*NURSING > SHADOW HEALTH > Shadow Health Gastrointestinal Documentation (All)
Shadow Health Gastrointestinal Documentation
Document Content and Description Below
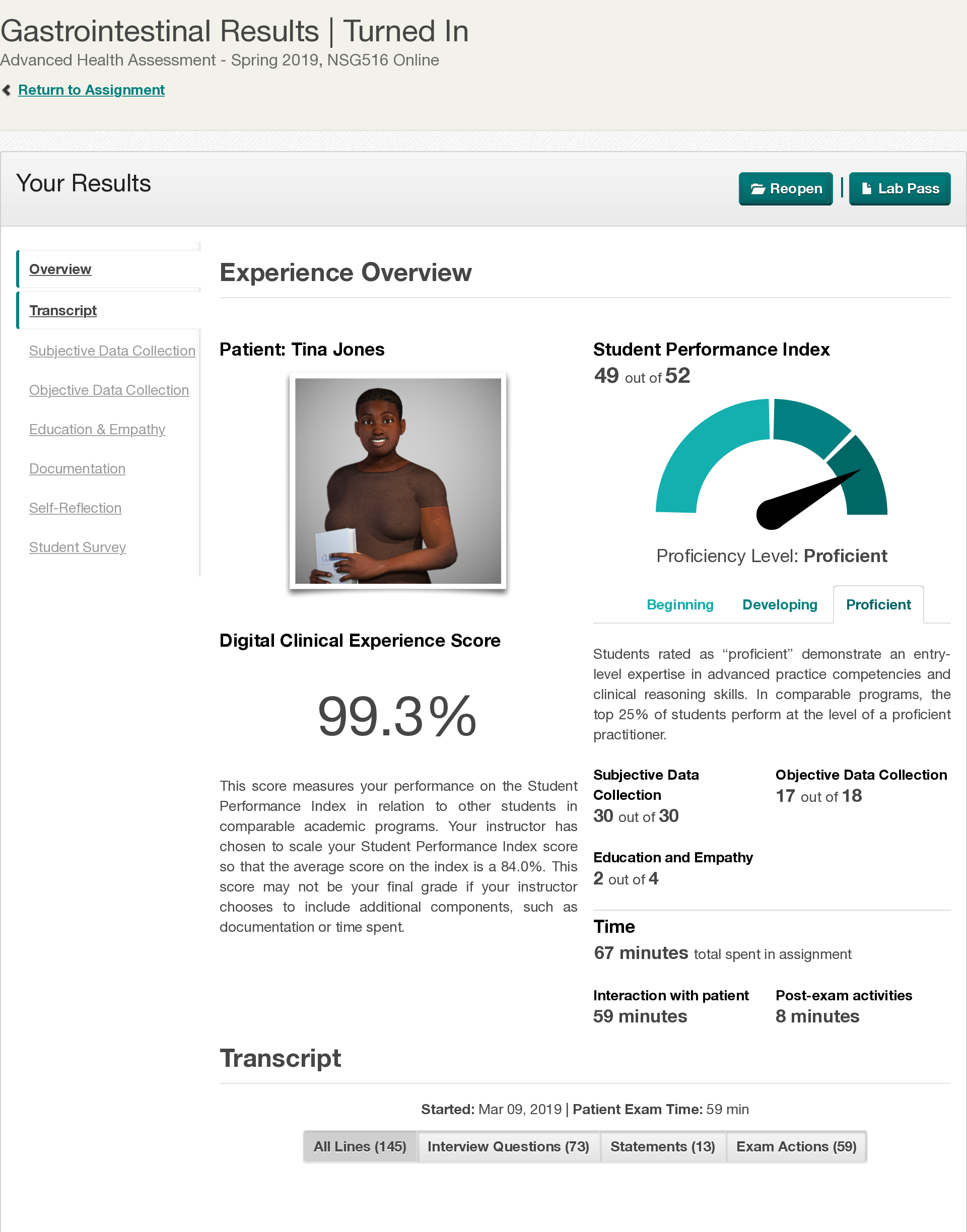
Shadow Health Gastrointestinal Documentation Documentation / Electronic Health Record • Document: Provider Notes Document: Provider Notes Student Documentation Model Documentation HPI: Ms. Jon... es is a pleasant 28-year-old African American woman who presented to the clinic with complaints of upper stomach pain after eating. She noticed the pain about a month ago. She states that she experiences pain daily, but notes it to be worse 3-4 times per week. Pain is a 5/10 and is located in her upper stomach. She describes it “kind of like heartburn” but states that it can be sharper. She notes it to increase with consumption of food and specifically fast food and spicy food make pain worse. She does notice that she has increased burping after meals. She states that time generally makes the pain better, but notes that she does treat the pain “every few days” with an over the counter antacid with some relief. Social History: She denies any specific changes in her diet recently, but notes that she has increased her water intake. Breakfast is usually a muffin or pumpkin bread, lunch is a sandwich with chips, dinner is a homemade meal of a meat and vegetable, snacks are French fries or pretzels. She denies coffee intake, but does drink diet cola on a regular basis. She denies use of tobacco and illicit drugs. She drinks alcohol occasionally, last was 2 weeks ago, and was 1 drink. She does not exercise. Review of Systems: General: Denies changes in weight and general fatigue. She denies fevers, chills, and night sweats. • Cardiac: Denies a diagnosis of hypertension, but states that she has been told her blood pressure was high in the past. She denies known history of murmurs, dyspnea on exertion, orthopnea, paroxysmal nocturnal dyspnea, or edema. • Respiratory: She denies shortness of breath, wheezing, cough, sputum, hemoptysis, pneumonia, bronchitis, emphysema, tuberculosis. She has a history of asthma, last hospitalization was age 16, last chest XR was age 16. • Gastrointestinal: States that in general her appetite is unchanged, although she does note that she will occasionally experience loss of appetite in anticipation of the pain associated with eating. Denies