In the majority culture of America, coughing, sweating, and diarrhea are symptoms of an illness. For some individuals of Mexican-American origin, however, these symptoms are a normal part of living. The nurse recognizes
...
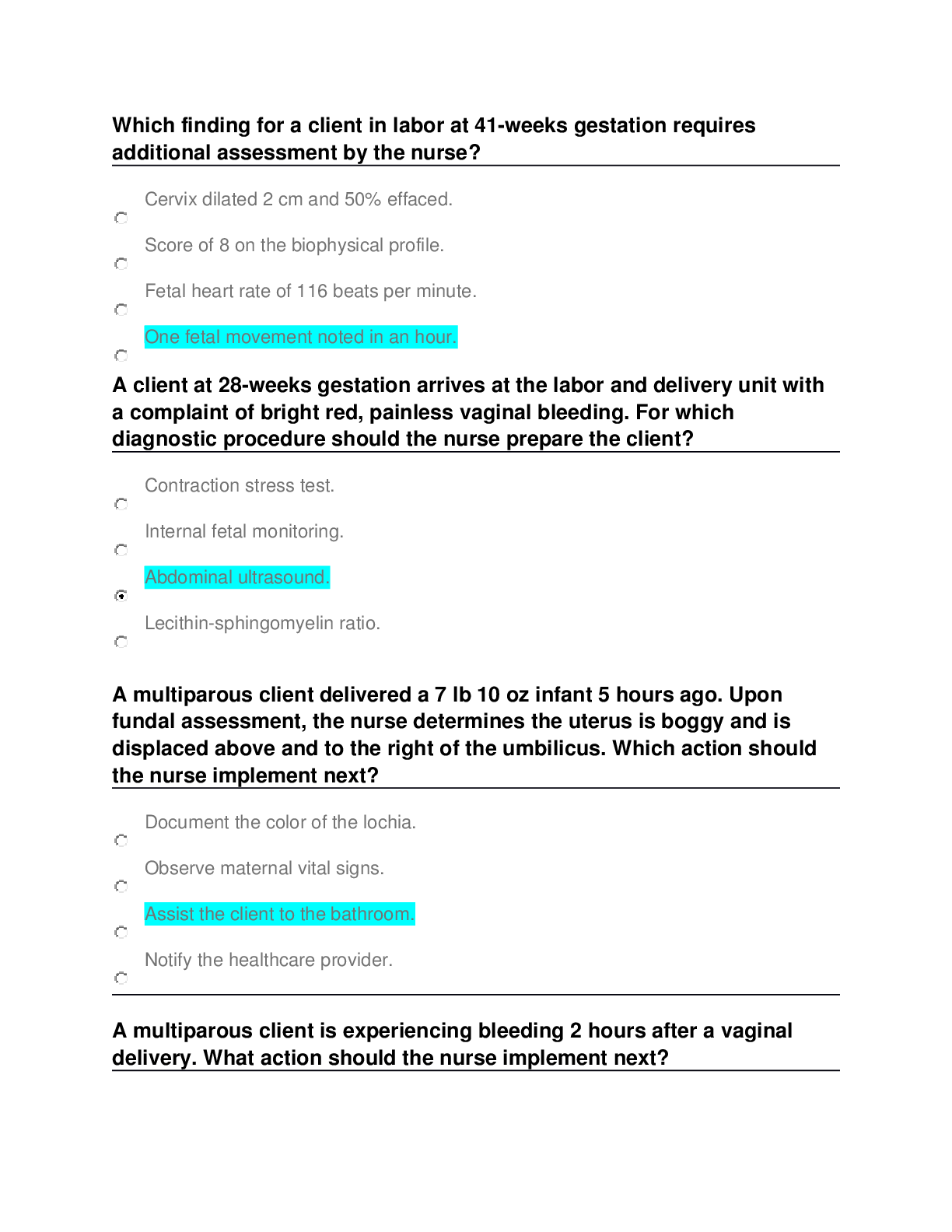
In the majority culture of America, coughing, sweating, and diarrhea are symptoms of an illness. For some individuals of Mexican-American origin, however, these symptoms are a normal part of living. The nurse recognizes that this is true, probably because Mexican-Americans:
A) have less efficient immune systems and are often ill.
B) consider these symptoms a part of normal living, not symptoms of ill health.
C) come from Mexico and coughing is normal and healthy there.
