NR_602_Final_Exam_Study_Guide. wk 5,6,7,8
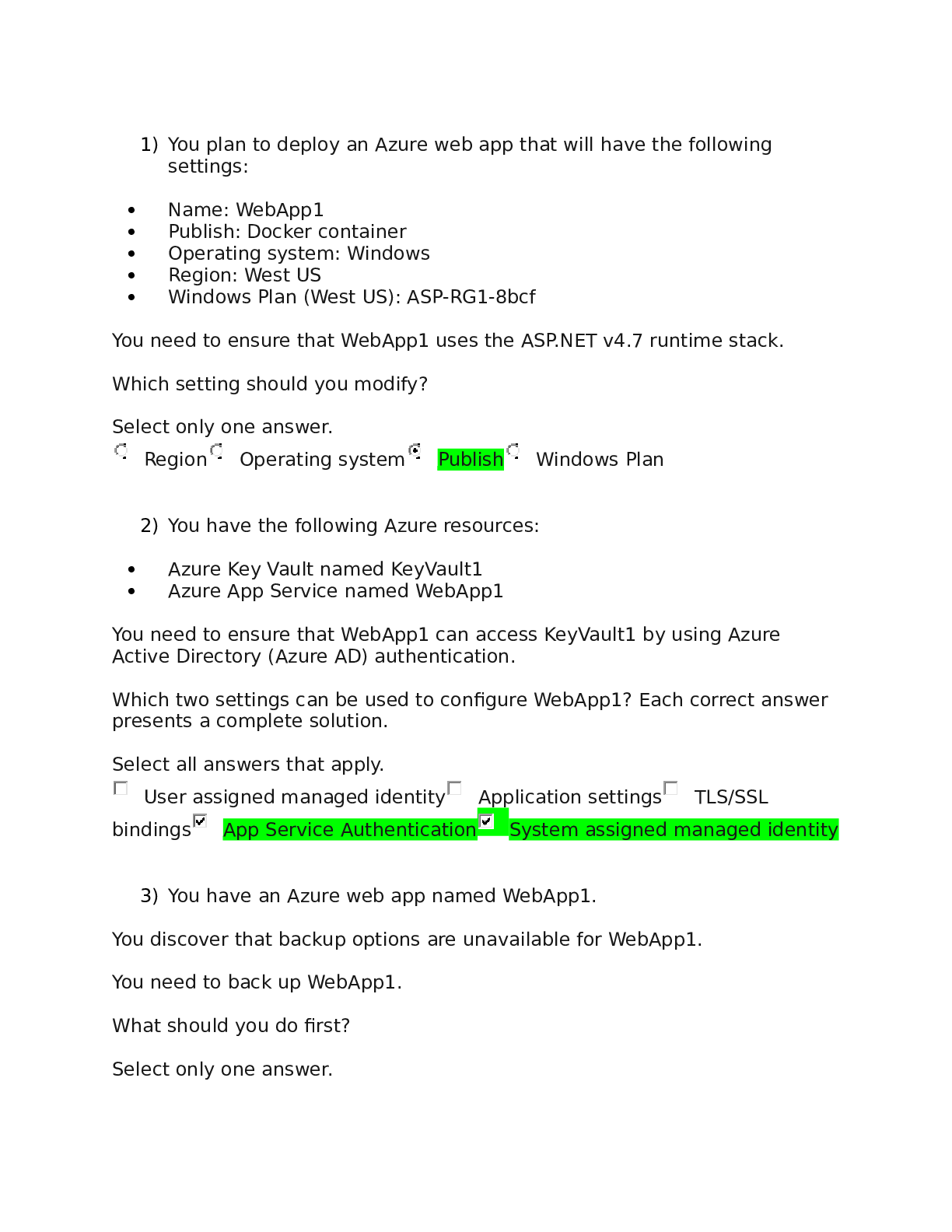
Document Content and Description Below
NR 602 Final Exam Study Guide
Week 5
Pediatrics
• Unit II - Child Development
o Chapter 34 - Dermatologic Disorders
o Chapter 35 - Eye and Vision Disorders
o Chapter 36 - Ear and Hearing Disor
...
