Health Care > EXAM > CRCR EXAM MULTIPLE CHOICE, CRCR Exam Prep, Certified Revenue Cycle Representative - CRCR 2023,100% C (All)
CRCR EXAM MULTIPLE CHOICE, CRCR Exam Prep, Certified Revenue Cycle Representative - CRCR 2023,100% CORRECT
Document Content and Description Below
CRCR EXAM MULTIPLE CHOICE, CRCR Exam Prep, Certified Revenue Cycle Representative - CRCR 2023 What are collection agency fees based on? - CORRECT ANSWERSA percentage of dollars collected Self-... funded benefit plans may choose to coordinate benefits using the gender rule or what other rule? - CORRECT ANSWERSBirthday In what type of payment methodology is a lump sum or bundled payment negotiated between the payer and some or all providers? - CORRECT ANSWERSCase rates What customer service improvements might improve the patient accounts department? - CORRECT ANSWERSHolding staff accountable for customer service during performance reviews What is an ABN (Advance Beneficiary Notice of Non-coverage) required to do? - CORRECT ANSWERSInform a Medicare beneficiary that Medicare may not pay for the order or service What type of account adjustment results from the patient's unwillingness to pay for a self-pay balance? - CORRECT ANSWERSBad debt adjustment What is the initial hospice benefit? - CORRECT ANSWERSTwo 90-day periods and an unlimited number of subsequent periods When does a hospital add ambulance charges to the Medicare inpatient claim? - CORRECT ANSWERSIf the patient requires ambulance transportation to a skilled nursing facility How should a provider resolve a late-charge credit posted after an account is billed? - CORRECT ANSWERSPost a late-charge adjustment to the account an increase in the dollars aged greater than 90 days from date of service indicate what about accounts - CORRECT ANSWERSThey are not being processed in a timely manner What is an advantage of a preregistration program? - CORRECT ANSWERSIt reduces processing times at the time of service What are the two statutory exclusions from hospice coverage? - CORRECT ANSWERSMedically unnecessary services and custodial care What core financial activities are resolved within patient access? - CORRECT ANSWERSScheduling, insurance verification, discharge processing, and payment of point-of-service receipts What statement applies to the scheduled outpatient? - CORRECT ANSWERSThe services do not involve an overnight stay How is a mis-posted contractual allowance resolved? - CORRECT ANSWERSComparing the contract reimbursement rates with the contract on the admittance advice to identify the correct amount What type of patient status is used to evaluate the patient's need for inpatient care? - CORRECT ANSWERSObservation Coverage rules for Medicare beneficiaries receiving skilled nursing care require that the beneficiary has received what? - CORRECT ANSWERSMedically necessary inpatient hospital services for at least 3 consecutive days before the skilled nursing care admission When is the word "SAME" entered on the CMS 1500 billing form in Field 0$? - CORRECT ANSWERSWhen the patient is the insured What are non-emergency patients who come for service without prior notification to the provider called? - CORRECT ANSWERSUnscheduled patients If the insurance verification response reports that a subscriber has a single policy, what is the status of the subscriber's spouse? - CORRECT ANSWERSNeither enrolled not entitled to benefits Regulation Z of the Consumer Credit Protection Act, also known as the Truth in Lending Act, establishes what? - CORRECT ANSWERSDisclosure rules for consumer credit sales and consumer loans What is a principal diagnosis? - CORRECT ANSWERSPrimary reason for the patient's admission Collecting patient liability dollars after service leads to what? - CORRECT ANSWERSLower accounts receivable levels What is the daily out-of-pocket amount for each lifetime reserve day used? - CORRECT ANSWERS50% of the current deductible amount What service provided to a Medicare beneficiary in a rural health clinic (RHC) is not billable as an RHC services? - CORRECT ANSWERSInpatient care What code indicates the disposition of the patient at the conclusion of service? - CORRECT ANSWERSPatient discharge status code What are hospitals required to do for Medicare credit balance accounts? - CORRECT ANSWERSThey result in lost reimbursement and additional cost to collect When an undue delay of payment results from a dispute between the patient and the third party payer, who is responsible for payment? - CORRECT ANSWERSPatient Medicare guidelines require that when a test is ordered for a LCD or NCD exists, the information provided on the order must include: - CORRECT ANSWERSA valid CPT or HCPCS code With advances in internet security and encryption, revenue-cycle processes are expanding to allow patients to do what? - CORRECT ANSWERSAccess their information and perform functions on-line What date is required on all CMS 1500 claim forms? - CORRECT ANSWERSonset date of current illness What does scheduling allow provider staff to do - CORRECT ANSWERSReview appropriateness of the service request What code is used to report the provider's most common semiprivate room rate? - CORRECT ANSWERSCondition code Regulations and requirements for coding accountable care organizations, which allows providers to begin creating these organizations, were finalized in: - CORRECT ANSWERS2012 What is a primary responsibility of the Recover Audit Contractor? - CORRECT ANSWERSTo correctly identify proper payments for Medicare Part A & B claims How must providers handle credit balances? - CORRECT ANSWERSComply with state statutes concerning reporting credit balance Insurance verification results in what? - CORRECT ANSWERSThe accurate identification of the patient's eligibility and benefits What form is used to bill Medicare for rural health clinics? - CORRECT ANSWERSCMS 1500 What activities are completed when a scheduled pre-registered patient arrives for service? - CORRECT ANSWERSRegistering the patient and directing the patient to the service area In addition to being supported by information found in the patient's chart, a CMS 1500 claim must be coded using what? - CORRECT ANSWERSHCPCS (Healthcare Common Procedure Coding system) What results from a denied claim? - CORRECT ANSWERSThe provider incurs rework and appeal costs Why does the financial counselor need pricing for services? - CORRECT ANSWERSTo calculate the patient's financial responsibility What type of provider bills third-party payers using CMS 1500 form - CORRECT ANSWERSHospital-based mammography centers How are disputes with nongovernmental payers resolved? - CORRECT ANSWERSAppeal conditions specified in the individual payer's contract The important message from Medicare provides beneficiaries with information concerning what? - CORRECT ANSWERSRight to appeal a discharge decision if the patient disagrees with the services Why do managed care plans have agreements with hospitals, physicians, and other healthcare providers to offer a range of services to plan members? - CORRECT ANSWERSTo improve access to quality healthcare If a patient remains an inpatient of an SNF (skilled nursing facility for more than 30 days, what is the SNF permitted to do? - CORRECT ANSWERSSubmit interim bills to the Medicare program. 90. MSP (Medicare Secondary Payer) rules allow providers to bill Medicare for liability claims after what happens? - CORRECT ANSWERS120 days passes, but the claim then be withdrawn from the liability carrier What data are required to establish a new MPI entry? - CORRECT ANSWERSThe patient's full legal name, date of birth, and sex What should the provider do if both of the patient's insurance plans pay as primary? - CORRECT ANSWERSDetermine the correct payer and notify the incorrect payer of the processing error What do EMTALA regulations require on-call physicians to do? - CORRECT ANSWERSPersonally appear in the emergency department and attend to the patient within a reasonable time At the end of each shift, what must happen to cash, checks, and credit card transaction documents? - CORRECT ANSWERSThey must be balanced What will cause a CMS 1500 claim to be rejected? - CORRECT ANSWERSThe provider is billing with a future date of service Under Medicare regulations, which of the following is not included on a valid physician's order for services? - CORRECT ANSWERSThe cost of the test how are HCPCS codes and the appropriate modifiers used? - CORRECT ANSWERSTo report the level 1, 2, or 3 code that correctly describes the service provided If a Medicare patient is admitted on Friday, what services fall within the three-day DRG window rule? - CORRECT ANSWERSDiagnostic and clinically-related non-diagnostic charges provided on the Tuesday, Wednesday, Thursday, and Friday before admission What is a benefit of pre-registering patient's for service? - CORRECT ANSWERSPatient arrival processing is expedited, reducing wait times and delays What is a characteristic of a managed contracting methodology? - CORRECT ANSWERSProspectively set rates for inpatient and outpatient services What do the MSP disability rules require? - CORRECT ANSWERSThat the patient's spouse's employer must have less than 20 employees in the group health plan what organization originated the concept of insuring prepaid health care services? - CORRECT ANSWERSBlue Cross and blue Shield What is true about screening a beneficiary for possible MSP situations? - CORRECT ANSWERSIt is acceptable to complete the screening form after the patient has completed the registration process and been sent to the service department If the patient cannot agree to payment arrangements, what is the next option? - CORRECT ANSWERSWarn the patient that unpaid accounts are placed with collection agencies for further processing In services lines such as cardiology or orthopedics, what does the case-rate payment methodology allow providers to do? - CORRECT ANSWERSReceive a fixed for specific procedures What will comprehensive patient access processing accomplish? - CORRECT ANSWERSMinimize the need for follow-up on insurance accounts Through what document does a hospital establish compliance standards? - CORRECT ANSWERSCode of conduct How does utilization review staff use correct insurance information? - CORRECT ANSWERSTo obtain approval for inpatient days and coordinate services When is it not appropriate to use observation status? - CORRECT ANSWERSAs a substitute for an inpatient admission What is a serious consequence of misidentifying a patient in the MPI? - CORRECT ANSWERSThe services will be documented in the wrong record When a patient reports directly to a clinical department for service, what will the clinical department staff do? - CORRECT ANSWERSRedirect the patient to the patient access department for registration What process can be used to shorten claim turnaround time? - CORRECT ANSWERSSend high-dollar hard-copy claims with required attachments by overnight mail or registered mail How are patient reminder calls used? - CORRECT ANSWERSTo make sure the patient follows the prep instructions and arrives at the scheduled time for service If a patient declares a straight bankruptcy, what must the provider do? - CORRECT ANSWERSWrite off the account to the contractual adjustment account According to the Department of Health and Human Services guidelines, what is NOT considered income? - CORRECT ANSWERSSale of property, house, or car The situation where neither the patient nor spouse is employed is described to the patient using: - CORRECT ANSWERSA condition code What option is an alternative to valid long-term payment plans? - CORRECT ANSWERSBank loans What is an advantage of using a collection agency to collect delinquent patient accounts? - CORRECT ANSWERSCollection agencies collect accounts faster than hospital does What statement DOES NOT apply to revenue codes? - CORRECT ANSWERSrevenue codes identify the payer When a patient's illness results in an unusually high amount of medical bills not covered by insurance or other patient pay resources, what type of account is created - CORRECT ANSWERScatastrophic charity What happens when a patient receives non-emergent services from and out-of-network provider? - CORRECT ANSWERSPatient payment responsibility is higher Every patient who is new to the healthcare provider must be offered what? - CORRECT ANSWERSA printed copy of the provider's privacy notice How may a collection agency demonstrate its performance? - CORRECT ANSWERSCalculate the rate of recovery What is true of the information the provider supplies to indicate that an authorization for service has been received from the patient's primary payer? - CORRECT ANSWERSIt is posted on the remittance advice by the payer What standard claim forms are currently used by the healthcare industry to submit claims to third-party payers? - CORRECT ANSWERSThe UB-04 and the CMS 1500 Unless the patient encounter is an emergency, what is the efficient and effective procedure for obtaining information? - CORRECT ANSWERSObtain the required demographic and insurance information before services are rendered what protocol was developed through the Patient Friendly Billing Project? - CORRECT ANSWERSProvide information using language that is easily understood by the average reader What technique is acceptable way to complete the MSP screening for a facility situation? - CORRECT ANSWERSAsk if the patient's current services was accident related What is a valid reason for a payer to delay a claim? - CORRECT ANSWERSFailure to complete authorization requirements IF outpatient diagnostic services are provided within three days of the admission of a Medicare beneficiary to an IPPS (Inpatient Prospective Payment System) hospital, what must happen to these charges - CORRECT ANSWERSThey must be combined with the inpatient bill and paid under the MS-DRG system What do large adjustments require? - CORRECT ANSWERSManager-level approval What items are valid identifiers to establish a patient's identification? - CORRECT ANSWERSPhoto identification, date of birth, and social security number What must a provider do to qualify an account as a Medicare bad debts? - CORRECT ANSWERSPursue the account for 120 days and then refer it to an outside collection agency What restriction does a managed care plan place on locations that must be used if the plan is to pay for the services provided? - CORRECT ANSWERSSite-of-service limitation What is an example of an outcome of the Patient Friendly Billing Project? - CORRECT ANSWERSRedesigned patient billing statements using patient-friendly language What statement describes the APC (Ambulatory payment classification) system? - CORRECT ANSWERSAPC rates are calculated on a national basis and are wage-adjusted by geographic region What is a benefit of insurance verification? - CORRECT ANSWERSPre-certification or pre-authorization requirements are confirmed What is an effective tool to help staff collect payments at the time of service? - CORRECT ANSWERSDevelop scripts for the process of requesting payments What is a benefit of electronic claims processing? - CORRECT ANSWERSProviders can electronically view patient's eligibility What does Medicare Part D provide coverage for? - CORRECT ANSWERSPrescription drugs What are some core elements of a board-approved financial policy - CORRECT ANSWERSCharity care, payment methods, and installment payment guidelines What circumstance would result in an incorrect nightly room charge? - CORRECT ANSWERSIf the patient's discharge, ordered for tomorrow, has not been charted What is NOT a typical charge master problem that can result in a denial? - CORRECT ANSWERSDoes not include required modifiers Access - CORRECT ANSWERSAn individual's ability to obtain medical services on a timely and financially acceptable level Administrative Services Only (ASO) - CORRECT ANSWERSUsually contracted administrative services to a self-insured health plan Case management - CORRECT ANSWERSThe process whereby all health-related components of a case are managed by a designated health