D) are usually in a lower socioeconomic group and are more likely to be sick. - ANSWER B) consider these symptoms a part of normal living, not symptoms of ill health.
Page: 27 The nurse needs to identify the meaning of health to the patient, remembering that concepts are derived, in part, from the way in which members of the cultural group define health
The nurse recognizes that working with children with a different cultural perspective may be especially difficult because:
A) children have spiritual needs that are influenced by their stages of development.
B) children have spiritual needs that are direct reflections of what is occurring in their homes.
C) religious beliefs rarely affect the parents' perceptions of the illness.
D) parents are often the decision makers, and they have no knowledge of their children's spiritual needs. - ANSWER A
Page: 20. Illness during childhood may be an especially difficult clinical situation. Children, as well as adults, have spiritual needs that vary according to the child's developmental level and the religious climate that exists in the family. The other statements are not correct.
The nurse is preparing to do a functional assessment. Which statement best describes the purpose of a functional assessment?
A. It assesses how the individual is coping with life at home.
B. It determines how children are meeting developmental milestones.
C. It can identify any problems with memory the individual may be experiencing.
D. It helps to determine how a person is managing day-to-day activities. - ANSWER D
Page: 56. The functional assessment measures how a person manages day-to-day activities. The other answers do not reflect the purpose of a functional assessment.
During an examination, the nurse can assess mental status by which activity?
A) Examining the patient's electroencephalogram
B) Observing the patient as he or she performs an IQ test
C) Observing the patient and inferring health or dysfunction
D) Examining the patient's response to a specific set of questions - ANSWER C
Pg. 67: Mental status cannot be scrutinized directly like the characteristics of skin or heart sounds. Its functioning is inferred through assessment of an individual's behaviors, such as consciousness, language, mood and affect, and other aspects.
The nurse would use bimanual palpation technique in which situation?
A) Palpating the thorax of an infant
B) Palpating the kidneys and uterus
C) Assessing pulsations and vibrations
D) Assessing the presence of tenderness and pain - ANSWER B
Pg 115: Bimanual palpation requires the use of both hands to envelop or capture certain body parts or organs such as the kidneys, uterus, or adnexa. The other situations are not appropriate for bimanual palpation.
The nurse is examining an infant and prepares to elicit the Moro reflex at which time during the examination?
A) When the infant is sleeping
B) At the end of the examination
C) Before auscultation of the thorax
D) Halfway through the examination - ANSWER B
Pg 122: Elicit the Moro or "startle" reflex at the end of the examination because it may cause the infant to cry.
During a nutritional assessment, why is it important for the nurse to ask a patient what medications he or she is taking?
A) Certain drugs can affect the metabolism of nutrients.
B) The nurse needs to assess the patient for allergic reactions.
C) Medications need to be documented on the record for the physician's review.
D) Medications can affect one's memory and ability to identify food eaten in the last 24 hours. - ANSWER A) Certain drugs can affect the metabolism of nutrients.
Page: 183
Analgesics, antacids, anticonvulsants, antibiotics, diuretics, laxatives, antineoplastic drugs, steroids, and oral contraceptives are drugs that can interact with nutrients, impairing their digestion, absorption, metabolism, or use. The other responses are not correct.
A 65-year-old man with emphysema and bronchitis has come to the clinic for a follow-up appointment. On assessment, the nurse might expect to see which assessment finding?
A) Anasarca
B) Scleroderma
C) Pedal erythema
D) Clubbing of the nails - ANSWER D
Pages: 213. Clubbing of the nails occurs with congenital cyanotic heart disease, neoplastic, and pulmonary diseases. The other responses are assessment findings not associated with pulmonary diseases.
A patient has been admitted for severe psoriasis. The nurse can expect to see what finding in the patient's fingernails?
A) Splinter hemorrhages
B) Paronychia
C) Pitting
D) Beau lines - ANSWER C
Pages: 236. Pitting nails are characterized by sharply defined pitting and crumbling of the nails with distal detachment, and they are associated with psoriasis. See Table 12-13 for descriptions of the other terms.
During an examination, the nurse knows that Paget's disease would be indicated by which of these assessment findings?
A) Positive Macewen sign
B) Premature closure of the sagittal suture
C) Headache, vertigo, tinnitus, and deafness
D) Elongated head with heavy eyebrow ridge - ANSWER C
Paget's disease occurs more often in males and is characterized by bowed long bones, sudden fractures, and enlarging skull bones that press on cranial nerves causing symptoms of headache, vertigo, tinnitus, and progressive deafness.
