*NURSING > Class Notes > South University, SavannahSouth University, Savannah - FAMILY NUR NSG6001. Class Notes and Study Gui (All)
South University, SavannahSouth University, Savannah - FAMILY NUR NSG6001. Class Notes and Study Guide
Document Content and Description Below
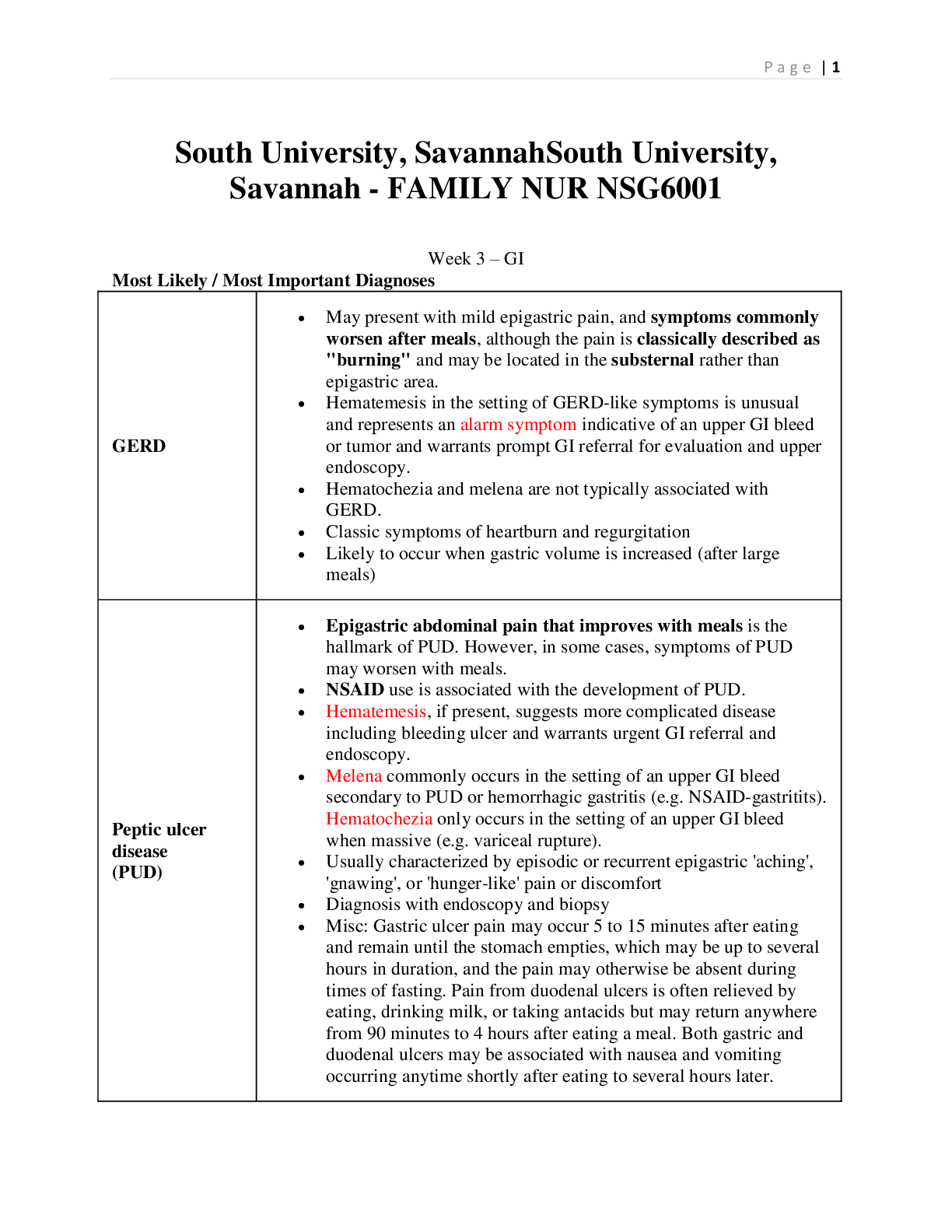
South University, SavannahSouth University, Savannah - FAMILY NUR NSG6001 Week 3 – GI Most Likely / Most Important Diagnoses GERD • May present with mild epigastric pain, and symptoms commo... nly worsen after meals, although the pain is classically described as "burning" and may be located in the substernal rather than epigastric area. • Hematemesis in the setting of GERD-like symptoms is unusual and represents an alarm symptom indicative of an upper GI bleed or tumor and warrants prompt GI referral for evaluation and upper endoscopy. • Hematochezia and melena are not typically associated with GERD. • Classic symptoms of heartburn and regurgitation • Likely to occur when gastric volume is increased (after large meals) Peptic ulcer disease (PUD) • Epigastric abdominal pain that improves with meals is the hallmark of PUD. However, in some cases, symptoms of PUD may worsen with meals. • NSAID use is associated with the development of PUD. • Hematemesis, if present, suggests more complicated disease including bleeding ulcer and warrants urgent GI referral and endoscopy. • Melena commonly occurs in the setting of an upper GI bleed secondary to PUD or hemorrhagic gastritis (e.g. NSAID-gastritits). Hematochezia only occurs in the setting of an upper GI bleed when massive (e.g. variceal rupture). • Usually characterized by episodic or recurrent epigastric 'aching', 'gnawing', or 'hunger-like' pain or discomfort • Diagnosis with endoscopy and biopsy • Misc: Gastric ulcer pain may occur 5 to 15 minutes after eating and remain until the stomach empties, which may be up to several hours in duration, and the pain may otherwise be absent during times of fasting. Pain from duodenal ulcers is often relieved by eating, drinking milk, or taking antacids but may return anywhere from 90 minutes to 4 hours after eating a meal. Both gastric and duodenal ulcers may be associated with nausea and vomiting occurring anytime shortly after eating to several hours later. Gastritis • Inflammation or irritation of the stomach lining often causing sharp epigastric pain. This pain may be variably worsened or improved with eating food. • Inflammatory forms of gastritis may be caused by chronic infections such as H. pylori or acute infections such as viruses. • Non-inflammatory forms of 'gastritis' are more properly histologically termed gastropathy. These may be caused by chemical irritants to the stomach, including alcohol and NSAIDs. Agents that Cause or Contribute to Peptic Ulcer Disease • Aspirin and other non-steroidal anti-inflammatory drugs (NSAIDs) are the predominant pharmacologic agents that contribute to the development of PUD. Classically, the elderly are at the highest attributable risk of ulceration and perforation due to chronic NSAID use. Chronic NSAID use is a leading cause of morbidity in the elderly. • Moderate to severe physiologic stress may lead to stress ulceration, predominantly in patients in the intensive care unit (ICU). • Colonization of the stomach by H. pylori renders the underlying mucosa more vulnerable to peptic acid damage by disrupting the mucous layer, liberating enzymes and toxins, and adhering to the gastric epithelium. In addition, the body's immune response to H. pylori incites an inflammatory reaction that contributes to tissue injury and leads to chronic gastritis. In most individuals the chronic gastritis is asymptomatic and does not progress. In some cases, however, altered gastric secretion coupled with tissue injury leads to peptic ulcer disease. In other cases, gastritis progresses to mucosal atrophy, intestinal metaplasia, and eventually gastric carcinoma. Rarely, persistent immune stimulation of gastric lymphoid tissue can lead to gastric lymphoma. COMPLICATIONS OF GERD AND PUD GERD • Esophagitis