professional. Intended to ensure continuity of healthcare accessibility and services Claim - CORRECT ANSWERSA demand by an insured person for the benefits provided by the group contract Coordination of benefits (COB) - CORRECT ANSWERSa typical insurance provision that determines the responsibility for primary payment when the patient is covered by more than one employer-sponsored health benefit program Discounted fee-for-service - CORRECT ANSWERSA reimbursement methodology whereby a provider agrees to provide service on a fee for service basis, but the fees are discounted by certain packages Eligibility - CORRECT ANSWERSPatient status regarding coverage for healthcare insurance benefits First dollar coverage - CORRECT ANSWERSA healthcare insurance policy that has no deductible and covers the first dollar of an insured's expenses Gatekeeping - CORRECT ANSWERSA concept wherein the primary care physician provides all primary patient care and coordinates all diagnostic testing and specialty referrals required for a patient's medical care Health plan - CORRECT ANSWERSan insurance company that provides for the delivery or payment of healthcare services Indemnity insurance - CORRECT ANSWERSnegotiated healthcare coverage within a framework of fee schedules, limitations, and exclusions that is offered by insurance companies or benevolent associations Medically necessary - CORRECT ANSWERSHealthcare services that are required to preserve or maintain a person's health status in accordance with medical practice standards Out-of-area benefits - CORRECT ANSWERShealthcare plan coverage allowed to covered persons for emergency situations outside of the prescribed geographic area of the HMO Out-of-pocket payments - CORRECT ANSWERSCash payments made by the insured for services not covered by the health insurance plan Pre-admission review - CORRECT ANSWERSthe practice of reviewing requests for inpatient admission before the patient is admitted to ensure that the admission is medically necesary Pre-existing condition limitation - CORRECT ANSWERSA restriction on payments for charges directly resulting from a pre-existing health conditions Same-day admission - CORRECT ANSWERSA cost containment practice that reduces a surgical patient's inpatient stay by requiring that pre-procedure testing and preparation are completed on an outpatient basis and the patient is admitted the same day as the procedure Self-insured - CORRECT ANSWERSLarge employers who assume direct responsibility or risk for paying employees' healthcare without purchasing health insurance Subrogation - CORRECT ANSWERSSeeking, by legal or administrative means, reimbursement from another party that is primarily responsible for a patient's medical expenses Subscriber - CORRECT ANSWERSAn employer, a union, or an association that contracts with an insurance company for the healthcare plan it offers to eligible employees Sub-specialist - CORRECT ANSWERSA healthcare professional who is recognized to have expertise in a specialty of medicine or surgery Third-part administrator (TPA) - CORRECT ANSWERSProvides services to employers or insurance companies for utilization review, claims payment and benefit design Third-party reimbursement - CORRECT ANSWERSA general term used for the healthcare benefit payments - used to identify that for benefit plans there are three parties in the transaction Usual, customary, and reasonable (UCR) - CORRECT ANSWERSHealth insurance plan reimbursement methodology that limits payment to the lower billed charges, the provider's customary charge, or the prevailing charge for the service in the community Utilization review - CORRECT ANSWERSReview conducted by professional healthcare personnel of the appropriateness of, quality of, and need for healthcare services provided to patients Charge - CORRECT ANSWERSThe dollar amount a provider sets for services rendered before negotiating any discounts. The charge can be different from the amount paid Cost - CORRECT ANSWERSThe definition of cost varies by party incurring the expense Price - CORRECT ANSWERSthe total amount a provider expects to be paid by payers and patients for healthcare services Care purchaser - CORRECT ANSWERSIndividual or entity that contributes to the purchase of healthcare services Payer - CORRECT ANSWERSAn organization that negotiates or sets rates for provider services, collects revenue through premium payments or tax dollars, processes provider claims for service, and pays provider claims using collected premium or tax revenues Provider - CORRECT ANSWERSAn entity, organization, or individual that furnishes a healthcare service Out of pocket payment - CORRECT ANSWERSThe portion of the total payment for medical services and treatment for which the patient is responsible, including copayments, coinsurance, and deductibles Price transparency - CORRECT ANSWERSIn health care, readily available information on the price of healthcare services that, together, with other information helps define the value of those services and enables patients and other care purchasers to identify, compare, and choose providers that offer the desired level of value Value - CORRECT ANSWERSThe quality of a healthcare service in relation to the total price paid for the service by care purchasers What areas does the code of conduct typically focus on? - CORRECT ANSWERSHuman resources. Privacy/confidentiality. Quality of care. Billing/coding. Conflicts of interest. Laws/regulations FERA - CORRECT ANSWERSFraud Enforcement and Recovery act ESRD - CORRECT ANSWERSEnd-stage renal disease. The patient has permanent kidney failure, is covered by a GHP, and has not yet completed the 30-month coordination period What is the purpose of a compliance program? - CORRECT ANSWERSMitigate potential fraud and abuse in the industry-specific key risk areas What is important about an effective corporate compliance program? - CORRECT ANSWERSA program that embodies many elements to create a program that is transparent, clearly articulated and emphasized at all employee levels as a seriously held personal and organizational responsibility, one that relies on full communication inside and outside the organization What is a CCO - CORRECT ANSWERSChief compliance officer - they typically report directly to the board of directors/trustees as well as the chief executive officer, and has limited responsibilities for other operational aspects of the organization What are the situations where another payer may be completely responsible for payment? - CORRECT ANSWERSWork-related accidents, black lung program services, patient is enrolled in Medicare Advantage, Federal grant programs Under Medicare rules, certain outpatient services that are provided within three days of the admission date, by hospitals or by entities owned or controlled by hospitals, must be billed as part of an inpatient stay. - CORRECT ANSWERSTRUE The OIG has issued compliance guidance/model compliance plans for all of the following entities: - CORRECT ANSWERShospices. physician practices. ambulance providers Providers who are found to be in violation of CMS regulations are subject to: - CORRECT ANSWERSCorporate integrity agreements What MSP situation requires LGHP - CORRECT ANSWERSDisability The disadvantages of outsourcing include all of the following EXCEPT: a) The impact of customer service or patient relations b) The impact of loss of direct control of accounts receivable services c) Increased costs due to vendor ineffectiveness d) Reduced internal staffing costs and a reliance on outsourced staff - CORRECT ANSWERSD The Medicare fee-for service appeal process for both beneficiaries and providers includes all of the following levels EXCEPT: a) Medical necessity review by an independent physician's panel b) Judicial review by a federal district court c) Redetermination by the company that handles claims for Medicare d) Review by the Medicare Appeals Council (Appeals Council) - CORRECT ANSWERSB Business ethics, or organizational ethics represent: a) The principles and standards by which organizations operate b) Regulations that must be followed by law c) Definitions of appropriate customer service d) The code of acceptable conduct - CORRECT ANSWERSA A portion of the accounts receivable inventory which has NOT qualified for billing includes: a) Charitable pledges b) Accounts created during pre-registration but not activated c) Accounts coded but held within the suspense period d) Accounts assigned to a pre-collection agency - CORRECT ANSWERSA Local Coverage Determinations (LCD) and National Coverage Determinations (NCD) are Medicare established guideline(s) used to determine: a) Medicare and Medicaid provider eligibility b) Medicare outpatient reimbursement rates c) Which diagnoses, signs, or symptoms are reimbursable d) What Medicare reimburses and what should be referred to Medicaid - CORRECT ANSWERSC Days in A/R is calculated based on the value of: a) The total accounts receivable on a specific date b) Total anticipated revenue minus expenses c) The time it takes to collect anticipated revenue d) Total cash received to date - CORRECT ANSWERSC Patients are contacting hospitals to proactively inquire about costs and fees prior to agreeing to service. The problem for hospitals in providing such information is: a) That hospitals don't want to establish a price without knowing if the patient has insurance and how much reimbursement can be expected b) The fact that charge master lists the total charge, not net charges that reflect charges after a payer's contractual adjustment c) That hospitals don't want to be put in the position of "guaranteeing" price without having room for additional charges that may arise in the course of treatment d) Their reluctance to share proprietary information - CORRECT ANSWERSB Across all care settings, if a patient consents to a financial discussion during a medical encounter to expedite discharge, the HFMA best practice is to: a) Make sure that the attending staff can answer questions and assist in obtaining required patient financial data b) Have a patient financial responsibilities kit ready for the patient, containing all of the required registration forms and instructions c) Support that choice, providing that the discussion does not interfere with patient care or disrupt patient flow d) Decline such request as finance discussions can disrupt patient care and patient flow - CORRECT ANSWERSC A comprehensive "Compliance Program" is defined as a) Annual legal audit and review for adherence to regulations b) Educating staff on regulations c) Systematic procedures to ensure that the provisions of regulations imposed by a government agency are being met d) The development of operational policies that correspond to regulations - CORRECT ANSWERSC Case Management requires that a case manager be assigned a) To patients of any physician requesting case management b) To a select patient group c) To every patient d) To specific cases designated by third party contractual agreement - CORRECT ANSWERSB Pricing transparency is defined as readily available information on the price of healthcare services, that together with other information, help define the value of those services and enable consumers to a) Identify, compare, and choose providers that offer the desired level of value b) Customize health care with a personally chosen mix of providers c) Negotiate the cost of health plan premiums d) Verify the cost of individual clinicians - CORRECT ANSWERSA Any healthcare insurance plan that provides or ensures comprehensive health maintenance and treatment services for an enrolled group of persons based on a monthly fee is known as a a) MSO b) HMO c) PPO d) GPO - CORRECT ANSWERSB In a Chapter 7 Straight Bankruptcy filing a) The court liquidates the debtor's nonexempt property, pays creditors, and discharges the debtor from the debt b) The court liquidates the debtor's nonexempt property, pays creditors, and begins to pay off the largest claims first. All claims are paid some portion of the amount owed c) The court vacates all claims against a debtor with the understanding that the debtor may not apply for credit without court supervision d) The court establishes a creditor payment schedule with the longest outstanding claims paid first - CORRECT ANSWERSA The core financial activities resolved within patient access include: a) Scheduling, pre-registration, insurance verification and managed care processing b) Scheduling, insurance verification, clinical discharge processing and payment posting of point of service receipts c) Scheduling, registration, charge entry and managed care processing d) Scheduling, pre-registration, registration, medical necessity screening and patient refunds - CORRECT ANSWERSA Which of the following is NOT contained in a collection agency agreement? a) A clear understanding that the provider retains ownership of any outsourced activities b) Specific language as to who will pay legal fees, if needed c) An annual renewal clause d) A mutual hold-harmless clause - CORRECT ANSWERSD Maintaining routine contact with the health plan or liability payer, making sure all required information is provided and all needed approvals are obtained is the responsibility of: a) Patient Accounts b) Managed Care Contract Staff c) HIM staff d) Case Management - CORRECT ANSWERSD What is required for the UB-04/837-I, used by Rural Health Clinics to generate payment from Medicare? a) Revenue codes b) Correct Part A and B procedural codes c) The CMS 1500 Part B attachment d) Medical necessity documentation - CORRECT ANSWERSA Before classifying and subsequently writing off an account to financial assistance or bad debt, the hospital must establish policy, define appropriate criteria, implement procedures for identifying and processing accounts: a) Monitor compliance b) Have the account triaged for any partial payment possibilities c) Assist in arranging for a commercial bank loan d) Obtain the patients income tax statements from the prior 2 years - CORRECT ANSWERSA For routine scenarios, such as patients with insurance coverage or a known ability to pay, financial discussions: a) Are optional b) Should take place between the patient or guarantor and properly trained provider representatives c) May take place between the patient and discharge planning d) Are focused on verifying required third-party payer information - CORRECT ANSWERSB The purpose of a financial report is to: a) Provide a public record, if reqluested b) Present financial information to decision makers c) Prepare tax documents d) Monitor expenses - CORRECT ANSWERSB Which statement is an EMTALA (Emergency Medical Treatment and Active Labor Act) violation? a) Registration staff may routinely contact managed are plans for prior authorizations before the patient is seen by the on-duty physician b) Initial registration activities may occur so long as these activities do not delay treatment or suggest that treatment with not be provided to uninsured individuals c) Co-payments may be collected at the time of service once the medical screening and stabilization activities are completed d) Signage must be posted where it can be easily seen and read by patients - CORRECT ANSWERSA A claim is denied for the following reasons, EXCEPT: a) The health plan cannot identify the subscriber b) The frequency of service was outside the coverage timeline c) The submitted claim does not have the physicians signature d) The subscriber was not enrolled at the time of service - CORRECT ANSWERSC Any provider that has filed a timely cost report may appeal an adverse final decision received from the Medicare Administrative Contractor (MAC). This appeal may be filed with a) A court appointed federal mediator b) The Department of Health and Human Services Provider Relations Division c) The Office of the Inspector General d) The Provider Reimbursement Review Board - CORRECT ANSWERSD Charges, as the most appropriate measurement of utilization, enables a) Generation of timely and accurate billing b) Managing of expense budgets