Grading Rubric
1. 40% = History questions
2. 30% = physical exam
3. 10% = differential diagnosis list
4. 10% = ranking the differential diagnosis
5. 10% = lab test
6. 0% = science exercises
7. 0% = management plan
...
Grading Rubric
1. 40% = History questions
2. 30% = physical exam
3. 10% = differential diagnosis list
4. 10% = ranking the differential diagnosis
5. 10% = lab test
6. 0% = science exercises
7. 0% = management plan – faculty scores this.
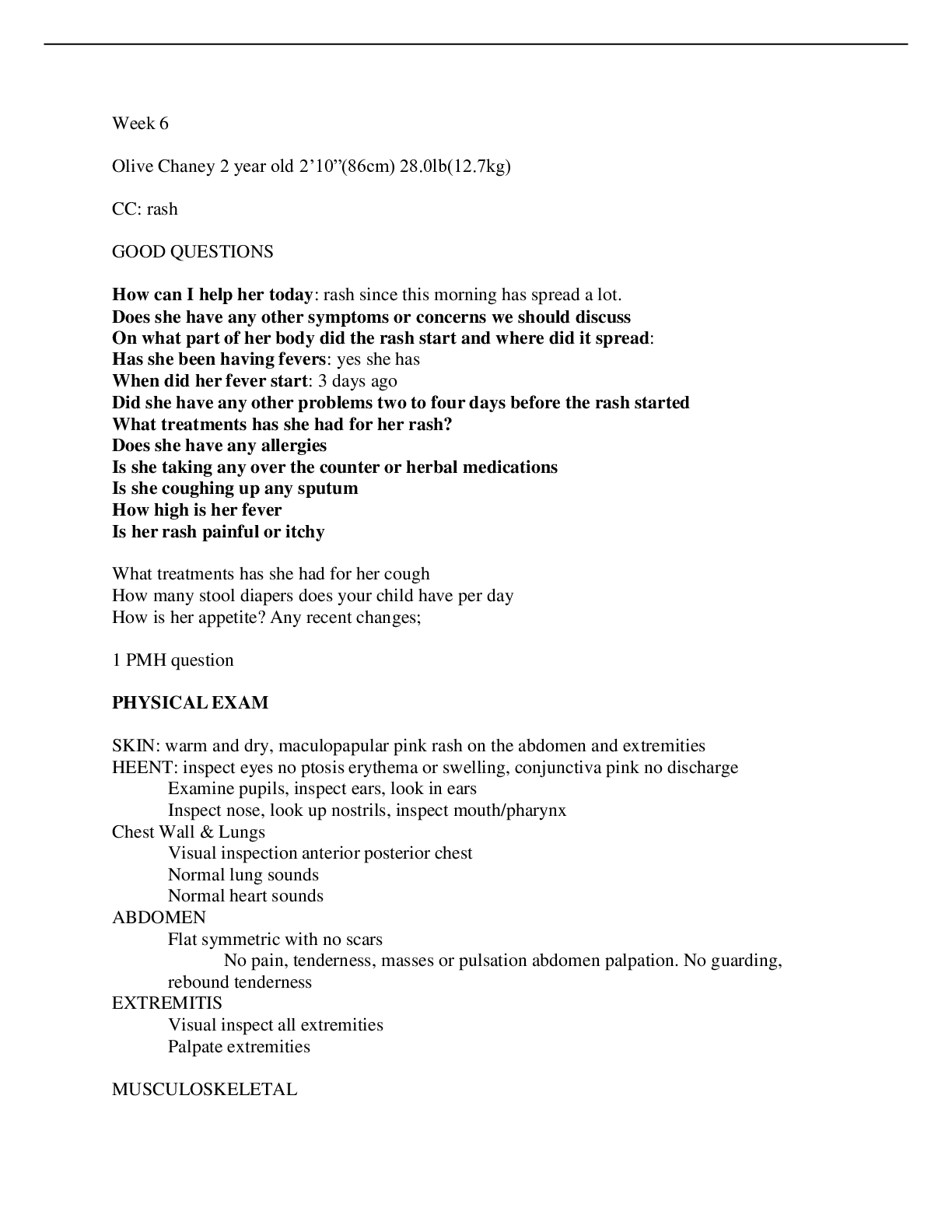
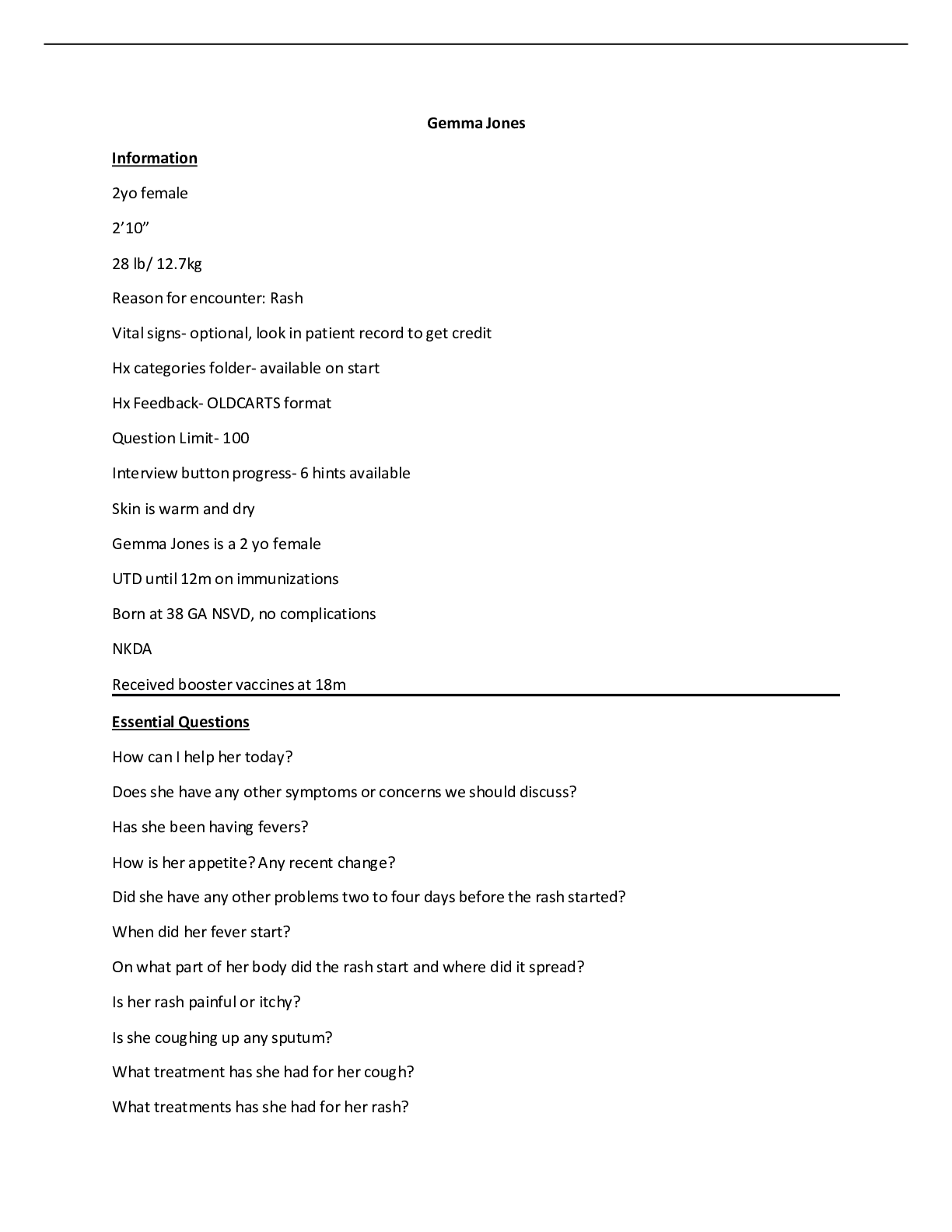
Case Help
HISTORY:
Patient interview reminder sheet- document in key findings
“Good Question” means you asked a required question
Step 1: Start by asking 2 open ended patient centric questions:
1. How can I help you today?
2. Any other symptoms or concerns?
Step 2: Obtain an HPI using “OLDCARTS”
O = Onset; circumstances surrounding start of symptom
L = Location, radiation
D = Duration
C = Characteristics (sharp, dull, cramping)
A = Aggravating
R = Relieving
T = Treatments
S = Severity
Step 3: PMH
No patient record – Obtain history
Have patient record – Update allergies, medications, OTC drugs
Step 4: FH
No patient record – Obtain history
Step 5: SH
No patient record- obtain history
Have patient record- Update if major changes in living situation, death of partner, loss of
job etc.
Step 6: ROS
Questions for systems not addressed in HPI
Choose ROS for the body systems you do not have information on. Use the large
multipart questions
Physical Exam
Do those physical assessment maneuvers as needed
Choose ROS for those body systems you do not have information on. Use large multipart
questions.
Assessment
Organize key findings list by selecting the MSAP (Most significant active problem).
Mark other findings as; related, unrelated, unknown, PMH/resolved.
Problem Statement
Short summary of patient’s presentation. Should contain: 1. Demographic description, 2.
Chief complaint, 3. Hx and PE key findings, 4. Risk factors. Keep it concise.
Differential Diagnosis
List disease you are considering Prior to ordering tests.