ders
o Chapter 37 - Respiratory Disorders
Lieberthal, A. S., Carroll, A. E., Chonmaitree, T., Ganiats, T. G., Hoberman, A., Jackson, M. A., ... & Schwartz, R. H. (2013). The diagnosis
and management of acute otitis media. Pediatrics, 131(3), e964-e999. https://chamberlain-on-worldcatorg.chamberlainuniversity.idm.oclc.org/oclc/8588117369
Week 6
Pediatrics
Unit IV - Common Childhood Conditions and Disorders
• Chapter 38 - Cardiovascular Disorders
• Chapter 39 - Hematologic Disorders
• Chapter 46 - Neurologic Disorders
• Chapter 43 - Musculoskeletal Disorders
, G. C., Tulloh, L. E., & Tulloh, R. R. (2016). Kawasaki disease incidence in children and adolescents: an observational study in
primary care. The British Journal of General Practice: The Journal of The Royal College of General Practitioners, 66(645),
e271-e276. doi:10.3399/bjgp16X684325 (Links to an external site.)
tin-Hermoso, M. R., Berger, S., Bhatt, A. B., Richerson, J. E., Morrow, R., Freed, M. D., & Beekman, R. H. (2017). The care of
children with congenital heart disease in their primary medical home. Pediatrics, 140(5), e20172607. https://chamberlainon-worldcat-org.chamberlainuniversity.idm.oclc.org/oclc/7285161978
Week 7
Pediatrics
Unit IV - Common Childhood Conditions and Disorders
• Chapter 18 - Elimination
• Chapter 40 - Gastrointestinal Disorders
• Chapter 41 - Genitourinary Disorders
• Chapter 45 - Endocrine and Metabolic Disorders
• Chapter 33 - Atopic, Rheumatic, and Immunodeficiency Disorders
Week 8
Pediatrics
Unit IV - Common Childhood Conditions and Disorders
• Chapter 15 - Behavioral and Mental Health Promotion
• Chapter 24 - Injury Prevention and Child Maltreatment
• Chapter 30 - Neurodevelopmental, Behavioral, and Mental Health Disorders
Eye disorders
2
• USPSTF recommendations for vision screening for children 6 months to 5 years of age note
that screening tests have reasonable accuracy in identifying strabismus, amblyopia, and
refractive errors in children 3 to 5 years of age.
• Refractive errors are the most common visual disorders seen in children
o Myopia, or nearsightedness, exists when the axial length of the eye is increased in
relation to the eye’s optical power. As a result, light from a distant object is focused in
front of the retina rather than directly on it. A myopic child sees close objects clearly but
distant objects are blurry.
▪ Myopia may be present at birth however more likely to develop between 6 and 9
years of age, with increased prevalence after the adolescent growth spurt. Mild
hyperopia is normal in a young child and should decrease rapidly between 7 and
14 years of age.
o Hyperopia, or farsightedness, exists when the visual image is focused behind the
retina. As a result, distant objects are seen clearly but close objects are blurry.
o Astigmatism exists when the curvature of the cornea or the lens is uneven; thus the
retina cannot appropriately focus light from an object regardless of the distance, which
makes vision blurry close up and far away. Rarely, astigmatism can be caused by an
alteration in the corneal sphere caused by a soft tissue mass on the inner aspect of the
eyelid, such as a chalazion or hemangioma.
o Anisometropia is a different refractive error in each eye. It may consist of any
combination of refractive errors discussed earlier, or it may occur with aphakia.
• Amblyopia usually a unilateral deficit in which there is defective development of the visual
pathways needed to attain central vision
o Clear focused images fail to reach the brain, resulting in reduced or permanent loss of
vision.
o The condition is labeled (or typed) according to the structural or refractive problem that
is causing the poor visual image to reach the brain: deprivational, or obstruction of
vision (e.g., caused by ptosis, cataract, nystagmus), strabismic (caused by strabismus
or lazy eye), or refractive (myopia, hyperopia, astigmatism, anisometropia). Diagnosis of
amblyopia prevents permanent loss of vision in the affected eye.
o clinical findings:
▪ Squinting, tendency to cover or close one eye when concentrating
▪ Abnormal vision, cover/uncover, and/or fundoscopic exam
▪ Pain in or around eyes and/or headaches (rare)
▪ Fatigue, dizziness
▪ Developmental delay
▪ Family history of refractive errors, strabismus, or amblyopia
o Management:
▪ Refer to an ophthalmologist or optometrist for prescription corrective lenses.