c) Accuracy of expense and cost capture d) Effective HIM planning - CORRECT ANSWERS???Number 24??? Ambulance services are billed directly to the health plan for a) All pre-admission emergency transports b) Services provided before a patient is admitted and for ambulance rides arranged to pick up the patient from the hospital after discharge to take him/her home or to another facility c) The portion of the bill outside of the patient's self-pay d) Transports deemed medically necessary by the attending paramedic-ambulance crew - CORRECT ANSWERSC An individual enrolled in Medicare who is dissatisfied with the government's claim determination is entitled to reconsideration of the decision. This type of appeal is known as a) A beneficiary appeal b) A Medicare supplemental review c) A payment review d) A Medicare determination appeal - CORRECT ANSWERSA The nuanced data resulting from detailed ICD-10 coding allows senior leadership to work with physicians to do all of the following EXCEPT: a) Drive significant improvements in the areas of quality and the patient experience b) Embrace new reimbursement models c) Improve outcomes d) Obtain higher compensation for physicians - CORRECT ANSWERSD Duplicate payments occur: a) When providers re-bill claims based on nonpayment from the initial bill submission b) When service departments do not process charges with the organization's suspense days c) When the payer's coordination of benefits is not captured correctly at the time of patient registration d) When there are other healthcare claims in process and the anticipated deductibles and co-insurance amounts still show open but will be met by the in-process claims - CORRECT ANSWERSa The Affordable Care Act legislated the development of Health Insurance Exchanges, where individuals and small businesses can a) Purchase qualified health benefit plans regardless of insured's health status b) Obtain price estimates for medical services c) Negotiate the price of medical services with providers d) Meet federal mandates for insurance coverage and obtain the corresponding tax deduction - CORRECT ANSWERSA The most common resolution methods for credit balances include all of the following EXCEPT: a) Designate the overpayment for charity care b) Submit the corrected claim to the payer incorporating credits c) Either send a refund or complete a takeback form as directed by the payer d) Determine the correct primary payer and notify incorrect payer of overpayment - CORRECT ANSWERSA EFT (electronic funds transfer) is a) An electronic claim submission b) The record of payments in the hospital's accounting system c) An electronic confirmation that a payment is due d) An electronic transfer of funds from payer to payee - CORRECT ANSWERSD Revenue cycle activities occurring at the point-of-service include all of the following EXCEPT: a) The monitoring of charges b) The provision of case management and discharge planning services c) Providing charges to the third-party payer as they are incurred d) The generation of charges - CORRECT ANSWERSC Medicare beneficiaries remain in the same "benefit period" a) Up to hospitalization discharge b) Until the beneficiary is "hospitalization and/or skilled nursing facility-free" for 60 consecutive days c) Each calendar year d) Up to 60 days - CORRECT ANSWERSB Key Performance Indicators (KPIs) set standards for accounts receivables (A/R) and a) Provide evidence of financial status b) Provide a method of measuring the collection and control of A/R c) Establish productivity targets d) Make allowance for accurate revenue forecasting - CORRECT ANSWERSB Recognizing that health coverage is complicated and not all patients are able to navigate this terrain, HFMA best practices specify that a) The patient accounts staff have someone assigned to research coverage on behalf of patients b) Patients should be given the opportunity to request a patient advocate, family member, or other designee to help them in these discussions c) Patient coverage education may need to be provided by the health plan d) A representative of the health plan be included in the patient financial responsibilities discussion - CORRECT ANSWERSB When there is a request for service, the scheduling staff member must confirm the patient's unique identification information to a) Check if there is any patient balance due b) Verify the patient's insurance coverage if the patient is a returning customer c) Confirm that physician orders have been received d) Ensure that she/he accesses the correct information in the historical database - CORRECT ANSWERSD Once the price is estimated in the pre-service stage, a provider's financial best practice is to a) Explain to the patient their financial responsibility and to determine the plan for payment b) Allow the patient time to compare prices with other providers c) Lock-in the prices d) Have another employee double check the price estimate - CORRECT ANSWERSA What type of account adjustment results from the patient's unwillingness to pay a self- pay balance? a) Charity adjustment b) Bad debt adjustment c) Contractual adjustment d) Administrative adjustment - CORRECT ANSWERSB All of the following are conditions that disqualify a procedure or service from being paid for by Medicare EXCEPT a) Medically unnecessary b) Not delivered in a Medicare licensed care setting c) Offered in an outpatient setting d) Services and procedures that are custodial in nature - CORRECT ANSWERSD All of the following are forms of hospital payment contracting EXCEPT a) Contracted Rebating b) Per Diem Payment c) Fixed Contracting d) Bundled Payment - CORRECT ANSWERSA Overall aggregate payments made to a hospice are subject to a computed "cap amount" calculated by: a) The Center for Medicare and Medicaid Services (CMS) b) Each state's Medicaid plan c) Medicare d) The Medicare Administrative Contractor (MAC) at the end of the hospice cap period - CORRECT ANSWERSD With the advent of the Affordable Care Act Health Insurance Marketplaces and the expansion of Medicaid in some states, it is more important than ever for hospitals to a) Reschedule the visit for non-payment of a prior balance b) Strictly limit charity care and bad-debt c) Collect patient's self-pay and deductibles in the first encounter d) Assist patients in understanding their insurance coverage and their financial obligation - CORRECT ANSWERSD A nightly room charge will be incorrect if the patient's a) Discharge for the next day has not been charted b) Condition has not been discussed during the shift change report meeting c) Pharmacy orders to the ICU have not been entered in the pharmacy system d) Transfer from ICU (intensive care unit) to the Medical/Surgical floor is not reflected in the registration system - CORRECT ANSWERSD Which of the following is required for participation in Medicaid? a) Meet income and assets requirements b) Meet a minimum yearly premium c) Be free of chronic conditions d) Obtain a health insurance policy - CORRECT ANSWERSA HFMA best practices call for patient financial discussions to be reinforced a) By issuing a new invoice to the patient b) By copying the provider's attorney on a written statement of conversation c) By obtaining some type of collateral d) By changing policies to programs - CORRECT ANSWERSB A Medicare Part A benefit period begins: a) With admission as an inpatient b) The first day in which an individual has not been a hospital inpatient not in a skilled nursing facility for the previous 60 days c) Upon the day the coverage premium is paid d) Immediately once authorization for treatment is provided by the health plan - CORRECT ANSWERSA If further treatment can only be provided in a hospital setting, the patient's condition cannot be evaluated and/or treated within 24 hours, or if there is not an anticipation of improvement in the patient's condition with 24 hours, the patient a) Will remain in observation for up to 72 hours after which the patient is admitted as an inpatient b) Will be admitted as an inpatient c) Will be discharged and if needed, designated to a priority one outpatient status d) Will have his/her case reviewed by the attending physician, a consulting physician and the primary care physician and a future course of care will then be determined - CORRECT ANSWERSB It is important to have high registration quality standards because a) Incomplete registrations will trigger exclusion from Medicare participation b) Incomplete registrations will raise satisfaction scores for the hospital c) Inaccurate registration may cause discharge before full treatment is obtained d) Inaccurate or incomplete patient data will delay payment or cause denials - CORRECT ANSWERSD Medicare will only pay for tests and services that a) Constitute appropriate treatment and are fairly priced b) Have solid documentation c) Can be demonstrated as necessary d) Medicare determines are "reasonable and necessary" - CORRECT ANSWERSD Room and bed charges are typically posted a) From case management reports generated for contracted payers b) Through the case management daily resource report c) At the end of each business day d) From the midnight census - CORRECT ANSWERSD The process of creating the pre=registration record ensures a) Ability to pursue extraordinary collection activities b) Early and productive communication with a third-party payer c) Accurate billing d) That access staff will have the compete and valid information needed to finalize any remaining pre-access activities - CORRECT ANSWERSC Once the EMTALA requirements are satisfied a) Third-party payer information should be collected from the patient and the payer should be notified of the ED visit b) The patient then assumes full liability for services unless a third- party is notified or the patient applies for financial assistance with the first 48 hours c) The remaining registration processing is initiated at the bedside or in a registration area d) An initial registration records is completed so that the proper coding can be initiated - CORRECT ANSWERSC This directive was developed to promote and ensure healthcare quality and value and also to protect consumers and workers in the healthcare system. This directive is called a) Payer quality monitoring b) Medicare patient and staff safety standards c) Joint Commission for Accreditation of Healthcare Organizations (JCAHO) safety d) Patient bill of rights - CORRECT ANSWERSD A scheduled inpatient represents an opportunity for the provider to do which of the following? a) Refer the patient to another location with the health system b) Comply with EMTALA (Emergency Medical Treatment and Labor Act) requirements before service c) Complete registration and insurance approval before service d) Register the patient after he or she is placed in a bed on that service unit. - CORRECT ANSWERSC The first and most critical step in registering a patient, whether scheduled or unscheduled, is a) Having the patient initial the HIPAA privacy statement b) Verifying insurance to activate the patient medical record c) Verifying the patient's identification d) Check the schedule for treatment availability - CORRECT ANSWERSC The legal authority to request and analyze provider clam documentation to ensure that IPPS services were reasonable and necessary is given to a) Recovery Audit Contractors (RAC) b) The Office of the U.S. Inspector General (OIG) c) All health plans d) State insurance commissioners - CORRECT ANSWERSB An advantage of a pre-registration program is a) The opportunity to reduce processing times at the time of service b) The ability to eliminate no-show appointments c) The opportunity to reduce the corporate compliance failures within the registration process d) The marketing value of such a program - CORRECT ANSWERSC Claims with dates of service received later than one calendar year beyond the date of service, will be a) Denied by Medicare b) The provider's responsibility but can be deemed charity care c) Fully paid with interest d) The full responsibility of the patient. - CORRECT ANSWERSA This concept encompasses all activities required to send a request for payment to a third-party health plan for payment of benefits a) Third-party invoicing b) Account resolution c) Claims processing d) Billing - CORRECT ANSWERSC The ACO investment model will test the use of pre-paid shared savings to a) Raise quality ratings in designated hospitals. b) Encourage new ACOs to form in rural and underserved areas c) Attract physicians to participate in the ACO payment system d) Invest in treatment protocols that reduce costs to Medicare - CORRECT ANSWERSB Chapter 13 Bankruptcy, debtor rehabilitation, is a court proceeding a) That establishes a payment priority order to creditors' claims b) That classifies the debtor as eligible for government financial assistance for housing, medical treatment and food as debts are paid c) That creates a clear court-supervised payment accountability plan going forward d) That reorganizes a debtor's holdings and instructs creditors to look to the debtor's future earnings for payment - CORRECT ANSWERSD HFMA's patient financial communication best practices specify that patients should be told about the types of services provided and a) A satisfaction survey regarding clinical service providers b) The price of service to their covering health plan c) The service providers that typically participate in the service, e.g., radiologists, pathologists, etc. d) An expiration of why a specific service is not provided - CORRECT ANSWERSC The important Message from Medicare provides beneficiaries information concerning their a) Understanding of billing issues and the deductibles and/or co-insurance due for the current visit b) Right to refuse to use lifetime reserve days for the current stay c) Right to appeal a discharge decision if the patient disagrees with the plan d) Obligation to reimburse the hospital for any services not covered by the Medicare program - CORRECT ANSWERSC All of the following are potential causes of credit balances EXCEPT a) Duplicate payments b) Primary and secondary payers both paying as primary c) Inaccurate upfront collections based on incorrect liability estimates d) A patient's choice to build up a credit against future medical bills - CORRECT ANSWERSD Medicare Part B has an annual deductible, and the beneficiary is responsible for a) A co-insurance payment for all Part B covered services b) Physicians office fees c) Tests outside of an inpatient setting d) Prescriptions - CORRECT ANSWERSA The importance of medical records being maintained by HIM is that the patient records a) Are the primary source for clinical data required for reimbursement by health plans and liability payers b) Are the strongest evidence and defense in the event of a Medicare audit c) Are evidence used in assessing the quality of care d) Are the evidence cited in quality review - CORRECT ANSWERSA A decision on whether a patient should be admitted as an inpatient or become an outpatient observation patient requires medical judgments based on all of the following EXCEPT a) The patient's home care coverage b) Current medical needs c) The likelihood of an adverse event occurring to the patient d) The patient's medical history - CORRECT ANSWERSA Medicare has established guidelines called the Local Coverage Determinations (LCD) and National Coverage Determinations (NCD) that establish a) Provider and physician reimbursement for specific diagnoses and tests b) Prospective Medicare patient financial responsibilities for a given diagnosis c) Reasonable and customary prices for services in a given area d) What services or healthcare items are covered under Medicare - CORRECT ANSWERSD What are some core elements if a board-approved financial assistance policy? a) Payment requirements, staffing hours, and admission policies b) Case management, payment methods, and discharge policies c) Deposit requirements, pre-registration calling hours, and charity care policy d) Eligibility, application process, and nonpayment collection activities - CORRECT ANSWERSD The ICD-10 codes set and CPT/HCPCS code sets combines provide a) Pricing floors for services b) The financial data required for activity-based costing c) Patients an overview of services covered by their health insurance plan d) The specificity and coding needed to support reimbursement claims - CORRECT ANSWERSD A recurring/series registration is characterized by a) A creation of multiple registrations for multiple services b) The creation of one registration record for multiple days of service c) The creation of multiple patient types for one date of service d) The creation of one registration record per diagnosis per visit - CORRECT ANSWERSB Under EMTALA (Emergency Medical Treatment and Labor Act) regulations, the provider may not ask about a patient's insurance information if it would delay what? a) Complete course of treatment b) Medical screening and stabilizing treatment c) Admission to observation status d) Transfer to another facility - CORRECT ANSWERSB In resolving medical accounts, a law firm may be used as: a) An independent auditor of a financial assistance policy b) Legal counsel to patients regarding financing options c) An independent broker of patient financial assistance from banks d) A substitute for a collection agency - CORRECT ANSWERSD The unscheduled "direct" admission represents a patient who: a) Is admitted from a physician's office on an urgent basis b) Arrives at the hospital via ambulance for treatment in the emergency room c) Is an ambulatory patient who collapses in the hospital lobby d) Arrives on the medical helicopter for trauma services - CORRECT ANSWERSA In the balance resolution process, providers should: a) Stress to the patient that serious consequences may result from refusal to pay b) Remind the patient of their legal responsibility to pay the balance due c) Ask the patient if he or she would like to receive information about payment options and supportive financial assistance programs d) Tag the patients record for possible financial assistance for bad debt - CORRECT ANSWERSC Which of the following in NOT included in the Standardized Quality Measures a) Clinical outcomes b) Patient perceptions c) Health care processes d) Cost of services - CORRECT ANSWERSD In the pre-service stage, the requested service is screened for medical necessity, health plan coverage and benefits are verified and: a) Billing authorization is signed by the patient b) The patient signs the consents for treatment c) The patient signs a statement attesting an understanding and acceptance of payment policies d) Pre-authorization are obtained - CORRECT ANSWERSD Improving the overall patient experience requires revenue cycle leadership and staff to simultaneously be: a) Clear on policies and consistent in applying the policies b) Careful in screening patient demands c) Monitoring the costs and charges the patient incurs d) Inquisitive, responsive and flexible - CORRECT ANSWERSA Hospitals need which of the following information sets to assess a patient's financial status: a) Income, expenses, debt b) Patient and guarantor's income, expenses and assets c) Income, expenses and capacity to take on more debt d) Assets liquidity, Income, expenses, credit worthiness - CORRECT ANSWERSB For scheduled patients, important revenue cycle activities I the Time of Service stage DO NOT INCLUDE: a) Pre-registration record is activated, consents are signed, and co-payment is collected b) Positive patient identification is completed, and patient is given an armband c) Final bill is presented for payment d) Preprocessed patients may report to a designated "express arrival" desk - CORRECT ANSWERSC The Electronic Remittance Advice (ERA) data set is : a) Used for Electronic Funds Transfers between hospitals and a bank b) A standardized form that provides 3rd party payment details to providers c) Required for annual Medicare quality reporting forms d) Safeguards the Electronic claims process - CORRECT ANSWERSB Appropriate training for patient financial counseling staff must cover all of the following EXCEPT: a) Patient financial communications best practices specific to staff role b) Financial assistance policies c) Documenting the conversation in the medical records d) Available patient financing options - CORRECT ANSWERSC All of the following information should be reviewed as part of schedule finalization EXCEPT: a) The results of any and all test b) The service to be provided c) The arrival time and procedure time d) The patient's preparation instructions - CORRECT ANSWERSA Indemnity plans usually reimburse: a) Only for contracted Services b) A claim up to 80% of the charges c) A certain percentage of the charges after the patient meets the policy's annual deductible d) A patient for out-of-pocket charges - CORRECT ANSWERSC Because 501(r) regulations focus on identifying potential eligible financial assistants patients hospitals must: a) Capture their experience with such patients to properly budget b) Hold financial conversations with patients as soon as possible c) Build the necessary processes to handle the potentially lengthy payment schedule d) Expedite payment processing of normal accounts receivable to protect cash flow - CORRECT ANSWERSB Which option is a benefit of pre-registering a patient for services a) The patient arrival process is expedited, reducing wait times and delays b) The verification of insurance after completion of the services c) Service departments have the ability to override schedules and block time to reduce testing volume d) The patient receiving multiple calls from the provider - CORRECT ANSWERSA HIPPA had adopted Employer Identification Numbers (EIN) to be used in standard transactions to identify the employer of an individual described in a transaction EIN's are assigned by a) The Social Security Administration b) The US department of the Treasury c) The United States department of labor d) The Internal Revenue Service - CORRECT ANSWERSD The nightly room charge will be incorrect if the patient's a) Transfer from ICU to the Medical/Surgical floor is not reflected in the registration system. b) Pharmacy orders to the ICU have not been entered into the pharmacy system c) Condition has not been discussed during the shift change report meeting d) Discharge for the next day has not been charted - CORRECT ANSWERSA With any remaining open balances, after insurance payments have been posted, the account financial liability is a) Written off as bad debt b) Potentially transferred to the patient c) Sold to a collection agency d) Treated as the cost of doing business - CORRECT ANSWERSB When there is a request for service the scheduling staff member must confirm the patient's unique identification information to: a) Verify the patient's insurance coverage if the patient is a returning customer b) Ensure that she/he accesses the correct information in the historical database c) Confirm that physician orders have been received d) Check if any patient balance due - CORRECT ANSWERSB Identifying the patient, in the MPI, creating the registration record, completing medical necessity screening, determining insurance eligibility and benefits resolving managed care, requirements and completing financial education/resolution are all a) The data collection steps for scheduling and pre-registering a patient b) Registration steps that must be completed before any medical services are provided c) The steps mandated for billing Medicare Part A d) The process of closing an account - CORRECT ANSWERSA Insurance verification results in which of the following a) The accurate identification of the patient's eligibility and benefits b) The consistent formatting of the patient's name and identification number The resolution of managed care and billing requirements The identification of physician fee schedule amounts and the NPI (national provider identifier) numbers - CORRECT ANSWERSA A four digit number code established by the National Uniform Billing Committee (NUBC) that categorizes/classifies a line item in the charge master is known as a) HCPCs codes b) ICD-10 Procedural codes c) CPT codes d) Revenue codes - CORRECT ANSWERSD The importance of Medical records being maintained by HIM is that the patient records: a) Are evidence used in assessing the quality of care b) Are the primary source for clinical data required for reimbursement by health plans and liability payers C) Are the strongest evidence and defense in the event of a Medicare Audit d) Are the evidence cited in quality review - CORRECT ANSWERSB Medicare patients are NOT required to produce a physician order to receive which of these services a) Diagnostic Mammography, flu vaccine, or B-12 shots b) Diagnostic Mammography, flu vaccine, or pneumonia vaccine c) Screening Mammography, flu vaccine or pneumonia vaccine d) Screening Mammography, flu vaccine or B-12 shots - CORRECT ANSWERSC Patients should be informed that costs presented in a price estimate may a) Vary from estimates, depending on the actual services performed b) Be guaranteed if the patient satisfies all patient financial responsibilities at the time of registration c) Be lower as price estimates use the highest market price d) Only determine the percentage of the total that the patient is responsible for and not the actual cost - CORRECT ANSWERSA Ambulance services are billed directly to the health plan for a) All pre-admission emergency transports b) Transport deemed medically necessary by the attending paramedic-ambulance crew c) Services provided before a patient is admitted and for ambulance rides arranged to pick up the patient from the hospital after discharge to take him/her home or to another facility d) The portion of the bill outside of the patient's self-pay - CORRECT ANSWERSC In Chapter 7 straight bankruptcy filling a) The court establishes a creditor payment schedule with the longest outstanding claims paid first b) The court liquidates the debtor's nonexempt property, pays creditors, and discharges the debtor from the debt c) The court vacates all claims against a debtor with the understanding that the debtor may not apply for credit without court supervision d) The court liquidates the debtor's nonexempt property, pays creditors, and begins to pay off the largest claims first. All claims are paid some portions of the amount owed. - CORRECT ANSWERSB The activity which results in the accurate recording of patient bed and level of care assessment, patient transfer and patient discharge status on a real-time basis is known as a) Utilization review b) Case management c) Census management d) Patient through-put - CORRECT ANSWERSB Which of the following is required for participation in Medicaid a) Obtain a supplemental health insurance policy b) Meet income and assets requirements c) Meet a minimum yearly premium d) Be free of chronic conditions - CORRECT ANSWERSB When primary payment is received, the actual reimbursement a) Is compared to the expected reimbursement b) Is recorded by Patient Accounting and the patient's account is the closed c) Is compared to the expected reimbursement, the remaining contractual adjustments are posted, and secondary claims are submitted d) Trigger that the secondary claims can then be prepared. - CORRECT ANSWERSC Days in A/R is calculated based on the value of a) Total cash received to date b) The time it takes to collect anticipated revenue c) The total accounts receivable on a specific date d) Total anticipated revenue minus expenses - CORRECT ANSWERSC All of the following are forms of hospital payment contracting EXCEPT a) Per diem payment b) Bundled Payment c) Fixed Contracting d) Contracted Rebating - CORRECT ANSWERSD The standard claim form used for billing by hospitals, nursing facilities, and other in- patient services is called the a) UB-04 b) 1500 c) COST REPORT d) REMITTANCE NOTICE - CORRECT ANSWERSA To maximize the value derived from customer complaints, all consumer complaints should be a) Responded to within two business days b) Tracked and shared to improve the customer experience c) Handled by a specially trained "service recovery" team d) Brought immediately to management's attention - CORRECT ANSWERSA The HCAHPS (hospital consumer assessment of healthcare providers and systems) initiative was launched to a) Gather national date on overall trust in the nation's health care system b) Create a national database on physician quality c) Provide a standardized method for evaluating patient's perspective on hospital care. ? d) Provide data for building shared savings reimbursement for quality procedures. - CORRECT ANSWERSC Health Plan Contracting Departments do all of the following EXCEPT a) Establish a global reimbursement rate to use with all third-party payer b) Review all managed care contracts for accuracy for loading contract terms into the patient accounting system c) Review payment schemes to ensure that the health plan and provider understand how reimbursements must be calculated d) Review contracts to ensure the appeals process for denied claims is clearly specified - CORRECT ANSWERSA The benefit of Medicare Advantage Plan is a) It is a less costly plan compared to traditional Medicare b) Patients may retain a primary care physician and see another physician for a second opinion at no charge c) Patients generally have their Medicare-coverage healthcare through the plan and do not need to worry about "part a" or "part b" benefits d) Patients receive significant discounting on services contracted by the federal government - CORRECT ANSWERSC Once the EMTALA requirements are satisfied a) Third-party payer info should be collected from the pt and the payer should be notified of the ED visit b) An initial registration record is completed so that the proper coding can be initiated c) The pt then assumes full liability for services unless a third-party payer is notified or the pt applies for financial assistance within the first 48 hours d) The remaining registration processing is initiated either at the bedside or In a registration area - CORRECT ANSWERSA The soft cost of a dissatisfied customer is a) The "cost" of staff providing extra attention in trying to perform service recovery b) The customer passing on info about their negative experience to potential pts or through social media channels c) Potentially negative treatment outcomes leading to expanding length-of-stay d) Lowered quality outcomes for the dissatisfied pt - CORRECT ANSWERSB Concurrent review and discharge planning a) Occurs during service b) Is performed by the health plan during the time of service c) Is a significant part of quality and is performed by the clinical treatment team d) Is performed at discharge with the pt - CORRECT ANSWERSA In a self-insured (or self-funded) plan, the costs of medical care are a) Borne by the employer on a pay-as-you-go basis b) Backed-up by stop-loss insurance against a catastrophic claim c) Mandated by the Affordable Care Act for small businesses unable to obtain commercial coverage d) Created by a combination of employer and employee contributions - CORRECT ANSWERSA In choosing a setting for pt financial discussions, organizations should first and foremost a) Have processes in place to document the discussions b) Assess locations for convenience, professionalism, and comfort c) Respect the pts privacy d) Ensure all staff involved are properly trained and the pt financial education is included in all discussions - CORRECT ANSWERSC All of the following are steps in safeguarding collections EXCEPT a) Placing collections in a lock-box for posting review the next business day b) Posting the payment to the pts account c) Completing balance activities d) Issuing receipts - CORRECT ANSWERSD Which option is a government-sponsored health care program that is financed through taxesand general revenue funds a) Medicaid b) Medicare c) Insurance exchange d) Social security - CORRECT ANSWERSB It is important to calculate reserves to ensure a) Stable financial operations and accurate financial reporting b) Collateral