NURSING 212 Test banks Exam 2 potter and perry ,100% CORRECT
Document Content and Description Below
1. Which nurse most likely kept records on sanitation techniques and the effects on health? a. Florence Nightingale b. Mary Nutting c. Clara Barton d. Lillian Wald ANS: A Nightingale was the fir... st practicing nurse epidemiologist. Her statistical analyses connected poor sanitation with cholera and dysentery. Mary Nutting, Clara Barton, and Lillian Wald came after Nightingale, each contributing to the nursing profession in her own way. Mary Nutting was instrumental in moving nursing education into universities. Clara Barton founded the American Red Cross. Lillian Wald helped open the Henry Street Settlement. DIF:Understand (comprehension)REF:5 OBJ: Discuss the influence of social, historical, political, and economic changes on nursing practices. TOP: Evaluation MSC: Health Promotion and Maintenance 2. The nurse prescribes strategies and alternatives to attain expected outcome. Which standard of nursing practice is the nurse following? a. Assessment b. Diagnosis c. Planning d. Implementation ANS: C In planning, the registered nurse develops a plan that prescribes strategies and alternatives to attain expected outcomes. During assessment, the registered nurse collects comprehensive data pertinent to the patient’s health and/or the situation. In diagnosis, the registered nurse analyzes the assessment data to determine the diagnoses or issues. During implementation, the registered nurse implements (carries out) the identified plan. DIF:Understand (comprehension)REF:2 OBJ: Discuss the development of professional nursing roles. TOP: Planning MSC:Management of Care 3. An experienced medical-surgical nurse chooses to work in obstetrics. Which level of proficiency is the nurse upon initial transition to the obstetrical floor? a. Novice b. Proficient c. Competent d. Advanced beginner ANS: A A beginning nursing student or any nurse entering a situation in which there is no previous level of experience (e.g., an experienced operating room nurse chooses to now practice in home health) is an example of a novice nurse. A proficient nurse perceives a patient’s clinical situation as a whole, is able to assess an entire situation, and can readily transfer knowledge gained from multiple previous experiences to a situation. A competent nurse understands the organization and specific care required by the type of patients (e.g., surgical, oncology, or orthopedic patients). This nurse is a competent practitioner who is able to anticipate nursing care and establish long-range goals. A nurse who has had some level of experience with the situation is an advanced beginner. This experience may only be observational in nature, but the nurse is able to identify meaningful aspects or principles of nursing care. DIF:Apply (application)REF:2 OBJ: Discuss the development of professional nursing roles. TOP: Evaluation MSC:Management of Care 4. A nurse assesses a patient’s fluid status and decides that the patient needs to drink more fluids. The nurse then encourages the patient to drink more fluids. Which concept is the nurse demonstrating? a. Licensure b. Autonomy c. Certification d. Accountability ANS: B Autonomy is an essential element of professional nursing that involves the initiation of independent nursing interventions without medical orders. To obtain licensure in the United States, the RN candidate must pass the NCLEX-RN®. Beyond the NCLEX-RN®, the nurse may choose to work toward certification in a specific area of nursing practice. Accountability means that you are responsible, professionally and legally, for the type and quality of nursing care provided. DIF:Apply (application)REF:3 OBJ: Discuss the roles and career opportunities for nurses. TOP: Implementation MSC:Management of Care 5. A nurse prepares the budget and policies for an intensive care unit. Which role is the nurse implementing? a. Educator b. Manager c. Advocate d. Caregiver ANS: B A manager coordinates the activities of members of the nursing staff in delivering nursing care and has personnel, policy, and budgetary responsibility for a specific nursing unit or facility. As an educator, you explain concepts and facts about health, describe the reason for routine care activities, demonstrate procedures such as self-care activities, reinforce learning or patient behavior, and evaluate the patient’s progress in learning. As a patient advocate, you protect your patient’s human and legal rights and provide assistance in asserting these rights if the need arises. As a caregiver, you help patients maintain and regain health, manage disease and symptoms, and attain a maximal level function and independence through the healing process. DIF:Apply (application)REF:4 OBJ: Describe the roles and career opportunities for nurses. TOP: Implementation MSC:Management of Care 6. The nurse has been working in the clinical setting for several years as an advanced practice nurse. However, the nurse has a strong desire to pursue research and theory development. To fulfill this desire, which program should the nurse attend? a. Doctor of Nursing Science degree (DNSc) b. Doctor of Philosophy degree (PhD) c. Doctor of Nursing Practice degree (DNP) d. Doctor in the Science of Nursing degree (DSN) ANS: B Some doctoral programs prepare nurses for more rigorous research and theory development and award the research-oriented Doctor of Philosophy (PhD) in nursing. Professional doctoral programs in nursing (DSN or DNSc) prepare graduates to apply research findings to clinical nursing. The DNP is a practice doctorate that prepares advanced practice nurses such as nurse practitioners. DIF:Understand (comprehension)REF:10 OBJ: Describe educational programs available for professional registered nurse (RN) education. TOP:Teaching/LearningMSC:Management of Care 7. A nurse attends a workshop on current nursing issues provided by the American Nurses Association. Which type of education did the nurse receive? a. Graduate education b. Inservice education c. Continuing education d. Registered nurse education ANS: C Continuing education involves formal, organized educational programs offered by universities, hospitals, state nurses associations, professional nursing organizations, and educational and health care institutions. After obtaining a baccalaureate degree in nursing, you can pursue graduate education leading to a master’s or doctoral degree in any number of graduate fields, including nursing. Inservice education programs are instruction or training provided by a health care facility or institution. Registered nurse education is the education preparation for an individual intending to be an RN. DIF:Apply (application)REF:10 OBJ: Describe educational programs available for professional registered nurse (RN) education. TOP:Teaching/LearningMSC:Management of Care 8. A nurse identifies gaps between local and best practices. Which Quality and Safety Education for Nurses (QSEN) competency is the nurse demonstrating? a. Safety b. Patient-centered care c. Quality improvement d. Teamwork and collaboration ANS: C Quality improvement identifies gaps between local and best practices. Safety minimizes risk of harm to patients and providers through both system effectiveness and individual performance. Patient-centered care recognizes the patient or designee as the source of control and full partner in providing compassionate and coordinated care based on respect for patient’s preferences, values, and needs. Teamwork and collaboration allows effective functioning within nursing and interprofessional teams, fostering open communication, mutual respect, and shared decision making. DIF:Understand (comprehension)REF:7 | 8 OBJ: Describe the roles and career opportunities for nurses. TOP: Evaluation MSC:Management of Care 9. A nurse has compassion fatigue. What is the nurse experiencing? a. Lateral violence and intrapersonal conflict b. Burnout and secondary traumatic stress c. Short-term grief and single stressor d. Physical and mental exhaustion ANS: B Compassion fatigue is a term used to describe a state of burnout and secondary traumatic stress. Compassion fatigue may contribute to what is described as lateral violence (nurse-nurse interactions, not intrapersonal). Frequent, intense, or prolonged exposure to grief and loss places nurses at risk for developing compassion fatigue. Stressors, not a single stressor, contribute to compassion fatigue. Physical and mental exhaustion describes burnout only. DIF:Understand (comprehension)REF:6 OBJ: Discuss the influence of social, historical, political, and economic changes on nursing practices. TOP: Assessment MSC: Health Promotion and Maintenance 10. A patient is scheduled for surgery. When getting ready to obtain the informed consent, the patient tells the nurse, “I have no idea what is going to happen. I couldn’t ask any questions.” The nurse does not allow the patient to sign the permit and notifies the health care provider of the situation. Which role is the nurse displaying? a. Manager b. Patient educator c. Patient advocate d. Clinical nurse specialist ANS: C As a patient advocate, the nurse protects the patient’s human and legal rights, including the right of the patient to understand procedures before signing permits. Although nurses can be educators, it is the responsibility of the surgeon to provide education for the patient in preparation for surgery, and it is the nurse’s responsibility to notify the health care provider if the patient is not properly educated. Managers coordinate the activities of members of the nursing staff in delivering nursing care, and clinical nurse specialists are experts in a specialized area of nursing practice in a variety of settings. DIF:Apply (application)REF:3 OBJ: Describe the roles and career opportunities for nurses. TOP: Evaluation MSC:Management of Care 11. The patient requires routine gynecological services after giving birth to her son, and while seeing the nurse-midwife, the patient asks for a referral to a pediatrician for the newborn. Which action should the nurse-midwife take initially? a. Provide the referral as requested. b. Offer