PN3 FINAL STUDY GUIDE; FOR PN 161 PRACTICAL NURSING III FINAL EXAM
Module 1 and 2
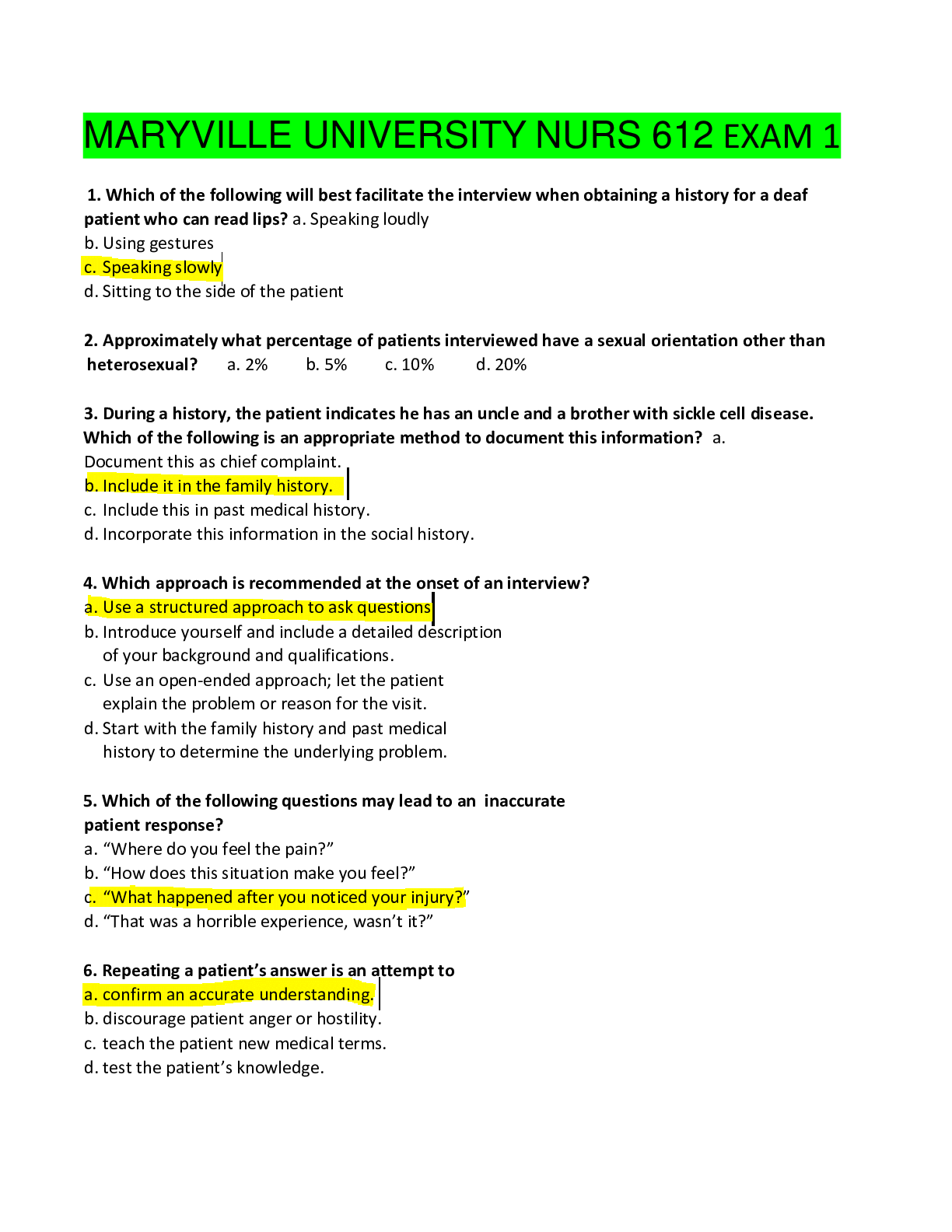
1. Identify how to properly assess a client using the Glasgow coma scale and important nursing interventions related to scoring.
a. T
...