for credit c) Expense coverage in the event of a revenue short fall d) Coverage of B/D write offs and charity care costs - CORRECT ANSWERSA Successful account resolution begins with a) Educating pts on their estimated financial responsibility b) Collecting all deductibles and copayments during the pre-service stage c) Accurate documentation of services d) Pt compliance with the course of treatment - CORRECT ANSWERSB An individual enrolled in Medicare who is dissatisfied with the government's claim determination is entitled to reconsideration of the decision. This type of appeal is known as a) A medicare determination appeal b) A payment review c) A medicare supplemental review d) A beneficiary appeal - CORRECT ANSWERSD A portion of the accounts receivable inventory which has NOT qualified for billing includes a) Charitable pledges b) Accounts assigned to a pre-collection agency c) Accounts coded but held within the suspense period d) Accounts created during pre-registration but not activated - CORRECT ANSWERSA Checks received through mail, cash received through mail, and lock box are all examples of a) Highly fraud prone processes b) Payment methods in which the majority of fraud occurs c) Payment methods being phased out for more secure payment method options d) Control points for cash posting - CORRECT ANSWERSD Recognizing that health coverage is complicated and not all pts are able to navigate this terrain, HFMA best practices specify that a) A representative of the health plan be included in the pt financial responsibilities discussion b) The patient accounts staff have someone assigned to research coverage on behalf of pts c) Pts should be given the opportunity to request a pt advocate, family member or other designee to help them In these discussions d) Pt coverage education may need to be provided by the health plan - CORRECT ANSWERSC Once the price is estimated in the pre-service stage, a provider's financial best practice is to a) Allow the pt time to compare prices with other providers b) Have another employee double check the price estimate c) Lock-in the prices d) Explain to the pt their financial responsibility and to determine the plan for payment - CORRECT ANSWERSD Charges as the most appropriate measurement of utilization enables a) Accuracy of expense and cost capture b) Managing of expense budgets c) Effective HIM planning d) Generation of timely and accurate billing - CORRECT ANSWERSA Any healthcare insurance plan that provides or ensures comprehensive health maintenance and treatment services for an enrolled group of persons based on; a monthly fee is known as a a) HMO b) PPO c) MSO d) GPO - CORRECT ANSWERSA Charges are the basis for a) Third party and regulatory review of resources used b) Evaluating quality c) Separation of fiscal responsibilities between the pt and the health plan d) Demonstrating medical necessity - CORRECT ANSWERSC Chapter 13 Bankruptcy, debtor rehabilitation is a court proceeding a) That reorganizes a debtor's holdings and instructs creditors to look to the debtors' future earnings for payment b) That establishes a payment priority order to creditos' c) That creates a clear court-supervised payment accountability plan going forward d) That classifies the debtor as eligible for government financial assistance for housing medical treatment and food as debts are paid - CORRECT ANSWERSA Pt financial communications best practices produce communications that are a) Timely and remind pts of their financial responsibilities b) Consistent, clear and transparent c) Current and report the status of a pts claim d) Timely, comprehensive and specifying next steps - CORRECT ANSWERSB Key performance indicators (KPIs) set standards for accounts receivables (A/R) and a) Establish productivity targets b) Provide a method of measuring the collection and control of A/R c) Provide evidence of financial status d) Make allowance for accurate revenue forecasting - CORRECT ANSWERSB When Recovery Audit Contractors (RAC) identify improper payments as over payments, the claims processing contractor must a) Assume legal responsibility for repaying the overage amount b) Make recovery of the overpayment the top processing priority c) Send a demand letter to the provider to recover the over payment amount d) Conduct an audit of all the effected providers claims within the past twelve months - CORRECT ANSWERSC A recurring/series registration is characterized by a) The creation of one registration record for multiple days of service b) The creation of multiple registrations for multiple services c) The creation of one registration record per diagnosis per visits d) The creation of multiple pt types for one date of service - CORRECT ANSWERSA It is important to have high registration quality standards because a) Inaccurate or incomplete pt data will delay payment or cause denials b) Incomplete registrations will trigger exclusion from Medicare participation c) Inaccurate registration may cause discharge before full treatment is obtained d) Incomplete registrations will raise satisfaction scores for the hospital - CORRECT ANSWERSA When recovery audit contractors (RAC) identify improper payments as over payments the claims processing contractor must a) Assume legal responsibility for repaying the overage amount b) Make recovery of the overpayment the top processing priority c) Send a demand letter to the provider to recover the over payment amount d) Conduct an audit of all the effected providers claims within the past 12 months - CORRECT ANSWERSC Internal controls addressing coding and reimbursement changes are put I place to guard against a) Underpayments b) Denials c) Compliance fraud by upcoding d) Charge master error - CORRECT ANSWERSC The pt discharge process begins when a) The physician writes the discharge orders b) Clinical services are completed and pt accounts have all the info necessary to bill c) The physician writes the discharge orders and the third-party payer sign-off on the necessity of the services provided d) Clinical services are completed, pt accounts can generated and accurate bill and there is agreement o the handling of pt financial responsibilities - CORRECT ANSWERSA Most major health plans including medicare and Medicaid, offer a) Toll free verification hot lines, staffed around the clock b) Electronic and/or web portal verification c) Pt "verification of benefits" cards d) A grace period for obtaining verification within 72 hours of treatment - CORRECT ANSWERSB The physician who wrote the order for an inpatient service and is in charge of the pts treatment during admission is a) The pts personal physician b) The primary care physician c) The attending physician d) The physician pt care director - CORRECT ANSWERSC An originating site is a) The location where the pts bill is generated b) The location of the pt at the time the service is provided c) The site that generates reimbursement of a claim d) The location of the medical treatment provider - CORRECT ANSWERSB HFMA best practices stipulate that a reasonable attempt should be made to have the financial responsibilities discussion a) As early as possible, before a financial obligation is incurred b) During the registration process c) Before scheduling of services d) No later than the evening of the day of admission - CORRECT ANSWERSA HFMA's pt financial communications best practices specify that pts should be told about the types of services provided and a) An explanation of why a specific service is not provided b) The service providers that typically participate in the service, e.g.radiologists, pathologists, etc. c) A satisfaction survey regarding clinical service providers d) The price of service to their covering health plan - CORRECT ANSWERSB Telemed seeks to improve a pt's health by a) Permitting 2-way real time interactive communication between the pt and the clinical professional b) Using high-compression fiber optics to transmit medical data c) Providing relevant, on-demand consumer medical education d) Providing physician access to the most current medical research - CORRECT ANSWERSA A large number of credit balances are not the result of overpayments but of a) Posting errors in the pt accounting system b) Incorrect claim submissions c) Inadequate staff training d) Banking transaction errors - CORRECT ANSWERSA Across all care settings, if a pt consents to a financial discussion during a medical encounter to expedite discharge, the HFMA best practice is to a) Have a pt financial responsibilities kit ready for the pt containing all of the required registration forms and instructions b) Make sure that the attending staff can answer questions and assist in obtaining required pt financial data c) Support that choice, providing that the discussion does not interfere with pt care or disrupt pt flow d) Decline such request as finance discussions can disrupt pt care and pt flow - CORRECT ANSWERSC The office of inspector general (OIG) publishes a compliance work plan a) Monthly b) Quarterly c) Semi-annually d) Annually - CORRECT ANSWERSD What are collection agency fees based on? - CORRECT ANSWERSA percentage of dollars collected Self-funded benefit plans may choose to coordinate benefits using the gender rule or what other rule? - CORRECT ANSWERSBirthday In what type of payment methodology is a lump sum or bundled payment negotiated between the payer and some or all providers? - CORRECT ANSWERSCase rates What customer service improvements might improve the patient accounts department? - CORRECT ANSWERSHolding staff accountable for customer service during performance reviews What is an ABN (Advance Beneficiary Notice of Non-coverage) required to do? - CORRECT ANSWERSInform a Medicare beneficiary that Medicare may not pay for the order or service What type of account adjustment results from the patient's unwillingness to pay for a self-pay balance? - CORRECT ANSWERSBad debt adjustment What is the initial hospice benefit? - CORRECT ANSWERSTwo 90-day periods and an unlimited number of subsequent periods When does a hospital add ambulance charges to the Medicare inpatient claim? - CORRECT ANSWERSIf the patient requires ambulance transportation to a skilled nursing facility How should a provider resolve a late-charge credit posted after an account is billed? - CORRECT ANSWERSPost a late-charge adjustment to the account an increase in the dollars aged greater than 90 days from date of service indicate what about accounts - CORRECT ANSWERSThey are not being processed in a timely manner What is an advantage of a preregistration program? - CORRECT ANSWERSIt reduces processing times at the time of service What are the two statutory exclusions from hospice coverage? - CORRECT ANSWERSMedically unnecessary services and custodial care What core financial activities are resolved within patient access? - CORRECT ANSWERSScheduling, insurance verification, discharge processing, and payment of point-of-service receipts What statement applies to the scheduled outpatient? - CORRECT ANSWERSThe services do not involve an overnight stay How is a mis-posted contractual allowance resolved? - CORRECT ANSWERSComparing the contract reimbursement rates with the contract on the admittance advice to identify the correct amount What type of patient status is used to evaluate the patient's need for inpatient care? - CORRECT ANSWERSObservation Coverage rules for Medicare beneficiaries receiving skilled nursing care require that the beneficiary has received what? - CORRECT ANSWERSMedically necessary inpatient hospital services for at least 3 consecutive days before the skilled nursing care admission When is the word "SAME" entered on the CMS 1500 billing form in Field 0$? - CORRECT ANSWERSWhen the patient is the insured What are non-emergency patients who come for service without prior notification to the provider called? - CORRECT ANSWERSUnscheduled patients If the insurance verification response reports that a subscriber has a single policy, what is the status of the subscriber's spouse? - CORRECT ANSWERSNeither enrolled not entitled to benefits Regulation Z of the Consumer Credit Protection Act, also known as the Truth in Lending Act, establishes what? - CORRECT ANSWERSDisclosure rules for consumer credit sales and consumer loans What is a principal diagnosis? - CORRECT ANSWERSPrimary reason for the patient's admission Collecting patient liability dollars after service leads to what? - CORRECT ANSWERSLower accounts receivable levels What is the daily out-of-pocket amount for each lifetime reserve day used? - CORRECT ANSWERS50% of the current deductible amount What service provided to a Medicare beneficiary in a rural health clinic (RHC) is not billable as an RHC services? - CORRECT ANSWERSInpatient care What code indicates the disposition of the patient at the conclusion of service? - CORRECT ANSWERSPatient discharge status code What are hospitals required to do for Medicare credit balance accounts? - CORRECT ANSWERSThey result in lost reimbursement and additional cost to collect When an undue delay of payment results from a dispute between the patient and the third party payer, who is responsible for payment? - CORRECT ANSWERSPatient Medicare guidelines require that when a test is ordered for a LCD or NCD exists, the information provided on the order must include: - CORRECT ANSWERSA valid CPT or HCPCS code With advances in internet security and encryption, revenue-cycle processes are expanding to allow patients to do what? - CORRECT ANSWERSAccess their information and perform functions on-line What date is required on all CMS 1500 claim forms? - CORRECT ANSWERSonset date of current illness What does scheduling allow provider staff to do - CORRECT ANSWERSReview appropriateness of the service request What code is used to report the provider's most common semiprivate room rate? - CORRECT ANSWERSCondition code Regulations and requirements for coding accountable care organizations, which allows providers to begin creating these organizations, were finalized in: - CORRECT ANSWERS2012 What is a primary responsibility of the Recover Audit Contractor? - CORRECT ANSWERSTo correctly identify proper payments for Medicare Part A & B claims How must providers handle credit balances? - CORRECT ANSWERSComply with state statutes concerning reporting credit balance Insurance verification results in what? - CORRECT ANSWERSThe accurate identification of the patient's eligibility and benefits What form is used to bill Medicare for rural health clinics? - CORRECT ANSWERSCMS 1500 What activities are completed when a scheduled pre-registered patient arrives for service? - CORRECT ANSWERSRegistering the patient and directing the patient to the service area In addition to being supported by information found in the patient's chart, a CMS 1500 claim must be coded using what? - CORRECT ANSWERSHCPCS (Healthcare Common Procedure Coding system) What results from a denied claim? - CORRECT ANSWERSThe provider incurs rework and appeal costs Why does the financial counselor need pricing for services? - CORRECT ANSWERSTo calculate the patient's financial responsibility What type of provider bills third-party payers using CMS 1500 form - CORRECT ANSWERSHospital-based mammography centers How are disputes with nongovernmental payers resolved? - CORRECT ANSWERSAppeal conditions specified in the individual payer's contract The important message from Medicare provides beneficiaries with information concerning what? - CORRECT ANSWERSRight to appeal a discharge decision if the patient disagrees with the services Why do managed care plans have agreements with hospitals, physicians, and other healthcare providers to offer a range of services to plan members? - CORRECT ANSWERSTo improve access to quality healthcare If a patient remains an inpatient of an SNF (skilled nursing facility for more than 30 days, what is the SNF permitted to do? - CORRECT ANSWERSSubmit interim bills to the Medicare program. 