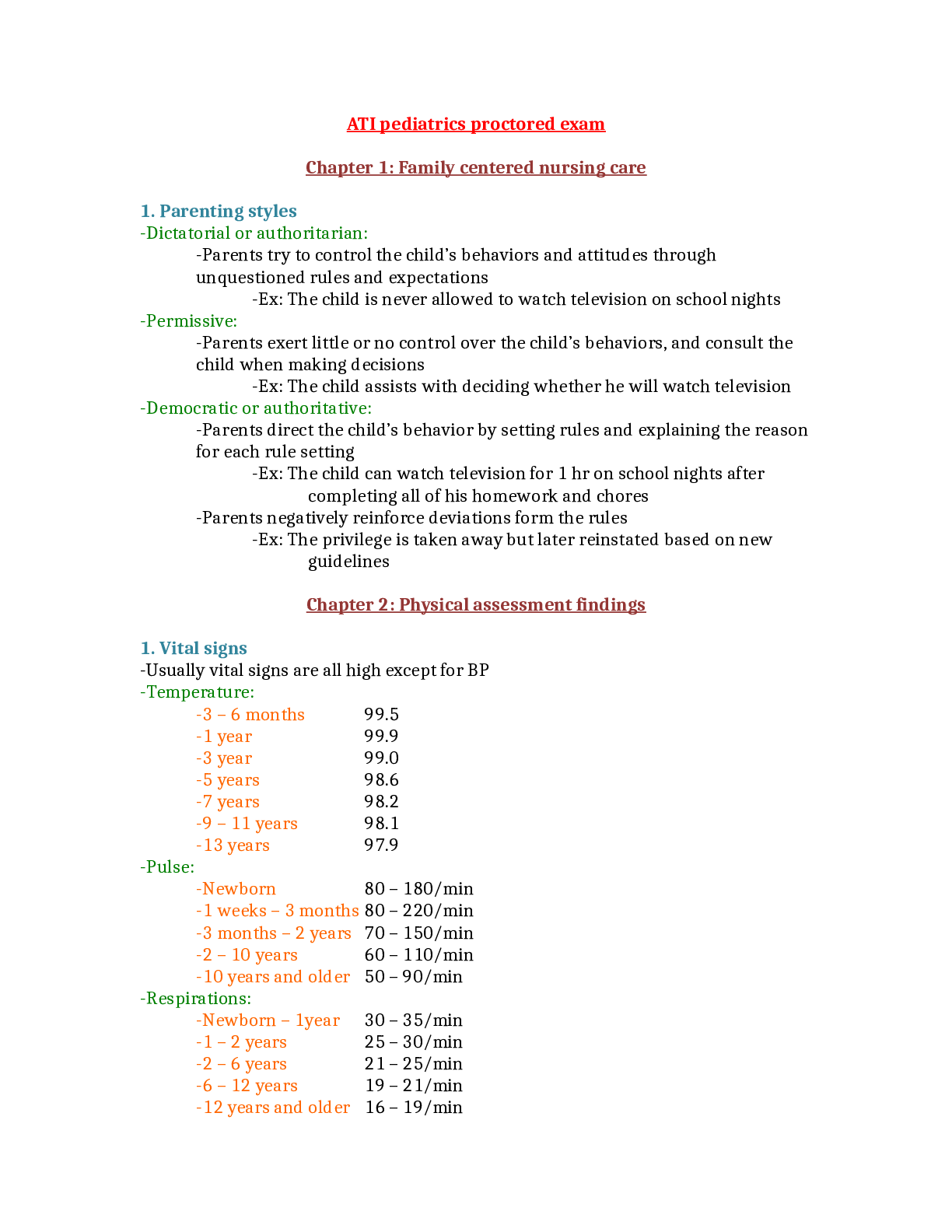
Signs of pregnancy
presumptive (subjective signs) Amenorrhea, nausea, vomiting, increased urinary frequency, excessive fatigue, breast tenderness, quickening at 18–20 weeks
probable (objective signs) Goodell sign (soft
...