develops when the mucosal defenses that normally counteract the effect of injurious agents are overwhelmed by refluxed acid, pepsin, or bile. • Peptic strictures from fibrosis and constriction occur in about 10 percent of patients with reflux esophagitis. • Replacement of the squamous epithelium of the esophagus by columnar epithelium (Barrett's esophagus) may result from reflux esophagitis. Two to five percent of cases of Barrett's esophagus may be further complicated by adenocarcinoma. PUD • Hemorrhage or perforation into the peritoneal cavity or adjacent organs (causing severe, persistent abdominal pain). • Ulcer scar healing or inflammation can impair gastric emptying leading to gastric outlet obstruction syndrome. Alarm Symptoms Warranting Referral to Gastroenterology for Endoscopy Dysphagia Difficulty in swallowing. Dysphagia to solids suggests possible development of peptic stricture. Rapidly progressive dysphagia potentially indicates adenocarcinoma. Dysphagia to liquids suggests development of a motility disorder. Initial onset of upper GI symptoms after age 50 Increased chance of cancer. Early satiety May be associated with gastroparesis or gastric outlet obstruction (stricture or cancer). Hematemesis Vomiting blood, which suggests bleeding ulcer, mucosal erosions (erosive gastritis/esophagitis), esophageal tear (Mallory-Weiss), or esophageal varices. Hematochezia Passing red blood with stool, which may indicate a rapidly bleeding ulcer or mucosal erosions. Iron deficiency anemia The presence of hematemesis, hematochezia, and/or iron deficiency anemia may indicate possible bleeding from a peptic ulcer, mucosal erosions, or cancer. Odynophagia Painful swallowing, which is associated with infections (e.g. candida), erosions, or cancer. Recurrent vomiting Suggestive of gastric outlet obstruction. Weight loss Associated with malignancy. Treatment GERD: Self-directed trial of over-the-counter anti-secretory therapy, either a histamine-2 receptor antagonist or a proton-pump inhibitor (PPI) Lifestyle modifications. PUD from H. pylori "Triple therapy" for 10 to 14 days (70% to 85% eradication rate): • PPI standard dose twice daily (esomeprazole is dosed once daily) • Amoxicillin 1 g twice daily • Clarithromycin 500 mg twice daily "Quadruple therapy" for 10 to 14 days (75% to 90% eradication rate): • PPI standard dose once or twice daily (OR ranitidine 150 mg twice daily) • Metronidazole 250 mg four times daily • Tetracycline 500 mg four times daily • Bismuth subsalicylate 525 mg four times daily An alternative 10- to 14-day triple regimen to consider in patients who are allergic to penicillin (70% to 85% eradication rate): • PPI standard dose twice daily • Clarithromycin 500 mg twice daily • Metronidazole 500 mg twice daily Evaluation of Persistent Symptoms of Dyspepsia - Investigating H. pylori Eradication The fecal antigen test and urea breath test are reasonable next steps to evaluate eradication of H. pylori. 1. The fecal antigen test – less costly 2. The urea breath test • If the fecal antigen test or the urea breath test is positive, the patient will require re-treatment for a resistant infection, but this should not be given prior to testing for the presence of active H. pylori infection. • If the fecal antigen test or urea breath test is negative, and the patient continues to have symptoms, refer to GI for EGD and mucosal biopsy. Abdominal pains and infections Visceral pain – dull, crampy, constant – poorly localized. Parietal pain – sharp, well-localized (appendicitis) Referred pain – aching – away from the disease process RUQ – emanates from the chest cavity, liver, gallbladder, stomach, bowel, right kidney or ureter. LUQ – heart or chest cavity, spleen, stomach, pancreas, left kidney or ureter. LLQ bowel, eft ureter, pelvis – most common is diverticulitis. RLQ – appendix, bowel, right ureter, pelvis – most common appendicitis Consider cholecystitis or PUD too. Migrating pain across several quadrants typically associated with bowel Abdominal wall pain from trauma or inflammation – occurs anywhere Elderly <c/o pain but present as hypotensive, lethargic, or confused. Female – lower abdominal or pelvic pain suggests Gyn problem. Always perform pregnancy test, even if tubal ligation, to r/o ectopic. Consider PID. Appendicitis Described as simple, gangrenous or perforated based on operative findings. Gangrene and perforation develop in 24-36 hours. 