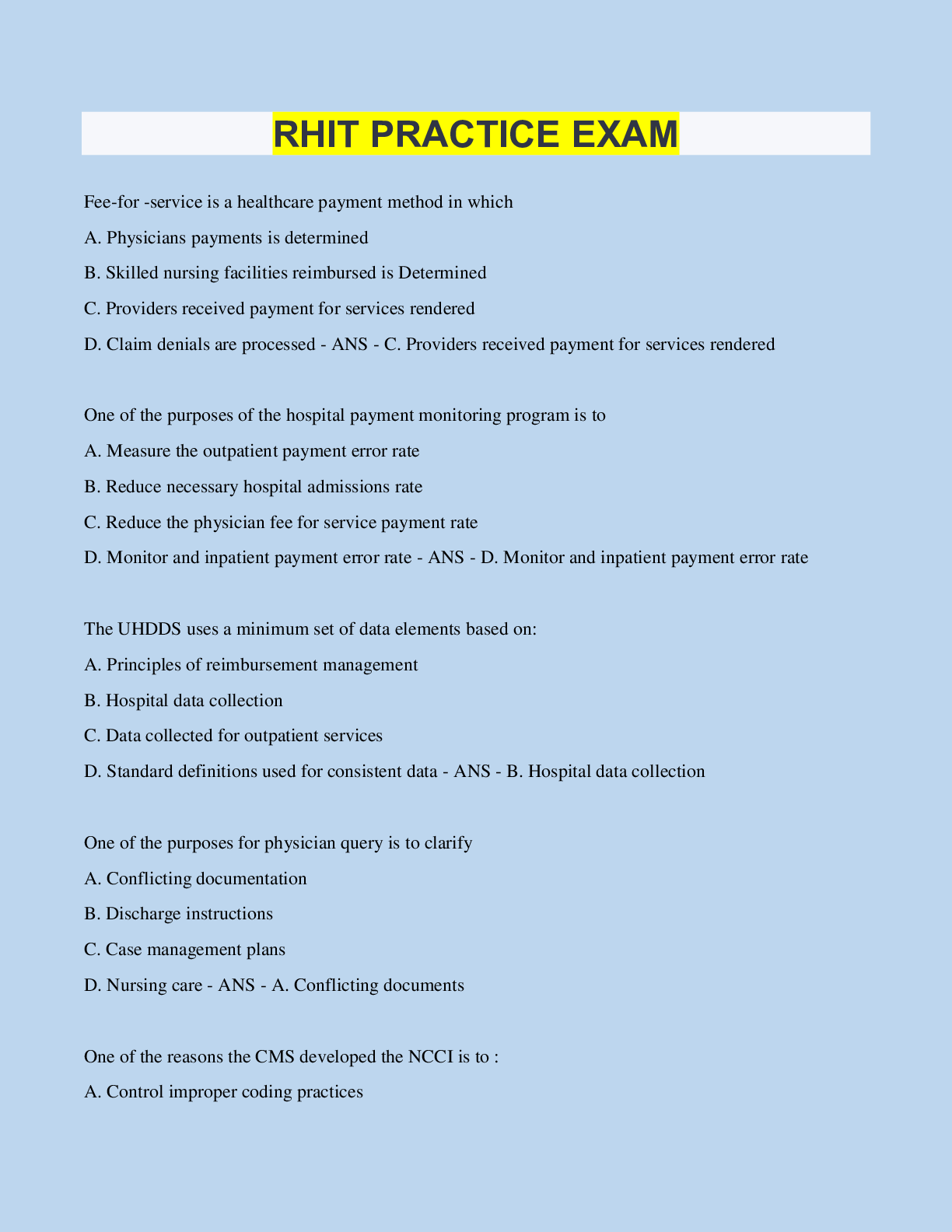
RHIT PRACTICE EXAM
Fee-for -service is a healthcare payment method in which
A. Physicians payments is determined
B. Skilled nursing facilities reimbursed is Determined
C. Providers received payment for services rende
...