to provide the newborn care. c. Refer the patient to the supervising provider. d. Tell the patient that is not allowed to make referrals. ANS: B The practice of nurse-midwifery involves providing independent care for women during normal pregnancy, labor, and delivery, as well as care for the newborn. After being apprised of the midwifery role, if the patient insists on seeing a pediatrician, the nurse-midwife should provide the referral. The supervising provider is an obstetric provider, not a pediatrician. A nurse-midwife can make referrals. DIF:Analyze (analysis)REF:4 OBJ: Describe the roles and career opportunities for nurses. TOP: Implementation MSC:Management of Care 12. The nurse has a goal of becoming a certified registered nurse anesthetist (CRNA). Which activity is appropriate for a CRNA? a. Manages gynecological services such as PAP smears b. Works under the guidance of an anesthesiologist c. Obtains a PhD degree in anesthesiology d. Coordinates acute medical conditions ANS: B Nurse anesthetists provide surgical anesthesia under the guidance and supervision of an anesthesiologist, who is a physician (health care provider) with advanced knowledge of surgical anesthesia. Nurse practitioners, not CRNAs, manage self-limiting acute and chronic stable medical conditions; certified nurse-midwives provide gynecological services such as routine Papanicolaou (Pap) smears. The CRNA is an RN with an advanced education in a nurse anesthesia accredited program. A PhD is not a requirement. DIF:Understand (comprehension)REF:4 OBJ: Describe the roles and career opportunities for nurses. TOP: Implementation MSC:Management of Care 13. A nurse teaches a group of nursing students about nurse practice acts. Which information is most important to include in the teaching session about nurse practice acts? a. Protects the nurse b. Protects the public c. Protects the provider d. Protects the hospital ANS: B The nurse practice acts regulate the scope of nursing practice and protect public health, safety, and welfare. They do not protect the nurse, provider, or hospital. DIF:Understand (comprehension)REF:10 OBJ: Discuss the influence of social, historical, political, and economic changes on nursing practices. TOP: Teaching/Learning MSC: Management of Care 14. A bill has been submitted to the State House of Representatives that is designed to reduce the cost of health care by increasing the patient-to-nurse ratio from a maximum of 2:1 in intensive care units to 3:1. What should the nurse realize? a. Legislation is politics beyond the nurse’s control. b. National programs have no bearing on state politics. c. The individual nurse can influence legislative decisions. d. Focusing on nursing care provides the best patient benefit. ANS: C Nurses can influence policy decisions at all governmental levels. One way is to get involved by participating in local and national efforts. This effort is critical in exerting nurses’ influence early in the political process. Legislation is not beyond the nurse’s control. National program can have bearing on state politics. The question is focusing on legislation and health care costs, not nursing care. DIF:Analyze (analysis)REF:9 OBJ:Discuss the influence of social, historical, political, and economic changes on nursing practices.TOP:EvaluationMSC:Management of Care 15. A nurse is using a guide that provides principles of right and wrong to provide care to patients. Which guide is the nurse using? a. Code of ethics b. Standards of practice c. Standards of professional performance d. Quality and safety education for nurses ANS: A The code of ethics is the philosophical ideals of right and wrong that define the principles you will use to provide care to your patients. The Standards of Practice describe a competent level of nursing care. The ANA Standards of Professional Performance describe a competent level of behavior in the professional role. Quality and safety education for nurses addresses the challenge to prepare nurses with the competencies needed to continuously improve the quality of care in their work environments. DIF:Understand (comprehension)REF:3 OBJ: Discuss the influence of social, historical, political, and economic changes on nursing practices. TOP: Implementation MSC: Management of Care 16. A graduate of a baccalaureate degree program is ready to start working as an RN in the emergency department. Which action must the nurse take first? a. Obtain certification for an emergency nurse. b. Pass the National Council Licensure Examination. c. Take a course on genomics to provide competent emergency care. d. Complete the Hospital Consumer Assessment of Healthcare Providers Systems. ANS: B Currently, in the United States, the most common way to become a registered nurse (RN) is through completion of an associate’s degree or baccalaureate degree program. Graduates of both programs are eligible to take the National Council Licensure Examination for Registered Nurses (NCLEX-RN) to become registered nurses in the state in which they will practice. Certification can be obtained after passing the NCLEX and working for the specified amount of time. Genomics is a newer term that describes the study of all the genes in a person and interactions of these genes with one another and with that person’s environment. Consumers can also access Hospital Consumer Assessment of Healthcare Providers Systems (HCAHPS) to obtain information about patients’ perspectives on hospital care. DIF:Remember (knowledge)REF:9 OBJ: Describe educational programs available for professional registered nurse (RN) education. TOP:ImplementationMSC:Management of Care 17. While providing care to a patient, the nurse is responsible, both professionally and legally. Which concept does this describe? a. Autonomy b. Accountability c. Patient advocacy d. Patient education ANS: B Accountability means that the nurse is responsible, professionally and legally, for the type and quality of nursing care provided. Autonomy is an essential element of professional nursing that involves the initiation of independent nursing interventions without medical orders. As a patient advocate, the nurse protects the patient’s human and legal rights and provides assistance in asserting these rights if the need arises. As an educator, the nurse explains concepts and facts about health, describes the reasons for routine care activities, demonstrates procedures such as self-care activities, reinforces learning or patient behavior, and evaluates the patient’s progress in learning. DIF:Remember (knowledge)REF:3 OBJ:Discuss the influence of social, historical, political, and economic changes on nursing practices.TOP:EvaluationMSC:Management of Care 18. A nurse is teaching the staff about Benner’s levels of proficiency. In which order should the nurse place the levels from beginning level to ending level? 1. Expert 2. Novice 3. Proficient 4. Competent 5. Advanced beginner a. 2, 4, 5, 1, 3 b. 2, 5, 4, 3, 1 c. 4, 2, 5, 3, 1 d. 4, 5, 2, 1, 3 ANS: B Benner’s levels of proficiency are as follows: novice, advanced beginner, competent, proficient, and expert. DIF:Understand (comprehension)REF:2 OBJ: Discuss the development of professional nursing roles. TOP: Teaching/Learning MSC:Management of Care MULTIPLE RESPONSE 1. A nurse is preparing a teaching session about contemporary influences on nursing. Which examples should the nurse include? (Select all that apply.) a. Human rights b. Affordable Care Act c. Demographic changes d. Medically underserved e. Decreasing health care costs ANS: A, B, C, D Multiple external forces affect nursing, including the need for nurses’ self-care, Affordable Care Act (ACA) and rising (not decreasing) health care costs, demographic changes of the population, human rights, and increasing numbers of medically underserved. DIF:Understand (comprehension)REF:6 OBJ: Discuss the influence of social, historical, political, and economic changes on nursing practices. TOP: Teaching/Learning MSC: Management of Care 2. After licensure, the nurse wants to stay current in knowledge and skills. Which programs are the most common ways nurses can do this? (Select all that apply.) a. Master’s degree b. Inservice education c. Doctoral preparation d. Continuing education e. National Council Licensure Examination retakes ANS: B, D Continuing education programs help nurses maintain current nursing skills, gain new knowledge and theory, and obtain new skills reflecting the changes in the health care delivery system. Inservice education programs are provided by a health care facility to increase the knowledge, skills, and competencies of nurses employed by the institution. Both can help the nurse stay current. Master’s degree programs are valuable for those in the role of nurse educator, nurse administrator, or advanced practice nurse. Professional doctoral programs in nursing (DSN or DNSc) prepare graduates to apply research findings to clinical nursing. National Council Licensure Examination retakes are not to keep current; this test is taken to enter RN practice. DIF:Understand (comprehension)REF:10 OBJ: Describe educational programs available for professional registered nurse (RN) education. TOP:Teaching/LearningMSC:Management of Care 3. A nurse wants to become an advanced practice registered nurse. Which options should the nurse consider? (Select all that apply.) a. Patient advocate b. Nurse administrator c. Certified nurse-midwife d. Clinical nurse specialist e. Certified nurse practitioner ANS: C, D, E Although all nurses should function as patient advocates, “advanced practice nurse” is an umbrella term for an advanced clinical nurse such as a certified nurse practitioner, clinical nurse specialist, certified registered nurse anesthetist, or certified nurse-midwife. A nurse administrator is not an example of advanced practice. DIF:Understand (comprehension)REF:4 OBJ: Describe the roles and career opportunities for nurses. TOP: Teaching/Learning MSC:Management of Care 4. The nurse manager from the oncology unit has had two callouts; the orthopedic unit has had multiple discharges and probably will have to cancel one or two of its nurses. The