Tests:
Determine what tests are needed to rule in or rule out each diagnosis on authors corrected
list.
Review authors corrected list of test results.
Final Diagnosis
Select a final diagnosis or diagnoses.
Treatment plan
Write a treatment plan following your instructors’ guidelines.
Gear head exercises
Complete exercises found throughout the case (look for the brain with gears icon in steps
of the case)
Summary
Proceed all the way to the “Summary” tab.
Submit your case and press the “see evaluation” button to see your first evaluation.
Paisley Ward
16 y/o
5’5 (165cm)
150.0lb (68.2kg)
BMI 25
A&Ox4
Reason for encounter: Cough and SOB
Vital Signs
Temp: 37.0 (98.6)
Pulse: 88 bpm, rhythm: regular, strength: normal
BP L/arm 112/82, R/arm 114/80, assessment: normal, pulse pressure: normal
RR:26 bpm, rhythm: regular, effort: unlabored
SpO2: 94%
3 yr ago visit:
Reason: For Physical examination
Psych: stress at home with financial situation of family. No anxiety or SI
PMH: Eczema: uses moisturizer daily no flares for several yrs.
Hosp/Surg: Normal birth, full term, no medical problems. No major accidents or injuries. No surgeries.
Prev health: last check up 1 yr ago. UTD on all immunizations
Meds: None
Allg: NKDA
Social:
Lives at home with mother and father. Only child. Father lost job, works odd jobs to pay bills. Mother
works at fast food restaurant. Evicted from home looking for place to live.
Denies past/present use of alcohol, tobacco, or illicit drugs. Never been sexually active. States she does
get sad sometimes due to her family’s recent financial and living situation but she does not feel like she
is depressed. She denies SI.
FHX: Father: Eczema, otherwise healthy, Mother: no medical problems, No other significant family
history.
HISTORY Questions:
Skin: pink, warm, moist
1. How can I help you today?
Cough for the last three weeks which has been getting worse. I’ve also had SOB when
walking to my next class at school. I have to stop and take a break.
2. Do you have any other symptoms or concerns we should discuss?
[Show More]