PN3 FINAL STUDY GUIDE; FOR PN 161 PRACTICAL NURSING III FINAL EXAM
Module 1 and 2
1. Identify how to properly assess a client using the Glasgow coma scale and important nursing interventions related to scoring.
a. The Glasgow coma scale measures eye opening, verbal response, and motor response
i. Monitor for improvements or worsening signs
b. See level of consciousness!
c. 3 is the lowest score
d. Highest score 15
e. A score of 7 or less is considered a state of coma
2. Understand important considerations for neurological assessments.
a. Health history
i. Headaches
ii. Clumsiness
iii. Loss or change in function of extremity
iv. Seizure activity
v. Numbness or tingling
vi. Change in vision
vii. Pain
viii. Extreme fatigue
ix. Personality changes or mood swings
3. Review the physiology of CNS, PNS, and sympathetic/parasympathetic nervous systems.
a. CNS
i. Brain
1. Controls, initiates, and integrates body functions
ii. Spinal cord
1. Carries sensory impulses
a. Cerebrospinal fluid
i. Absorbs shock
b. PNS
i. Somatic nervous system
1. Conscious activities
ii. Autonomic nervous system
1. Unconsciousness activity
iii. Spinal nerves
1. Reflex activity
c. Sympathetic
i. Neurological
1. Pupils dilated
2. Heightened awareness
3. Fight or flight
d. Parasympathetic
i. Neurological
1. Pupils normal size
2. Rest and digest
4. Identify important observations to include when assessing a pt.’s. mental status.
a. Appearance
b. Behavior
c. Posture
d. Mood
e. Gestures
f. Movements and facial expressions
5. Safety factors in Parkinson’s patients.
a. Ambulation with assistance
b. Provide an elevated toilet seat
6. S/S of encephalitis, meningitis and review nursing actions when caring for patients with them.
a. Encephalitis
i. Inflammation of brain
ii. Fever, headache, nuchal rigidity, photophobia, irritability, lethargy, nausea/vomiting
b. Meningitis
i. Inflammation of meninges
ii. Fever, headache, nuchal rigidity, photophobia, irritability, lethargy, and nausea/vomiting
c. Nursing care
i. Monitor for changes in neurological status
ii. Quiet environment decreases external stimulation
iii. Observe for seizure activity and protect from injury
iv. Comfort measures offered
7. Post-op care of patient following back surgery.
a. Monitor neurological status and vital signs
b. Encourage client to cough, deep breathe, use incentive spirometer hourly, and move legs as allowed
c. Provide adequate fluids to prevent renal stasis and constipation
8. List the S/S of herniated disks.
a. Pain
b. Motor changes
c. Sensory changes
d. Alterations in reflexes
9. S/S and exacerbations of them in MS patients.
a. S/S of MS
i. Vary according to the areas of demyelination
ii. Vary from hour to hour or day to day
iii. May be sensory, motor, or other disturbances
1. Visual disturbances
2. Numbness
3. Paresthesia
4. Pain
5. Decreased sense of temperature
6. Decreased muscle strength
7. Spasticity
8. Paralysis
9. Bowel and bladder incontinence or retention
b. Exacerbations
i. Periods of exacerbation and remission also make diagnosis difficult
ii. Are frequently precipitated by periods of emotional or physical stress
1. Infections
2. Pregnancy
3. Trauma
4. Fatigue
10. Review the care of a client with seizures.
a. If client is in bed:
i. Be sure the side rails are up
ii. Put padding (blankets) on the side rails to prevent injury
b. If client is out of bed:
i. Carefully ease the client to the floor
ii. Move nearby objects so the client will not be injured
iii. Place a soft item beneath the client’s head
c. Never leave the client alone
d. Don NOT restrain the client
e. Do not attempt to put anything in the client’s mouth
f. Loosen any restrictive clothing around the client’s neck
g. Turn the client’s head to the side
h. Monitor seizure activity carefully, noting exact time that the seizure began and ended
i. After the seizure
i. Call the client by name and ask her to perform a simple command
ii. Test the client’s memory by asking her to remember two words
iii. Ask the client whether an aura was experienced before the seizure
iv. Check the oral cavity—especially the tongue—for injury
v. Offer comfort and reassurance, because the client may be frightened and embarrassed
vi. Document the length of the seizure and everything observed
vii. Keep the client in a side-lying position if the client remains lethargic
j. Monitor for toxic signs of anticonvulsant medications
k. Importance for compliance with prescribed medication schedule
l. Encourage client to have anticonvulsant medication blood level checked regularly
11. Review various treatments for headaches.
a. Surgical
i. Repair of an aneurysm or resection of a brain tumor
b. Pharmacological
i. Aleve, Advil, imitrex, maxalt, aomig, amerge, axert,
c. Diet
i. Triggering foods
1. Alcohol, cured meats containing nitrates, aged cheeses, monosodium glutamate (MSG), citrus fruits, chocolate, red wines