orthopedic unit has agreed to “float” two of its nurses to the oncology unit if oncology can “float” a nursing assistant to the orthopedic unit to help with obtaining vital signs. Which concepts does this situation entail? (Select all that apply.) a. Autonomy b. Informatics c. Accountability d. Political activism e. Teamwork and collaboration ANS: A, C, E Staffing is an independent nursing intervention and is an example of autonomy. Along with increased autonomy comes accountability or responsibility for outcomes of an action. When nurses work together this is teamwork and collaboration. Informatics is the use of information and technology to communicate, manage knowledge, mitigate error, and support decision making. Political activism usually involves more than day-to-day activities such as unit staffing. Chapter 16: Nursing Assessment Potter et al.: Fundamentals of Nursing, 9th Edition MULTIPLE CHOICE 1. The nurse is using critical thinking skills during the first phase of the nursing process. Which action indicates the nurse is in the first phase? a. Completes a comprehensive database b. Identifies pertinent nursing diagnoses c. Intervenes based on priorities of patient care d. Determines whether outcomes have been achieved ANS: A The assessment phase of the nursing process involves data collection to complete a thorough patient database and is the first phase. Identifying nursing diagnoses occurs during the diagnosis phase or second phase. The nurse carries out interventions during the implementation phase (fourth phase), and determining whether outcomes have been achieved takes place during the evaluation phase (fifth phase) of the nursing process. DIF:Apply (application)REF:210 OBJ: Discuss the relationship between critical thinking and nursing assessment. TOP:AssessmentMSC:Health Promotion and Maintenance 2. A nurse is using the problem-oriented approach to data collection. Which action will the nurse take first? a. Complete the questions in chronological order. b. Focus on the patient’s presenting situation. c. Make accurate interpretations of the data. d. Conduct an observational overview. ANS: B A problem-oriented approach focuses on the patient’s current problem or presenting situation rather than on an observational overview. The database is not always completed using a chronological approach if focusing on the current problem. Making interpretations of the data is not data collection. Data interpretation occurs while appropriate nursing diagnoses are assigned. The question is asking about data collection. DIF:Apply (application)REF:210 | 213 OBJ: Describe the methods of data collection. TOP: Assessment MSC:Health Promotion and Maintenance 3. After reviewing the database, the nurse discovers that the patient’s vital signs have not been recorded by the nursing assistive personnel (NAP). Which clinical decision should the nurse make? a. Administer scheduled medications assuming that the NAP would have reported abnormal vital signs. b. Have the patient transported to the radiology department for a scheduled x-ray, and review vital signs upon return. c. Ask the NAP to record the patient’s vital signs before administering medications. d. Omit the vital signs because the patient is presently in no distress. ANS: C The nurse should ask the nursing assistive personnel to record the vital signs for review before administering medicines or transporting the patient to another department. The nurse should not make assumptions when providing high-quality patient care, and omitting the vital signs is not an appropriate action. DIF:Analyze (analysis)REF:210 OBJ: Discuss the relationship between critical thinking and nursing assessment. TOP: Implementation MSC: Health Promotion and Maintenance 4. The nurse is gathering data on a patient. Which data will the nurse report as objective data? a. States “doesn’t feel good” b. Reports a headache c. Respirations 16 d. Nauseated ANS: C Objective data are observations or measurements of a patient’s health status, like respirations. Inspecting the condition of a surgical incision or wound, describing an observed behavior, and measuring blood pressure are examples of objective data. States “doesn’t feel good,” reports a headache, and nausea are all subjective data. Subjective data include the patient’s feelings, perceptions, and reported symptoms. Only patients provide subjective data relevant to their health condition. DIF:Apply (application)REF:214 OBJ: Differentiate between subjective and objective data. TOP: Assessment MSC:Health Promotion and Maintenance 5. A patient expresses fear of going home and being alone. Vital signs are stable and the incision is nearly completely healed. What can the nurse infer from the subjective data? a. The patient can now perform the dressing changes without help. b. The patient can begin retaking all of the previous medications. c. The patient is apprehensive about discharge. d. The patient’s surgery was not successful. ANS: C Subjective data include expressions of fear of going home and being alone. These data indicate (use inference) that the patient is apprehensive about discharge. Expressing fear is not an appropriate sign that a patient is able to perform dressing changes independently. An order from a health care provider is required before a patient is taught to resume previous medications. The nurse cannot infer that surgery was not successful if the incision is nearly completely healed. DIF:Apply (application)REF:212-213 OBJ: Differentiate between subjective and objective data. TOP: Assessment MSC: Psychosocial Integrity 6. Which method of data collection will the nurse use to establish a patient’s database? a. Reviewing the current literature to determine evidence-based nursing actions b. Checking orders for diagnostic and laboratory tests c. Performing a physical examination d. Ordering medications ANS: C You will learn to conduct different types of assessments: the patient-centered interview during a nursing health history, a physical examination, and the periodic assessments you make during rounding or administering care. A nursing database includes a physical examination. The nurse reviews the current literature in the implementation phase of the nursing process to determine evidence-based actions, and the health care provider is responsible for ordering medications. The nurse uses results from the diagnostic and laboratory tests to establish a patient database, not checking orders for tests. DIF:Understand (comprehension)REF:211 OBJ: Describe the methods of data collection. TOP: Assessment MSC:Health Promotion and Maintenance 7. A nurse is gathering information about a patient’s habits and lifestyle patterns. Which method of data collection will the nurse use that will best obtain this information? a. Carefully review lab results. b. Conduct the physical assessment. c. Perform a thorough nursing health history. d. Prolong the termination phase of the interview. ANS: C The nursing health history also includes a description of a patient’s habits and lifestyle patterns. Lab results and physical assessment will not reveal as much about the patient’s habits and lifestyle patterns as the nursing health history. Collecting data is part of the working phase of the interview. DIF:Analyze (analysis)REF:219 OBJ: Describe the methods of data collection. TOP: Assessment MSC:Health Promotion and Maintenance 8. While interviewing an older female patient of Asian descent, the nurse notices that the patient looks at the ground when answering questions. What should the nurse do? a. Consider cultural differences during this assessment. b. Ask the patient to make eye contact to determine her affect. c. Continue with the interview and document that the patient is depressed. d. Notify the health care provider to recommend a psychological evaluation. ANS: A To conduct an accurate and complete assessment, consider a patient’s cultural background. This nurse needs to practice culturally competent care and appreciate the cultural differences. Assuming that the patient is depressed or in need of a psychological evaluation or to force eye contact is inappropriate. DIF:Apply (application)REF:218-219 OBJ: Explain ways to make an assessment patient centered. TOP: Assessment MSC: Psychosocial Integrity 9. A nurse has already set the agenda during a patient-centered interview. What will the nurse do next? a. Begin with introductions. b. Ask about the chief concerns or problems. c. Explain that the interview will be over in a few minutes. d. Tell the patient “I will be back to administer medications in 1 hour.” ANS: B After setting the agenda, the nurse should conduct the actual interview and proceed with data collection, such as asking about the patient’s current chief concerns or problems. Introductions occur before setting the agenda. Begin an interview by introducing yourself and your position and explaining the purpose of the interview. Your aim is to set an agenda for how you will gather information about a patient’s current chief concerns or problems. The termination phase includes telling the patient when the interview is nearing an end. Telling the patient that medications will be given later when the nurse returns would typically take place during the termination phase of the interview. DIF:Understand (comprehension)REF:216 OBJ: Discuss how to conduct a patient-centered interview. TOP: Assessment MSC:Health Promotion and Maintenance 10. The nurse is attempting to prompt the patient to elaborate on the reports of daytime fatigue. Which question should the nurse ask? a. “Is there anything that you are stressed about right now that I should know?” b. “What reasons do you think are contributing to your fatigue?” c. “What are your normal work hours?” d. “Are you sleeping 8 hours a night?” ANS: B The question asking the patient what factors might be contributing to the fatigue will elicit the best open-ended response. Asking whether the patient is stressed and asking if the patient is sleeping 8 hours a night are closed-ended questions eliciting simple yes or no responses. Asking about normal work hours will elicit a matter-of-fact response and does not