90. MSP (Medicare Secondary Payer) rules allow providers to bill Medicare for liability claims after what happens? - CORRECT ANSWERS120 days passes, but the claim then be withdrawn from the liability carrier What data are required to establish a new MPI entry? - CORRECT ANSWERSThe patient's full legal name, date of birth, and sex What should the provider do if both of the patient's insurance plans pay as primary? - CORRECT ANSWERSDetermine the correct payer and notify the incorrect payer of the processing error What do EMTALA regulations require on-call physicians to do? - CORRECT ANSWERSPersonally appear in the emergency department and attend to the patient within a reasonable time At the end of each shift, what must happen to cash, checks, and credit card transaction documents? - CORRECT ANSWERSThey must be balanced What will cause a CMS 1500 claim to be rejected? - CORRECT ANSWERSThe provider is billing with a future date of service Under Medicare regulations, which of the following is not included on a valid physician's order for services? - CORRECT ANSWERSThe cost of the test how are HCPCS codes and the appropriate modifiers used? - CORRECT ANSWERSTo report the level 1, 2, or 3 code that correctly describes the service provided If a Medicare patient is admitted on Friday, what services fall within the three-day DRG window rule? - CORRECT ANSWERSDiagnostic and clinically-related non-diagnostic charges provided on the Tuesday, Wednesday, Thursday, and Friday before admission What is a benefit of pre-registering patient's for service? - CORRECT ANSWERSPatient arrival processing is expedited, reducing wait times and delays What is a characteristic of a managed contracting methodology? - CORRECT ANSWERSProspectively set rates for inpatient and outpatient services What do the MSP disability rules require? - CORRECT ANSWERSThat the patient's spouse's employer must have less than 20 employees in the group health plan what organization originated the concept of insuring prepaid health care services? - CORRECT ANSWERSBlue Cross and blue Shield What is true about screening a beneficiary for possible MSP situations? - CORRECT ANSWERSIt is acceptable to complete the screening form after the patient has completed the registration process and been sent to the service department If the patient cannot agree to payment arrangements, what is the next option? - CORRECT ANSWERSWarn the patient that unpaid accounts are placed with collection agencies for further processing In services lines such as cardiology or orthopedics, what does the case-rate payment methodology allow providers to do? - CORRECT ANSWERSReceive a fixed for specific procedures What will comprehensive patient access processing accomplish? - CORRECT ANSWERSMinimize the need for follow-up on insurance accounts Through what document does a hospital establish compliance standards? - CORRECT ANSWERSCode of conduct How does utilization review staff use correct insurance information? - CORRECT ANSWERSTo obtain approval for inpatient days and coordinate services When is it not appropriate to use observation status? - CORRECT ANSWERSAs a substitute for an inpatient admission What is a serious consequence of misidentifying a patient in the MPI? - CORRECT ANSWERSThe services will be documented in the wrong record When a patient reports directly to a clinical department for service, what will the clinical department staff do? - CORRECT ANSWERSRedirect the patient to the patient access department for registration What process can be used to shorten claim turnaround time? - CORRECT ANSWERSSend high-dollar hard-copy claims with required attachments by overnight mail or registered mail How are patient reminder calls used? - CORRECT ANSWERSTo make sure the patient follows the prep instructions and arrives at the scheduled time for service If a patient declares a straight bankruptcy, what must the provider do? - CORRECT ANSWERSWrite off the account to the contractual adjustment account According to the Department of Health and Human Services guidelines, what is NOT considered income? - CORRECT ANSWERSSale of property, house, or car The situation where neither the patient nor spouse is employed is described to the patient using: - CORRECT ANSWERSA condition code What option is an alternative to valid long-term payment plans? - CORRECT ANSWERSBank loans What is an advantage of using a collection agency to collect delinquent patient accounts? - CORRECT ANSWERSCollection agencies collect accounts faster than hospital does What statement DOES NOT apply to revenue codes? - CORRECT ANSWERSrevenue codes identify the payer When a patient's illness results in an unusually high amount of medical bills not covered by insurance or other patient pay resources, what type of account is created - CORRECT ANSWERScatastrophic charity What happens when a patient receives non-emergent services from and out-of-network provider? - CORRECT ANSWERSPatient payment responsibility is higher Every patient who is new to the healthcare provider must be offered what? - CORRECT ANSWERSA printed copy of the provider's privacy notice How may a collection agency demonstrate its performance? - CORRECT ANSWERSCalculate the rate of recovery What is true of the information the provider supplies to indicate that an authorization for service has been received from the patient's primary payer? - CORRECT ANSWERSIt is posted on the remittance advice by the payer What standard claim forms are currently used by the healthcare industry to submit claims to third-party payers? - CORRECT ANSWERSThe UB-04 and the CMS 1500 Unless the patient encounter is an emergency, what is the efficient and effective procedure for obtaining information? - CORRECT ANSWERSObtain the required demographic and insurance information before services are rendered what protocol was developed through the Patient Friendly Billing Project? - CORRECT ANSWERSProvide information using language that is easily understood by the average reader What technique is acceptable way to complete the MSP screening for a facility situation? - CORRECT ANSWERSAsk if the patient's current services was accident related What is a valid reason for a payer to delay a claim? - CORRECT ANSWERSFailure to complete authorization requirements IF outpatient diagnostic services are provided within three days of the admission of a Medicare beneficiary to an IPPS (Inpatient Prospective Payment System) hospital, what must happen to these charges - CORRECT ANSWERSThey must be combined with the inpatient bill and paid under the MS-DRG system What do large adjustments require? - CORRECT ANSWERSManager-level approval What items are valid identifiers to establish a patient's identification? - CORRECT ANSWERSPhoto identification, date of birth, and social security number What must a provider do to qualify an account as a Medicare bad debts? - CORRECT ANSWERSPursue the account for 120 days and then refer it to an outside collection agency What restriction does a managed care plan place on locations that must be used if the plan is to pay for the services provided? - CORRECT ANSWERSSite-of-service limitation What is an example of an outcome of the Patient Friendly Billing Project? - CORRECT ANSWERSRedesigned patient billing statements using patient-friendly language What statement describes the APC (Ambulatory payment classification) system? - CORRECT ANSWERSAPC rates are calculated on a national basis and are wage-adjusted by geographic region What is a benefit of insurance verification? - CORRECT ANSWERSPre-certification or pre-authorization requirements are confirmed What is an effective tool to help staff collect payments at the time of service? - CORRECT ANSWERSDevelop scripts for the process of requesting payments What is a benefit of electronic claims processing? - CORRECT ANSWERSProviders can electronically view patient's eligibility What does Medicare Part D provide coverage for? - CORRECT ANSWERSPrescription drugs What are some core elements of a board-approved financial policy - CORRECT ANSWERSCharity care, payment methods, and installment payment guidelines What circumstance would result in an incorrect nightly room charge? - CORRECT ANSWERSIf the patient's discharge, ordered for tomorrow, has not been charted What is NOT a typical charge master problem that can result in a denial? - CORRECT ANSWERSDoes not include required modifiers Access - CORRECT ANSWERSAn individual's ability to obtain medical services on a timely and financially acceptable level Administrative Services Only (ASO) - CORRECT ANSWERSUsually contracted administrative services to a self-insured health plan Case management - CORRECT ANSWERSThe process whereby all health-related components of a case are managed by a designated health professional. Intended to ensure continuity of healthcare accessibility and services Claim - CORRECT ANSWERSA demand by an insured person for the benefits provided by the group contract Coordination of benefits (COB) - CORRECT ANSWERSa typical insurance provision that determines the responsibility for primary payment when the patient is covered by more than one employer-sponsored health benefit program Discounted fee-for-service - CORRECT ANSWERSA reimbursement methodology whereby a provider agrees to provide service on a fee for service basis, but the fees are discounted by certain packages Eligibility - CORRECT ANSWERSPatient status regarding coverage for healthcare insurance benefits First dollar coverage - CORRECT ANSWERSA healthcare insurance policy that has no deductible and covers the first dollar of an insured's expenses Gatekeeping - CORRECT ANSWERSA concept wherein the primary care physician provides all primary patient care and coordinates all diagnostic testing and specialty referrals required for a patient's medical care Health plan - CORRECT ANSWERSan insurance company that provides for the delivery or payment of healthcare services Indemnity insurance - CORRECT ANSWERSnegotiated healthcare coverage within a framework of fee schedules, limitations, and exclusions that is offered by insurance companies or benevolent associations Medically necessary - CORRECT ANSWERSHealthcare services that are required to preserve or maintain a person's health status in accordance with medical practice standards Out-of-area benefits - CORRECT ANSWERShealthcare plan coverage allowed to covered persons for emergency situations outside of the prescribed geographic area of the HMO Out-of-pocket payments - CORRECT ANSWERSCash payments made by the insured for services not covered by the health insurance plan Pre-admission review - CORRECT ANSWERSthe practice of reviewing requests for inpatient admission before the patient is admitted to ensure that the admission is medically necesary Pre-existing condition limitation - CORRECT ANSWERSA restriction on payments for charges directly resulting from a pre-existing health conditions Same-day admission - CORRECT ANSWERSA cost containment practice that reduces a surgical patient's inpatient stay by requiring that pre-procedure testing and preparation are completed on an outpatient basis and the patient is admitted the same day as the procedure Self-insured - CORRECT ANSWERSLarge employers who assume direct responsibility or risk for paying employees' healthcare without purchasing health insurance Subrogation - CORRECT ANSWERSSeeking, by legal or administrative means, reimbursement from another party that is primarily responsible for a patient's medical expenses Subscriber - CORRECT ANSWERSAn employer, a union, or an association that contracts with an insurance company for the healthcare plan it offers to eligible employees Sub-specialist - CORRECT ANSWERSA healthcare professional who is recognized to have expertise in a specialty of medicine or surgery Third-part administrator (TPA) - CORRECT ANSWERSProvides services to employers or insurance companies for utilization review, claims payment and benefit design Third-party reimbursement - CORRECT ANSWERSA general term used for the healthcare benefit payments - used to identify that for benefit plans there are three parties in the transaction Usual, customary, and reasonable (UCR) - CORRECT ANSWERSHealth insurance plan reimbursement methodology that limits payment to the lower billed charges, the provider's customary charge, or the prevailing charge for the service in the community Utilization review - CORRECT ANSWERSReview conducted by professional healthcare personnel of the appropriateness of, quality of, and need for healthcare services provided to patients Charge - CORRECT ANSWERSThe dollar amount a provider sets for services rendered before negotiating any discounts. The charge can be different from the amount paid Cost - CORRECT ANSWERSThe definition of cost varies by party incurring the expense Price - CORRECT ANSWERSthe total amount a provider expects to be paid by payers and patients for healthcare services Care purchaser - CORRECT ANSWERSIndividual or entity that contributes to the purchase of healthcare services Payer - CORRECT ANSWERSAn organization that negotiates or sets rates for provider services, collects revenue through premium payments or tax dollars, processes provider claims for service, and pays provider claims using collected premium or tax revenues Provider - CORRECT ANSWERSAn entity, organization, or individual that furnishes a healthcare service Out of pocket payment - CORRECT ANSWERSThe portion of the total payment for medical services and treatment for which the patient is responsible, including copayments, coinsurance, and deductibles Price transparency - CORRECT ANSWERSIn health care, readily available information on the price of healthcare services that, together, with other information helps define the value of those services and enables patients and other care purchasers to identify, compare, and choose providers that offer the desired level of value Value - CORRECT ANSWERSThe quality of a healthcare service in relation to the total price paid for the service by care purchasers What areas does the code of conduct typically focus on? - CORRECT ANSWERSHuman resources. Privacy/confidentiality. Quality of care. Billing/coding. Conflicts of interest. Laws/regulations FERA - CORRECT ANSWERSFraud Enforcement and Recovery act ESRD - CORRECT ANSWERSEnd-stage renal disease. The patient has permanent kidney failure, is covered by a GHP, and has not yet completed the 30-month coordination period What is the purpose of a compliance program? - CORRECT ANSWERSMitigate potential fraud and abuse in the industry-specific key risk areas What is important about an effective corporate compliance program? - CORRECT ANSWERSA program that embodies many elements to create a program that is transparent, clearly articulated and emphasized at all employee levels as a seriously held personal and organizational responsibility, one that relies on full communication inside and outside the organization What is a CCO - CORRECT ANSWERSChief compliance officer - they typically report directly to the board of directors/trustees as well as the chief executive officer, and has limited responsibilities for other operational aspects of the organization What are the situations where another payer may be completely responsible for payment? - CORRECT ANSWERSWork-related accidents, black lung program services, patient is enrolled in Medicare Advantage, Federal grant programs Under Medicare rules, certain outpatient services that are provided within three days of the admission date, by hospitals or by entities owned or controlled by hospitals, must be billed as part of an inpatient stay. - CORRECT ANSWERSTRUE The OIG has issued compliance guidance/model compliance plans for all of the following entities: - CORRECT ANSWERShospices. physician practices. ambulance providers Providers who are found to be in violation of CMS regulations are subject to: - CORRECT ANSWERSCorporate integrity agreements What MSP situation requires LGHP - CORRECT ANSWERSDisability Which of the following statements are true of HFMA's Financial Communications Best Practices - CORRECT ANSWERSThe best practices