RHIT PRACTICE EXAM
Fee-for -service is a healthcare payment method in which
A. Physicians payments is determined
B. Skilled nursing facilities reimbursed is Determined
C. Providers received payment for services rendered
D. Claim denials are processed - ANS - C. Providers received payment for services rendered
One of the purposes of the hospital payment monitoring program is to
A. Measure the outpatient payment error rate
B. Reduce necessary hospital admissions rate
C. Reduce the physician fee for service payment rate
D. Monitor and inpatient payment error rate - ANS - D. Monitor and inpatient payment error rate
The UHDDS uses a minimum set of data elements based on:
A. Principles of reimbursement management
B. Hospital data collection
C. Data collected for outpatient services
D. Standard definitions used for consistent data - ANS - B. Hospital data collection
One of the purposes for physician query is to clarify
A. Conflicting documentation
B. Discharge instructions
C. Case management plans
D. Nursing care - ANS - A. Conflicting documents
One of the reasons the CMS developed the NCCI is to :
A. Control improper coding practices
B. Monitor medically unlike edits (MUE)
C. Correct improper use of modifier 59
D. Circumvent coding guidelines - ANS - A. Code improper coding practices
The UHDDS defines "other diagnoses " as
A. All conditions that developed after the time of admission
B. Conditions that should be reported based on hospital
C. Diagnosis that have no bearing on the present on the present ho
D. All conditions that coexist at the time of admission - ANS - C. Diagnosis that have no bearing on the
present
All general acute healthcare providers must report a Present on Admission (POA) indicator. The purpose
of reporting POA is to indicate conditions:
A. Reported as a chronic condition from a previous condition
B. Ruled out during present admission
C. Diagnosed three days into the present admission
D. Ruled out from previous admission - ANS - A. Reported as a chronic condition from a previous
condition
Which of the following best describes the database used in every industry to store large amounts of
information.
A. Data Systems
B. Data banks
C. Data mining
D. Data Repositories - ANS - D. Data Repositories
What is the process of determining a users information needs and identifying relationships among the
data?
A. Data Repositories
B. Data Modeling
C. Data Mining
D. Data Quality - ANS - C. Data Mining
Healthcare common procedures coding systems (HCPCS) is divided into two levels of code sets. The
first level of HCPCS consist of - ANS - Current procedural terminology codes
CMS transfer policy generally results in: - ANS - Cost share
In addition to promoting internationally comparability. International Classifications of Diseases was
originally designed as a means for : - ANS - Processing mortality statistics
According to CMS Hospital Conditions of Participation, a medical history and physicians examination
must be completed for a patient no more than 30 days before or: - ANS - 24 hours after admission
When a medical record analyst identifies an unsigned order, their first step should be to : - ANS - Flag
the record for the physician
The purpose of quantitative analysis is to - ANS - Determine the completeness of patient health records
Demographics is the study of statistical information and : - ANS - Human Populations
The UHDDS requires that all significant procedures be reported. A significant procedure is defined as -
ANS - Surgical in nature
Which agency is responsibility for the maintenance and distribution of HCPCS level II codes? - ANS -
American Medical Association
A classification systems is an arrangement of elements into groups according to established criteria. In
ICD-9-CM, these elements are: - ANS - Complications, comorbidities, major comborbidities
The UHDDS does not require the following items; - ANS - Family History
The UHDDS applications of definitions was expanded to include which type of health care facilities: -
ANS - Ambulatory surgery centers
Current Procedure Terminology (CPT) was originally designed for reporting - ANS - Physician services
A patient presents to a physician-owned clinic for a broken wrist, x-rays are taken in the office. The
clinic will bill 73100 radiology examination, wrist, 2 views. With what modifier? - ANS - No modifier
necessary
CPT defines a diagnostic endoscopy as a "separate procedure". If a surgical endoscopy is performed in
conjunction with the - ANS -
[Show More]



.png)