The AGACNP is reviewing a chart of a head-injured patient. Which of the following would alert the AGACNP
for the possibility that the patient is over hydrated, thereby increasing the risk for increased intracranial pre
...
The AGACNP is reviewing a chart of a head-injured patient. Which of the following would alert the AGACNP
for the possibility that the patient is over hydrated, thereby increasing the risk for increased intracranial pressure?
BUN = 10
Shift output = 800 ml, shift input = 825 ml Unchanged
weight Serum osmolality = 260
Answers available at https://bit.ly/2VNFmXT
A patient who has been in the intensive care unit for 17 days develops hypernatremic hyperosmolality. The
patient weighs 132 lb (59.9 kg), is intubated, and is receiving mechanical ventilation. The serum osmolality is
320 mOsm/L kg H2O. Clinical signs include tachycardia and hypotension. The adult-gerontology acute care
nurse practitioner's initial treatment is to:
reduce serum osmolality by infusing a 5% dextrose in 0.2% sodium chloride solution
reduce serum sodium concentration by infusing a 0.45% sodium chloride solution replenish volume by infusing
a 0.9% sodium chloride solution
replenish volume by infusing a 5% dextrose in water solution.
Answers available at https://bit.ly/2VNFmXT
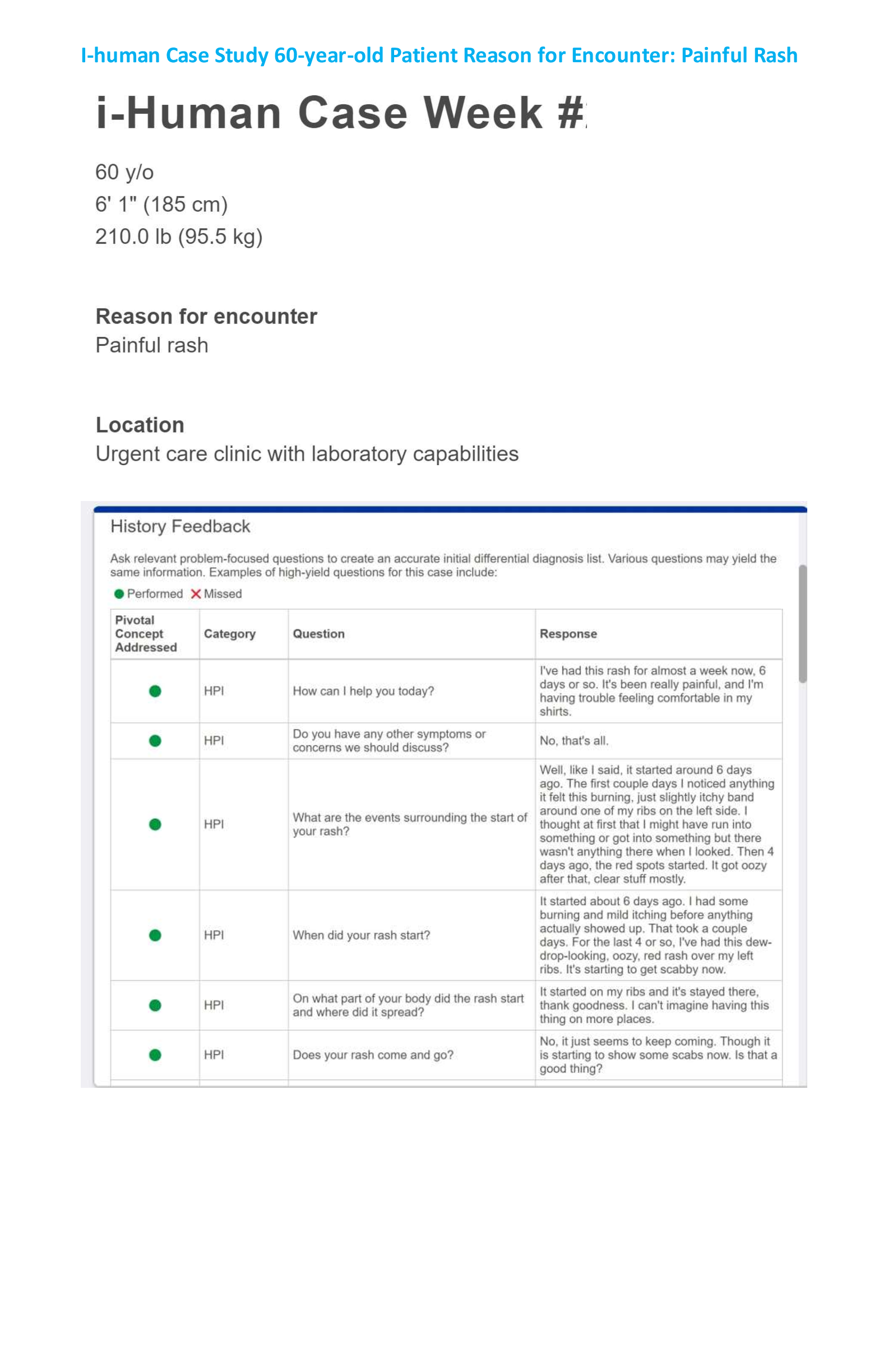
A 16-year-old male presents with fever and right lower quadrant discomfort. He complains of nausea and has
had one episode of vomiting, but he denies any diarrhea. His vital signs are as follows: temperature 101.9°F,
pulse 100 bpm, respirations 16 breaths per minute, and blood pressure 110/70 mm Hg. A complete blood count
reveals a WBC count of 19,100 cells/µL. The AGACNP expects that physical examination will reveal:
+ Murphy’s sign
+ Chvostek’s sign
+ McBurney’s sign
+ Kernig’s sign
Myasthenia gravis is best described as:
An imbalance of dopamine and acetylcholine in the basal ganglia Demyelination of peripheral ascending nerves
Demyelination in the central nervous system
An autoimmune disorder characterized by decreased neuromuscular activation
Mrs. Coates is a 65-year-old female who is on postoperative day 1 following a duodenal resection for a bleeding
ulcer. She had an uneventful immediate postoperative course, but throughout the course of day 1 she has
complained of a mild abdominal discomfort that has progressed throughout the day. This evening the AGACNP
is called to the bedside to evaluate the patient for persistent and progressive discomfort. Likely causes of her
symptoms include all of the following except:
Colic due to return of peristalsis Leakage from the duodenal stump Gastric retention
Hemorrhage
Answers available at https://bit.ly/2VNFmXT
[Show More]