were developed specifically to help patients understand the cost of services, their individual insurance benefits, and their responsibility for balances after insurance, if any. The patient experience includes all of the following except: - CORRECT ANSWERSThe average number of positive mentions received by the health system or practice and the public comments refuting unfriendly posts on social media sites. Corporate compliance programs play an important role in protecting the integrity of operations and ensuring compliance with federal and state requirements. The code of conduct is: - CORRECT ANSWERSAll of the above Specific to Medicare fee-for-service patients, which of the following payers have always been liable for payment? - CORRECT ANSWERSPublic health service programs, Federal grant programs, veteran affairs programs, black lung program services and work-related injuries and accidents (worker' compensation claims) Provider policies and procedures should be in place to reduce the risk of ethics violations. Examples of ethics violations include: - CORRECT ANSWERSAll of the above Providers are now being reimbursed with a focus on the value of the services provided, rather than volume, which requires collaboration among providers. What is the intended outcome of collaborations made through an ACO delivery system for a population of patients? - CORRECT ANSWERSTo eliminate duplicate services, prevent medical errors and ensure appropriateness of care. Historically, revenue cycle has delt with contractual adjustments, bad debt and charity deductions from gross revenue. Although deductions continue to exist, the definition of net revenue has been modified through the implementation of ASC 606. Developed by the Financial Accounting Standards Board (FASB), this change became effective in 2018. What is the new terminology now employed in the calculation of net patient services revenues? - CORRECT ANSWERSExplicit prices concessions and implicit price concessions Key performance indicators set standards for A/R and provide a method for measuring the control and collection of A/R. What are the two KPIs used to monitor performance related to the production and submission of claims to third party payers and patients (self-pay)? - CORRECT ANSWERSElapsed days from discharge to final bill and elapsed days from final bill to claim/bill submission. Consents are signed as part of the post-services process. - CORRECT ANSWERSTrue **False Patient service costs are calculated in the pre-service process for schedule patients - CORRECT ANSWERS**True False The patient is scheduled and registered for service is a time-of-service activity - CORRECT ANSWERSTrue **False The patient account is monitored for payment is a time-of-service activity - CORRECT ANSWERSTrue **False Case management and discharge planning services are a post-service activty - CORRECT ANSWERSTrue **False Sending the bill electronically to the health plan is a time-of-service activity - CORRECT ANSWERSTrue **False What happens during the post-service stage? - CORRECT ANSWERS**A. Final coding of all services, preparation and submission of claims, payment processing and balance billing and resolution. B. Orders are entered, results are reported, charges are generated, and diagnostic and procedural coding is initiated. C. The encounter record is generated, and the patient and guarantor information is obtained and/or updated as required. D. The focus is on the patient and his/her financial care, in addition to the clinical care provided for the patient. The following statements describe best practices established by the Medical Debt Task Force. Check the box next to the True statements - CORRECT ANSWERS**Educate Patients **Coordinate to avoid duplicate patient contacts Exercise moderate judgement when communicating with providers about scheduled services **Be consistent in key aspects of account resolution Report to healthcare plans when the patient's account is transferred to collection agency **Follow best practices for communication Which option is NOT a main HFMA Healthcare Dollars & Sense® revenue cycle initiative? - CORRECT ANSWERSA. Patient Financial Communications B. Price Transparency C. Medical Account Resolution **D. Process Compliance What is the objective of the HCAHPS initiative? - CORRECT ANSWERS**A. To provide a standardized method for evaluating patients' perspective on hospital care. B. To provide clear communication and good customer service, which will give the provider a competitive edge. C. To conduct evaluations concerning patients' perspective on hospital care. D. To make certain that during registration key information is verified by means of a picture ID and an insurance card. Which option is NOT a department that supports and collaborates with the revenue cycle? - CORRECT ANSWERSA. Information Technology B. Clinical Services C. Finance **D. Assisted Living Services Which option is NOT a continuum of care provider? - CORRECT ANSWERSA. Physician **B. Health Plan Contracting C. Hospice D. Skilled Nursing Facility Which of the following are essential elements of an effective compliance program? - CORRECT ANSWERS**Reasonable methods to achieve compliance with standards, including monitoring systems and hotlines **Established compliance standards and procedures Automatic dismissal of any employee excluded from participation in a federal healthcare program **Designation of a compliance officer employed within the Billing Department **Oversight of personnel by high-level personnel. Annually, the OIG publishes a work plan of compliance issues and objectives that will be focused on throughout the following year. Identify which option is NOT a work plan task mentioned in this course. - CORRECT ANSWERSA. Payments to Physicians for Co-Surgery Procedures B. Denials and Appeals in Medicare Part D C. Medicare Hospital Payments for Claims Involving the Acute- and Post-Acute-Care Transfer Policies **D. Standard Unique Employer Identifier In order to promote the use of correct coding methods on a national basis and prevent payment errors due to improper coding, CMS developed what? - CORRECT ANSWERS**A. The Correct Coding Initiative (CCI) B. The Advance Beneficiary Notice of Noncoverage (ABN) C. The Medicare Secondary Payer (MSP) D. Modifiers Indicate if the activity is described by the appropriate description of the violation involved: - CORRECT ANSWERSTrue - A staff member receives cash in the mail and does not immediately report the case to the manager for special handling. This is an example of financial misconduct False - A mother sees a charge on her hospital bill for a circumcision for a newborn girl. This is an example of falsifying medical records to boost reimbursement. True - A patient access staff member takes several file folders and highlighters home for personal use. This is an example of theft of property. False - A physician documents a fictitious epidural in a patient's medical record in an effort to receive additional payment. This is an example of miscoding claims True - Several unauthorized claims are sent to a health plan with the wrong procedure code. This is an example of overcharging. What do business/organizational ethics represent? - CORRECT ANSWERS**A. Principles and standards by which organizations operate B. A healthcare provider's practices and principles C. An employee's actions influenced by experiences and value system D. The patient privacy standard within healthcare What is the intended outcome of collaborations made through an ACO delivery system? - CORRECT ANSWERS**A. To ensure appropriateness of care, elimination of duplicate services, and prevention of medical errors for a population of patients. B. To create cost-containment provisions to reform the healthcare delivery system. C. To reform the healthcare system into a system that rewards greater value, improves the quality of care and increases efficiency in the delivery of services. D. To provide financial incentives to physicians for reporting quality data to CMS. Which of these statements describes the new methodology for the determination of net patient service revenue: - CORRECT ANSWERSA. Net patient service revenue is defined as the average payment amount for the payer but not recorded until the end of the month processing is completed. B. Gross patient service revenue is recorded as net patient service revenue until such time as all payments are received. **C. Net patient service revenue is defined as the total incurred charges, less the explicit price concession, less any applicable implicit price concession(s) as applied to the specific portfolio of accounts. D. Net patient service revenue is gross revenue minus any contractual adjustments applicable to the account. Any additional adjustments are not recorded until the account reaches a zero balance. E. Net patient service revenue is the sum of the balances of all charges and payments recorded in the accounting period. What are KPIs? - CORRECT ANSWERSA. Benchmarks which are used to compare Key Performance Indicators in an organization to an agreed upon average or expected standard within the same industry. **B. Key performance indicators, which set standards for accounts receivable (A/R) and provide a method of measuring the collection and control of A/R. C. Days in A/R is calculated based on the value of the total accounts receivable on a specific date. D. A component that can divide the accounts receivable into 30, 60, 90, 120 days, and over 120 days categories, based on the date of service/discharge While the highest level of differentiation among patients is scheduled patient vs unscheduled patient, a variety of patient types are routinely identified in both the acute and non-acute settings. Which patient types are typically considered acute care patient types? - CORRECT ANSWERSObservation, newborn, Emergency (ED) Accurate identification of the patient is the first step in the scheduling process. Identifiers used in various combination to achieve accurate patient identification include? - CORRECT ANSWERSFull legal name, date of birth, sex and social security number Pre-registration is defined as: - CORRECT ANSWERSThe collection of demographic information, insurance data, financial information, providing reminders, prep information, and identifying the potential need for financial assistance for scheduled patients. Medicare has unique features not found in other health plan programs. It is government sponsored and financed through taxes and general revenue funds. Which of the following statements accurately describes the various Medicare benefits programs: - CORRECT ANSWERSMedicare Part A provides benefits for inpatient hospital services, skilled nursing care and home health care; Medicare Part B covers outpatient and professional services, Medicare Part C or Medicare Advantage plans are managed care plans combining Part A and Part B Coverages; and Medicare Part D is the prescription drug coverage benefit. Which of the following statements about Medicaid eligibility is not true? - CORRECT ANSWERSMedicaid categories are restricted to children, pregnant women and elderly in nursing homes. Examples of managed care plans include: - CORRECT ANSWERSAll of the above Patient Financial Communications best practices include all of the following activities except: - CORRECT ANSWERSCollecting payment or initiating the process to immediately remove the patient from the service schedule. Which statement includes the required components of an accurate pricing determination? - CORRECT ANSWERSInsurance coverage and benefits, service or test involved, diagnosis and procedure codes, total estimated charges, adjudication calculations based on the patient's benefit package. The value of a robust scheduling and pre-registration process includes all of the following except: - CORRECT ANSWERSIdentification of patients who are likely to be "no shows". Which patients are considered scheduled? - CORRECT ANSWERSA. Observation Patients B. Emergency Department Patients **C. Recurring/Series Patients D. Hospice Care Name the guideline that Medicare established to determine which diagnoses, signs, or symptoms are payable. - CORRECT ANSWERSA. Patient Identifiers **B. Local Coverage Determinations C. Advance Beneficiary Notice D. Scheduling Instructions What is the purpose of insurance verification? - CORRECT ANSWERSA. To identify information that does not have to be collected from the patient. **B. To ensure accuracy of the health plan information. C. To effectively complete the MSP screening process. D. To complete guarantor information if the guarantor is not the patient. Which option is a federally-aided, state-operated program to provide health and long-term care coverage? - CORRECT ANSWERSA. Medicare **B. Medicaid C. Self-Insured Plans D. Liability Coverage Which option is NOT a specific managed care requirement? - CORRECT ANSWERSA. Referrals B. Notification **C. Preferred Provider Organization D. Discharge Planning What is the first component of a pricing determination? - CORRECT ANSWERSA. Identify the service or test involved **B. Verification of the patient's insurance eligibility and benefits C. Inform the patient that physician services are or are not included D. Use a worksheet or other tool for guidance in determining an estimate The correct sequential order of the financial counseling steps for an uninsured patient's surgery case are: - CORRECT ANSWERSGreet patient and give your name Explain organization's financial care approach and patient's financial responsibility Review patient's health plan benefits and status Review anticipated charges and patient's anticipated liability Ask patient to resolve liability by reviewing payment options For uninsured, explain financial assistance options What is the purpose of financial counseling? - CORRECT ANSWERSA. To address the most appropriate ways to conduct financial interactions at every point B. To train staff on how to request payment and conduct conversations **C. To educate the patient on his/her health plan coverage and financial responsibility for healthcare services D. To help the patient understand exactly how a contracted health plan will resolve their benefit package EMTALA prohibits inquiries about health plan or liability payer information if the inquiry will delay examination or treatment. What other requirements apply to the Emergency Department registration work? - CORRECT ANSWERSALL of the above Typical activities which much be performed when an unscheduled patient arrives for service include: - CORRECT ANSWERSIdentification of patient in the MPI or initiation of a new MPI record, insurance verification of eligibility and benefits, managed care screening, medical necessity screening, price estimation and financial counseling to achieve the appropriate account resolution. Case managers are involved from admission with the discharge planning process. The purpose of discharge planning is: - CORRECT ANSWERSTo estimate how long the patient will be in the hospital, identify the expected outcome of the hospitalization and initiate any special requirements for services at or after the time of discharge. The chargemaster is basically a list of services, procedures, room accommodations, supplies, drugs, tests, etc. typically associated with the billing for services rendered to patients. Challenges typically associated with the billing for services rendered to patients. Challenges typically associated with the chargemaster include: - CORRECT ANSWERSOmission of charges, obsolete or invalid codes, and the omission of required modifiers. Ultimately, the services provided in the healthcare system are reduced to standard codes. The primary types of coding systems currently used in healthcare are: - CORRECT ANSWERSICD-10-CM/ICD-10-PCS; CPT/HCPCS codes There are four code sets that provide health plans with additional information as they process claims. Those code sets are: - CORRECT ANSWERSCondition codes, occurrence codes, occurrence span codes and value codes