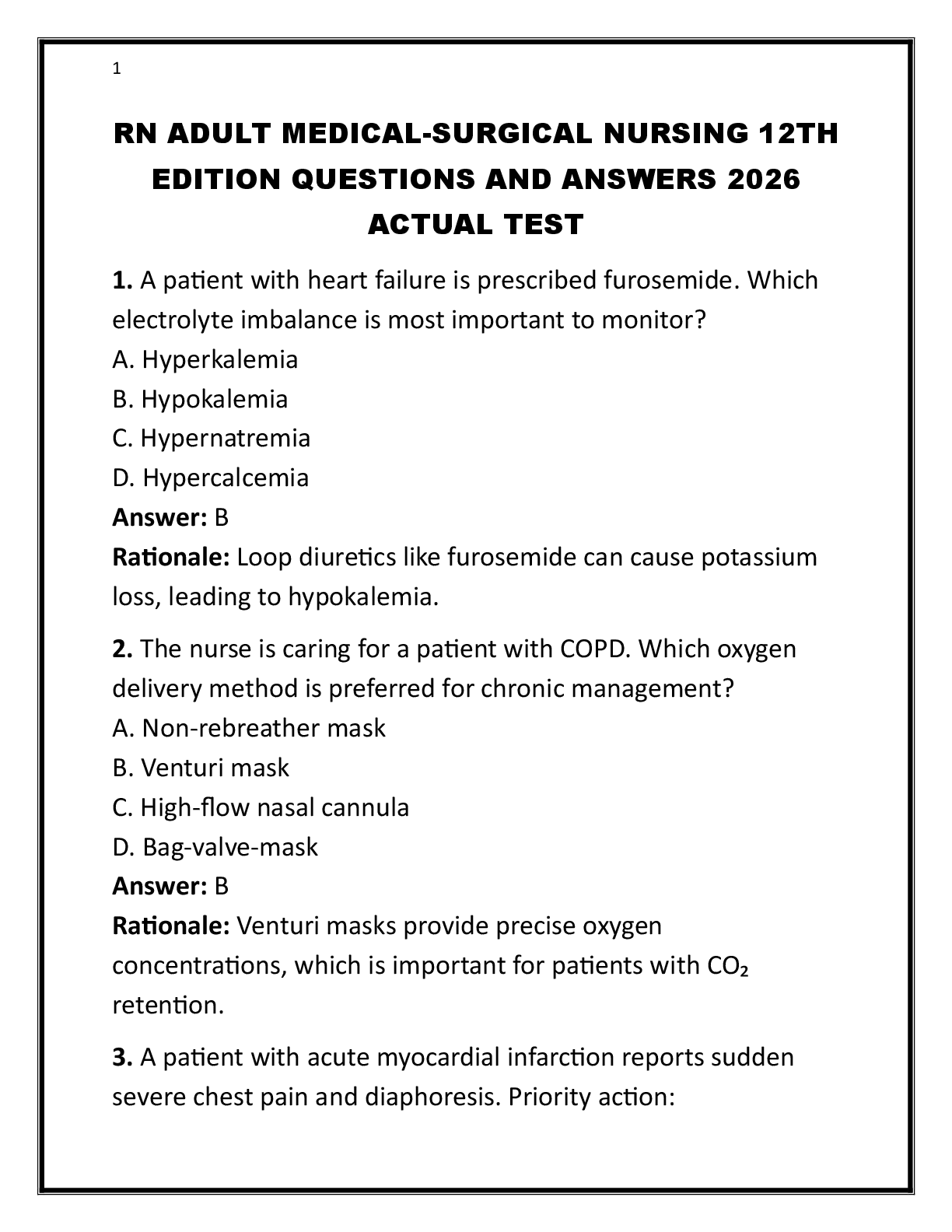
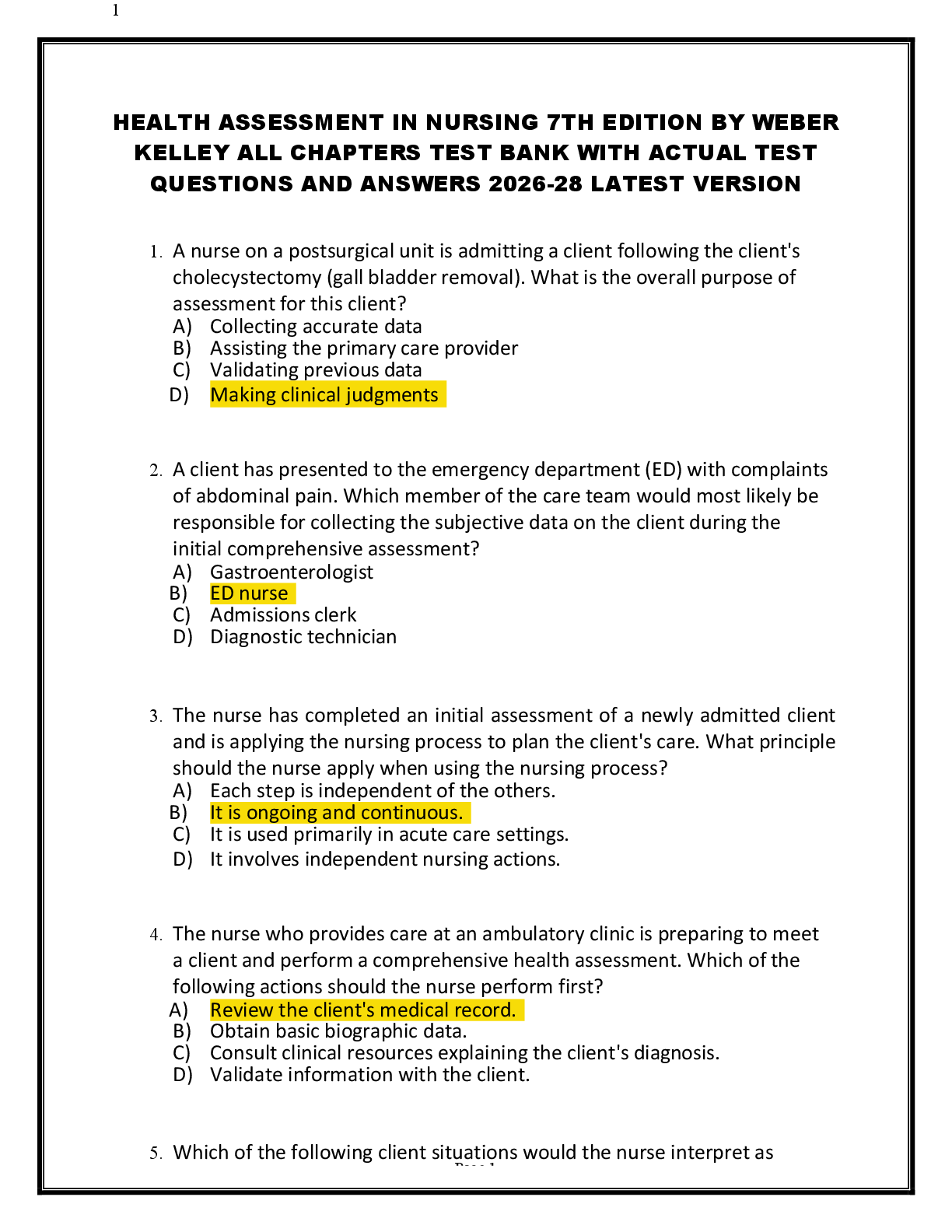
The peak pressure alarm is sounding on the ventilator of the client with a recent tracheostomy. What intervention should be done first?
A. Assess the client's respiratory status
B. Decrease the sensitivity of the ala
...
The peak pressure alarm is sounding on the ventilator of the client with a recent tracheostomy. What intervention should be done first?
A. Assess the client's respiratory status
B. Decrease the sensitivity of the alarm
C. Ensure that the connecting tubing is not kinked
D. Suction the client - ANSWER A
The client must always be assessed before attention is turned to equipment.
The client with respiratory failure has been intubated and placed on a ventilator and is requiring 100% oxygen delivery to maintain adequate oxygenation. Twenty-four hours later, the nurse notes new-onset crackles and decreased breath sounds, and the most recent ABGs show a PaO2 level of 95 mm Hg. The ventilator is not set to provide positive end-expiratory pressure (PEEP). Why is the nurse concerned?