Signs of pregnancy
presumptive (subjective signs) Amenorrhea, nausea, vomiting, increased urinary frequency, excessive fatigue, breast tenderness, quickening at 18–20 weeks
probable (objective signs) Goodell sign (softening of cervix) Chadwick sign (cervix is blue/purple)
Hegar’s sign (softening of lower uterine segment) Uterine enlargement
Braxton Hicks contractions (may be palpated by 28 weeks)
Uterine soufflé (soft blowing sound due to blood pulsating through the placenta) Integumentary pigment changes
Ballottement, fetal outline definable, positive pregnancy test (could be hydatidiform mole, choriocarcinoma, increased pituitary gonadotropins at menopause) positive (diagnostic signs) Fetal heart rate auscultated by fetoscope at 17–20 weeks or by Doppler at 10–12 weeks Palpable fetal outline and fetal movement after 20 weeks
Visualization of fetus with cardiac activity by ultrasound (fetal parts visible by 8 weeks)
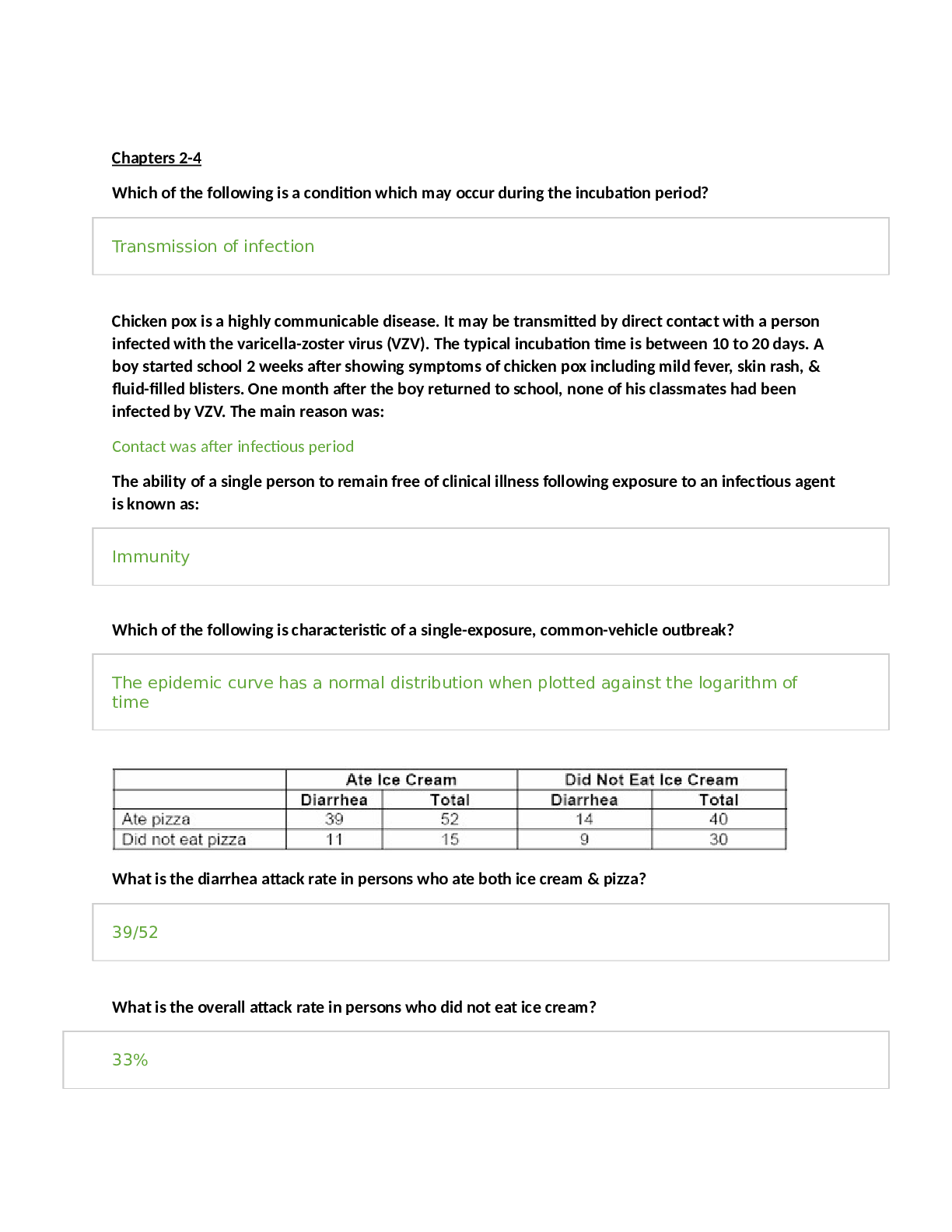
Pregnancy and fundal height measurement