prompt the patient to elaborate on the daytime fatigue or ask about the contributing reasons. DIF:Apply (application)REF:216-217 OBJ: Discuss how to conduct a patient-centered interview. TOP: Assessment MSC:Health Promotion and Maintenance 11. A nurse is conducting a nursing health history. Which component will the nurse address? a. Nurse’s concerns b. Patient expectations c. Current treatment orders d. Nurse’s goals for the patient ANS: B Some components of a nursing health history include chief concern, patient expectations, spiritual health, and review of systems. Current treatment orders are located under the Orders section in the patient’s chart and are not a part of the nursing health history. Patient concerns, not nurse’s concerns, are included in the database. Goals that are mutually established, not nurse’s goals, are part of the nursing care plan. DIF:Understand (comprehension)REF:219 OBJ: Describe the components of a nursing history. TOP: Assessment MSC:Health Promotion and Maintenance 12. While the patient’s lower extremity, which is in a cast, is assessed, the patient tells the nurse about an inability to rest at night. The nurse disregards this information, thinking that no correlation has been noted between having a leg cast and developing restless sleep. Which action would have been best for the nurse to take? a. Tell the patient to just focus on the leg and cast right now. b. Document the sleep patterns and information in the patient’s chart. c. Explain that a more thorough assessment will be needed next shift. d. Ask the patient about usual sleep patterns and the onset of having difficulty resting. ANS: D The nurse must use critical thinking skills in this situation to assess first in this situation. The best response is to gather more assessment data by asking the patient about usual sleep patterns and the onset of having difficulty resting. The nurse should assess before documenting and should not ignore the patient’s report of a problem or postpone it till the next shift. DIF:Analyze (analysis)REF:210 | 212 | 219 OBJ:Conduct a nursing assessment.TOP:Assessment MSC:Health Promotion and Maintenance 13. The nurse begins a shift assessment by examining a surgical dressing that is saturated with serosanguineous drainage on a patient who had open abdominal surgery yesterday (or 1 day ago). Which type of assessment approach is the nurse using? a. Gordon’s Functional Health Patterns b. Activity-exercise pattern assessment c. General to specific assessment d. Problem-oriented assessment ANS: D The nurse is not doing a complete, general assessment and then focusing on specific problem areas. Instead, the nurse focuses immediately on the problem at hand (dressing and drainage from surgery) and performs a problem-oriented assessment. Utilizing Gordon’s Functional Health Patterns is an example of a structured database-type assessment technique that includes 11 patterns to assess. The nurse in this question is performing a specific problem-oriented assessment approach, not a general approach. The nurse is not performing an activity-exercise pattern assessment in this question. DIF:Apply (application)REF:213 OBJ: Describe the methods of data collection. TOP: Assessment MSC:Health Promotion and Maintenance 14. Which statement by a nurse indicates a good understanding about the differences between data validation and data interpretation? a. “Data interpretation occurs before data validation.” b. “Validation involves looking for patterns in professional standards.” c. “Validation involves comparing data with other sources for accuracy.” d. “Data interpretation involves discovering patterns in professional standards.” ANS: C Validation, by definition, involves comparing data with other sources for accuracy. Data interpretation involves identifying abnormal findings, clarifying information, and identifying patient problems. The nurse should validate data before interpreting the data and making inferences. The nurse is interpreting and validating patient data, not professional standards. DIF:Understand (comprehension)REF:220 OBJ: Explain the relationship between data interpretation and validation. TOP:AssessmentMSC:Health Promotion and Maintenance 15. Which scenario best illustrates the nurse using data validation when making a nursing clinical decision for a patient? a. The nurse determines to remove a wound dressing when the patient reveals the time of the last dressing change and notices old and new drainage. b. The nurse administers pain medicine due at 1700 at 1600 because the patient reports increased pain and the family wants something done. c. The nurse immediately asks the health care provider for an order of potassium when a patient reports leg cramps. d. The nurse elevates a leg cast when the patient reports decreased mobility. ANS: A The only scenario that validates a patient’s report with a nurse’s observation is changing the wound dressing. The nurse validates what the patient says by observing the dressing. The rest of the examples have the nurse acting only from a patient and/or family reports, not the nurse’s assessment. DIF:Analyze (analysis)REF:220 OBJ: Explain the relationship between data interpretation and validation. TOP:AssessmentMSC:Health Promotion and Maintenance 16. While completing an admission database, the nurse is interviewing a patient who states “I am allergic to latex.” Which action will the nurse take first? a. Immediately place the patient in isolation. b. Ask the patient to describe the type of reaction. c. Proceed to the termination phase of the interview. d. Document the latex allergy on the medication administration record. ANS: B The nurse should further assess and ask the patient to describe the type of reaction. The patient will not need to be placed in isolation; before terminating the interview or documenting the allergy, health care personnel need to be aware of what type of response the patient suffered. DIF:Apply (application)REF:219 OBJ:Conduct a nursing assessment.TOP:Assessment MSC:Health Promotion and Maintenance 17. A patient verbalizes a low pain level of 2 out of 10 but exhibits extreme facial grimacing while moving around in bed. What is the nurse’s initial action in response to these observations? a. Proceed to the next patient’s room to make rounds. b. Determine the patient does not want any pain medicine. c. Ask the patient about the facial grimacing with movement. d. Administer the pain medication ordered for moderate to severe pain. ANS: C First, the nurse needs to clarify/verify what was observed with what the patient states. Proceeding to the next room is ignoring this visual cue. The nurse cannot assume the patient does not want pain medicine just because he reports a 2 out of 10 on the pain scale. The nurse should not administer medication for moderate to severe pain if it is not necessary. DIF:Analyze (analysis)REF:212 | 220 OBJ:Conduct a nursing assessment.TOP:Assessment MSC:Health Promotion and Maintenance 18. The nurse is interviewing a patient with a hearing deficit. Which area should the nurse use to conduct this interview? a. The patient’s room with the door closed b. The waiting area with the television turned off c. The patient’s room before administration of pain medication d. The waiting room while the occupational therapist is working on leg exercises ANS: A Distractions should be eliminated as much as possible when interviewing a patient with a hearing deficit. The best place to conduct this interview is in the patient’s room with the door closed. The waiting area does not provide privacy. Pain can sometimes inhibit someone’s ability to concentrate, so before pain medication is administered is not advisable. It is best for the patient to be as comfortable as possible when conducting an interview. Assessing a patient while another member of the health care team is working would be distracting and is not the best time for an interview to take place. DIF:Analyze (analysis)REF:215-216 OBJ: Describe how courtesy, comfort, connection, and confirmation establish a foundation for patient assessment. TOP: Assessment MSC: Health Promotion and Maintenance 19. A new nurse is completing an assessment on an 80-year-old patient who is alert and oriented. The patient’s daughter is present in the room. Which action by the nurse will require follow-up by the charge nurse? a. The nurse makes eye contact with the patient. b. The nurse speaks only to the patient’s daughter. c. The nurse leans forward while talking with the patient. d. The nurse nods periodically while the patient is speaking. ANS: B Gathering data from family members is acceptable, but when a patient is able to interact, nurses need to include information from the older adult to complete the assessment. Therefore, the charge nurse must correct this misconception. When assessing an older adult, nurses need to listen carefully and allow the patient to speak. Positive nonverbal communication, such as making eye contact, nodding, and leaning forward, shows interest in the patient. Thus, the charge nurse does not need to intervene or follow up. DIF:Apply (application)REF:214-215 OBJ: Describe how developing relationships with patients fosters the assessment process. TOP:EvaluationMSC:Management of Care MULTIPLE RESPONSE 1. A nurse is completing an assessment. Which findings will the nurse report as subjective data? (Select all that apply.) a. Patient’s temperature b. Patient’s wound appearance c. Patient describing excitement about discharge d. Patient pacing the floor while awaiting test results e. Patient’s expression of fear regarding upcoming surgery ANS: C, E Subjective data include patient’s feelings, perceptions, and reported symptoms. Expressing feelings such as excitement or fear is an example of subjective data. Objective data are observations or measurements of a patient’s health status. In this question, the appearance of the wound and the patient’s temperature are objective data. Pacing is an observable patient behavior and is also considered objective data. DIF:Apply (application)REF:213-214 OBJ: Differentiate between subjective and objective data. TOP: Assessment MSC:Health Promotion and Maintenance MATCHING A nurse is completing an assessment using the PQRST to obtain data about the patient’s chest pain. Match the questions to the components of the PQRST that the nurse will be using. a. Where is the pain located? b. What causes the pain? c. Does it come and go? d. What does the pain feel like? e. What is the rating on a scale of 0 to 10? 