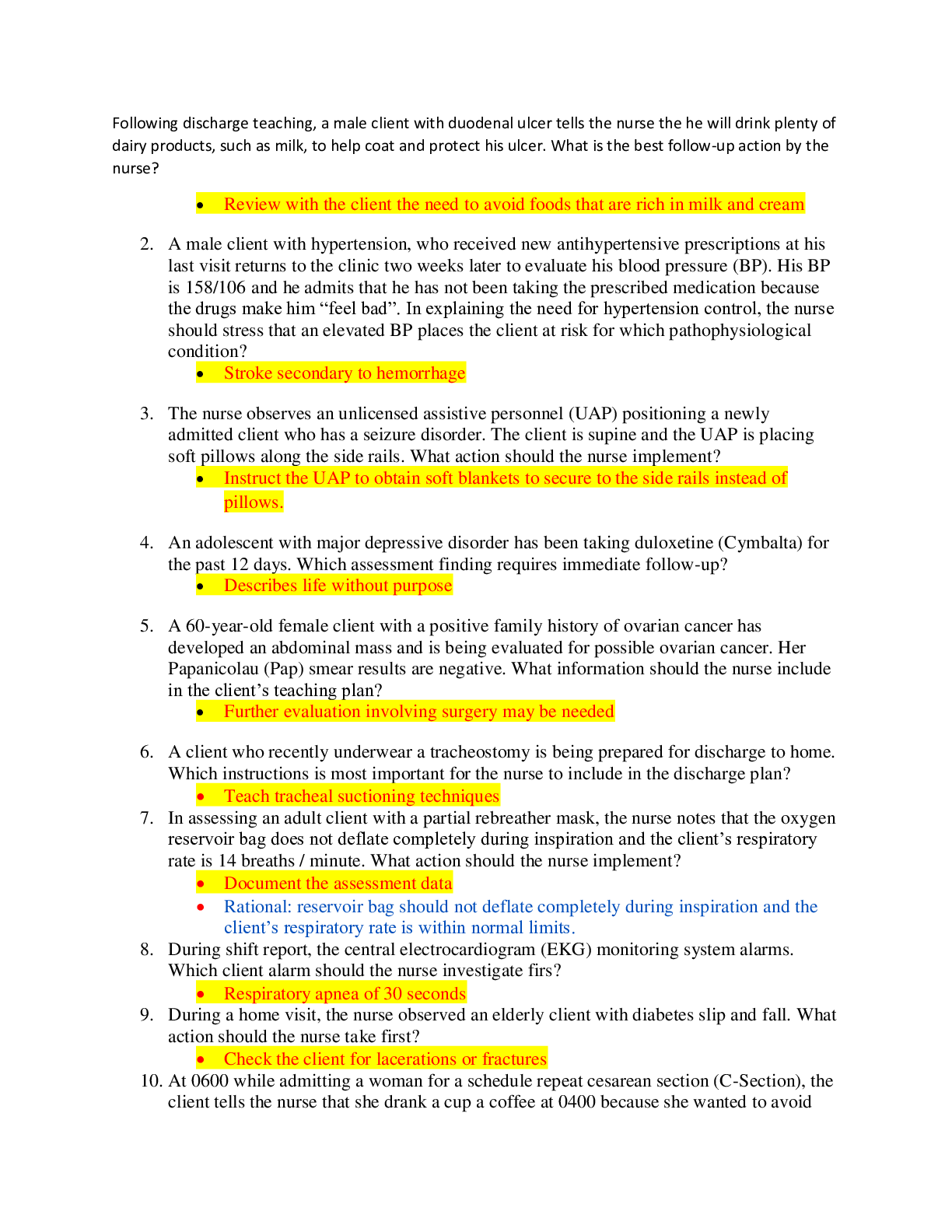
MS EXAM - QUESTIONS AND ANSWERS LATEST 2021
Document Content and Description Below
MS EXAM - QUESTIONS Time Remaining (Minutes): 30 1. A patient’s blood transfusion has been hanging for 2 hours. The patient is complaining of a raised itchy rash and shortness of breath; she is ... wheezing, anxious, and very restless. Which of the following is suggested by the assessment findings? a. Acute transfusion reaction b. Circulatory overload c. Febrile reaction d. Hemolytic reaction 2. When evaluating a patient with symptoms of shock, the nurse must differentiate between neurogenic and hypovolemic shock. How do the symptoms of neurogenic shock differ from hypovolemic shock? a. In hypovolemic shock, capillary refill is brisk. b. In hypovolemic shock, there is bradycardia. c. In neurogenic shock, capillary refill is delayed. d. In neurogenic shock, the skin is warm and dry. 3. A 67-year-old man had a physical examination prior to beginning volunteer work at a hospital. A routine chest x-ray demonstrated left ventricular hypertrophy. His blood pressure was 180/110. He is 45 pounds overweight, his diet is high in sodium and fat, and he has a strong family history of hypertension. His provider placed him on anti-hypertensive medication, a diet low in sodium and fat, and an exercise regimen. On his next visit to the provider, his willingness to adhere to the treatment plan would best be determined with: a. a blood pressure reading of 130/70 and a 5 pound weight loss. b. no evidence of left ventricular hypertrophy on the chest x-ray. c. no side effects from the medication and an accurate pill count. d. serum blood levels of the anti-hypertensive medication within a therapeutic range. 4. A patient is being discharged and will continue enteral feedings at home. Which of the following statements by a family member indicates the need for further teaching? a. “I should anticipate that he will gain about 2 pounds per day now that he is on continuous feedings." b. “I should use prepared or open formula within 24 hours and store unused portions in the refrigerator.” c. “If he develops diarrhea lasting for more than 2-3 days, I will contact the doctor or nurse.” d. “It is important to get him to sit up in a chair during feedings or keep the head of his bed elevated.” 5. Prior to administering digoxin (Lanoxin®) to a patient with congestive heart failure, the nurse needs to assess the: a. apical pulse for 1 minute. b. radial pulse for 1 minute. c. radial pulse for 2 minutes. d. respiratory rate for 1 minute. 6. The most reliable indicator of renal function is: a. alanine aminotransferase (ALT). b. serum creatinine. c. serum potassium. d. urinalysis. 7. Crackles heard on lung auscultation indicate: a. airway narrowing. b. bronchospasm. c. fluid in the alveoli. d. pulmonary hypertension. 8. A 27-year-old patient reports right leg pain 3 hours following a knee reduction. The first thing the nurse should do is: a. assess the patient's vital signs. b. elevate the right leg. c. perform a lower extremity neurovascular check. d. remind the patient that he has a PCA pump and instruct him to give himself another dose of pain medication. 9. A 70-year-old homeless person is admitted with pneumonia. The patient is weak, emaciated, and febrile. The provider orders intermittent enteral feedings via nasogastric tube. While preparing to insert the nasogastric tube, the nurse should instruct the patient that once the tube passes through the oropharynx, he should: a. cough as the tube passes. b. hold his breath as the tube passes. c. swallow as the tube passes. d. tilt his head backwards. 