Signs of pregnancy (presumptive, probable, positive)
Pregnancy and fundal height measurement As pregnancy progresses, the fundus rises out of the pelvis (Figure 29-1). At 12 weeks’ gestation, the fundus is located at the level of the symphysis pubis. By week 16, it rises to midway between symphysis pubis and the umbilicus. By 20 weeks’ gestation, the fundus is typically at the same height as the umbilicus. Until term, the fundus enlarges approximately 1 cm per week. As the time for birth approaches, the fundal height drops slightly. This process, which is commonly called lightening, occurs for a woman who is a primigravida around 38 weeks’ gestation but may not occur for the woman who is a multigravida until she goes into labor
DOWNLOAD TO PASS
QUIZGUIDER82
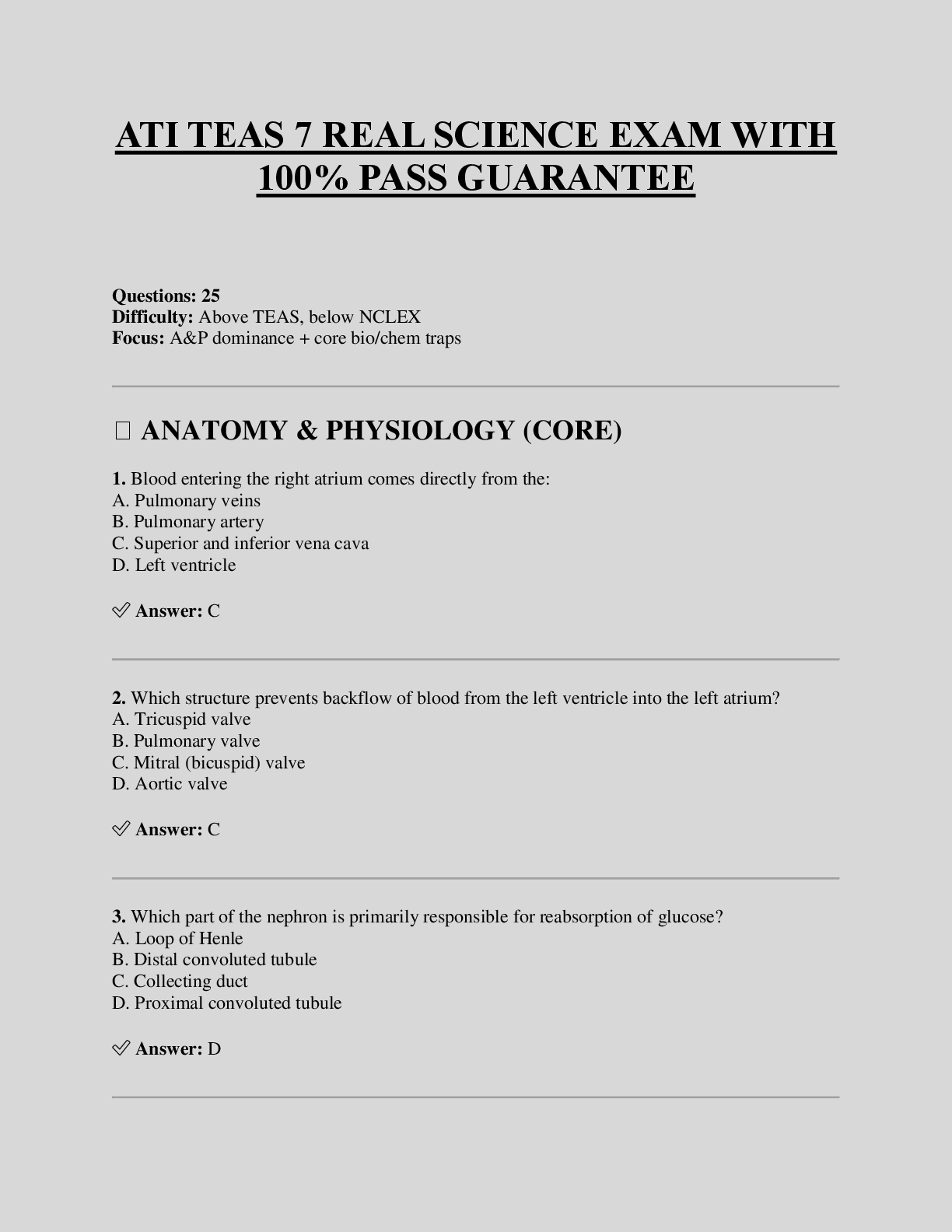
Naegele’s rule
Add seven days to the first day of your LMP and then subtract three months. For example, if your LMP was November 1, 2017: Add seven days (November 8, 2017). Subtract three months (August 8, 2017).