(This info is not in our texts for HA)
A woman comes to the clinic and states, "I've been sick for so long! My eyes have gotten so puffy, and my eyebrows and hair have become coarse and dry." The nurse will assess for other signs and symptoms of:
A) cachexia.
B) Parkinson's syndrome.
C) myxedema.
D) scleroderma. - ANSWER C
Pages: 277. Myxedema (hypothyroidism) is a deficiency of thyroid hormone that, when severe, causes a non pitting edema or myxedema. The patient will have a puffy edematous face especially around eyes (periorbital edema), coarse facial features, dry skin, and dry, coarse hair and eyebrows. See Table 13-4, Abnormal Facial Appearances with Chronic Illnesses, for descriptions of the other responses.
The physician reports that a patient with a neck tumor has a tracheal shift. The nurse is aware that this means that the patient's trachea is:
A) pulled to the affected side.
B) pushed to the unaffected side.
C) pulled downward.
D) pulled downward in a rhythmic pattern - ANSWER B
Pages: 262 The trachea is pushed to the unaffected side with an aortic aneurysm, a tumor, unilateral thyroid lobe enlargement, and pneumothorax. The trachea is pulled to the affected side with large atelectasis, pleural adhesions, or fibrosis. Tracheal tug is a rhythmic downward pull that is synchronous with systole and occurs with aortic arch aneurysm.
A mother asks when her newborn infant's eyesight will be developed. The nurse should reply:
A) "Vision is not totally developed until 2 years of age."
B) "Infants develop the ability to focus on an object at around 8 months."
C) "By about 3 months, infants develop more coordinated eye movements and can fixate on an object."
D) "Most infants have uncoordinated eye movements for the first year of life." - ANSWER C)
Page: 285. Eye movements may be poorly coordinated at birth, but by 3 to 4 months of age, the infant should establish binocularity and should be able to fixate on a single image with both eyes simultaneously.
The nurse notices the presence of periorbital edema when performing an eye assessment on a 70-year-old patient. The nurse should:
A) check for the presence of exophthalmos.
B) suspect that the patient has hyperthyroidism.
C) ask the patient if he or she has a history of heart failure.
D) assess for blepharitis because this is often associated with periorbital edema. - ANSWER C
Page: 313. Periorbital edema occurs with local infections, crying, and systemic conditions such as heart failure, renal failure, allergy, and hypothyroidism. Periorbital edema is not associated with blepharitis.
A patient comes to the emergency department after a boxing match, and his left eye is swollen almost shut. He has bruises on his face and neck. He says he is worried because he "can't see well" from his left eye. The physician suspects retinal damage. The nurse recognizes that signs of retinal detachment include:
A) loss of central vision.
B) shadow or diminished vision in one quadrant or one half of the visual field.
C) loss of peripheral vision.
D) sudden loss of pupillary constriction and accommodation. - ANSWER B
Page: 287 and 318. With retinal detachment, the person has shadows or diminished vision in one quadrant or one half of the visual field. The other responses are not signs of retinal detachment.
A 68-year-old woman is in the eye clinic for a checkup. She tells the nurse that she has been having trouble with reading the paper, sewing, and even seeing the faces of her grandchildren. On examination, the nurse notes that she has some loss of central vision but her peripheral vision is normal. These findings suggest that:
A) she may have macular degeneration.
B) her vision is normal for someone her age.
C) she has the beginning stages of cataract formation.
D) she has increased intraocular pressure or glaucoma. - ANSWER A
Page: 285. Macular degeneration is the most common cause of blindness. It is characterized by loss of central vision. Cataracts would show lens opacity. Chronic open-angle glaucoma, the most common type of glaucoma, involves a gradual loss of peripheral vision.
An ophthalmic examination reveals papilledema. The nurse is aware that this finding indicates:
A) retinal detachment.
B) diabetic retinopathy.
C) acute-angle glaucoma.
D) increased intracranial pressure. - ANSWER D
Pages: 322. Papilledema, or choked disk, is a serious sign of increased intracranial pressure, which is caused by a space-occupying mass such as a brain tumor or hematoma. This pressure causes venous stasis in the globe, showing redness, congestion, and elevation of the optic disc, blurred margins, hemorrhages, and absent venous pulsations. Papilledema is not associated with the conditions in the other responses.
During an examination, a patient states that she was diagnosed with open-angle
[Show More]