1. Provokes 2. Quality 3. Radiate 4. Severity 5.Time 1.ANS:BDIF:Apply (application)REF:219 OBJ: Describe the methods of data collection. TOP: Assessment MSC: Basic Care and Comfort 2.ANS:DDIF:Apply (application)REF:219 OBJ: Describe the methods of data collection. TOP: Assessment MSC: Basic Care and Comfort 3.ANS:ADIF:Apply (application)REF:219 OBJ: Describe the methods of data collection. TOP: Assessment MSC: Basic Care and Comfort 4.ANS:EDIF:Apply (application)REF:219 OBJ: Describe the methods of data collection. TOP: Assessment MSC: Basic Care and Comfort 5.ANS:CDIF:Apply (application)REF:219 OBJ: Describe the methods of data collection. TOP: Assessment MSC: Basic Care and Comfort Chapter 17: Nursing Diagnosis Potter et al.: Fundamentals of Nursing, 9th Edition MULTIPLE CHOICE 1. After assessing a patient, a nurse develops a standard formal nursing diagnosis. What is the rationale for the nurse’s actions? a. To form a language that can be encoded only by nurses b. To distinguish the nurse’s role from the physician’s role c. To develop clinical judgment based on other’s intuition d. To help nurses focus on the scope of medical practice ANS: B The standard formal nursing diagnosis serves several purposes. Nursing diagnoses distinguish the nurse’s role from that of the physician/health care provider and help nurses focus on the scope of nursing practice (not medical) while fostering the development of nursing knowledge. A nursing diagnosis provides the precise definition that gives all members of the health care team a common language for understanding the patient’s needs. A diagnosis is a clinical judgment based on information. DIF:Understand (comprehension)REF:225 | 227 OBJ: Discuss how a nursing diagnosis guides nursing practice. TOP: Diagnosis MSC:Management of Care 2. Which diagnosis will the nurse document in a patient’s care plan that is NANDA-I approved? a. Sore throat b. Acute pain c. Sleep apnea d. Heart failure ANS: B Acute pain is the only NANDA-I approved diagnosis listed. Sleep apnea and heart failure are medical diagnoses, and sore throat is subjective data. DIF:Understand (comprehension)REF:227 | 233 OBJ: Discuss how a nursing diagnosis guides nursing practice. TOP: Diagnosis MSC:Management of Care 3. A nurse develops a nursing diagnostic statement for a patient with a medical diagnosis of pneumonia with chest x-ray results of lower lobe infiltrates. Which nursing diagnosis did the nurse write? a. Ineffective breathing pattern related to pneumonia b. Risk for infection related to chest x-ray procedure c. Risk for deficient fluid volume related to dehydration d. Impaired gas exchange related to alveolar-capillary membrane changes ANS: D The related to factor of alveolar-capillary membrane changes is accurately written because it is a patient response to the disease process of pneumonia that the nurse can treat. The related to factor should be the cause of the problem (nursing diagnosis) that a nurse can address. The related to factors of dehydration and pneumonia are all medical diagnoses that the nurse cannot change. A diagnostic test or a chronic dysfunction is not an etiology or a condition that a nursing intervention is able to treat. DIF:Apply (application)REF:230 | 232 | 236 OBJ: Discuss the relationship of critical thinking to the nursing diagnostic process. TOP:DiagnosisMSC:Management of Care 4. The nurse is reviewing a patient’s plan of care, which includes the nursing diagnostic statement, Impaired physical mobility related to tibial fracture as evidenced by patient’s inability to ambulate. Which part of the diagnostic statement does the nurse need to revise? a. Etiology b. Nursing diagnosis c. Collaborative problem d. Defining characteristic ANS: A The etiology, or related to factor, of tibial fracture is a medical diagnosis and needs to be revised. The nursing diagnosis is appropriate because the patient is unable to ambulate. A collaborative problem is an actual or potential physiological complication that nurses monitor to detect the onset of changes in a patient’s health status; there is no collaborative problem listed. The defining characteristic (subjective and objective data that support the diagnosis) is appropriate for Impaired physical mobility. DIF:Apply (application)REF:233 | 235 | 236 OBJ: Differentiate among a nursing diagnosis, medical diagnosis, and collaborative problem. TOP:DiagnosisMSC:Management of Care 5. A nurse is using assessment data gathered about a patient and combining critical thinking to develop a nursing diagnosis. What is the nurse doing? a. Assigning clinical cues b. Defining characteristics c. Diagnostic reasoning d. Diagnostic labeling ANS: C Diagnostic reasoning is defined as a process of using the assessment data gathered about a patient to logically explain a clinical judgment, in this case a nursing diagnosis. Defining characteristics are assessment findings that support the nursing diagnosis. Defining characteristics are the subjective and objective clinical cues, which a nurse gathers intentionally and unintentionally. The nurse organizes all of the patient’s data into meaningful and usable data clusters, which lead to a diagnostic conclusion. Diagnostic labeling is simply the name of the diagnosis. DIF:Understand (comprehension)REF:230 OBJ: Discuss the relationship of critical thinking to the nursing diagnostic process. TOP:DiagnosisMSC:Management of Care 6. A patient presents to the emergency department following a motor vehicle crash and suffers a right femur fracture. The leg is stabilized in a full leg cast. Otherwise, the patient has no other major injuries, is in good health, and reports only moderate discomfort. Which is the most pertinent nursing diagnosis the nurse will include in the plan of care? a. Posttrauma syndrome b. Constipation c. Acute pain d. Anxiety ANS: C Based on the assessment data provided, the only supportive evidence for one of the diagnosis options is “Reports only moderate discomfort,” which would support Acute pain. No supportive evidence is provided for any of the other diagnoses. The patient may indeed develop signs or symptoms of the other problems, but supportive data are presently lacking in the provided information. DIF:Apply (application)REF:230 | 233 OBJ: Discuss the relationship of critical thinking to the nursing diagnostic process. TOP:DiagnosisMSC:Management of Care 7. The nurse is reviewing a patient’s database for significant changes and discovers that the patient has not voided in over 8 hours. The patient’s kidney function lab results are abnormal, and the patient’s oral intake has significantly decreased since previous shifts. Which step of the nursing process should the nurse proceed to after this review? a. Diagnosis b. Planning c. Implementation d. Evaluation ANS: A After a thorough assessment, the nurse should proceed to analyzing the data and formulating a nursing diagnosis before proceeding with developing the plan of care and determining appropriate interventions; this is the diagnosis phase. The evaluation phase involves determining whether the goals were met and interventions were effective. DIF:Apply (application)REF:226 | 230 OBJ: Describe the steps of the nursing diagnostic process. TOP: Diagnosis MSC:Management of Care 8. A patient with a spinal cord injury is seeking to enhance urinary elimination abilities by learning self-catheterization versus assisted catheterization by home health nurses and family members. The nurse adds Readiness for enhanced urinary elimination in the care plan. Which type of diagnosis did the nurse write? a. Risk b. Problem focused c. Health promotion d. Collaborative problem ANS: C A health promotion nursing diagnosis is a clinical judgment concerning motivation and desire to increase well-being and actualize human health potential. A problem-focused nursing diagnosis describes a clinical judgment concerning an undesirable human response to a health condition/life process that exists in an individual, family, or community. A risk nursing diagnosis is a clinical judgment concerning the vulnerability of an individual, family, group or community for developing an undesirable human response to health conditions/life processes. A collaborative problem is an actual or potential physiological complication that nurses monitor to detect the onset of changes in a patient’s health status. DIF:Apply (application)REF:227 | 230 OBJ:Describe the differences among health promotion, problem focused, and risk nursing diagnoses.TOP:DiagnosisMSC:Management of Care 9. A nurse administers an antihypertensive medication to a patient at the scheduled time of 0900. The nursing assistive personnel (NAP) then reports to the nurse that the patient’s blood pressure was low when it was taken at 0830. The NAP states that was busy and had not had a chance to tell the nurse yet. The patient begins to complain of feeling dizzy and light-headed. The blood pressure is rechecked and it has dropped even lower. In which phase of the nursing process did the nurse first make an error? a. Assessment b. Diagnosis c. Implementation d. Evaluation ANS: A The diagnostic process should flow from the assessment. In this case, the nurse should have assessed the patient’s blood pressure before giving the medication. The nurse could have prevented the patient’s untoward reaction if the low blood pressure was assessed first. Diagnosis follows assessment. Administering the medication occurs in implementation, but this is not the first error. There are no errors in evaluation. DIF:Apply (application)REF:226 | 230 | 233 OBJ: Discuss the relationship of critical thinking to the nursing diagnostic process. TOP:DiagnosisMSC:Management of Care 10. A nurse adds the following diagnosis to a patient’s care plan: Constipation related to decreased