School-age children and teenagers should participate in the selection of frames;
contact lenses may be considered.
▪ Once a refractive error has been determined or if a child is wearing glasses,
annual evaluations are recommended.
▪ Moderate amblyopia usually responds to 2 hours of daily patching or weekend
atropine (produces cycloplegia of nonamblyopic eye).
▪ Untreated or inadequately treated amblyopia in young childhood results in
irreversible and lifelong visual loss
• Strabismus defect in ocular alignment, or the position of the eyes in relation to each other;it
is commonly called lazy eye.
o strabismus may be hereditary or the result of various eye diseases (e.g.,
neuroblastoma), trauma, systemic or neurologic dysfunction that paralyzes the
3
extraocular muscles, uncorrected hyperopia, craniofacial abnormalities,
accommodation, and accommodative convergence
o A phoria is an intermittent deviation in ocular alignment that is held latent by sensory
fusion.
▪ The child can maintain alignment on an object. Deviation occurs when binocular
fusion is disrupted, most often during the cover/uncover test.
o A tropia is a consistent or intermittent deviation in ocular alignment.
▪ A child with a tropia is unable to maintain alignment on an object of fixation.
Intermittent tropia may occur when a child is tired.
o Phorias and tropias are classified according to the pattern of deviation seen:
▪ • Hyper- (up) and hypo- (down) are used to classify vertical strabismus.
▪ Exo- (away from the nose) and eso- (toward the nose) describe horizontal
deviations.
• Esotropia can also be seen in those with a history of prematurity, low birth
weight, cerebral palsy, hydrocephalus, and maternal substance or tobacco
use
▪ Cyclo- describes a rotational or torsional deviation.
o clinical findings:
▪ Intermittent exotropia in children (6 months to 4 years of age) who are ill, tired,
exposed to bright light, or with sudden changes from close to distant vision. It is
more often seen when the child is looking with distant fixation.
▪ When only one eye is affected (i.e., child always fixates with the unaffected eye).
▪ When both eyes are affected, the eye that looks straight at any given time is the
fixating eye.
▪ The angle of deviation may be inconsistent in all fields of gaze.
▪ Persistent squinting, head tilting, face turning, overpointing, awkwardness,
marked decreased visual acuity in one eye, or nystagmus may be seen.
▪ Cataracts, retinoblastoma, anisometropia, and severe refractive errors are rare
o management:
▪ Any ocular misalignment seen after the age of 4 months is considered
suspicious, and the child should be referred. Hyper-, hypo-, and exotropia,
acquired esotropia or exotropia, cyclovertical deviation, or any fixed deviations is
an indication for referral as soon as first observed.
▪ The unaffected (“good”) eye is occluded (using an adhesive bandage eyepatch,
an occlusive contact lens, or an overplussed lens), which forces the child to use
the deviating eye. Patching for 2 hours a day is as successful as patching for 6
hours a day
▪ Surgical alignment of the eyes may be necessary, but this does not preclude
additional amblyopia therapy.
▪ Corrective lenses alone improve amblyopia in 27% of patients. Assessment for
amblyopia should be done at every visit, even after straightening the eyes,
because changes in alignment can occur through the fifth year.
▪ The ocular status of an affected child’s siblings is monitored.
• Blepharoptosis or ptosis is drooping of the upper eyelids affecting one or both eyes (It can
be congenital or acquired, secondary to trauma or inflammation)
o Parents may remark that one eye appears smaller.
o In severe cases, children may have a chin-up head position or adapt by raising their
brow.
o Management
▪ correct any underlying systemic diseas
[Show More]
Last updated: 3 years ago
Preview 1 out of 93 pages

.png)







pdf (1).png)