Health Care > iHuman Case Studies > IHUMAN CASE #2: HEENT EMMA RYAN 2Y/O CC: RUNNY NOSE, COUGH AND FEVER (All)
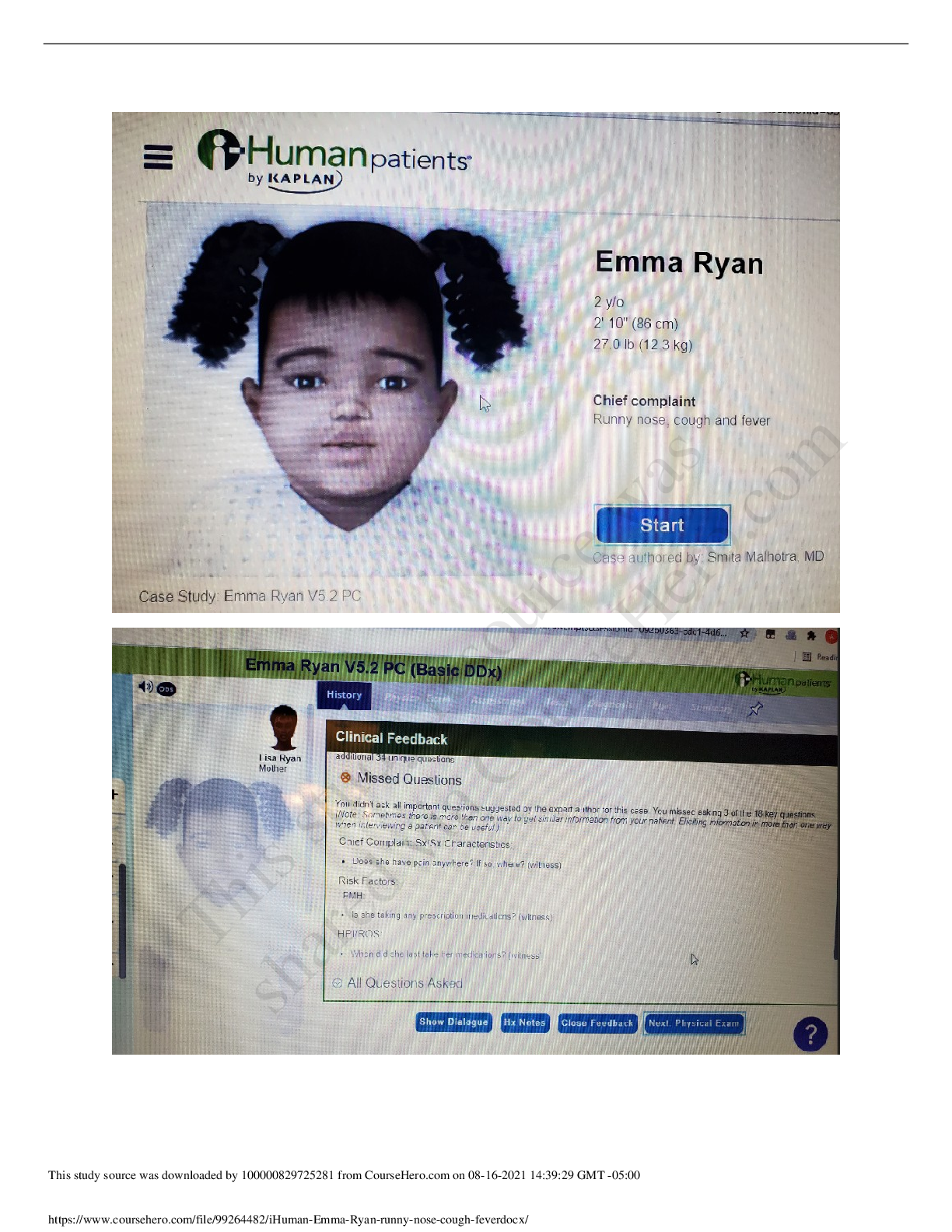
IHUMAN CASE #2: HEENT EMMA RYAN 2Y/O CC: RUNNY NOSE, COUGH AND FEVER
Document Content and Description Below
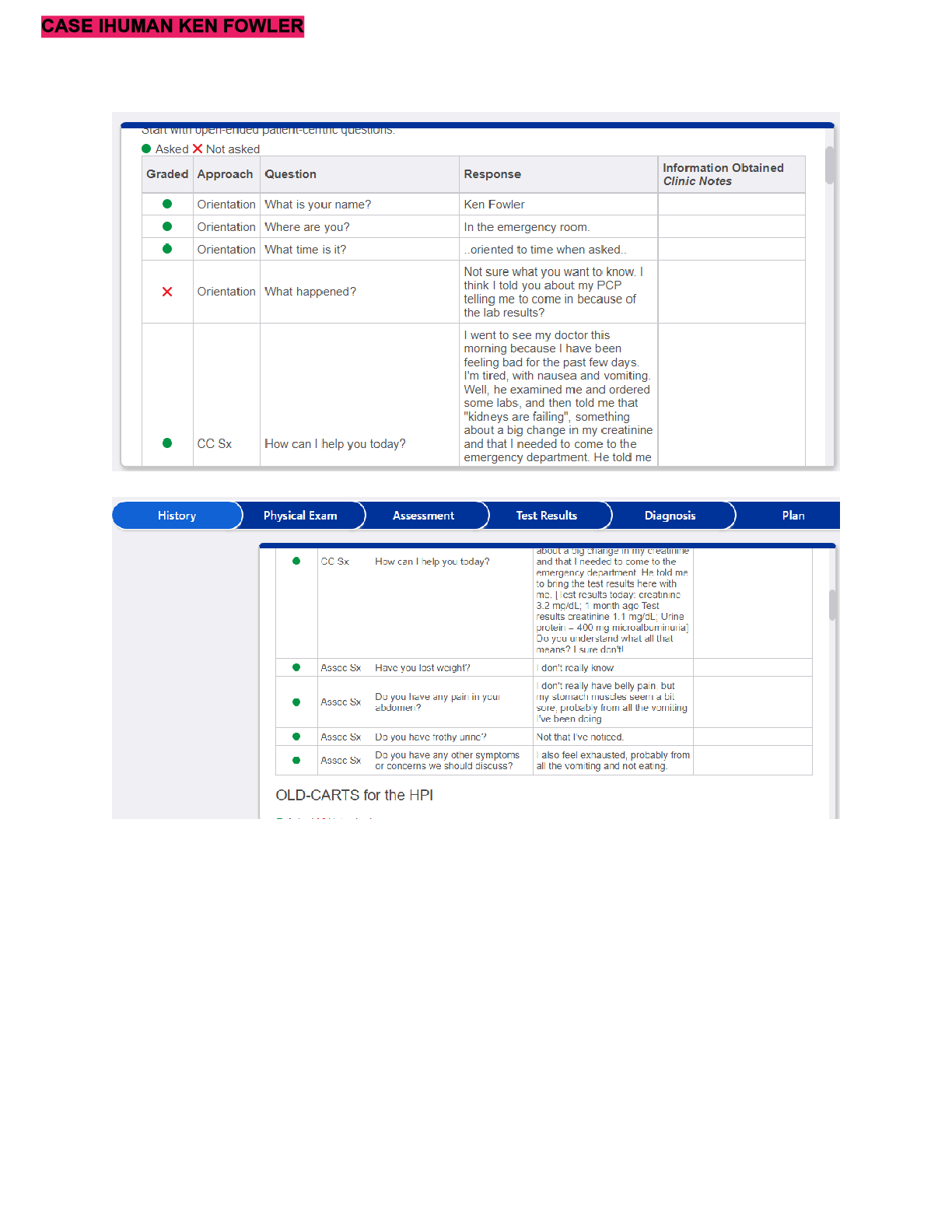
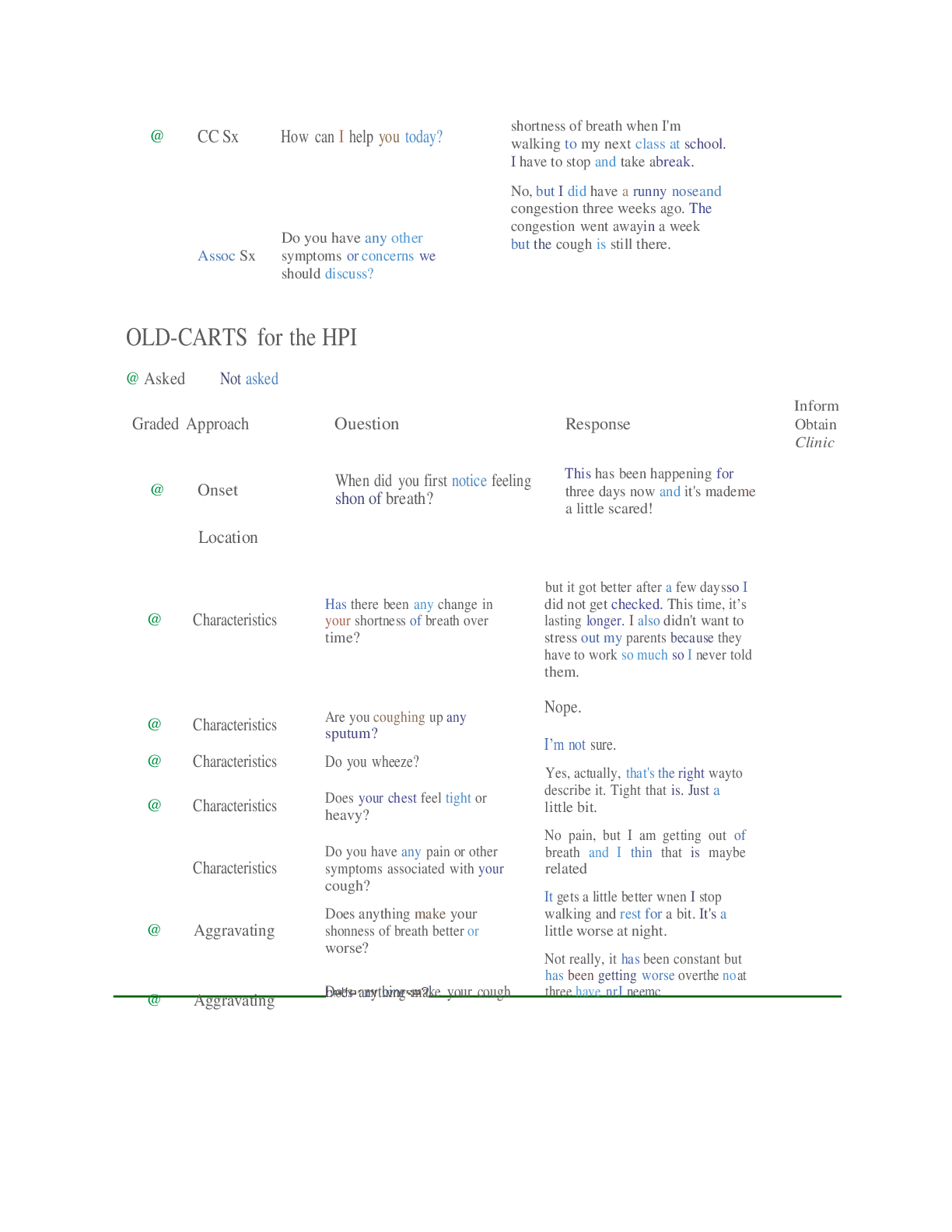
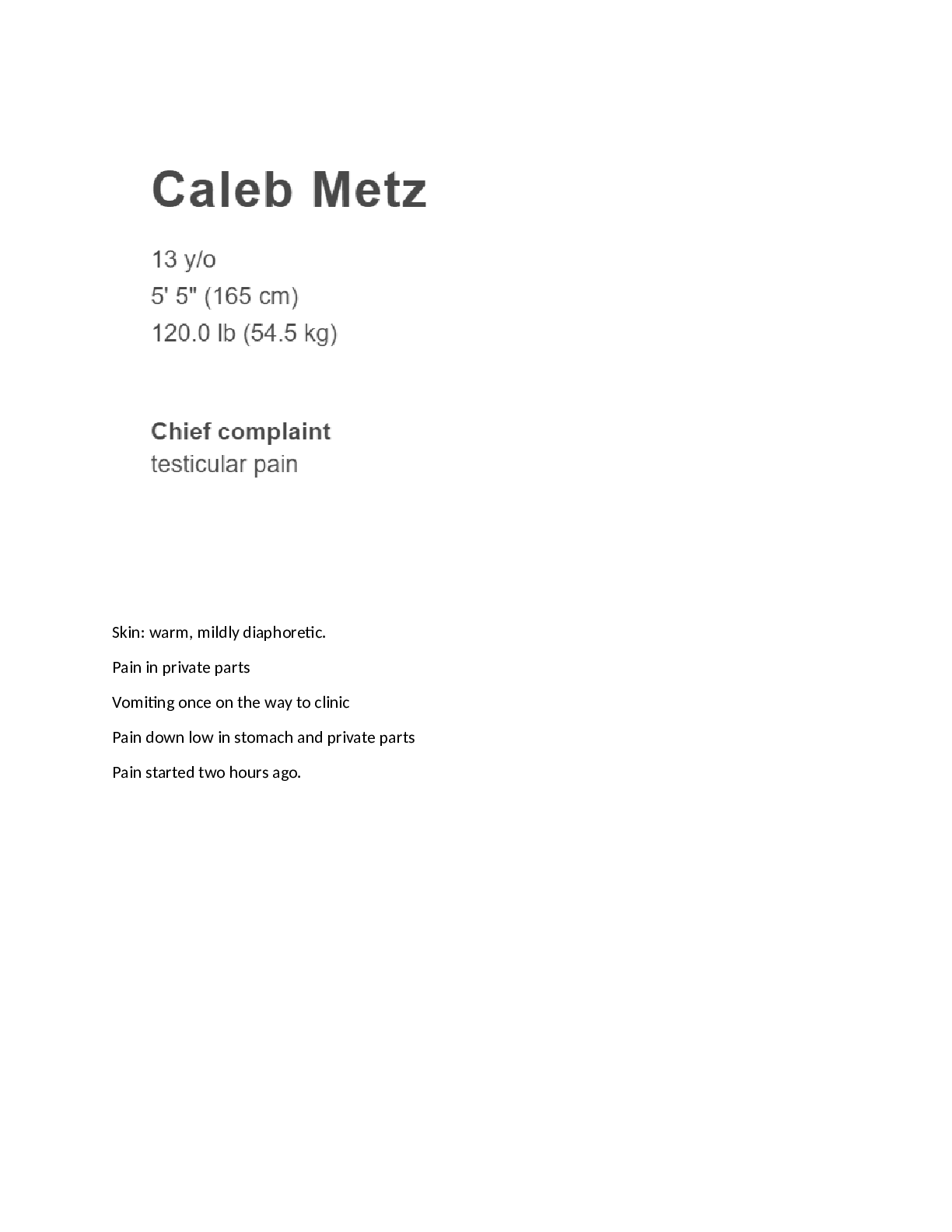
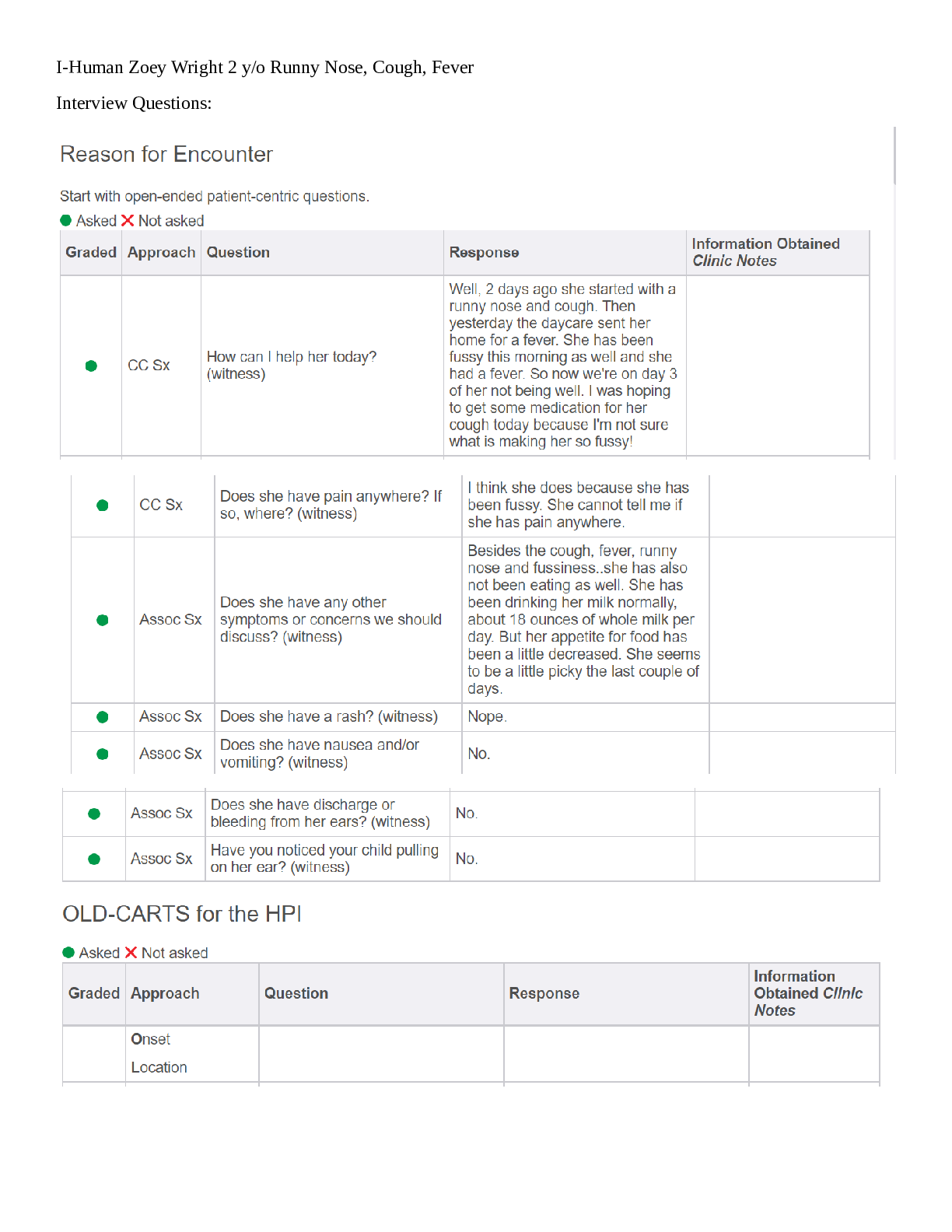
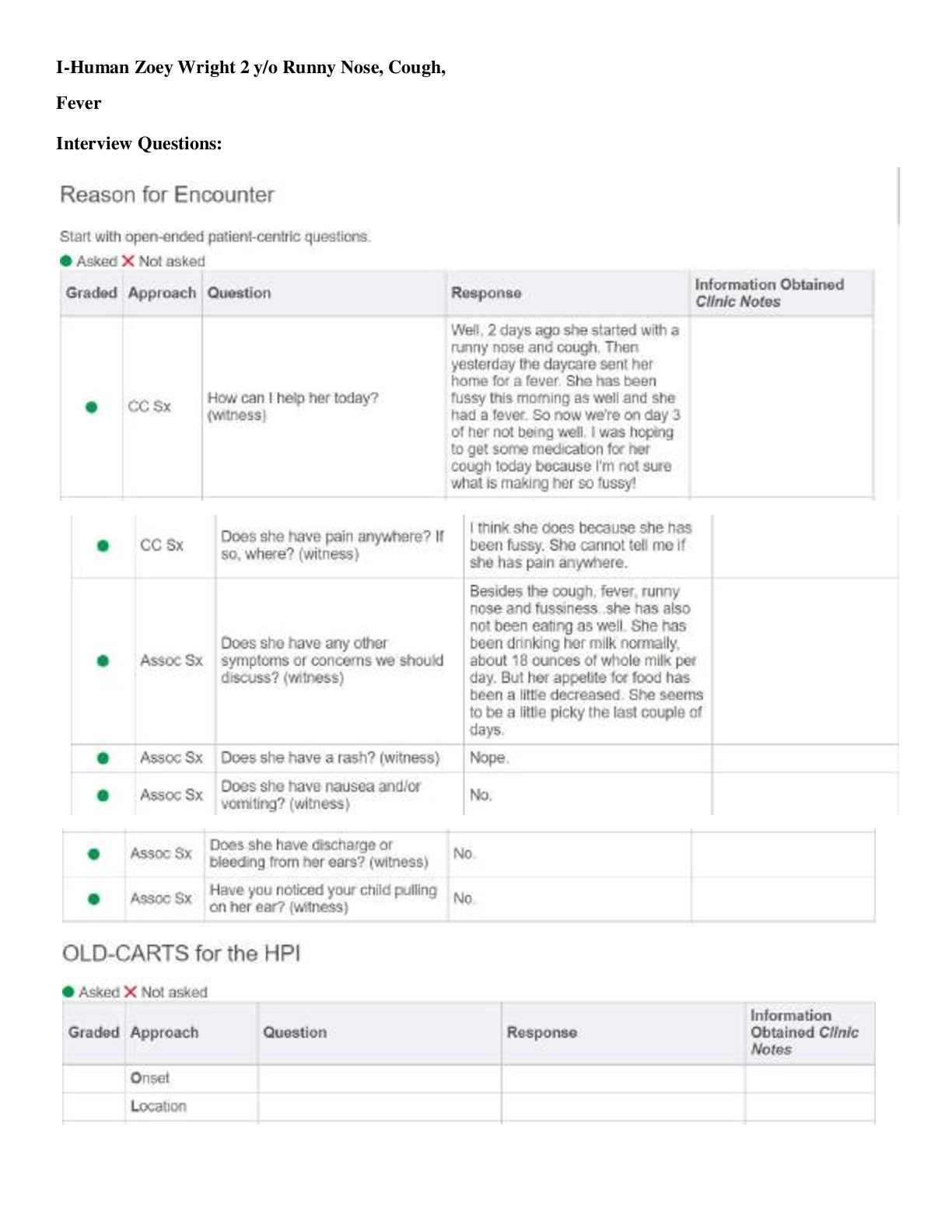
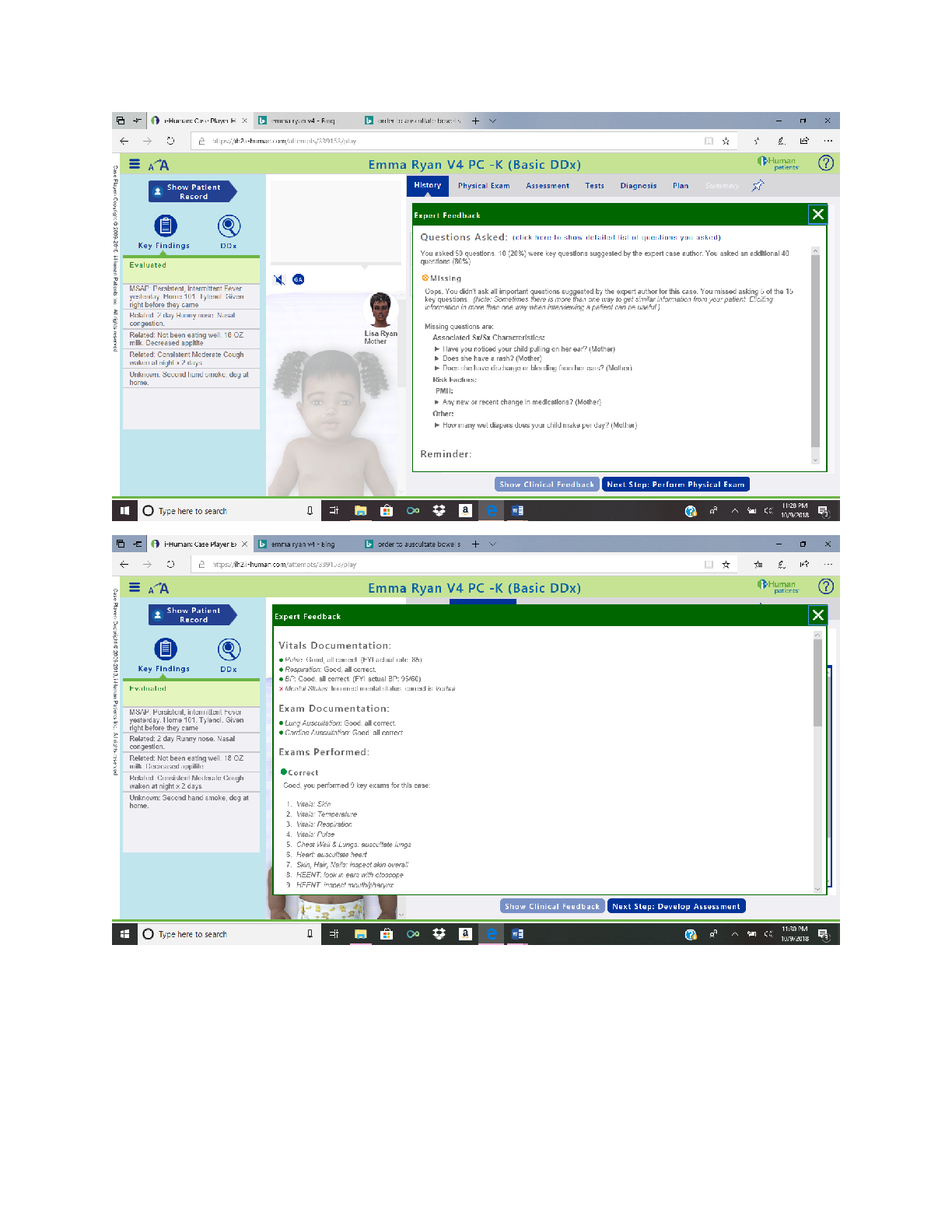
Case: 165481 Emma Ryan Date: 02/28/2021 CC: 2 y/o M/F Chief complaint is a short 1-2 statement or word phrase from patient and should be listed in “quotes” Mother’s statement “2 