gastrointestinal motility secondary to pain medication administration as evidenced by the patient reporting no bowel movement in seven days, abdominal distention, and abdominal pain. Which element did the nurse write as the defining characteristic? a. Decreased gastrointestinal motility b. Pain medication c. Abdominal distention d. Constipation ANS: C Abdominal distention, no reported bowel movement, and abdominal pain are the defining characteristics. Decreased gastrointestinal motility secondary to pain medication is an etiology or related to factor. Constipation (problem or NANDA-1 diagnosis) is the identified problem derived from the defining characteristics. DIF:Apply (application)REF:227 | 230 | 231 | 233 OBJ:Explain how defining characteristics and the etiological factor individualize a nursing diagnosis.TOP:DiagnosisMSC:Management of Care 11. The patient database reveals that a patient has decreased oral intake, decreased oxygen saturation when ambulating, reports of shortness of breath when getting out of bed, and a productive cough. Which elements will the nurse identify as defining characteristics for the diagnostic label of Activity intolerance? a. Decreased oral intake and decreased oxygen saturation when ambulating b. Decreased oxygen saturation when ambulating and reports of shortness of breath when getting out of bed c. Reports of shortness of breath when getting out of bed and a productive cough d. Productive cough and decreased oral intake ANS: B There are defining characteristics (observable assessment cues such as patient behavior, physical signs) that support each problem-focused diagnostic judgment. The signs and symptoms, or defining characteristics, for the diagnosis Activity intolerance include decreased oxygen saturation when ambulating and reports of shortness of breath when getting out of bed. The key to supporting the diagnosis of Activity intolerance is that only these two characteristics involve how the patient tolerates activity. Decreased oral intake and productive cough do not define activity intolerance. DIF:Analyze (analysis)REF:230 | 233 OBJ:Explain how defining characteristics and the etiological factor individualize a nursing diagnosis.TOP:DiagnosisMSC:Management of Care 12. A nurse performs an assessment on a patient. Which assessment data will the nurse use as an etiology for Acute pain? a. Discomfort while changing position b. Reports pain as a 7 on a 0 to 10 scale c. Disruption of tissue integrity d. Dull headache ANS: C Disruption of tissue integrity is a possible cause or etiology of pain. A report of pain, headache, and discomfort are examples of things a patient might say (subjective data or defining characteristics) that may lead a nurse to select Acute pain as a nursing diagnosis. DIF:Apply (application)REF:232-233 OBJ:Explain how defining characteristics and the etiological factor individualize a nursing diagnosis.TOP:DiagnosisMSC:Management of Care 13. A new nurse writes the following nursing diagnoses on a patient’s care plan. Which nursing diagnosis will cause the nurse manager to intervene? a. Wandering b. Hemorrhage c. Urinary retention d. Impaired swallowing ANS: B Hemorrhage is a collaborative problem, not a nursing diagnosis; the nurse manager will need to correct this misunderstanding with the new nurse. Nurses manage collaborative problems such as hemorrhage, infection, and paralysis using medical, nursing, and allied health (e.g., physical therapy) interventions. Wandering, urinary retention, and impaired swallowing are all examples of nursing diagnoses. DIF:Analyze (analysis)REF:225 | 231 | 232 OBJ: Differentiate among a nursing diagnosis, medical diagnosis, and collaborative problem. TOP:DiagnosisMSC:Management of Care 14. A patient has a bacterial infection in left lower leg. Which nursing diagnosis will the nurse add to the patient’s care plan? a. Infection b. Risk for infection c. Impaired skin integrity d. Staphylococcal leg infection ANS: C Impaired skin integrity is the only nursing diagnosis listed that will correlate to the patient information. While risk for infection is a nursing diagnosis, the patient is not at risk; the patient has an actual infection. Infection can be a medical diagnosis as well as a collaborative problem. Staphylococcal leg infection is a medical diagnosis. DIF:Apply (application)REF:225 OBJ: Differentiate among a nursing diagnosis, medical diagnosis, and collaborative problem. TOP:DiagnosisMSC:Management of Care 15. A nurse adds a nursing diagnosis to a patient’s care plan. Which information did the nurse document? a. Decreased cardiac output related to altered myocardial contractility. b. Patient needs a low-fat diet related to inadequate heart perfusion. c. Offer a low-fat diet because of heart problems. d. Acute heart pain related to discomfort. ANS: A Decreased cardiac output related to altered myocardial contractility is a correctly written nursing diagnosis. Patient needs a low-fat diet related to inadequate heart perfusion is a goal phrased statement, not a nursing diagnosis. Offer a low-fat diet is an intervention, not a diagnosis. Acute pain related to discomfort is a circular diagnosis and gives no direction to nursing care. DIF:Apply (application)REF:230 | 233 | 234-236 OBJ: Describe sources of diagnostic errors. TOP: Diagnosis MSC:Management of Care 16. A charge nurse is evaluating a new nurse’s plan of care. Which finding will cause the charge nurse to follow up? a. Assigning a documented nursing diagnosis of Risk for infection for a patient on intravenous (IV) antibiotics b. Completing an interview and physical examination before adding a nursing diagnosis c. Developing nursing diagnoses before completing the database d. Including cultural and religious preferences in the database ANS: C Developing nursing diagnoses before completion of the database needs to be corrected by the charge nurse. Always identify a nursing diagnosis from the data, not the reverse. The data should be clustered and reviewed to see if any patterns are present before a nursing diagnosis is assigned. Risk for infection is an appropriate diagnosis for a patient with an intravenous (IV) site in place. The IV site involves a break in skin integrity and is a potential source of infection. The diagnostic process should proceed in steps. Completing the interview and physical examination before adding a nursing diagnosis is appropriate. The patient’s cultural background and developmental stage are important to include in a patient database. DIF:Analyze (analysis)REF:230 | 234-236 OBJ: Describe sources of diagnostic errors. TOP: Diagnosis MSC:Management of Care 17. A patient exhibits the following symptoms: tachycardia, increased thirst, headache, decreased urine output, and increased body temperature. The nurse analyzes the data. Which nursing diagnosis will the nurse assign to the patient? a. Adult failure to thrive b. Hypothermia c. Deficient fluid volume d. Nausea ANS: C The signs the patient is exhibiting are consistent with deficient fluid volume (dehydration). Even without knowing the clinical manifestations of dehydration, the question can be answered by the process of elimination. Adult failure to thrive, hypothermia, and nausea are not appropriate diagnoses because data are insufficient to support these diagnoses. DIF:Analyze (analysis)REF:230 | 233 OBJ: Identify nursing diagnoses from a nursing assessment. TOP: Diagnosis MSC:Management of Care 18. Which question would be most appropriate for a nurse to ask a patient to assist in establishing a nursing diagnosis of Diarrhea? a. “What types of foods do you think caused your upset stomach?” b. “How many bowel movements a day have you had?” c. “Are you able to get to the bathroom in time?” d. “What medications are you currently taking?” ANS: B The nurse needs to first ensure that the symptoms support the diagnosis. By definition, diarrhea means that a patient is having frequent stools; therefore, asking about the number of bowel movements is most appropriate. Asking about irritating foods and medications may help the nurse determine the cause of the diarrhea, but first the nurse needs to make sure the diagnosis is appropriate. Asking the patient if he can make it to the bathroom will help to establish a diagnosis of incontinence, not diarrhea. The question is asking for the most appropriate statement to establish the diagnosis of Diarrhea. DIF:Analyze (analysis)REF:230 OBJ: Identify nursing diagnoses from a nursing assessment. TOP: Diagnosis MSC:Management of Care 19. A nurse assesses that a patient has not voided in 6 hours. Which question should the nurse ask to assist in establishing a nursing diagnosis of Urinary retention? a. “Do you feel like you need to go to the bathroom?” b. “Are you able to walk to the bathroom by yourself?” c. “When was the last time you took your medicine?” d. “Do you have a safety rail in your bathroom at home?” ANS: A The nurse must establish that the patient feels the urge and is unable to void. The question “Do you feel like you need to go to the bathroom?” is the most appropriate to ask. This question can be answered without knowledge of the diagnosis of Urinary retention. Discussing the ability to walk to the bathroom and asking about safety rails pertain to mobility and safety issues, not to retention of urine. Taking certain medications may lead to urinary retention, but that information would establish the etiology. The question is asking for the nurse to first establish the correct diagnosis. DIF:Analyze (analysis)REF:230 | 235 OBJ: Identify nursing diagnoses from a nursing assessment. TOP: Diagnosis MSC:Management of Care 20. A nurse is developing nursing diagnoses for a patient. Beginning with the first step, place in order the steps the nurse will use. 1. Observes the patient having dyspnea (shortness of breath) and a diagnosis of asthma 2. Writes a diagnostic label of impaired gas exchange 3. Organizes data into meaningful clusters 4. Interprets information from patient 5. Writes an etiology a. 1, 3, 4, 2, 5 b. 1, 3, 4, 5, 2 c. 1, 4, 3, 5, 2 d. 1, 4, 3, 2, 5 ANS: A The diagnostic process flows from the assessment process (observing and gathering