A. The low PaO2 level may result in oxygen toxicity
B. The 100% oxygen delivery requirement indicates immediate extubation
C. Lung sounds may indicate absorption atelectasis
D. The level of oxygen delivery may indicate absorption atelectasis - ANSWER C
High levels of oxygen delivery can result in collapsed alveoli and absorption atelectasis. PEEP can help alveoli remain properly inflated.
The medical nurse is creating the care plan of an adult patient requiring mechanical ventilation. What nursing action is most appropriate?
A) Keep the patient in a low Fowlers position.
B) Perform tracheostomy care at least once per day.
C) Maintain continuous bedrest.
D) Monitor cuff pressure every 8 hours. - ANSWER D
The acute medical nurse is preparing to wean a patient from the ventilator. Which assessment parameter is most important for the nurse to assess?
A) Fluid intake for the last 24 hours
B) Baseline arterial blood gas (ABG) levels
C) Prior outcomes of weaning
D) Electrocardiogram (ECG) results - ANSWER B
A patient recovering from thoracic surgery is on long-term mechanical ventilation and becomes very frustrated when he tries to communicate. What intervention should the nurse perform to assist the patient?
A) Assure the patient that everything will be all right and that remaining calm is the best strategy.
B) Ask a family member to interpret what the patient is trying to communicate.
C) Ask the physician to wean the patient off the mechanical ventilator to allow the patient to speak freely.
D) Express empathy and then encourage the patient to write, use a picture board, or spell words with an alphabet board. - ANSWER D
The physician has ordered continuous positive airway pressure (CPAP) with the delivery of a patients high-flow oxygen therapy. The patient asks the nurse what the benefit of CPAP is. What would be the nurses best response?
A) CPAP allows a higher percentage of oxygen to be safely used.
B) CPAP allows a lower percentage of oxygen to be used with a similar effect.
C) CPAP allows for greater humidification of the oxygen that is administered.
D) CPAP allows for the elimination of bacterial growth in oxygen delivery systems. - ANSWER B
The nurse is caring for a patient who is ready to be weaned from the ventilator. In preparing to assist in the collaborative process of weaning the patient from a ventilator, the nurse is aware that the weaning of the patient will progress in what order?
A) Removal from the ventilator, tube, and then oxygen
B) Removal from oxygen, ventilator, and then tube
C) Removal of the tube, oxygen, and then ventilator
D) Removal from oxygen, tube, and then ventilator - ANSWER A
The critical care nurse and the other members of the care team are assessing the patient to see if he is ready to be weaned from the ventilator. What are the most important predictors of successful weaning that the nurse should identify?
A) Stable vital signs and ABGs
B) Pulse oximetry above 80% and stable vital signs
C) Stable nutritional status and ABGs
D) Normal orientation and level of consciousness - ANSWER A
The nurse is caring for a client with an endotracheal tube who is on a ventilator. When assessing the client, the nurse knows to maintain what cuff pressure to maintain appropriate pressure on the tracheal wall?
A) Between 10 and 15 mm Hg
B) Between 15 and 20 mm Hg
C) Between 20 and 25 mm Hg
D) Between 25 and 30 mm Hg - ANSWER B
The decision has been made to discharge a ventilator-dependent patient home. The nurse is developing a teaching plan for this patient and his family. What would be most important to include in this teaching plan?
A) Administration of inhaled corticosteroids
B) Assessment of neurologic status
C) Turning and coughing
D) Signs of pulmonary infection - ANSWER D
The RN is supervising a nursing student who will suction a patient on a mechanical ventilator. Which actions indicate that the student has a correct understanding of this procedure? Select all that apply.
1.) The student nurse uses a sterile catheter and glove.
2.)The student nurse applies suction while inserting the catheter.
3.)The student nurse applies suction during catheter removal.
4.) The student nurses uses a twirling motion when withdrawing the catheter.
5.)The student nurse uses a no. 12 French catheter.
6.)The student nurse applies suction for at least 20 seconds. - ANSWER 1345
The standard size catheter for an adult is a no. 12 or 14 French. Infection is possible because each catheter pass can introduce bacteria into the trachea. In the hospital, use sterile technique for suctioning and for all suctioning equipment (e.g., suction catheters, gloves, saline or water). Apply suction only during catheter withdrawal and use a twirling motion to prevent the catheter from grabbing tracheal mucosa and leading to damage to tracheal tissue. Apply suction for no more than 10 seconds to minimize hypoxemia during suctioning.