d. Activity
i. Stressful situations
1. Biofeedback, relaxation techniques, stress reduction, development of coping mechanisms
12. Review the different spinal cord injuries and the focus of medical management.
a. Complete
i. No impulses are carried below the level of injury
b. Incomplete
i. Some of the spinal cords tracts are affected while others are able to carry impulses normally
c. Hyperflexion
i. Extreme forward movement of head
ii. Causes compression of the vertebral bodies and damage to the posterior ligaments and intervertebral disks
d. Hyperextension
i. Extreme backward movement of head
ii. Injury to the posterior vertebral structures and the anterior ligaments
e. Axial loading
i. Extreme pressure is placed on the spinal column
1. Driving accidents or falls landed on feet or buttocks
f. Excessive rotation injury
i. Turning the head beyond the normal range
13. Identify s/s of autonomic dysreflexia and appropriate nursing actions.
a. S/S of autonomic dysreflexia
i. Increased blood pressure
ii. Sudden throbbing headache
iii. Chills
iv. Pallor
v. Goose flesh
vi. Nausea
vii. Metallic taste
b. Appropriate nursing action
i. Teach client of s/s
ii. Implement a bowel and bladder training program
iii. Observe vital signs (monitor BP)
iv. Raise head of bed and lower legs to reduce BP
v. Assess client for a distended bladder and empty bladder
vi. Check for fecal impaction
14. Identify healthcare team members that may be involved in a CVA patient.
a. Nurses
b. Physical occupational and speech therapists
15. List appropriate goals when caring for AD and ALS patients.
a. Ambulation and other activities are encouraged as long as possible
b. Physical occupational and speech therapists
c. Encourage independence as long as possible
d. Assist with personal hygiene and getting in and out of bed
e. Maintain highest possible functional level
16. Review the early s/s of increased intracranial pressure.
a. Deterioration in level of consciousness
b. Confusion
c. Difficulty rousing
d. Initially restlessness
17. Review important points to educate patients on in an effort to prevent strokes.
a. Have an annual blood pressure check
b. Be aware of cholesterol level
c. Consume lesser amounts of sodium and fat
d. Exercise daily
e. Do not smoke
f. If you drink alcohol do so in moderation
g. Check with a doctor for symptoms of atrial fibrillation
h. Check cholesterol level
i. Control diabetes
j. Check with a doctor for circulation problems
k. See a doctor immediately with any stroke-like symptoms
18. Identify important safety considerations to teach patients with cataracts.
a. Assist with ambulation
b. Maintain eye patch
c. Teach client or family to administer eye drops and ointments
d. Encourage client to keep all follow-up appointments
19. Identify risk factors for glaucoma.
a. Administer eye drops and ointments
b. Keep all follow-up appointments
c. Administer medications as ordered
d. Stress client compliance with prescribed medication therapy
e. Encourage glaucoma screening for all persons older than 35
20. Review important factors to educate a patient requiring hearing aids.
a. May need to experiment with several different types of hearing aids
b. May need speech therapy, lip reading, and auditory training may be necessary to help discriminate speech and develop better listening skills
c. Convert environmental sound and speech into electronic signals that are amplified and converted to acoustic signals
d. Makes speech and sound louder but not going to make it more clear
21. Review cranial nerve function.
a. Olfactory (I)
i. Sensory
1. Smell
b. Optic (II)
i. Sensory
1. Vision
c. Oculomotor (III)
i. Motor
1. Pupil constriction
d. Trochlear (IV)
i. Motor
1. Upper eyelid elevation, extraocular eye movement
e. Trigeminal (V)
i. Sensory
1. Cornea, nose, and oral mucosa
ii. Motor
1. Mastication
f. Abducens (VI)
i. Motor
1. Extraocular eye movement
g. Facial (VII)
i. Motor
1. Facial muscles
ii. Sensory
1. Taste (anterior 2/3 of tongue)
h. Acoustic (VIII)
i. Sensory:
1. Hearing equilibrium
i. Glossopharyngeal (IX)
i. Sensory
1. Sensation to throat and taste (posterior 1/3 of tongue)
ii. Motor
1. Swallowing
j. Vagus (X)
i. Motor and sensory
k. Spinal accessory (XI)
i. Motor
1. Sternocleidomastoid muscle, trapezius muscle
l. Hypoglossal (XII)