The EDD is calculated by adding seven days to the first day of the last menstrual period, subtracting three months and adding one year.
This formula is known as Naegele's Rule. For example, if the patient's last menstrual period, LMP, was on August 10, 2019, the EDD would be calculated as follows. LMP equals August 10, 2019 plus seven days. August 17, 2019, minus three months. May 17, 2019 plus one year and that equals May 17, 2020.
Hematological changes during pregnancy
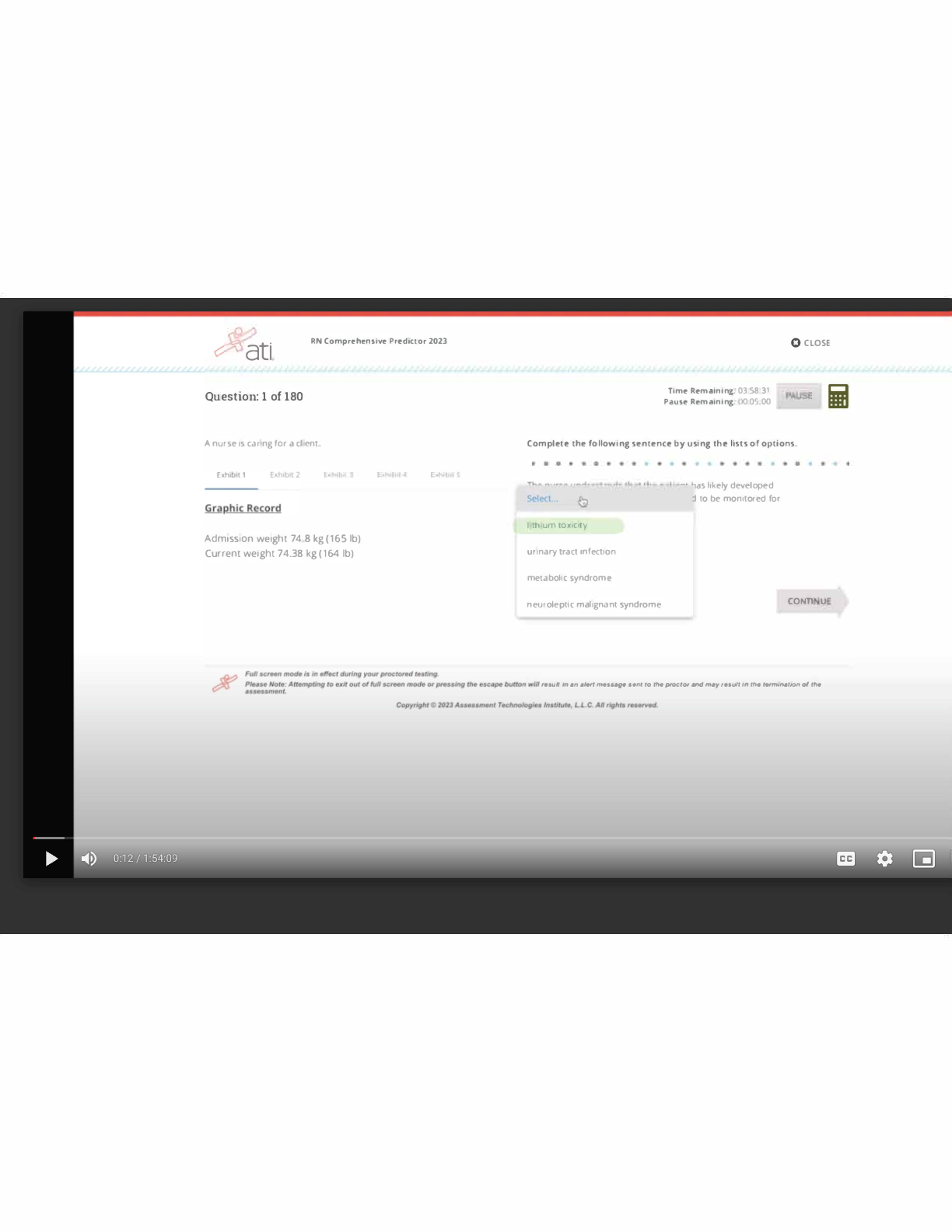
During pregnancy, the heart is displaced upward and to the left within the chest cavity by the gravid uterus’s pressure on the diaphragm. As pregnancy progresses, the risk for inferior vena cava and aortic compression leading to supine hypotension increases when the woman lies in a supine position. To avoid hypotension and potential syncope, the woman should be advised to lie in a left lateral position. Hemodynamic changes and anatomic changes also may alter vital signs in the pregnant woman (Table 29-2).