nausea, vomiting, diarrhea, and constipation. Bowel movements are daily and generally brown in color. Denies any change in stool color, consistency, or frequency. Denies blood in stool, dark stools, or maroon stools. No blood in emesis. No known jaundice, problems with liver or spleen. Objective Ms. Jones is a pleasant, alert and oriented 28-year-old African American woman. Cardiovascular: S1, S2 present. No bruits over abdominal aorta, femoral, iliac, or renal with auscultation. Respiratory: Lung sounds clear to anteriourly and posteriorly presents all areas. No adventitious sound noted. Gastrointestinal: symmetric, protuberant, no visible abnormalities noted. Bowel sounds present and normaoactive in all quadrants. Tympanic sounds throughout abdomen, and spleen area. No CVA tenderness noted. No tenderness to light or deep palpation. Liver palpable. The spleen and bilateral kidneys are not palpable. General: Ms. Jones is a pleasant, obese 28-year-old African American woman in no acute distress. She is alert and oriented. She maintains eye contact throughout interview and examination. • Abdominal: Abdomen is soft and protuberant without scars or skin lesions; skin is warm and dry, without tenting. Bowel sounds present and normoactive in all quadrants. No tenderness to light or deep palpation. Tympanic throughout. Liver is 7 cm at the MCL and 1 cm below the right costal margin. Spleen and bilateral kidneys are not palpable. No CVA tenderness. • Cardiovascular: Regular rate and rhythm, S1 and S2 present, no murmurs, rubs, gallops, clicks, precordial movements. No bruits with auscultation over abdominal aorta. No femoral, iliac, or renal bruits. • Respiratory: Chest is symmetrical with respirations. Lung sounds clear to auscultation anteriorly and posteriorly without wheezes, crackles, or cough. Assessment Gastroesophageal reflux disease Differential diagnosis as cardiac disease, pregnancy, cholelithasis, pancreatitis, peptic ulcer disease, esophageal spasm, pulmonary edema. Gastroesophageal reflux disease without evidence of esophagitis ……………………………………..CONTINUED………………………… [Show More]
Last updated: 2 years ago
Preview 1 out of 3 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$7.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Feb 08, 2021
Number of pages
3
Written in
Additional information
This document has been written for:
Uploaded
Feb 08, 2021
Downloads
0
Views
264