i. Motor
1. Tongue movement
22. Identify appropriate goals for caring for a client with a brain tumor.
a. Monitor for increase of intracranial pressure
b. Destroy the tumor cells
23. List nursing interventions RT unilateral neglect.
a. Failure to recognize or care for the affected side of the body
b. Interventions
i. Adapt environment to prevent injury
1. Positioning water and personal items to the unaffected side
ii. Approach the client from the unaffected side
iii. Gradually cue client to remind to tend to the neglected side
iv. Remind client of safety factors
v. Teach client and family to place small bites of food on unaffected side and to check for food in the cheek on the affected side after meals
vi. Scan environment for safety factors at all times
24. Define homonymous hemianopia.
a. The loss of vision in half of the visual field on the same side of both eyes
25. Identify appropriate positions for clients with a head injury.
a. Head elevated slightly and neck kept straight
Module 3
26. Review important nursing considerations to remember when caring for clients who are receiving chemotherapy.
a. Blood counts are monitored
b. White-cell count
c. Platelet count
Module 4
27. Review the treatment of a client with a DVT and appropriate lab tests to monitor.
a. Put patient on bedrest
b. Periodically elevate extremity to promote venous return
c. Started on a blood thinner
i. Lovenox, heparin
d. Partial thromboplastin time (PTT), activated partial thromboplastin time (APTT)
i. Effective heparin treatment the APTT or PTT should be 2.5 times the baseline
e. Platelet count performed
f. If started on Coumadin
i. International Normalized Ratio (INR)
1. Performed daily until effective dose has been obtained
ii. Always started before heparin is discontinued
g. Adequate hydration for people at risk for thrombi
h. Prevention is the best way to treat DVT
i. Hydration, ambulation, compression socks
i. Heparin therapy and PTT and aPTT should be 2.5 times more above base line
j. Put on bed rest to prevent embolism from traveling
28. Review the cause and treatment of dysrhythmias.
a. Bradycardia—cause: myocardial ischemia, electrolyte imbalances, vagal stimulation, beta blockers, heart block, drug toxicity, intracranial tumors, sleep, and vomiting
i. Treatment: administration of atropine some clients may require a permanent pacemaker
b. Tachycardia—cause: exercise, emotional stress, fever, medications, pain, anemia, thyrotoxicosis, pericarditis, heart failure, excessive caffeine intake and tobacco use
i. Treatment: depends on the cause
c. Atrial flutter—causes: myocardial infarction, heart failure, electrolyte imbalances, emotional stress, and drugs
i. Treatment—(intervention is needed immediately) medications, electric shock, or procedures that destroy abnormal tissue in the heart may be used to restore a normal heart beat control heart rate or prevent blood clots
d. Atrial fibrillation—causes: coronary artery disease, heart failure, and hypertension
i. Secondary causes: thyrotoxicosis, caffeine intake, alcohol intoxication, stress, electrolyte imbalances, and cardiac surgery (once the underlying condition is treated AF may stop)
1. Treatment: digoxin, beta-adrenergic blockers, and calcium channel blockers, electric shock (electrical cardioversion) (patient with be sedated) performed if medications do not stop the atrial fibrillation
e. Ventricular fibrillation—causes: coronary artery disease (most common) will not have a pulse, blood pressure, or respirations
i. Treatment: CPR and defibrillate the client immediately
f. Cause: electrolyte imbalance, heart failure, coronary artery disease, myocardial infarction, drug toxicity
g. Bradycardia: administer atropine
h. Ventricular fib: CPR and immediate defibrillation (best treatment)
i. Tachycardia: depends on cause
29. Explain the correlation of atrial fibrillation to a CVA.
a. Individual with atrial fibrillation are 5 times more likely to have a CVA
i. Due to blood pooling in the atria, predisposing the person to thrombi forming and dislodging and traveling to the brain
30. Understand the nursing care of a client with a pacemaker.
a. Avoid contact sports
b. Monitor vital signs including apical pulse
c. Provide rest periods throughout the day
d. Encourage client to verbalize concerns about condition and potential complications
e. Teach relaxation methods
f. identification tag
31. List important points to teach a client with thrombophlebitis.
a. Drink 2-3 quarts of water per day
b. So not sit with legs crossed
c. Elevate both legs when sitting
d. Avoid sitting or standing for extended periods
e. Wear support hose
f. When standing, shift weight frequently and occasionally stand on tiptoes to stimulate the calf muscle to pump blood
g. Notify the physician immediately if leg pain, tenderness or swelling, difficulty breathing, or chest pain is experienced
32. Explain potential complications of rheumatic fever.
a. Rheumatic heart disease
b. Mitral valve prolapse
c. Endocardium, myocardium, and epicardium can become inflamed, with most of the damage occurring to the mitral valve