DOWNLOAD TO PASS
QUIZGUIDER82
Cardiac output in pregnancy increases by 30% to 50% over that in women who are not pregnant (Blackburn, 2013; Ouziunian & Elkayam, 2012). This increase peaks in the early third trimester and is maintained until birth. Half of the total increase in cardiac output, however, occurs by the eighth week of pregnancy (Blackburn, 2013). Therefore, women with cardiac disease may become symptomatic during the first trimester. Stroke volume is also increased during pregnancy by 20% to 30%. These increases in cardiac output and stroke volume allow for the 30% increase in oxygen consumption observed during pregnancy.
TABLE 29-2 Vital Sign Changes in Pregnancy
Vital Sign
Changes in Pregnancy
Measurement Alterations in Pregnancy
Heart rate and heart sounds
Volume of the first heart sound may be increased with splitting. Third heart sound may be detected. Systolic murmurs may be detected. Increases by 15–20 beats/min by 32 weeks’ gestation.
Palpate the maternal pulse when auscultating the fetal heart rate to be able to distinguish between the two.
Respiratory rate
Increases by 1–2 breaths/min
None
BP
First trimester: same as prepregnancy values Second trimester: systolic BP decreases by 2–8 mm Hg and diastolic BP decreases by 5–15 mm Hg due to peripheral vascular resistance
Third trimester: gradually returns to prepregnancy values
Use of an automated cuff may improve accuracy of measurement, as some pregnant women do not have a fifth Korotkoff sound.
Systolic and diastolic BP may be 16 mm Hg higher when taken while the woman is sitting.
BP readings may decrease in the maternal left lateral position.
Abbreviation: BP, blood pressure.
Data from Jarvis, C. (2016). Physical examination and health assessment (7th ed.). St. Louis, MO: Saunders Elsevier; Ouziunian, J., & Elkayam, U. (2012). Physiologic changes during normal pregnancy and delivery. Cardiology Clinics, 30, 317–329; Tan, E., & Tan, E. (2013). Alterations in physiology and anatomy during pregnancy. Best Practice & Research Clinical Obstetrics & Gynaecology, 27, 791–802. During pregnancy, blood volume increases by 30% to 50%, or 1,100 to 1,600 mL (Ouziunian & Elkayam, 2012), and peaks at 30 to 34 weeks’ gestation. The increase in blood volume improves blood flow to the vital organs and protects against excessive blood loss during birth. Fetal growth during pregnancy and newborn weight are correlated with the degree of blood volume expansion.
Of the blood volume expansion occurring during pregnancy, 75% is considered to be plasma (King et al., 2015). There is also a slight increase in red blood cell volume
[Show More]
![Preview image of NR602 MIDTERM STUDYGUIDE 2022[APPROVED] document](https://scholarfriends.com/storage/NR602 MIDTERM STUDYGUIDE 2022[APPROVED].png)




 Complete solutions.png)
 NURS 3247Pharmacology - Proctored Assessment,.png)