● GERD
○ What is it?
■ Gastric juices move up into the esophagus due to:
■ Weak LES (lower esophageal sphincter) opens and closes when
eating or drinking if not should be closed
■ Pressure changes after meals, pregn
...
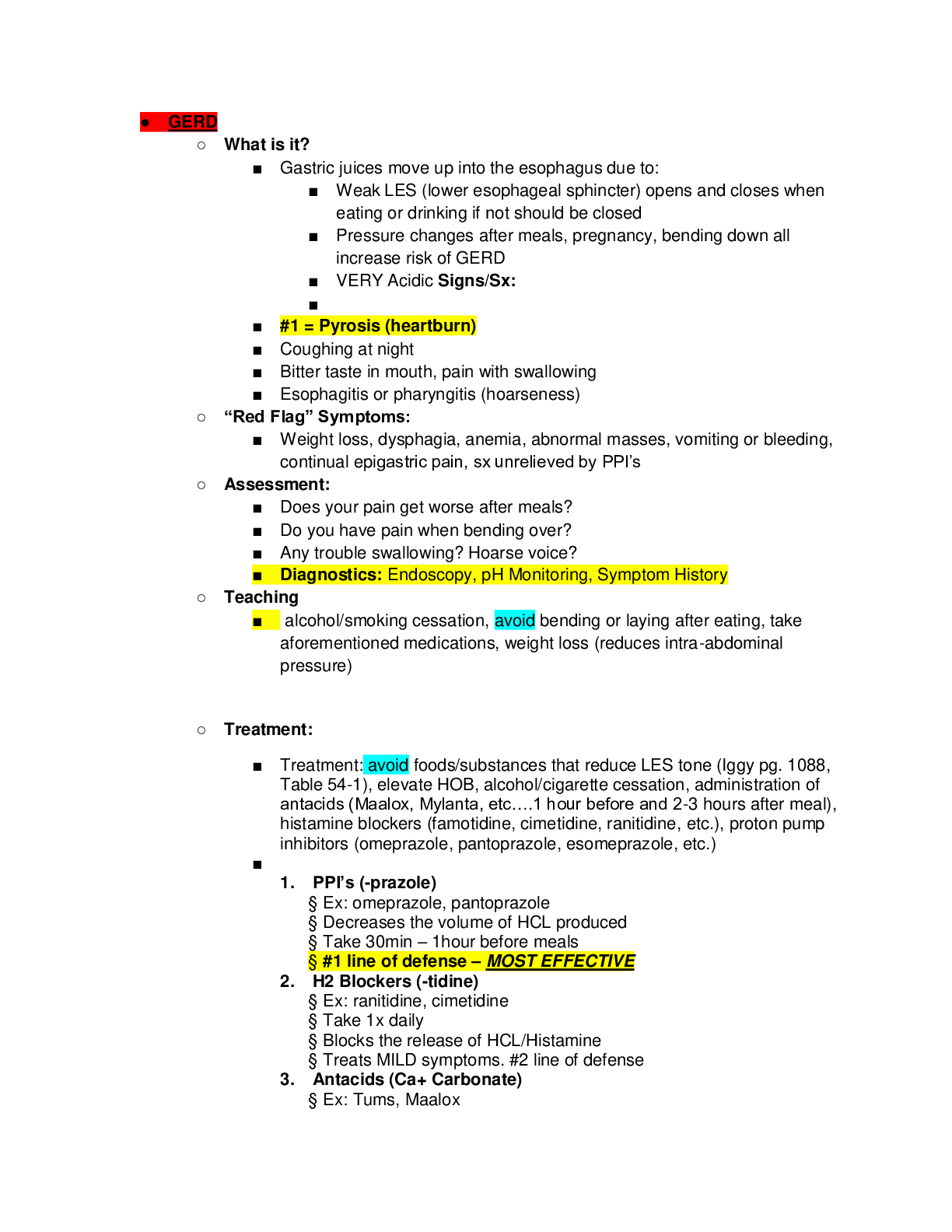
● GERD
○ What is it?
■ Gastric juices move up into the esophagus due to:
■ Weak LES (lower esophageal sphincter) opens and closes when
eating or drinking if not should be closed
■ Pressure changes after meals, pregnancy, bending down all
increase risk of GERD
■ VERY Acidic Signs/Sx:
■
■ #1 = Pyrosis (heartburn)
■ Coughing at night
■ Bitter taste in mouth, pain with swallowing
■ Esophagitis or pharyngitis (hoarseness)
○ “Red Flag” Symptoms:
■ Weight loss, dysphagia, anemia, abnormal masses, vomiting or bleeding,
continual epigastric pain, sx unrelieved by PPI’s
○ Assessment:
■ Does your pain get worse after meals?
■ Do you have pain when bending over?
■ Any trouble swallowing? Hoarse voice?