10. A 47-year-old patient is admitted for colon surgery. Although he has no known infection, intravenous antibiotics are begun 2 hours prior to surgery. The rationale for giving him antibiotics prior to surgery is to: a. provide a cathartic reaction within the colon. b. reduce the risk of intraoperative fever. c. reduce the risk of wound infection from anaerobic bacteria. d. relieve the client’s concern regarding possible infection. 11. Which type of insulin is used for intravenous administration? a. Human insulin b. Long-acting insulin c. NPH insulin d. Regular insulin 12. An 18-year-old girl is admitted to the hospital with a depressed skull fracture as a result of a car accident. If the patient exhibited a rising pulse rate and lowering blood pressure, the nurse would suspect that the patient is: a. beginning to experience a dangerously high level of anxiety. b. having a sudden and severe increase in intracranial pressure. c. having intracranial bleeding. d. showing signs of an internal injury in addition to the head injury. 13. The nurse should instruct a patient receiving heparin therapy to report: a. constipation. b. dyspnea. c. hematuria. d. pruritis. 14. A patient had a right below the knee amputation (BKA) 4 days ago. His incision is healing well, and he has gotten out of bed several times. Each time after returning to bed, he has experienced pain as if it were located in his right foot. The nurse should explain to the patient that: a. he will get accustomed to phantom pain as he continues to do normal, everyday activities. b. it is phantom pain and may occur because the nerves still carry pain sensation to the brain, even though the limb has been amputated. The pain is real and intense; it should be treated as such. c. phantom pain is caused by trauma and edema at the wound site and will decrease when the edema decreases. d. the pain is psychological and should not be treated. 15. A patient is receiving gentamicin (Garamycin®) IV for treatment of a wound infection. Knowing this drug is ototoxic, the nurse should: a. advise the patient to discontinue the medication at the first sign of dizziness. b. instruct the patient to use the Valsalva maneuver to equalize middle ear pressure to prevent hearing loss. c. instruct the patient to report any signs of tinnitus, dizziness, or difficulty hearing. d. order audiometric testing in order to determine if hearing loss has been caused by the medication. 16. A 55-year-old man has recently been diagnosed with hypertension. The provider orders a low-sodium diet for the patient. What should the nurse’s initial response be when the patient asks, “What does salt have to do with high blood pressure?” a. “Salt affects your blood vessels and causes your blood pressure to be high.” b. “Salt is needed to maintain blood pressure, but too much will cause hypertension.” c. “The reason too much sodium is associated with hypertension is unknown.” d. “Too much salt in your diet can cause you to retain fluid, and that increases your blood pressure.” 17. The preliminary diagnosis of pancreatitis would be confirmed if the patient’s blood work showed a significant elevation in: a. amylase. b. glucose. c. potassium. d. trypsin. 18. Which of the following is a complication of atrial fibrillation? a. Hypertension b. Increased cardiac output c. Lethal arrhythmia d. Stasis of blood in the atria 19. Which of the following nursing actions would be most helpful in promoting communication in a patient experiencing aphasia? a. Correcting the patient's speech errors b. Speaking loudly c. Using short sentences d. Writing out all directions 20. When inspecting a cardiovascular patient, the nurse notes that the patient needs to sit upright to breathe. This behavior is most indicative of: a. angina. b. anxiety. c. congestive heart failure (CHF). d. pericarditis. 