days ago... , she started with a runny nose and cough” HPI: pertinent s/s; +/- ROS/prior episodes/recent travel/ill contacts Emma Ryan is a 2-year-old girl who presented to the clinic with her mother with a complaint of runny nose and a cough that started 3 days ago and fever that started 2 days ago. She tolerates milk well, but her appetite is reduced with no change in the number of wet diapers. The mother reports she did not receive the flu vaccine this season; she is exposed to secondhand smoking at home and exposure to sick children at daycare. Onset: Cough and runny nose started 3 days ago and fever for the past 2 days Location: NA Duration: About 3 days and symptoms have persisted Character: Cough is unproductive Aggravating/alleviating factors: No aggravating or alleviating noticed or reported by mom Related symptoms: Fussiness and reduced appetite. Crying could be an indication of pain of discomfort (FLACC score of at least 2) Treatments: Tylenol every 4 hours for fever Significance: Fever in toddlers is significant and fussiness and loss of appetite is indicative of discomfort PMHx child/adult illness/hospitalizations/immunizations No hospitalizations, trauma, or other injuries Immunizations: Mother states she has not received flu vaccine this season but update on all recommended vaccinations. SurgHx type/when/why/complications No history of surgery This study source was downloaded by 100000844708667 from CourseHero.com on 08-31-2022 00:57:55 GMT -05:00 Case: 165481 Emma Ryan Date: 02/28/2021 FamHx Grandparents (if known)/Parents/siblings/children Mother-age 31-No history of medical problems Father-age 35 with history of mild intermittent asthma Brother-age 5 healthy SHx Tobacco/vaping/ETOH/illicit drug use/occupational/environmental/relationships Exposed to secondhand smoking by both parents in the home Reproductive Hx Female: Age of menarche/menstruation cycle duration/gravida para status/Childbirth hx/sexual hx and concerns/LMP/menopause Breast/cervical screening (if any) Male: Sexual hx and concerns/issues