3 signs and symptoms 1. Pain that starts in the epigastrium or periumbilical – migrates to RLQ – rigid abdomen 2. Acute onset 3. Anorexia n/v, constipation with fever Physical exam Palpation in non-affected area, ending in painful area to determine area of localized tenderness. Usually RLQ between umbilicus and anterosuperior iliac spine (McBurney point). Rovsing sign (RLQ pain) elicited by palpating LLQ. Peritoneal irritation by guarging, rebound tenderness and obturator sign (passive rotation of RLL with pt supine, rt hip and knee flexed) and psoas sign (supine pt raises straight RLL against resistance). Rectal exam to r/o mass. Diagnostics CBC with diff (elevated WBC) Amylase and lipase CRP Serum B-hCG (pregnancy test) Sickeldex test (sickle cell disease) UA Imaging not usually necessary but if atypical or extremes of age. U/S CT Treatment Appendectomy within 24 hours of symptoms to prevent perforation and peritonitis. Antibiotics Complications Gangrene,perforation with peritonitis, abscess, pylephlebitis (suspect if shaking chills), septicemia, urinary retention and infections, SBO, mesenteric thrombophlebitis. Anorectal complaints Hemorrhoids – present with bleeding, pruritus, protrusion, and pain. Internal usually painless but may cause bleeding. Four categories 1st degree – cause bright red, painless bleeding and may bulge but no prolapse 2nd degree – prolapse during defecation, reduce spontaneously. Bleeding and itching. 3rd degree – prolapse with defecation, manual reduction. Pain 2nd to local ischemia and mucoid drainage. 4th degree – permanently prolapsed, not reducible. If incarcerated, urgent surgery. Exam – knee-chest, lithotomy or left lateral prone. Internal hemorrhoids best visualized with anoscope. Rectal exam – internal not palpable unless thrombosed. External thrombosed appears dark, bluish nodular. Severe pain suggests gangrenous or thrombosed hemorrhoid. Gangrene requires immediate surgical evaluation. Diagnostics CBC - If heavy, prolonged bleeding Stool cards Treatment High fiber diet Increase fluids Topical analgesics or hydrocortisone Sitz bath Oral analgesics Thrombosed within 3 days, evacute Complications 4th degree at risk for strangulation – can be gangrenous Ligation associated with increased pain, infection and sepsis. Hemorrhoidectomy associated with UTI, retention, impaction Anal fissure Painful linear cracks or tears in the lining of the anal canal. Seen often in IBS, cancer, Crohn’s, TB, HIV, syphilis or leukemia. Caused by trauma from large, hard stool, chemical burn from diarrhea, and anal stenosis. S/S – severe rectal pain during and after BM + small amounts of bright red rectal bleeding on TP. Exam – Left lateral decubitus, apply topical anesthetic. Most located at posterior midline, the remainder at anterior midline. If more lateral may be STD, TB, HIV, ulcerative colitis, Crohn’s, cancer, etc – refer to specialist. Treatment Increase fiber Stool softeners, sitz bath Suppositories or foam anti-inflammatory agents Topical anesthetic applied before BM. Chronic fissures – topical or oral CCB or topical nitrates If failed topical treatment – botox Healing takes up to 6 weeks. Pruritus Ani Itching – idiopathic – mostly nocturnal. Check for pinworms. Anorectal abscess or fistula Abscess – acute Fistula – chronic Men > women, Chron’s Bacterial from the anal crypt glands causing acute pain and swelling. Pain increases with movement, sitting, or BM – persistent purulent drainage. Diagnostics CBC with diff CT or MRI if recurring or complex ie IBS Colonoscopy Treatment I&D Flagyl Cholelithiasis and cholecystitis Acute – adults of middle age and older, usually >40yo Women>men Gallstones – 3 types: Cholesterol, Pigmented, Mixed No stones – acalculous – more severe morbidity – common cause biliary dyskinesia S/S Cholelithiasis: Most asymptomatic, classic biliary colic – intermittent or steady RUQ pain with radiation to rt posterior shoulder within 1 hour of eating. Lasts 1-6 hours Cholecystitis – same but lasts 4-6 hours. Charcot triad: RUQ pain, fever, jaundice if stone lodged in CBD Acute acalculous cholecystitis are critically ill c/u n/v/fever/anorexia, positive Murphy sign Diagnostics CBC with diff Pregnancy test for women LFT Urinalysis Serum pancreatic enzymes U/S CT HIDA scan MRI ECG is cardiac risk factors present or involvement suspected Treatment IVF Antiinflammatory prostaglandin inhibitor (ketorolac) Lap chole Stones lodged in the ampulla of Vater cause pancreatitis Porcelain gallbladder – cancer Cirrhosis End-stage of progressive hepatic fibrosis – result of persistent exposure to toxins. ETOH, Hep c, non-alcoholic fatty liver and nonalcoholic steatohepatitis. Acetaminophen, amiodarone, methotrexate, isoniazid, various antibiotics, carbon tetrachloride. Scarring results in shunting of portal and atrial blood supply causing portal hypertension, HCC, failure. Micronodular – ETOH – nodules are fatty Macronodular – hepatitis and HCC – nodules are vascular Mixed-form MELD – model for end stage liver disease – tool for prognosis and prioritizing for transplant Portal hypertension – increased hydrostatic pressure – develops collateral circulation occurring mostly in peritoneum, retroperitoneum, and thoracic cavities. Complications include ascites, spenomegaly, and esophageal varices – susceptible to rupture, hemorrhage, and death. S/S -Early reports of pruritus, weight loss and fatigue progressing to dark urine, pale stools, anorexia, n/v. Hematemesis, abdominal pain, ascites, chest pain (cardiomegaly), confusion, jaundice. Other: Gynecomastia, palmar erythema, digital clubbing, asterixis. RUQ pain, peripheral edema, delirium, lethargy, coma. White band on nail beds (Muehrcke nails), whitening of proximal 2/3 nail, red of the rest (Terry nails), testicular atrophy, sweet breath odor (fetor hepaticus). Cruveilhier-Baumgarten murmur in portal hypertension (venous hum heard over epigastrium)-augmented by Valsalva maneuver. Diagnostics Early stages: nothing significant LFT, albumin levels, PT/PTT, platelets Lok index uses blood chemistries to calculate cirrhosis in Hep c pts – uses AST, ALT, INR, platelets Ultrasound MRI Doppler Biopsy EGD Treatment Diet - <2gNa+, protein 1.2-1.5g/kg/day Fluid restrictions PHARM: If Na+ ↑, spironolactone 100mg/day – recheck 1 week, if still ↑, increase 100mg q4-5d to max 400mg/day. Monitor for hyperkalemia. No more than0.5kg/d should be lost. Consider adding furosemide If ascites and peripheral edema max 1kg loss Decrease diuretics by 50% if s/s hypovolemia BB (propranolol) to prevent GI bleed LABS: monitor weight, electrolytes, BUN/Cr q week or more Immunize for pneumonia and flu, hep A & B unless already immune Constipation Rome III criteria (2 or more of the following for at least 3 months, onset 6 months prior to diagnosis: < 3 BM/week hard or lumpy stools Straining Incomplete evacuation Anorectal obstructions manual maneuvers to defecate 25% No soft stools without meds No IBS S/S - Subjective and varies Watch for alarm symptoms: sudden change in bowel habits, weight loss >10lbs, blood in stool, anemia, family hx colon ca or IBS, constipation resistant to tx, >50yo. Ortho or tachy – dehydration Weight loss – anorexia or carcinoma Look for abdominal scarring – surgery? Absent bowel sounds – ileus or obstruction? Rebound tenderness – peritoneal inflammation Gyn-retrocele Digital rectal Assess perineal descent – pt bears down while lying in left lateral – normal is 1-4cm Diagnostics CBC with diff, TSH, U/A Stool for occult blood Chem Abdominal x-rays or CT U/S Barium enema If alarms symptoms – colonoscopy Diarrhea 3+ stools/day, loose or liquid. Acute < 2weeks. Persistent 2-4 weeks may be protozoal or other endemic infection. Common in children. Chronic 1+ month. Diarrhea + fever, abdominal pain, dehydration or blood