21. A 52-year-old patient who underwent an exploratory laparoscopy for a bowel obstruction begins to report hunger on the third day after the procedure. The NG tube was removed this morning, and an IV of D5 ½ NS is running at 125 mL/hr. The patient asks when he can get rid of the IV and start eating. The nurse knows that the patient will be able to begin taking oral fluids and nourishment when: a. he has bowel sounds in all four quadrants. b. he is able to eat a full meal without evidence of nausea and vomiting. c. he shows no signs of wound infection. d. his blood pressure returns to its preoperative baseline or higher. 22. A 55-year-old patient is unconscious, and his provider has decided to begin tube feeding using a small-bore silicone feeding tube. After the tube is inserted, what is the most reliable way to confirm appropriate tube placement? a. Aspirate gastric content. b. Auscultate air insufflated through the tube. c. Obtain an x-ray (KUB). d. Place the tip of the tube under water and observe for air bubbles. 23. A 19-year-old patient fell to the ground from a ladder approximately 3 feet high. The patient did not lose consciousness but was taken to the emergency department by a friend to have a scalp laceration sutured. The nurse should instruct the patient to: a. clean the sutured laceration 4 times daily with povidone-iodine (Betadine®). b. remove the scalp sutures after 5 days. c. return to the hospital immediately if confusion, nausea, or vomiting occur. d. take meperidine (Demerol®) 50 mg by mouth every 4-6 hours as needed for headache. 24. Which of the following is a warfarin (Coumadin®) antagonist? a. Diazepam (Valium®) b. Diphenhydramine (Benadryl®) c. Epinephrine (Adrenaline®) d. Phytonadione (Mephyton®) 25. Which of the following is an expected outcome following intravenous administration of furosemide (Lasix®)? a. Decreased PVCs b. Decreased urine output c. Increased blood pressure d. Increased urine output 26. On admission, the patient has signs and symptoms of pulmonary edema. Which of the following is the most appropriate position for this patient? a. High Fowler's b. Left side-lying c. Sitting in a chair d. Supine with feet elevated 27. A patient diagnosed with severe anemia is to receive 2 units of packed red blood cells (PRBC). Prior to starting the blood infusion, the nurse must: a. get microdrip tubing for blood administration. b. hang ringer’s lactate as the companion fluid. c. have the charge nurse get the blood from the blood bank. d. take a baseline set of vital signs. 28. Which of the following physician’s orders for a patient with chronic arterial insufficiency should the nurse question? a. Arteriogram in the morning b. Elevate legs on pillow c. Neurovascular checks q 2 hrs d. No smoking 29. Which of the following complications is responsible for the most deaths following acute myocardial infarction? a. Cardiac dysrhythmia b. Pulmonary embolism c. Severe anxiety d. Ventricular septal rupture 30. Which of the following is the position of choice for a client with severe ascites? a. Fowler's b. Prone c. Reverse trendelenberg d. Side-lying [Show More]
Last updated: 2 years ago
Preview 1 out of 9 pages
.png)
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$7.50
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Jan 13, 2021
Number of pages
9
Written in
Additional information
This document has been written for:
Uploaded
Jan 13, 2021
Downloads
0
Views
102

.png)






.png)