data) and includes decision-making steps. These steps include data clustering, identifying patient health problems, and formulating the diagnosis (diagnosis is written as problem or NANDA-I approved diagnosis then etiology or cause). DIF:Apply (application)REF:230-231 OBJ: Describe the steps of the nursing diagnostic process. TOP: Diagnosis MSC:Management of Care MULTIPLE RESPONSE 1. A nurse is developing nursing diagnoses for a group of patients. Which nursing diagnoses will the nurse use? (Select all that apply.) a. Anxiety related to barium enema b. Impaired gas exchange related to asthma c. Impaired physical mobility related to incisional pain d. Nausea related to adverse effect of cancer medication e. Risk for falls related to nursing assistive personnel leaving bedrail down ANS: C, D Impaired physical mobility and Nausea are the only correctly written nursing diagnoses. All the rest are incorrectly written. Anxiety lists a diagnostic test as the etiology. Impaired gas exchange lists a medical diagnosis as the etiology. Risk for falls has a legally inadvisable statement for an etiology. DIF:Apply (application)REF:233-236 OBJ: Describe sources of diagnostic errors. TOP: Diagnosis MSC:Management of Care Chapter 28: Immobility Potter et al.: Fundamentals of Nursing, 9th Edition MULTIPLE CHOICE 1. A nurse is assessing body alignment. What is the nurse monitoring? a. The relationship of one body part to another while in different positions b. The coordinated efforts of the musculoskeletal and nervous systems c. The force that occurs in a direction to oppose movement d. The inability to move about freely ANS: A The terms body alignment and posture are similar and refer to the positioning of the joints, tendons, ligaments, and muscles while standing, sitting, and lying. Body alignment means that the individual’s center of gravity is stable. Body mechanics is a term used to describe the coordinated efforts of the musculoskeletal and nervous systems. Friction is a force that occurs in a direction to oppose movement. Immobility is the inability to move about freely. DIF:Understand (comprehension)REF:407-408 OBJ:Discuss physiological and pathological influences on mobility. TOP: Assessment MSC: Basic Care and Comfort 2. A nurse is providing range of motion to the shoulder and must perform external rotation. Which action will the nurse take? a. Moves patient’s arm in a full circle b. Moves patient’s arm cross the body as far as possible c. Moves patient’s arm behind body, keeping elbow straight d. Moves patient’s arm until thumb is upward and lateral to head with elbow flexed ANS: D External rotation: With elbow flexed, move arm until thumb is upward and lateral to head. Circumduction: Move arm in full circle (Circumduction is combination of all movements of ball-and-socket joint.) Adduction: Lower arm sideways and across body as far as possible. Hyperextension: Move arm behind body, keeping elbow straight. DIF:Understand (comprehension)REF:415 OBJ: Compare and contrast active and passive range-of-motion exercises. TOP: Implementation MSC: Basic Care and Comfort 3. A nurse is providing passive range of motion (ROM) for a patient with impaired mobility. Which technique will the nurse use for each movement? a. Each movement is repeated 5 times by the patient. b. Each movement is performed until the patient experiences pain. c. Each movement is completed quickly and smoothly by the nurse. d. Each movement is moved just to the point of resistance by the nurse. ANS: D Passive ROM exercises are performed by the nurse. Carry out movements slowly and smoothly, just to the point of resistance; ROM should not cause pain. Never force a joint beyond its capacity. Each movement needs to be repeated 5 times during the session. The patient moves all joints through ROM unassisted in active ROM. DIF:Understand (comprehension)REF:427 | 430 OBJ: Compare and contrast active and passive range-of-motion exercises. TOP: Implementation MSC: Basic Care and Comfort 4. A nurse is performing passive range of motion (ROM) and splinting on an at-risk patient. Which finding will indicate goal achievement for the nurse’s action? a. Prevention of atelectasis b. Prevention of renal calculi c. Prevention of pressure ulcers d. Prevention of joint contractures ANS: D Goal achievement for passive ROM is prevention of joint contractures. Contractures develop in joints not moved periodically through their full ROM. ROM exercises reduce the risk of contractures. Researchers noted that prompt use of splinting with prescribed ROM exercises reduced contractures and improved active range of joint motion in affected lower extremities. Deep breathing and coughing and using an incentive spirometer will help prevent atelectasis. Adequate hydration helps prevent renal calculi and urinary tract infections. Interventions aimed at prevention of pressure ulcers include positioning, skin care, and the use of therapeutic devices to relieve pressure. DIF:Apply (application)REF:412 | 414 OBJ: Evaluate patient outcomes as a result of a nursing plan for improving or maintaining mobility. TOP:EvaluationMSC:Management of Care 5. A nurse is preparing to reposition a patient. Which task can the nurse delegate to the nursing assistive personnel? a. Determining the level of comfort b. Changing the patient’s position c. Identifying immobility hazards d. Assessing circulation ANS: B The skill of moving and positioning patients in bed can be delegated to nursing assistive personnel (NAP). The nurse is responsible for assessing the patient’s level of comfort and for any hazards of immobility and assessing circulation. DIF:Understand (comprehension)REF:432 OBJ: Describe interventions for improving or maintaining patients’ mobility. TOP:PlanningMSC:Management of Care 6. A nurse is preparing to assess a patient for orthostatic hypotension. Which piece of equipment will the nurse obtain to assess for this condition? a. Thermometer b. Elastic stockings c. Blood pressure cuff d. Sequential compression devices ANS: C A blood pressure cuff is needed. Orthostatic hypotension is a drop of blood pressure greater than 20 mm Hg in systolic pressure or 10 mm Hg in diastolic pressure and symptoms of dizziness, light-headedness, nausea, tachycardia, pallor, or fainting when the patient changes from the supine to standing position. A thermometer is used to assess for fever. Elastic stockings and sequential compression devices are used to prevent thrombus. DIF:Apply (application)REF:411 OBJ: Identify changes in physiological and psychosocial function associated with immobility. TOP: Assessment MSC: Reduction of Risk Potential 7. The patient has been in bed for several days and needs to be ambulated. Which action will the nurse take first? a. Maintain a narrow base of support. b. Dangle the patient at the bedside. c. Encourage isometric exercises. d. Suggest a high-calcium diet. ANS: B To prevent injury, nurses implement interventions that reduce or eliminate the effects of orthostatic hypotension. Mobilize the patient as soon as the physical condition allows, even if this only involves dangling at the bedside or moving to a chair. A wide base of support increases balance. Isometric exercises (i.e., activities that involve muscle tension without muscle shortening) have no beneficial effect on preventing orthostatic hypotension, but they improve activity tolerance. A high-calcium diet can help with osteoporosis but can be detrimental in an immobile patient. DIF:Apply (application)REF:424 OBJ: Describe interventions for improving or maintaining patients’ mobility. TOP: Implementation MSC: Basic Care and Comfort 8. A nurse reviews an immobilized patient’s laboratory results and discovers hypercalcemia. Which condition will the nurse monitor for most closely in this patient? a. Hypostatic pneumonia b. Renal calculi c. Pressure ulcers d. Thrombus formation ANS: B Renal calculi are calcium stones that lodge in the renal pelvis or pass through the ureters. Immobilized patients are at risk for calculi because they frequently have hypercalcemia. Hypercalcemia does not lead to hypostatic pneumonia, pressure ulcers, or thrombus formation. Immobility is one cause of hypostatic pneumonia, which is inflammation of the lung from stasis or pooling of secretions. A pressure ulcer is an impairment of the skin that results from prolonged ischemia (decreased blood supply) within tissues. A thrombus is an accumulation of platelets, fibrin, clotting factors, and cellular elements of the blood attached to the interior wall of a vein or artery, which sometimes occludes the lumen of the vessel. DIF:Apply (application)REF:411-412 OBJ: Identify changes in physiological and psychosocial function associated with immobility. TOP: Assessment MSC: Physiological Adaptation 9. A nurse is caring for an immobile patient. Which metabolic alteration will the nurse monitor for in this patient? a. Increased appetite b. Increased diarrhea c. Increased metabolic rate d. Altered nutrient metabolism ANS: D Immobility disrupts normal metabolic functioning: decreasing the metabolic rate, altering the metabolism of carbohydrates, fats, and proteins; causing fluid, electrolyte, and calcium imbalances; and causing gastrointestinal disturbances such as decreased appetite and slowing of peristalsis, leading to constipation. DIF:Apply (application)REF:410 OBJ: Identify changes in physiological and psychosocial function associated with immobility. TOP: Assessment MSC: Physiological Adaptation 10. A nurse is preparing a care plan for a patient who is immobile. Which psychosocial aspect will the nurse consider? a. Loss of bone mass b. Loss of strength c. Loss of weight d. Loss of hope ANS: D Loss of hope is a psychosocial aspect. Patients with restricted mobility may have some depression. Depression is an affective disorder characterized by exaggerated feelings of sadness, melancholy, dejection, worthlessness, emptiness, and hopelessness out of proportion to reality. All the rest are physiological aspects: bone mass, strength, and weight. DIF:Apply (application)REF:413 OBJ: Identify changes in physiological and psychosocial function associated with