stool – immediate medical evaluation Secretory – most common – imbalance in fluid/electrolytes that cannot be adequately reabsorbed after high solute or high anion load. Caused by proximal hypersecretion of the gut – isotonic or hypertonic fluid in colon. Example: medications, endocrine d/o and cancer Osmotic – from laxatives Steatorrhea – malabsorption – IBS, colitis (Cdiff), celiac, AIDS – foul smelling. Maldigestion – cirrhosis, bile duct obstruction, pancreatitis, cystic fibrosis. Motility - post surgical – Whipple, Billroth II, gastric bypass, ileocolonic resection, ileocecal valve removal or compromise IBS – altered central nervous system pathways – visceral hypersitivity. Clinical presentation Pt keep a log. Chronic vs acute, pain, consistency, treatment for relief of symptoms, etc. Metformin – common side effect Consider: allergic reaction, environmental exposure, food reactions. Xylitol, sorbitol or mannitol are poorly absorbed. Vitamin deficiency – pellagra. Addison disease, Behcet disease, cystic fibrosis, celiac, DM, HIV, thyroid, pancreas, Zollinger-Ellison syndrome (pancreatic neuroendocrine tumor). Physical exam Temp and orthostatic vitals for dehydration, skin pallor, rash, hair thinning, etc. Diagnostics Acute Infectious: stool for ova/parasites, C&S No infection: abdominal x-ray (KUB) to r/o SBO or impaction CBC with diff Chronic CBC with diff LFT HgbA1C TSH IgGand IgA Urine IBD – stool sent for Wright stain 24 hour stool pH KUB, CT, Barium study Sigmoidoscopy, colonoscopy with biopsy EGD with small bowel follow through MRI CT-PET Treatment Fluid and electrolyte replacement – hyperosmolar with glucose and electrolytes Phenergan or Compazine (anticholinergic effects) or Zofran Kaopectate, Pepto-Bismol Donnatal – watch for aspirin intoxication – caution with warfarin Opiates for chronic, intractable diarrhea. IBS-D in women – Lotronex and FODMAP diet Celiac – gluten free (church wafers unexpected culprit) Empiric Antibiotics Rifaximin 400mg TIDx1w Metronidazole 250mg TIDx1w Cipro 500mg BIDx1w Cdiff Metronidazole 500mg TIDx10-14d Or Rifaximin 200-400mg BID or TID Fecal transplant Bile salt malabsorption Welchol 1875mg BID – not FDA approved for this indication yet Questran 4g one to two xday Diverticular disease Diverticulosis (multiple) – outpouching of mucosa through the colon wall, usually sigmoid. Disease acquired of 20th century western civilization from milling of crude cereal grain and wheat flour – loss of nonabsorbable fiber. Increased risk with red or processed meats, obesity and smoking. Mostly asymptomatic but 25% will have acute symptoms. 15% develop fistulas, abscesses, and perforations. c/o irregular defecation, intermittent abdominal pain, bloating, or excessive flatulence. LLQ pain, ribbon like stool or hard pellets – alternating. Younger pts c/o right sided pain easily mistaken for appendicitis. Diagnostics CBC with diff, ESR, urine, stool Barium enema, KUB, CT Colonscopy Treatment Increase fiber, low in saturated fats – avoid red meat Diverticulitis complication of diverticulosis – inflammatory change with diverticula – always symptomatic. Perforation most significant cause of morbidity and mortality. A large perforation may result in a walled-off pericolic abscess that may produce fistulas. Free perforation – peritonitis. S/S – mild to moderate, colicky to steady abdominal pain in LLQ with fever and leukocytosis. May have recurrent UTI or feculent vaginal discharge from fistulization. Tenderness in LLQ, hyperactive bowel sounds if obstruction present. Generalized abdominal pain and abdominal wall rigidity has a perforated viscus. Diagnostics CBC with diff, ESR, urine, stool CT scan U/S Angiography (if bleeding) Water soluable contrast enema Colonscopy Flex sigmoid Treatment Clears for 2-3 days, bedrest Bactrim DS 160/800mg BID and Metronidazole 500mg TID Augmentin or Cipro BID plus Metronidazole 500mg TID for 7-14 days Diverticular Bleeding – cause of massive lower GI bleeds. Rupture of one of the branches of vasa recta adjacent to a diverticulum - most common – right colon especially