosis- by clinical findings (back pain > 3 months improving with exercise and not by rest) and radiologic findings (changes to sacroiliac joint and lab findings of presence of HLA-B27). Treatment- PT, OT, NSAIDs, DMARDs and surgery. • Gout is caused by an inflammatory response to uric acid production or excretion causing high levels of uric acid in blood and other bodily fluids which is linked to purine metabolism and kidney function. Risk factors: age > 30 years, genetics, excessive alcohol, obesity, certain drugs (thiazides) and lead toxicity. Pathophysiology- Uric acid crystalizes in connective tissues and joints causing painful inflammation triggering inflammatory response by macrophages, activating interleukins resulting in joint damage. Primary gout- etiology unknown Secondary gout- etiology known Three stages- 1) Asymptomatic hyperuricemia- serum urate level elevated with no other symptoms 2) Acute gouty arthritis- attacks develop with increased serum urate triggered by increases in hyperuricemia or by trauma, drugs and alcohol. 3) Tophaceous gout- Chronic stage. Progressive inability to excrete uric acid until urate crystal deposits (tophi) appear in cartilage, synovial membranes and soft tissue Renal stones are 1000 times more prevalent in patients with primary gout. Treatment- Drugs (colchicine and NSAIDs, hydrocortisone injections), ice, reduce body weight, avoid alcohol, increase intake of low fat dairy, cherries, soybeans and vegetable protein. Male and female sex hormone production *See pgs 789-791 and 795-6 (male) and 776-78 (female) • The male sex hormones are androgens and testosterone is the primary male sex hormone. Leydig cells of the testes and, to a lesser degree, the adrenal glands produce testosterone and other androgens. In men, sex hormone production is relatively constant with some diurnal variation • The sex hormones are all steroid hormones and are synthesized from cholesterol Male and female sex hormones are present in all adults. However, the female body contains low levels of testosterone and other androgens, and the male body contains low levels of estrogen. Individual effects of sex hormones depend on their amount and concentration in the blood. • The dominant female sex hormones, estrogen and progesterone, are produced primarily by the ovaries. During fetal development, infancy, and childhood, sex hormone production is low. Endogenous antigen- There are two main types of antigens- exogenous and endogenous. Endogenous antigens are linked with MHC I molecules. Endogenous antigens are synthesized within a cell. This includes viruses due the fact that a virus infects a cell and uses the normal cellular protein synthesis mechanisms in order to translate viral genes into viral proteins. Cancer is an example also. When cells undergo malignant changes and begin producing unique proteins which are specific to the cancer cells, these are presented as foreign materials as a result of foreign antigens on the cell’s surface. Genital warts- There are 120 types of HPV- stereotypes 6 and 11 are the cause for 90% of genital warts (GW). GW are very contagious and the level of contagion depends on HPV type, lesion location, and cellular immune response. Pregnant moms can pass GW to the fetus in utero. Children with HPV/GW are often victims of sexual abuse. Epithelial cells infected with HPV undergo transformations and proliferate the growth of cells forming a warty type growth (called condylomata acuminate) which are soft skin colored growths. These growths can be single lesions or groups of lesions forming a cauliflower like mass. Locations include; male-frenulum, glans, foreskin, urinary meatus, shaft, scrotum or anus and female- labia, clitoris, perineum, vagina or anus. **Lesions are not painful but can cause painful intercourse and may also bleed easily. **Urethral condylomata can become cancerous. **Laryngeal papillomas can occur in infants contracted from mom at birth causing stridor, hoarse/abnormal cry, and respiratory distress. Treatment in adults of GW is considered cosmetic not curative. Treatments include trichloroacetic acid (TCA) and bichloroacetic acid (BCA), cryotherapy and surgical excision. Pancreatic enzymes- The secretion of pancreatic enzymes are controlled by both hormonal and vagal stimulation. Their purpose is to break down/hydrolyze protiens (proteases), carbs (amylases) and fats (lipases). Proteases= trypsin, chymotrysinogen, procarboxypeptidase and elastase- also carries the primary function of protecting the pancreas from its’ own juices. In the duodenum inactive proactins are activated by enerokinase. All proteases also reduce polypeptides to peptides. Pancreatic α amylase breaks the bonds of carbs to form glucose and maltose Pancreatic lipase hydrolyzes fats to form free fatty acids. Process of muscle contraction- Calcium Ions combine with troponin thus activating the inhibitory function of the troponin-tropomysin complex. Actin (a thin filament) slides towards then over myosin (a thick filament). ----Myosin heads attach to actin molecules (actin-myosin complex) and ATP is released. Actin slides onto myosin (causing shortening or contraction). The maximum usefulness of contraction is when the muscle is at 25%-35% or when actin and myosin have maximum potential interaction with one another thus equaling maximum force. Myosin heads connect with actin ATP released myosin releases from actin myosin is hydrolyzed energizing it to allow myosin to crawl along actin (grab-release-grab-release) Here is a short video with a simple explanation- Cervical dysplasia- Dysplasia=abnormal shape, size and organization of mature cells. Not a “true” adaptive process and is said to be related to hyperplasia. Is strongly associated with neoplastic growths found adjacent to cancer cells but does not necessarily indicate cancer. Dysplasia is categorized as mild, moderate and severe. Persistence of HPV virus (particularly subtypes 16 and 18), immune response, smoking and hormone based contraceptives) illicit prime conditions for abnormal cervical cell growth. Consanguinity- Marriage between two people who are related. Proven to be a factor in producing children with recessive diseases related to the fact that families generally carry the same recessive genes- often when rare recessive diseases (ie. Cystic fibrosis) are present, consanguinity is considered. Nephrotic syndrome- More common in children 1) 3 or more grams of protein in the urine per day 2) Less than 3 g/dl serum albumin 3) Peripheral edema [Show More]
Last updated: 3 years ago
Preview 1 out of 3 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Also available in bundle (1)
Click Below to Access Bundle(s)

Answered Final Exam-Pathophysiology2021- Requires Respondus LockDown Browser//Exam (elaborations), NR 507 COMPLETE PATHOPHYSIOLOGY FINAL EXAM STUDY GUIDE//Summary Lipscomb University - NURS 3093 Study
Final Exam-Pathophysiology2021- Requires Respondus LockDown Browser//Exam (elaborations) NR507 COMPLETE PATHOPHYSIOLOGY FINAL EXAM STUDY GUIDE UPDATED | NR 507 COMPLETE PATHOPHYSIOLOGY FINAL EXAM STUD...
By Simon94 3 years ago
$18.5
2
Reviews( 0 )
$13.50
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Jul 08, 2022
Number of pages
3
Written in
All
Additional information
This document has been written for:
Uploaded
Jul 08, 2022
Downloads
0
Views
116



.png)