33. Review the treatments for endocarditis and pericarditis.
a. Endocarditis
i. Surgical
1. Repair or placement of a valve
ii. Pharmacological
1. Antimicrobial drugs
2. IV antibiotics
a. 2-6 weeks
iii. Diet
1. Well-balanced nutritious diet with between-meal snacks
2. Adequate intake of protein, zinc, iron, phosphate and Vitamins A, B, C, D & E
iv. Activity
1. Bedrest
2. Calm quiet enviornment
b. Pericarditis
i. Medical
1. Pericardiocentesis
a. Aspirate the excess fluid from the pericardial sac
ii. Surgical
1. Pericardiectomy
a. Removal of the pericardium
iii. Pharmacological
1. Antipyretics, analgesics, and anti-inflammatory agents
2. Antibiotics
34. Review the procedure for cardioversion.
a. The delivery of a synchronized electrical shock to change dysrhythmia to a rhythm that circulates more blood to the body tissues and improves oxygenation of the tissues
b. Client is NPO 8 hours before cardioversion
c. Client is sedated for the procedure and does not feel the electrical shock
35. Review the electrical conduction of the heart.
a. SA node initiates electrical impulses that cause the heart to beat
b. Pass through the muscle fibers of the right and left atria
c. Atrial impulses are transmitted to the AV node located at lower part of the right atrium
d. AV node allows the atria to complete their contraction and empty the blood into the ventricles
e. Impulse then travels to the AV bundles (bundle of His)
f. Branch out to Purkinji fibers
i. Terminate in the ventricular muscle, causing the ventricles to contract
36. Define regurgitation.
a. When the valve does not close completely, blood leaks back into the chamber from which it was pumped
Module 5
37. Identify latex allergy precautions.
a. Avoidance of latex products is of utmost importance
b. Synthetic versions of products are often available
38. Review the care of a hemophilia client with bleeding in the joints.
a. Assess for signs of bleeding
i. Petechiae, Ecchymoses, Hematemesis, Epistaxis, Hematuria, Hemarthrosis, Abdominal rigidity
b. Note edematous or immobile joints
c. Encourage client to wear MedicAlert bracelet and avoid activites that cause trauma
d. Advise not to take aspirin, and to use an electric razor and a soft toothbrush
e. Apply ice and pressure to bleeding site
39. Define DIC and its treatment.
a. Syndrome that occurs because of a primary disease process or condition
b. Condition of alternating clotting and hemorrhaging
c. Treatment
i. Administer whole blood or blood products to normalize the clotting factor level
ii. Platelets and packed red cells are given to replace those lost during hemorrhage
iii. Cryoprecipitate or fresh-frozen plasma is given to normalize clotting factor levels
iv. Heparin has no effect on the thrombi that are already formed but is given to prevent the formation of more microthrombi
1. Controversial because of risk of hemorrhage
2. After thrombi formation is controlled with heparin
a. Aminocaproic acid (Amicar) is given to stop the bleeding because it stops the fibrinolytic process
40. Recognize the treatment and complications of a client in anaphylactic shock.
a. Treatment
i. Administer epinephrine
ii. Clients will be NPO until normal respiratory and circulatory function have been restored
iii. Remain on bed rest until vital signs are stable and breathing patterns have been restored
iv. Severe anaphylactic responses are generally transferred to ICU
v. Maintain open airway
b. Risks
i. Tachycardia
1. From epinephrine
ii. Respiratory failure
iii. Severe hypotension
iv. Anaphylactic shock
v. Death
1. Treatment initiated immediately because death can occur in minutes
41. Identify the meds that have immunosuppressive properties, along with potential adverse reactions.
a. Prednisone and methylprednisolone sodium succinate decrease inflammatory response