in older adults. Bleeding usually stops spontaneously. May have 1-3 BMs large volume of blood. May never have been diagnosed before with diverticular disease. Diagnostics CDC with diff and manual platelet count Stool, coag studies including LFT Angiography Bleeding scan EGD, colonoscopy Treatment Life threatening but most resolve spontaneously Hemodynamic stabilization and resuscitation Vasopressin Angiographic embolization, surgical resection Dysphagia Aspiration 1 year mortality rate of 45% Chewing involves CN V (trigeminal), VII (facial), IX (glossopharyngeal) and XII (hypoglassal) S/S – weight loss, malnutrition, dehydration, coughing or choking with eating, or PNA. Assess with Quality of Life in Swallowing Disorders (SWAL-QOL) Short duration with weight loss – malignancy Abrupt onset – CVA Gradual progressive – PD, ALS, scarcoidosis, myasthenia gravis, AD or other chronic diseases. Testing MBS CT or MRI Education Small bolus size, consistency, time, positioning Gastrointestinal Hemorrhage Melena, hematochezia, hematemesis. Overt – visible bright red or maroon blood in feces or emesis Occult - nonvisible Obscure – iron deficient anemia or positive fecal occult R/T ulceration, inflammation, erosion, or neoplasm. UGIB – proximal to the ligament of Treitz - variceal or non variceal (PUD, erosions/ulcers) LGIB – distal to the ligament of Treitz – diverticulosis or cancer, ulcers, fistula/fissures, postpolypectomy Contributing factors: smoking, NSAIDs, excess stomach acid production, H. pylori. AVM (angiodysplasias) S/S – Hematemesis, hematochezia. Hypotension does not occur until volume is 40% depleted Orthostatis with 15-20% volume loss. Systolic ↓ 20, diastolic ↓ 10 or heart rate ↑ by >20 Look for cutaneous lesions on BUE, lips and oral mucosa – hereditary hemorrhagic telangiectasia or blue rubber bleb nevus syndrome. Spider nevi, palmar erythema and scleral icterus – cirrhosis. Diagnostics H&H, platelets Type and cross Coags, LFT ABG ECG Abdominal series if suspected perforated viscus or obstruction Management Stabilize, stop bleeding, prevent recurrence. PRBC to keep hgb >7g/dl, FFP for coagulopathy, platelets if <50K Reverse anticoagulants, if possible Start PPI if UGIB Octreotide Hepatitis Viral: HAV, HBV, HCV, HDV, HEV Acute: range from asymptomatic to death (rare) Chronic: at least 6 months: minimal inflammation – cirrhosis – failure – need for transplant HAV – Fecal-oral route, person-to-person, ingestion of contaminated food or water and blood. Virus can survive for months in fresh and salt water (seafood.) Incubation 2-6 weeks with viral load peaking at 2 weeks. Cleared by CD4 T cells. Found in liver cells, bile, stool, and blood. Boil for 1 minute. Infectious 2 weeks before symptoms and 1 week after – no longer contagious by the time they are jaundiced – except neonates – infectious for up to 6 months after jaundice. Self limiting acute disease – not chronic HAB – DNA virus - endemic worldwide – especially Asia. Viral load peaks at 7-8 weeks after exposure. Increased lifetime risk of cirrhosis and HCC. Vaccination causing decline. Found in blood tears, CSF, breast milk, saliva, vaginal secretions and semen. Transmitted parenterally, sex (most common), and perinatally. Cleared by CD4 and CD8 T cells. Infectious 4-6 weeks before symptoms and thereafter. HCV –RNA virus - transmitted by flood (before July 1992), clotting factor components (before 1987), HD, IV drus, Intranasal drugs, tattoos, mani/pedi, body piercings. Incubation 2-22wks and evades the adaptive and innate components of immune system. Rapid turnover and elicits a strong type I IFN response. Infectious 4-6 weeks before symptoms and thereafter. HDV – RNA virus - requires coinfection with HBV for replication – most severe form. Transmitted parenterally (IVDA). Infectious 4-6 weeks before symptoms and thereafter. HEV – RNA virus – incubation 15-60 days – same route as HAV. Causes mortality in pregnancy (15-20%) andin pts with cirrhosis. Infectious 2 weeks before symptoms and 1 week after Alcoholic Hepatitis – excessive ETOH consumption >10 years affecting 10-35% of drinkers Nonalcoholic fatty liver disease (NAFLD) NAFLD and nonalcoholic steatohepatitis (NASH) associated with metabolic syndrome – most common in US – steadily increasing and correlated with increases in obesity. NASH is 3rd most common cause of cirrhosis and expect to be most common need for transplant by 2020. Drug-Induced liver injury (DILI) Rare reaction with meds (NSAIDs and antimicrobials) causing drug hepatoxicity. 