■ Diagnostics: Endoscopy, pH Monitoring, Symptom History
○ Teaching
■ alcohol/smoking cessation, avoid bending or laying after eating, take
aforementioned medications, weight loss (reduces intra-abdominal
pressure)
○ Treatment:
■ Treatment: avoid foods/substances that reduce LES tone (Iggy pg. 1088,
Table 54-1), elevate HOB, alcohol/cigarette cessation, administration of
antacids (Maalox, Mylanta, etc….1 hour before and 2-3 hours after meal),
histamine blockers (famotidine, cimetidine, ranitidine, etc.), proton pump
inhibitors (omeprazole, pantoprazole, esomeprazole, etc.)
■
1. PPI’s (-prazole)
§ Ex: omeprazole, pantoprazole
§ Decreases the volume of HCL produced
§ Take 30min – 1hour before meals
§ #1 line of defense – MOST EFFECTIVE
2. H2 Blockers (-tidine)
§ Ex: ranitidine, cimetidine
§ Take 1x daily
§ Blocks the release of HCL/Histamine
§ Treats MILD symptoms. #2 line of defense
3. Antacids (Ca+ Carbonate)
§ Ex: Tums, Maalox
§ Neutralizes stomach acid
§ Monitor for signs of Metabolic Alkalosis
4. Surgery
§ “Anti-Reflux Surgery” to tighten LES sphincter
§ “Nissen fundoplication” (more invasive surgery)
● Hiatal Hernia
○ Causes:
■ Part of the stomach protrudes through the esophageal hiatus/diaphragm.
■ Obesity, pregnancy, overeating, age (anything that puts extra pressure on
the diaphragm or that weakens it)
○ Signs/Sx:
■ GERD symptoms are common, otherwise patient is asymptomatic
■ Most common complaint is Pyrosis (heartburn)
○ Tests
■ Barium Swallow (barium + applesauce are swallowed and then patient is
monitored via fluoroscopy. If hernia is present, the barium will pool in the
out-pouching).
■ Fluoroscopy: continuous x-ray done to see if aspiration/deviation
occurs when eating or drinking
■ Upper Endoscopy (you can visually see the out-pouching with scope
inserted into the esophagus)
○ Treatment:
■ Treat GERD
■ Surgery (surgical repair)
○ Patient Education:
■ Avoid eating 2-3 hours before bed/laying down
■ Avoid straining,
■ Elevate HOB 8-12 in when sleeping
■ Avoid alcohol/caffeine/smoking/NSAIDS
■ Eat small meals (don’t overeat)
■ STOP: smoking, ETOH, caffeine, acidic foods, avoid NSAIDS
● ESOPHAGEAL CANCER
○ Highest cancer mortality rate (15% after 5 years) with two main types:
■ Adenocarcinoma- risk factors include smoking, chronic GERD, Barrett’s
esophagus
■ Squamous cell carcinoma- risk factors include smoking, alcohol ingestion,
ingestion of lye, Fanconi’s anemia
○ Signs/Sx:
■ persistent and progressive dysphagia, severe chest/abdominal pain,
regurgitation, hoarseness, anorexia, N/V, weight loss
○ Treatment
■ based on staging of the cancer, would be palliative or curative. Could
include esophagectomy or endoscopic mucosal resection. If metastasis
has occurred, chemo/radiation would be done prior to surgery.
● DYSPHAGIA
○ Difficulty swallowing is a major concern in the older adult as well as the majority
of stroke sufferers
○ Assessment:
■ difficulty swallowing liquids or solids, coughing after eating or drinking,
recurrent pulmonary infections, difficulty with speech (dysphonia) that
could indicate a motor dysfunction
○ Testing
■ Barium swallow- patient swallows a radioactive dye that can show areas
of dysfunction during swallowing
■ Endoscopic evaluation
○ Nursing Management:
■ thickened liquids/foods, HOB 30-45 degrees
○ Depending on the type and severity of dysphagia there are some surgical
interventions that can be done to treat the condition
● Peptic Ulcer Disease (PUD)
○ What is it?
■ Caused by dyspepsia (indigestion) which erodes the mucosal lining of the
stomach/duodenum
■ #1 cause = H. pylori
■ #2 cause = NSAIDs on empty stomach
■ Smoking, alcohol, family hx
○ Signs/Sx:
■ #1 Symptom = Burning/abdominal pain
■ Burning pain is often relieved by eating or antacids
■ Pain wakes patient up in the middle of the night
■ Bloating, pain in middle of night, weight loss, poor appetite
■ Worse if stomach is empty
○ Tests:
■ Endoscopy
■ H. pylori testing
○ Treatment:
■ OTC Antacids (risks: hypercalcemia, metabolic alkalosis, diarrhea,
constipation, Na+ overload
■ PPI’s, H2 Blockers, Metronidazole (Flagyl), Tetracycline (pg. 1359 in
book)
■ Cryoprotective agent: Sucralfate
■ Coats stomach & forms a barrier allowing the ulcer time to heal.
■ Take on empty stomach 1-2 hours before meals or 2 hours after
meal.
■ Risk: makes it harder for your body to absorb other medications
due to the coating on the stomach wall
[Show More]