The purpose of adding PEEP to positive pressure ventilation is to
a. increase functional residual capacity and improve oxygenation
b. increase FIO2 in an attempt to wean the patient and avoid O2 toxicity
c. determine if the patient is in synchrony with the ventilator or needs to be paralyzed
d. determine is the patient is able to be weaned and avoid the risk of pneumomediastinum - ANSWER A
The nursing management of a patient with an artificial airway includes
a. maintaining the ET tube cuff pressure at 30 cm H20
b. routine suctioning of the tube at least every 2 hours
c. observing for cardiac dysrhythmias during suctioning
d. preventing tube dislodgment by limiting mouth care to lubrication of the lips - ANSWER C
The nurses monitors the patient with positive pressure mechanical ventilation for
a. paralytic ileus because pressure on the abdominal contents affects bowel motility
b. diuresis and sodium depletion because of increased release of atrial natriuretic peptide
c. signs of cardiovascular insufficiency because pressure in the chest impedes venous return
d. respiratory acidosis in a patient with COPD because of alveolar hyperventilation and increased PaO2 levels - ANSWER C
Although his oxygen saturation is above 92%, an orally intubated, mechanically ventilated patient is restless and very anxious. What interventions will most likely decrease the risk of accidental extubation? Select all that apply
a. administer sedatives
b. have a caregiver stay with the patient
c. obtain an order and apply soft wrist restraints
d. remind the patient that he needs the tube inserted to breathe
e. move the patient to an area close to the nurse's station for closer observation - ANSWER AB
Which patient's medical diagnoses should the nurse know are most likely to need mechanical ventilation? Select all that apply
a. sleep apnea
b. cystic fibrosis
c. acute kidney injury
d. type 2 DM
e. acute respiratory distress syndrome (ARDS) - ANSWER BE
What characteristics describe positive pressure ventilators? Select all that apply
a. require an artificial airway
b. applied to outside of body
c. most similar to physiologic ventilation
d. most frequently used with critically ill patients
e. frequently used in the home for neuromuscular or nervous system disorders - ANSWER AD
What is included in the description of positive pressure ventilation? Select all that apply
a. peak inspiratory pressure predetermined
b. consistent volume delivered with each breath
c. increased risk for hyperventilation and hypoventilation
d. preset volume of gas delivered with variable pressure based on compliance
e. volume delivered varies based on selected pressure and patient lung compliance - ANSWER ACE
A patient in acute respiratory failure is receiving ACV with a positive end-expiratory pressure (PEEP) of 10 cm H20. What sign alerts the nurse to undesirable effects of increased airway and thoracic pressure?
a. decreased BP
b. decreased PaO2
c. increased crackles
d. decreased spontaneous respirations - ANSWER A
What should the nurse recognize as a factor commonly responsible for sodium and fluid retention in the patient on mechanical ventilation?
a. increased release of ADH
b. increased release of atrial natriuretic factor
c. increased insensible water loss via the airway
d. decreased renal perfusion with release of renin - ANSWER D
A patient receiving mechanical ventilation is very anxious and agitated, and neuromuscular blocking agents are used to promote vasodilation. What should the nurse recognize about the care of this patient?
a. the patient will be too sedated to be aware of the details of care
b. caregivers should be encouraged to provide stimulation and diversion
c. the patient should always be addressed and explanations of care given
d. communication will not be possible with the use of neuromuscular blocking agents - ANSWER C
The nurse determines that alveolar hypoventilation is occurring in a patient on a ventilator when what happens?
a. the patient develops cardiac dysrhythmias
b. auscultation reveals an air leak around the ET tube cuff
c. ABG results show a PaCO2 of 32 mm Hg and a pH of 7.47
d. the patient tries to breathe faster than the ventilator setting - ANSWER B
What plan should the nurse use when weaning a patient from a ventilator?
a. decrease the delivered FIO2 concentration
b. intermittent trials of spontaneous ventilation followed by ventilatory support to provide rest
[Show More]