1. Allergic reaction within 6 weeks (Dilantin) 2. Metabolic reaction within 1 year (isoniazid) Top offending drug were Amoxicillin-clavulanic acid, isoniazid, nitrofurantoin, sulfamethoxazole-trimethoprim, and minocycline. Autoimmune Hepatitis Rare – seen in 50-60yo - women 3x more likely. Treat with corticosteroids. May need transplant. S/S – acute presents similar to any mild viral illness. Jaundice with HBV Diagnostics LFT, hepatitis panel CBC with diff, platelets Coags, lipids, TSH Liver biopsy Abdominal U/S or CT Treatment HAV, HBV – supportive care Chronic HBV -Pegylated IFN, Entecavir, lamivudine, or tenofovir Chronic HCV – Pegylated IFN, imeprevir, ribavirin. Genotype I-ledipasvir-sofosbuvir Genotype 2&3-Sofosbuvir with ribavirin Immunize with immune globulin for HAV – lasts 6 months. Immunizations available for HAV, HBV Inflammatory Bowel Disease Crohn’s: from mouth to anus Mucosal involvement: patchy, cobblestone appearance if colon involved Inflammation is transmural Corticosteroids for moderate to severe disease Minimal effect with mesalamine Strictures, arthritis, lesions 75% need surgery Smoking increases risk, especially for women Familial Lifelong treatment U. Colitis Colon – partial or entire length Mucosal involvement: continuous, beginning at rectum Inflammation is mucosal and submucosal layers only Corticosteroids in only 15% of severe disease Excellent response to mesalamine Arthritis, skin lesions, eye spine, mouth, liver, perianal disease 10-20% total colectomy – curative Smoking may be protective – risk for disease after quitting Low familial connection 80% relapse without treatment S/S – abdominal pain or diarrhea intermittently for years. C/O rectal spasms, urgency, and fecal incontinence with active rectal inflammation. Fatigue, weight loss, anorexia, fever, chills, n/v, joint pains, and mouth sores. Tender lower abdomen, hyperactive bowel sounds, mass in LRQ can signify ileocecal inflammation. Diagnostics CBC with diff platelet CRP ESR CMP, LFT Celiac antibody panel Stool MRI, CT Small bowel series EGD/colonoscopy Flex sigmoid Barium enema Treatment PHARM: 5-Aminosalicylic Acid (mesalamine) – first in line for UC Corticosteroids Immuomodulators Biologics (Infliximab, Adalimumab = anti-TNF for CD) – significant risk for life-threatening infections, lymphoma, activation of TB and malignancy. Antibiotics – metronidazole Surgery Complications Increased risk of colorectal cancer, peripheral arthritis, legions, stomatitis, liver disease, gallstones, malabsorption, adrenal stones and osteoporosis. Irritable Bowel Syndrome Most common GI complaint – no identifiable organic or structural cause. Rome III Diagnosis: criteria at least 1x/week for at least 2 months before diagnosis 1. Abdominal discomfort or pain at least 3 days/month in the last 3 months with 2 or more: Improvement with defecation Onset w/change in frequency of stool Onset w/change in appearance of stool 2. No evidence of inflammatory, anatomic, metabolic, or neoplastic process that can explain symptoms IBS pts process sensory information from the gut differently. Altered motility Enhanced visceral sensation Have higher incidence of psychosocial stressors and abuse Comorbidity – GERD, psychiatric disorders, lactose intolerance Diagnostics CDC with diff ESR Electrolytes TSH Stool LFT IgA Hydrogen breath test (lactose intolerance) KUB Barium enema U/S Flex Sigmoid, colonscopy Treatment Dietary modifications PHARM: Antispasmodics Antidiarrheal Anticonstipation Psychotropics Alternative – cognitive behavior, hypnosis, guided imagery, relaxation, stress management, Acupunture. Peppermint oil