with fertility (if any)/Testicular or prostate screening (if applicable) Screening for STI’s (if applicable) Toddler, no schedule history Allergies (Food, Drug, Environmental, etc.) No known allergies List of Medications/supplements (prescription, OTC, complementary alternative therapies) Tylenol OTC for fever Review of Systems: (ROS) Use this column to document the ROS below. General: Crying HEENT: Runny nose Pulmonary: Nonproductive cough CV: No shortness of breath GI: Wears diapers. She has about 1-2 stool diapers per day, decreased appetite and no vomiting Decrease in appetite GU: No change in number of wet diapers From the ROS: list/highlight the current symptoms/complaints to generate a list of pertinent “reported or denied” symptoms below: Pertinent Positive ROS: Cough, runny nose, decreased appetite Pertinent Negative ROS: No signs of shortness of breath, No changes in voiding and bowel movement, no vomiting This study source was downloaded by 100000844708667 from CourseHero.com on 08-31-2022 00:57:55 GMT -05:00 Case: 165481 Emma Ryan Date: 02/28/2021 MS: No recent trauma or injury Heme: No sign bruising Lymph: No complaint Endocrine: No history of endocrine disorder Derm: No signs of rash Neuro: No history of Seizures Psych: No psychological concerns Physical Exam: (PE) Use this column to document the PE below. Vitals (HR/BP/RR/T/SpO2/Ht/Wt/BMI%) HR: 85, BP 95/60, RR: 20, SPO2: 98%, Height: 2ft 2 inches, Weight: 27lbs., BMI: 16.4 General: Crying toddler HEENT: Normocephalic, atraumatic, no deformities, face symmetrical, Pupils normal, reactive, ears have no discharge and appears normal, bilateral tympanic membranes with erythema and severe bulging, nose has no discharge or polyps, pharynx with erythema and exudates Neck: No visible scars or deformities or lesions Pulm Respirations regular and unlabored, normal lung sounds, negative for wheezing. CV: Normal heart sounds, HR 85 GI: No guarding or rebound tenderness. Bowel sounds present in all 4 quadrants GU: No diaper rash Neuro: Awake and alert Derm: Skin turgor normal. Skin warm and dry with no lesions MSK: Normal bulk and tone From the PE: list/highlight the presence or absence of objective findings to generate a list of pertinent “(+) or (-)” symptoms below: Pertinent Positive PE findings: Bilateral tympanic membranes with erythema and severe bulging, pharynx with erythema and exudates Pertinent Negative P [Show More]
Last updated: 3 years ago
Preview 1 out of 8 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$13.50
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Aug 31, 2022
Number of pages
8
Written in
Additional information
This document has been written for:
Uploaded
Aug 31, 2022
Downloads
0
Views
85