b. Cyclosporine, antihymocyte globulin, ATG and tacrolimus inhibit T cells
c. Azathioprine inhibits purine syntheses
d. Muromonab-CD3 prevents acute rejection in kidney transplant clients
e. Potential adverse reactions: infection
42. Define lupus and list the s/s and treatments of it.
a. Lupus
i. Chronic, progressive, incurable autoimmune disease affecting multiple body organs
ii. Characterized by periods of exacerbation and remission
iii. Most commonly in women during their child bearing years
iv. 2-3 times more common in African American women
v. B-lymphocyte cells produce autoantibodies that destroy body cells
vi. Tissue damage in the skin, brain, kidney, lung, heart or joints
vii. No single test to diagnose lupus
viii. (inflammatory disease of collagen in connective tissue)
b. S/S
i. Malar rash (over cheeks)
ii. Discoid rash
iii. Photosensitivity
iv. Oral ulcers
v. Arthritis
vi. Serositis (pleuritic or pericarditis)
vii. Excessive protein or cellular casts in the urine
viii. Seizures or psychosis
ix. Hemolytic anemia, Leukopenia, lymphopenia, or thrombocytopenia
x. Positive tests for LE cells, anti-DNA antibody, or anti-Sm or a false-positive syphilis test
xi. Four or more of these criteria are present a client is diagnosed with lupus
43. Review the criteria for the dx. Of AIDS
a. ELSIA
i. The basic screening test to detect antibodies to HIV
ii. Positive test result always retested to rule out a false-positive result and/or technician error
b. Western Blot Test
i. Confirmatory test
c. Results of both the ELISA and Western blot taken together have an extremely high accuracy rate
44. Review the procedure for blood transfusions, the LPNs responsibility RT it and s/s of a transfusions reaction as well as nursing interventions RT a transfusion reaction.
a. Before the transfusion, 2 nurses check the compatibility of the blood product with the client’s blood
b. The first 50 mL is given within 5-10 minutes
c. The client is observed closely for a hemolytic blood reaction during this time
d. If symptoms of a reaction, the infusion is stopped immediately and the physician notified
e. Follow institutional protocol
f. Should be completed within 4 hours of the start off administrations
g. No medications are given at the blood administration site during infusion
h. Administered with 0.9% sodium chloride solution with blood
i. LPN responsibilities
i. Follow agency protocol for use and administration of blood products. Assess vital signs before administration of blood products and at 15-min intervals four times during the transfusion. Stay with the client for at least the 1st 15 mins of administration. When reaction occurs, stop transfusion, but keep saline going for IV access if needed. Notify physician immediately. Monitor for any transfusion reactions such as fever, chills, nausea, headache, hypotension, respiratory problems
j. S/S of reaction
i. Febrile nonhemolytic (most common and occur in clients who have had previous blood transfusions as a result of an antibody-antigen reaction to WBCs)
ii. Allergic urticarial, delayed hemolytic, acute hemolytic, anaphylactic, fever, chills, rash, nausea, headache, hypotension, respiratory problems
45. Define urticarial.
a. (hives) are raised pruritic, red, nontender wheals on the skin
46. Identify complications of poor venous circulation.
a. Hypotension
b. Peripheral vascular disease
Module 6:
47. List the s/s of contact dermatitis.
a. Pruritus (itching), burning, and erythema (redness)
b. Maculopapular rash or a combination of papules and vesicles develop
48. Explain the different manifestations of each degree of burns.
a. First degree burns
i. Involve only the epidermis
ii. Skin is hot, red, painful, and may be slightly swollen (sunburn)
iii. Heal in about a week without scarring
b. Second degree burn
i. Damage the dermis and the epidermis
ii. Skin is red, hot, and painful
iii. Blisters form and tissue around the burn is edematous
iv. Skin may appear glossy from leaking fluid (boiling water on the skin)
c. Third degree burns
i. All dermal structures are destroyed and cannot be regenerated
ii. Subcutaneous tissue is also damaged
iii. Full thickness burns can be white, tan, brown, black, charred, or bright red in color
d. Fourth degree burn
i. Extend to the underlying muscles and bones
ii. Appear white to black or charred with dark networks of thrombosed capillaries visible inside the wound
iii. Result from fires, explosions and nuclear radiation
49. Review important components of burn care.
a. Asses a burn wound for color, odor, edema, amount of drainage, and signs of infection
b. Manage pain, high caloric diet
c. Highest priority is ineffective airway clearance, wear gown, gloves, masks, and caps, morphine is drug choice
50. Review the function of the integumentary system
a. Protection, temperature regulation, sensory perception, fluid and electrolyte balance
b. Protection: barrier against microorganisms and other substances that could be harmful
51. List causes of impaired wound healing and the phases of wound healing.
a. Age, oxygenation, smoking, drug therapy, obesity, and diseases such as diabetes, infection nutrition and diet can also affect the healing process
b. Phases of wound healing:
i. Primary intention
1. Wound layers are sutured together and have no gaping edges
2. Heals in 8-10 days but may take up to 3 months
3. Minimal scar formation
ii. Secondary intention
1. Filling with granulation tissue and by contracting where the skin edges are not approximated
2. Slow possibly taking months or years
iii. Tertiary intention
1. Allows an infection to drain or an area of extensive tissue remval to begin
2. Edges of wound are closed 4-6 days later
3. Scar is usually much wider
52. Review dietary interventions RT wound healing.
a. High protein diet
b. increase protein and caloric intake by twice as much
53. List types of exudate
a. Sanguineous
b. Serosanguinous
c. Serous
d. Purulent
54. Identify age related changes that present complications for wound healing
a. Blood flow to the skin is reduced, skin becomes thin, more easily injured, breaks down from prolonged pressure, sagging and wrinkling, dry skin, decreased ability to adapt to changes in environment temp
55. Identify skin assessment parameters
a. Integrity
b. Color
c. Temperature and moisture
d. Texture
e. Turgor and mobility
f. Sensation
g. Vascularity
56. Review lab tests RT nutrition.
a. Albumin
b. Prealbumin
c. Blood glucose, fasting blood sugar (FBS)
d. Carboxyhemoglobin
e. C-reactive protein test (CRP)
f. Electrolytes
i. Sodium (Na+)
ii. Potassium (K+)
iii. Chloride (Cl-)
g. Hemoglobin (Hgb) and hematocrit (Hct)
h. Red blood cells (RBCs)
i. Total protein
j. White blood cells (WBCs)
Module 7:
57. Identify the electrolyte imbalance RT infusion of a large amount of IV fluids.
a. Large amounts of fluid replacement can cause hypokalemia
58. Identify the nursing interventions for a client in shock.
a. Hypovolemic: replace fluids (0.09% normal saline)
59. Identify the early signs of septic shock
a. Mild tachycardia, slight fever, warm and flushed skin
60. List the phases of septic shock
a. Early sepsis
i. Warm, flushed skin
ii. Fever above 100.4
iii. Mild tachycardia
iv. Elevated respiratory rate above 20/min
v. WBC lower than 4,000 or greater than 10,000
b. Severe sepsis
i. Anxious
ii. Mild hypotension
iii. Hypoxia
iv. Higher fever
v. Mental status changes
c. Septic shock
i. Severe tachycardia
ii. Cool clammy extremities
iii. Weak and thread peripheral pulses
iv. Significant hypotension
v. Hypoxia
vi. Respiratory distress
vii. May be unresponsive
viii. Minimal urine output
61. Identify the nursing priority for the prevention of shock
a. Monitor patient for signs and symptoms of shock
b. Take immediate action if client becomes positive for shock
c. Be able to recognize s/s and immediately treat shock
62. Explain the causes and physiologic changes of each type of shock and the s/s of each
a. Hypovolemic s/s: increase HR, increase BP, cool and clammy skin
b. Cardiogenic shock is an early sign of mild tachycardia
63. Identify nursing assessments and interventions for a client in each type of shock
a. Hypovolemic
i. Nursing assessments
1. Subjective data
a. History, symptoms, fears
2. Objective data
a. Physical examination, mild tachycardia and mild hypotension, diminished urinary output, cardiac arrhythmias, evidence of cardiac ischemia
ii. Nursing interventions
1. Provide emotional support
2. Explain the treatment regimen
3. Inform the client about diagnostic testing results
4. Explain all procedures before they are performed
5. Administer IV fluids
6. Administer blood products
7. Monitor urinary output
8. Encourage slow position change
9. Administer oxygen as ordered
10. Administer vasopressors, as ordered
b. Anaphylactic Shock
i. Nursing assessments
1. Subjective data
a. Potential source, onset
2. Objective data
a. Physical examination, vital signs, EKG, pulse oximetry readings, diagnostic test results
ii. Nursing interventions
1. Administer oxygen as ordered
2. Administer epinephrine as ordered via IV, subQ, or endotracheal tube
3. Administer IV fluids as ordered
4. Administer corticosteroids as ordered
5. Educate patient about epi-pen
c. Neurogenic shock
i. Nursing assessment
1. Subjective data
a. Client understanding, physical status, anxiety level
2. Objective data
a. Head-to-toe exam, diagnostic tests, vital signs, EKG data, pulse oximetry
ii. Nursing interventions
1. Monitor client’s temperature
2. Administer antipyretics as ordered
3. Administer vasopressors as ordered
d. Cardiogenic shock
i. Nursing assessment
1. Subjective data
a. History, symptoms
2. Objective data
a. BP, urinary output, skin assessment, peripheral pulses, pulse oximetry
ii. Nursing interventions
1. Organize care to minimize night time interruptions
2. Monitor vital signs for changes
3. Administer IV fluids and vasopressors as ordered
4. Monitor client during activity for tachycardia, SOB decreased BP
5. Closely observe client for increased respiratory rate, decreased pulse oximetry, increase edema, crackles on auscultation of lung sounds and JVD