is a natural spasmodic – similar to CCB Refer to hospital for nocturnal symptoms, bloody stools, fever and weight loss. Jaundice Prehepatic – excessive bilirubin production (hemolysis ie sickle cell, blood transufion reaction). Increase in unconjugated bilirubin. Hepatic – hepatic injury from infection, toxins, autoimmune, and tumors. Increase in conjugated bilirubin. Posthepatic – obstructive – obstruction of bile ducts (pancreatic tumors and gallstones). Increase in conjugated bilirubin. S/S - Pruritus, cutaneous xanthomas, colicky RUQ pain, weight loss. Determine chronic vs acute. Chronic suggests hepatitis, biliary tract disease, pancreatitis, or chronic alcohol intake. Look for gynecomastia, testicular atrophy and spenlomegaly – strongly associated with cirrhosis from ETOH. Lymphadenopathy suggests malignancy r/t pancreatic tumor obstruction. Diagnostics LFTs, CBC with diff, platelets Coags Hepatitis profile Electrolytes Iron panel HIV U/S, CT ERCP, MRI, liver biopsy Nausea and vomiting Emergency referral if accompanied by pain, severe dehydration, acute abdomen, fever, neurological changes, or a metabolic imbalance Two CNS centers: Vomiting center (VC in medulla) and chemoreceptor trigger zone (CTZ floor of 4th ventricle). VC-stimulated by input (noxious substances) from various systems that mechanically irritate the pharyngeal afferents, leading to retching then vomiting. CTZ – sensitize to chemical agents with known emetogenic potential. Sensitive to changes in serotonin, dopamine, histamine, cholinergic, adrenergic, and opiate receptors. Pre-ejection – increase in salivation and swallowing, decrease in gastric tone, tachycardia, pallor and diaphoresis. Relaxation of the proximal stomach and contraction of the small intestine leads to regurgitation. Mediated by acetylcholine and vagus nerve. Ejection – abdominal muscles and diaphragm contract, lower esophageal sphincter relaxes, palate is elevated and contents is expelled. Post ejection – after expulsion, relieving nausea Get history! Early morning = metabolic disturbance, EYOH bingeing, and pregnancy Triggered by meals = pyloric channel ulcer, gastritis or psychogenic Appearance – coffee ground, feculent (SBO) Recent travel Last menstrual period – sexually active Force of vomiting Assess for dehydration, check fingers for calluses suggesting self-induced vomiting (and lanugo hair and loss of tooth enamel), abdomen for distention, visible peristalsis, hernias, scars, bowel sounds. Diagnostics UA for specific gravity Electrolytes Glucose Renal function Pancreatic enzymes LFTs Tox screen Pregnancy test Abdominal x-ray U/S Management Recognize and correct complication ID underlying cause – rule out intestinal obstruction or acute abdomen Increase fluids, diet restrictions (clears, BRAT, then bland) Antiemetics (Zofran has prolonged QT) Acute Pancreatitis Most common cause is gallstones followed by toxins (ETOH). ERCP causes 5%. Presents with sudden onset of constant, sharp, poorly localized abdominal pain that radiates to the back. Pain is so intense, leads to atelectasis – crackles may be present. Abdominal distension. Direct and rebound tenderness secondary to peritonitis are late signs associated with severe acute pancreatitis which is associated with a grave prognosis. Look for Cullen sign (bruising of the periumbilicus) or Grey Turner sign (bruising of the flank) consistent with hemorrhagic findings. Both are rare and increased mortality. Jaundice may be present although uncommon. Diagnostics Amylase and lipase Fasting lipids, chem 12 (electrolytes, BUN/CR, hepatic function panel) TSH KUB Abdominal U/S MRI with or without MRCP CT HIDA Treatment IVF, NPO Pain control (avoid Morphine – increase in pressure of the sphincter of Oddi) Chronic Pancreatitis [Show More]
Last updated: 2 years ago
Preview 1 out of 18 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$6.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Feb 02, 2020
Number of pages
18
Written in
Additional information
This document has been written for:
Uploaded
Feb 02, 2020
Downloads
0
Views
111