Each type of service has unique billing rules which come into play during the provision of service. For the skilled nursing facility, care is covered if which of the following factors are present: - CORRECT ANSWERSThe patient required skilled services on a daily basis and those services can only be provided on an inpatient basis in a SNF. DRG's are a system of classifying inpatients on the basis of diagnoses, procedures, and co-morbidities for purposes of payment to hospitals. Each DRG includes: - CORRECT ANSWERSA relative weight which is multiplied by the established base payment rate to calculate the reimbursement for a specific DRG. For exceptionally costly cases over a set dollar amount, an outlier payment is added to the calculated payment. PPO networks represent one form of discounting commonly used by commercial payers. The silent PPO represents: - CORRECT ANSWERSA discounting scheme whereby health plans apply generic PPO rates to discount a provider's claims, even though there is no contractual arrangement between the silent PPO and the provider. The concept of timely filing of claims is important to providers, payers and patients. Thus, providers are required to comply with timely claim filing rules. Which of the following statements are NOT true about timely filing limitations: - CORRECT ANSWERSPayers will waive timely filing denials for claims filed over a year from date of service. What does EMTALA require hospitals to do? - CORRECT ANSWERS**A. To provide a medical screening examination and stabilizing treatment to every person presenting at an ED and requesting medical evaluation or treatment. B. To initially triage patients, where a "quick" registration record is generated to specifically allow order entry. C. To complete a standardized form signed by all patients that is used to inform the patient about the admission and conditions which must be agreed upon. D. To confirm information that may be used to identify the patient in the provider's MPI, which includes the patient's full, legal name, SSN, and/or date of birth. In what manner do case managers assist revenue cycle staff? - CORRECT ANSWERSA. By reviewing a patient's individual case and recommend treatment changes. B. With monitoring the progression of high resource consumptive cases. C. By estimating how long the patient will be in the hospital and what the expected outcome will be. **D. Providing assistance with written appeals to health plans related to utilization and other care issues. Why is it critical that a chargemaster is reviewed and updated regularly? - CORRECT ANSWERS**A. To ensure it supports and represents the services provided within the organization. B. To ensure the most appropriate measure of the utilization of resources. C. So the CPT databases can have the most current and accurate information. D. Because charge descriptions can vary greatly between providers. What is the responsibility of HIM? - CORRECT ANSWERS**A. To maintain all patient medical records B. To make information available instantly and securely to authorized users C. To denote the medical procedures performed by a healthcare provider on a patient D. To substantiate health insurance claims filed by the patient, the physician, and the provider What are claim edits? - CORRECT ANSWERSA. Various data sources including Medicare and Medicaid bulletins and manuals, individual health plan manuals B. A multi-stakeholder collaboration of more than 130 organizations — providers, health plans, vendors, and government agencies **C. Rules developed to verify the accuracy and completeness of claims based on each health plan's policies D. The submission, receipt, and processing of automated claims, thereby eliminating mail time and reducing data entry time Which statement is NOT a unique billing rule specific to providers? - CORRECT ANSWERSA. Overall aggregate payments made to a hospice are subject to a "cap amount", calculated by the MAC at the end of the hospice cap period. B. With the exception of physician services, Medicare reimbursement for hospice care is made at one of four pre-determined rates for each day of hospice care. C. When billing services on a UB-04/837-I, specific CPT codes are collapsed into a single revenue code (520 or 521). **D. A patient may be balance billed for whatever amount the non-contracting physician charges above the health plan's reimbursement amount. Which of the following statements does not apply to billing during the COVID-19 public health emergency: - CORRECT ANSWERSA. Hospitals may change a sub-acute unit into an acute care unit without advanced approval from CMS. **B. Telemedicine claims are not payable if the patient conducts the telemedicine visit from home. C. CMS developed the concept of hospitals without walls to increase ICU and med-surge inpatient capacity during the COVID-19 pandemic. D. Cost sharing has been waived for testing for COVID-19 in the ED, physician office, urgent care center or other ambulatory location. What is the sequential order for a Silent PPO scheme? - CORRECT ANSWERSThe patient's claims is sent to the listed primary insurance carrier The patient's insurance company (a silent PPO) runs the healthcare provider's tax ID number through a PPO discount database or provides a repricing company a copy of the claim After a successful "hit", the claim is "re-priced" based on the PPO discounts that were accessed. After applying the discount, the silent PPO states on the EOB that the healthcare provider agreed to reduce your bill based on your contract with the PPO The medical provider accepts the health plan's statement on the EOB and writes the discount off-never knowing that the discount was invalid. Which concept is NOT a contracted payment model? - CORRECT ANSWERS**A. Stop-Loss Provision B. Percentage Discount C. Per Diem Payment D. Capitation Credit balances may be created by any of the following activities except: - CORRECT ANSWERSCredits to pharmacy charges posted before the claim final bills Which of the following statements represent common reasons for inpatient claim denials? - CORRECT ANSWERSFailure to obtain a required pre-authorization; failure to complete a continued stay authorization and services provided which were not medically necessary. A 68 year old patient, a Medicare beneficiary, was in a car accident. A medical insurance claim was filed with the auto insurance carrier. Six months later this claim remains unpaid. How can the provider pursue payment from Medicare? - CORRECT ANSWERSThe provider must first bill the auto insurer; however, after a period of 120 days, if the claim remains unpaid, the provider may cancel the liability claim and bill Medicare. The difference between bad debt and financial assistance (charity) is: - CORRECT ANSWERSBad debt represents a refusal to pay; charity represents an inability to pay In order to qualify for financial assistance, a patient or guarantor should: - CORRECT ANSWERSProvide the following documents: prior year tax return, employment check stubs from the prior three months and bank statements for the prior three months. To comply with the requirements of Section 501(r) for tax-exempt hospitals chartered as 510(c)3 providers, the hospital must complete which of the following activities: - CORRECT ANSWERSA community needs assessmenets The three types of bankruptcy as defined in the 1979 Bankruptcy Act are: - CORRECT ANSWERSChapter 7 - Straight Bankruptcy, Chapter 11- Debtor Reorganization and Chapter 13- Debtor Rehabilitation Which of the following medical debt collection practices are recommended as part of HFMA's Best Practices for medical account resolution: - CORRECT ANSWERSEstablish policies and ensure that they are followed Organizations may opt to contract with or outsource to specific vendors for some or all components of revenue cycle processing. This practice has both advantages and disadvantages. Which of the following statements is NOT an advantage of utilizing an outsourcing vendor? - CORRECT ANSWERSThe need for legal review if the outside vendor's staff represents themselves as employees of the healthcare facility. Each hospital covered by the 501(r) regulations is required to develop a financial assistance policy. Which of the following elements is NOT a required element of the policy? - CORRECT ANSWERSThe notice that individuals eligible for financial assistance under this policy may be charged more that the amount generally billed (AGB) to insured patients. Place the daily reconciliation process steps in the correct sequential order: - CORRECT ANSWERSObtain totals of all payments - cash, check, credit card, and debit card Divide remittances into batches and obtain a second total of the electronic remittance advices by payment and contractual allowances Endorse checks immediately. Prepare the bank deposit for all payments. Separate cash payments and contractual adjustments into separate batches and use separate payments and adjustment codes. Post unidentified payments to an unidentified cash account (deposit everything, do not hold unidentified payments) Balance and post batches. Balance payments to the bank deposit. Balance the bank deposit to the general ledger. Sue Smith came into the hospital. Her insurance provider sent an EFT directly into the hospital's account at the bank. John, the hospital representative, receives an electronic Level 2 ERA. What should he do next? - CORRECT ANSWERS**A. Manually match the ERA to the patient account. B. Nothing unless there is an error. What is EFT? - CORRECT ANSWERS**A. The electronic transfer of funds from payer to payee through the banking system. B. The establishment of internal audits by personnel outside the involved department. C. A standardized healthcare claim payment/advice known as the 835 format. D. A process that requires the separation of duties when processing patient payments. Which statement is false regarding credit balances? - CORRECT ANSWERSA. A small credit policy should be matched by a similar policy for small debit balances. B. Tracking reports should be developed to identify internal charge credits versus external charge credits. C. Hospital generated statements should be sent to patients regarding small credit balances. **D. There are no CMS hospital compliance requirements regarding credit balances. Which option is NOT a type of denial? - CORRECT ANSWERSA. Technical B. Clinical C. Underpayment **D. Contractual Adjustment Which option is NOT a lien type? - CORRECT ANSWERSA. Judicial **B. Subrogation C. Statutory D. Agreement (Consensus) Based on what you have just read, which activity is not considered when initiating self-pay follow-up and account resolution activities? - CORRECT ANSWERSA. Poverty Guidelines B. Financial Profile C. Presumptive Financial Assistance Determination **D. Patient Open Balance Billing Which option is NOT a required component of a FAP? - CORRECT ANSWERSA. Eligibility criteria B. Application process C. Application assistance **D. Out-of-network providers Which option is NOT a bankruptcy type governed by the 1979 Bankruptcy Act? - CORRECT ANSWERSA. Straight bankruptcy B. Debtor reorganization **C. Creditor priority D. Debtor rehabilitation Which evaluation criteria demonstrates reputation expectations: - CORRECT ANSWERSA. The agency's Yelp score and consumer comments. B. The amount of monies collected monthly. **C. The employment of staff who have documented experience working in financial areas of health care. D. The high turnover rate for entry level employees. Agency fees are: - CORRECT ANSWERSA. Paid by patients. **B. The cost to the provider for collection agency monies offset by the return on baddebt accounts. C. Only reported annually to the provider. D. Waived for accounts aged greater than one year from date of service. The correct way to handle the retention and payment of agency fees is: - CORRECT ANSWERSA. The agency provides an annual settlement of monies received by the health care provider and the agency. B. Compare estimated collection costs to actual costs incurred. C. Validate bank deposits weekly as funds are received from the agency. **D. Follow the contractual agreement between the agency and the provider as to how monies sent to the agency will be handled. Patient relations include: - CORRECT ANSWERS**A. The ability to sensitively deal with patients or individuals while managing collection efficiency. B. Applying hard-core techniques to collect monies owed regardless of what the patient or individual states during the call. C. Ignoring all patient complaint calls. D. Referring all patient complaint calls to the healthcare provider. Collection agency reports should be provided: - CORRECT ANSWERSA. Whenever staff have the time to generate them. B. Whenever an account is cancelled. **C. In at least two formats regarding accounts assigned on a routine basis. D. As needed to prove recovery rates. Collection results are: - CORRECT ANSWERSA. Always guaranteed by the collection agency. **B. Accurately calculated to demonstrate the actual recovery percentage rate. C. Calculated using agency's private formula. D. Never reported except during contract negotiations. Which option is NOT a HFMA best practice? - CORRECT ANSWERSA. Coordinate the resolution of bad debt accounts with a law firm B. Establish policies and ensure that they are followed NOT - C. Coordinate account resolution activities with business affiliates D. Report back to credit bureaus when an account is resolved True or False: The following statement represents an advantage of outsourcing: Access to qualified staff - CORRECT ANSWERS**True False True or False: The following statement represents an advantage of outsourcing: Vendor absorbs some financial risk based on "efficiency" factor - CORRECT ANSWERS**True False True or False: The following statement represents an advantage of outsourcing: Impact on direct control of accounts receivable - CORRECT ANSWERSTrue **False True or False: The following statement represents an advantage of outsourcing: Capitalizes on the economies of scale - CORRECT ANSWERS**True False True or False: The following statement represents an advantage of outsourcing: Limits internal staffing requirements - CORRECT ANSWERS**True False True or False: The following statement represents an advantage of outsourcing: Impact on customer service - CORRECT ANSWERSTrue **False True or False: The following statement represents an advantage of outsourcing: Legal impact if vendor represents themselves as provider employees - CORRECT ANSWERSTrue **False True or False: The following statement represents an advantage of outsourcing: Ineffective vendor results in increased costs - CORRECT ANSWERSTrue **False ABC Hospital has experienced a 16% increase in new patients over the past 6 months. The hospital is understaffed in its insurance claim and payment processing department and cannot handle this increase in work load. It is considering hiring an outsourcing vendor to assist. What are the steps that the hospital needs to take to establish and ensure a successful vendor relationship? - CORRECT ANSWERS**A. Distribute a RFP to solicit vendor capabilities, evaluate vendor's expertise to provide outsourcing services, visit vendor locations, perform vendor reference checks, talk with vendor clients, interview vendor employees to assess experience level. B. Evaluate vendor's expertise in providing outsourcing services, visit vendor locations, interview vendor employees to assess expertise level. Which function within the revenue cycle is NOT a good candidate for outsourcing? - CORRECT ANSWERS**A. Health Care Patient Services B. Patient Accounting C. Patient Access D. Health Information Management [Show More]
Last updated: 2 years ago
Preview 1 out of 87 pages
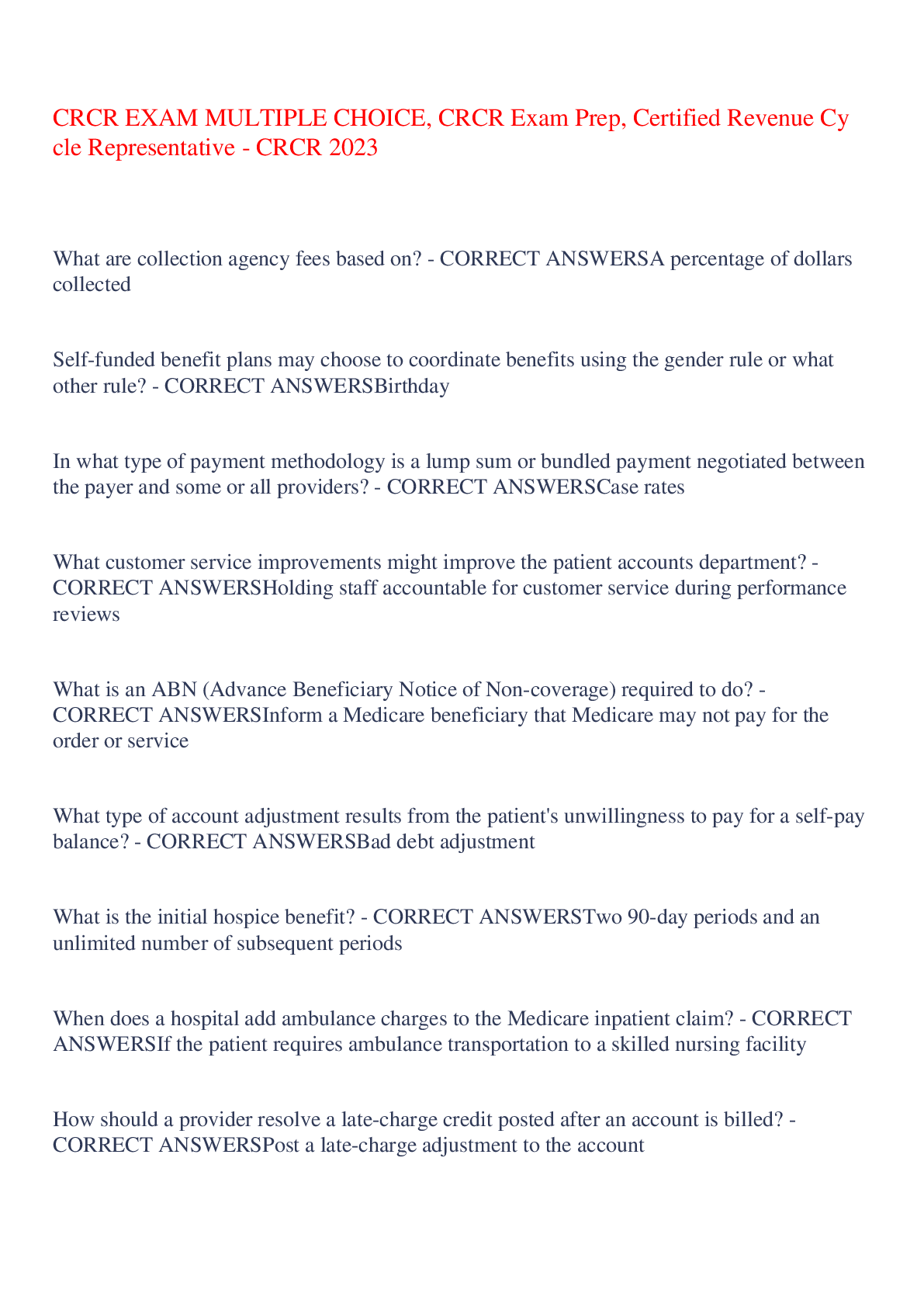
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$14.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Apr 22, 2023
Number of pages
87
Written in
Additional information
This document has been written for:
Uploaded
Apr 22, 2023
Downloads
0
Views
65