6. Administer diuretics as ordered
7. Teach client about the importance of a low-sodium diet
e. Septic shock
i. Nursing assessment
1. Subjective data
a. Symptoms, client understanding
2. Objective data
a. Physical examination, tachycardia, temperature elevation
ii. Nursing interventions
1. Assess for signs of hypotension or hypoxia
2. Administer antipyretics if the client is febrile
3. Monitor for hypothermia
4. Closely monitor client’s temperature
5. Administer oxygen as ordered
6. Administer vasopressors as ordered
64. Define what sepsis is and who is most vulnerable to it.
a. Increases with age
65. Define which clients are at highest risk for anaphylactic shock and review the common meds used to treat it.
a. The highest “at-risk” clients have penicillin allergies and insect sting reactions
b. Epinephrine is used to treat it
c. Can also use corticosteroids
66. Id meds or treatments used to treat different types of shock
a. Hypovolemic shock
i. Blood transfusion, IV fluid
ii. Epinephrine, dobutrex, intropin, primacor, nitroglycerin, nitroprusside sodium, norepinephrine, phenylephrine
b. Cardiogenic shock
i. Intropin, dobutrex primacor, norepinephrine, phenylephrine, nitroglycerin, nitropress
c. Septic shock
i. Broad-spectrum antibiotics are administered but will later be altered according to blood culture and sensitivity
ii. Methylprednisolone is steroid of choice
d. Neurogenic shock
i. IV gluid, vasopressors, supplemental oxygen, and respiratory support if needed
ii. IV administration is first line treatment option
e. Anaphylactic shock
i. Epinephrine (Epi-Pen)
67. Explain what the D-dimer test is for.
a. Fibrin degradation fragment
b. Elevated if a clot is present
c. Normal: 0.4 mcg/mL
68. Identify s/s of severe hypovolemic shock
a. Leads to poor tissue perfusion and hypoxia
69. Review what a nurse needs to include when teaching a client how to use an epi-pen
a. Do not inject intravenously or into buttocks (subcutaneous preferred), store at room temperature an do not expose to extreme heat or direct sunlight
b. Inject in outer thigh
Module 8 and 9
70. Review the definition of an emergency
a. Can be defined as a medical or surgical condition requiring immediate or timely intervention to prevent permanent disability or death
71. Review the methods of triage in an emergency department as well as the various categories.
a. Simplest method of triaging clients is to use the American heart association’s basic life support principles: compressions-airway-breathing (CAB)
b. Categories
i. Emergent
1. Require immediate care
ii. Urgent
1. Require care within 1-2 hours
iii. Nonurgent
1. Can be delayed without the risk of permanent consequences
c. Mass casualty is most likely to survive and traditional is most critical first
72. Review nursing interventions for an evisceration.
a. Instruct the client to remain quiet and avoid coughing or straining
b. Position the client to prevent further stress on the wound
c. Use sterile dressings, such as ABD pads soaked with sterile normal saline, to cover the wound and internal contents
d. Administer oxygen, initiate IV access, monitor bowel sounds
73. What determine the extent of injury when exposed to a chemical warfare agent?
a. What chemical it is
b. Length of exposure
c. Amount of chemical
74. List the symptoms of radiation sickness
a. Nausea
b. Vomiting
c. Diarrhea
75. Explain the procedure if a client experiences a chemical exposure of the eyes.
a.
76. Explain the procedure for administering ear drops to an adult client.
a. Pull pinnae up and back
Module 9:
77. Explain imagery and how it may be utilized to improve health
a. To visualize pleasant, soothing image
b. Nurses can use guided imagery with clients capable of hearing and understanding suggestions
78. Define antioxidants, the function they serve and give examples
a. Substances that prevent or inhibit oxidation
b. Prevent tissue damage from free radicals
c. May prevent heart disease, cancer, or cataracts
d. Examples
i. Vitamin C
ii. Vitamin E
iii. Vitamin A
iv. Beta-carotene
v. Selenium
79. Review appropriate CAMs for pain in general as well as cancer pain.
a. Relaxation
80. Define psychoneuroimmounology
a. Describes connection of thought with physical reaction
b. Supports that the human mind can alter the physiology of the body
81. Explain the use of biofeedback
a. Works by teaching clients to “recognize how their bodies are functioning and to control patterns of physiological function”
82. Review herbal substances to aid in lowering blood pressure as well as hyperlipidemia.
a. Garlic (Allium sativum)
[Show More]