immobility. TOP: Planning MSC: Psychosocial Integrity 11. The nurse is preparing to lift a patient. Which action will the nurse take first? a. Position a drawsheet under the patient. b. Assess weight and determine assistance needs. c. Delegate the task to a nursing assistive personnel. d. Attempt to manually lift the patient alone before asking for assistance. ANS: B When lifting, assess the weight you will lift, and determine the assistance you will need. The nurse has to assess before positioning a drawsheet or delegating the task. Manual lifting is the last resort, and it is used when the task at hand does not involve lifting most or all of the patient’s weight; most facilities have a no-lift policy. DIF:Apply (application)REF:421 OBJ: Describe interventions for improving or maintaining patients’ mobility. TOP: Implementation MSC: Basic Care and Comfort 12. The nurse is caring for an older-adult patient who has been diagnosed with a stroke. Which intervention will the nurse add to the care plan? a. Encourage the patient to perform as many self-care activities as possible. b. Provide a complete bed bath to promote patient comfort. c. Coordinate with occupational therapy for gait training. d. Place the patient on bed rest to prevent fatigue. ANS: A Nurses should encourage the older-adult patient to perform as many self-care activities as possible, thereby maintaining the highest level of mobility. Sometimes nurses inadvertently contribute to a patient’s immobility by providing unnecessary help with activities such as bathing and transferring. Placing the patient on bed rest without sufficient ambulation leads to loss of mobility and functional decline, resulting in weakness, fatigue, and increased risk for falls. After a stroke or brain attack, a patient likely receives gait training from a physical therapist; speech rehabilitation from a speech therapist; and help from an occupational therapist for ADLs such as dressing, bathing and toileting, or household chores. DIF:Apply (application)REF:413 OBJ: Develop individualized nursing care plans for patients with impaired mobility. TOP:PlanningMSC:Management of Care 13. The nurse is observing the way a patient walks. Which aspect is the nurse assessing? a. Activity tolerance b. Body alignment c. Range of motion d. Gait ANS: D Gait describes a particular manner or style of walking. Activity tolerance is the type and amount of exercise or work that a person is able to perform. Body alignment refers to the position of the joints, tendons, ligaments, and muscles while standing, sitting, and lying. Range of motion is the maximum amount of movement available at a joint in one of the three planes of the body: sagittal, frontal, or transverse. DIF:Understand (comprehension)REF:416 OBJ:Assess for correct and impaired body alignment and mobility. TOP: Assessment MSC: Basic Care and Comfort 14. A nurse is assessing the body alignment of a standing patient. Which finding will the nurse report as normal? a. When observed laterally, the spinal curves align in a reversed “S” pattern. b. When observed posteriorly, the hips and shoulders form an “S” pattern. c. The arms should be crossed over the chest or in the lap. d. The feet should be close together with toes pointed out. ANS: A When the patient is observed laterally, the head is erect and the spinal curves are aligned in a reversed “S” pattern. When observed posteriorly, the shoulders and hips are straight and parallel. The arms hang comfortably at the sides. The feet are slightly apart to achieve a base of support, and the toes are pointed forward. DIF:Apply (application)REF:417 OBJ:Assess for correct and impaired body alignment and mobility. TOP:AssessmentMSC:Health Promotion and Maintenance 15. The nurse is evaluating the body alignment of a patient in the sitting position. Which observation by the nurse will indicate a normal finding? a. The edge of the seat is in contact with the popliteal space. b. Both feet are supported on the floor with ankles flexed. c. The body weight is directly on the buttocks only. d. The arms hang comfortably at the sides. ANS: B Both feet are supported on the floor, and the ankles are comfortably flexed. Body weight is evenly distributed on the buttocks and thighs. A 1- to 2-inch space is maintained between the edge of the seat and the popliteal space on the posterior surface of the knee to ensure that no pressure is placed on the popliteal artery or nerve. The patient’s forearms are supported on the armrest, in the lap, or on a table in front of the chair. DIF:Apply (application)REF:417 OBJ:Assess for correct and impaired body alignment and mobility. TOP:AssessmentMSC:Health Promotion and Maintenance 16. The nurse is assessing body alignment for a patient who is immobilized. Which patient position will the nurse use? a. Supine position b. Lateral position c. Lateral position with positioning supports d. Supine position with no pillow under the patient’s head ANS: B Assess body alignment for a patient who is immobilized or bedridden with the patient in the lateral position, not supine. Remove all positioning supports from the bed except for the pillow under the head, and support the body with an adequate mattress. DIF:Apply (application)REF:418 OBJ:Assess for correct and impaired body alignment and mobility. TOP: Implementation MSC: Basic Care and Comfort 17. The nurse is assessing the patient for respiratory complications of immobility. Which action will the nurse take when assessing the respiratory system? a. Inspect chest wall movements primarily during the expiratory cycle. b. Auscultate the entire lung region to assess lung sounds. c. Focus auscultation on the upper lung fields. d. Assess the patient at least every 4 hours. ANS: B Auscultate the entire lung region to identify diminished breath sounds, crackles, or wheezes. Perform a respiratory assessment at least every 2 hours for patients with restricted activity. Inspect chest wall movements during the full inspiratory-expiratory cycle. Focus auscultation on the dependent lung fields because pulmonary secretions tend to collect in these lower regions. DIF:Apply (application)REF:419 OBJ:Assess for correct and impaired body alignment and mobility. TOP: Implementation MSC: Health Promotion and Maintenance 18. The nurse is assessing an immobile patient for deep vein thromboses (DVTs). Which action will the nurse take? a. Remove elastic stockings every 4 hours. b. Measure the calf circumference of both legs. c. Lightly rub the lower leg for redness and tenderness. d. Dorsiflex the foot while assessing for patient discomfort. ANS: B Measure bilateral calf circumference and record it daily as an assessment for DVT. Unilateral increases in calf circumference are an early indication of thrombosis. Homan’s sign, or calf pain on dorsiflexion of the foot, is no longer a reliable indicator in assessing for DVT, and it is present in other conditions. Remove the patient’s elastic stockings and/or sequential compression devices (SCDs) every 8 hours, and observe the calves for redness, warmth, and tenderness. Instruct the family, patient, and all health care personnel not to massage the area because of the danger of dislodging the thrombus. DIF:Apply (application)REF:419 OBJ:Assess for correct and impaired body alignment and mobility. TOP: Implementation MSC: Health Promotion and Maintenance 19. A nurse is assessing the skin of an immobilized patient. What will the nurse do? a. Assess the skin every 4 hours. b. Limit the amount of fluid intake. c. Use a standardized tool such as the Braden Scale. d. Have special times for inspection so as to not interrupt routine care. ANS: C Consistently use a standardized tool, such as the Braden Scale. This identifies patients with a high risk for impaired skin integrity. Skin assessment can be as often as every hour. Limiting fluids can lead to dehydration, increasing skin breakdown. Observe the skin often during routine care. DIF:Apply (application)REF:419 OBJ:Assess for correct and impaired body alignment and mobility. TOP: Implementation MSC: Basic Care and Comfort 20. The nurse is caring for an older-adult patient with a diagnosis of urinary tract infection (UTI). Upon assessment the nurse finds the patient confused and agitated. How will the nurse interpret these assessment findings? a. These are normal signs of aging. b. These are early signs of dementia. c. These are purely psychological in origin. d. These are common manifestation with UTIs. ANS: D The primary symptom of compromised older patients with an acute urinary tract infection or fever is confusion. Acute confusion in older adults is not normal; a thorough nursing assessment is the priority. With the diagnosis of urinary tract infection, these are not early signs of dementia and they are not purely psychological. DIF:Apply (application)REF:419 OBJ: Identify changes in physiological and psychosocial function associated with immobility. TOP: Assessment MSC: Physiological Adaptation 21. A patient has damage to the cerebellum. Which disorder is most important for the nurse to assess? a. Imbalance b. Hemiplegia c. Muscle sprain d. Lower extremity paralysis ANS: A Damage to the cerebellum causes problems with balance, and motor impairment is directly related to the amount of destruction of the motor strip. A stroke can lead to hemiplegia. Direct trauma to the musculoskeletal system results in bruises, contusions, sprains, and fractures. A complete transection of the spinal cord can lead to lower extremity paralysis. DIF:Apply (application)REF:409 OBJ:Discuss physiological and pathological influences on mobility. TOP: Assessment MSC: Physiological Adaptation 22. Which patient will cause the nurse to select a nursing diagnosis of Impaired physical mobility for a care plan? a. A patient who is completely immobile b. A patient who is not completely immobile c. A patient at risk for single-system involvement d. A patient who is at risk for multisystem problems ANS: B The diagnosis of Impaired physical mobility applies to the patient who has some limitation but is not completely immobile. The diagnosis of Risk for disuse syndrome applies to the patient who is immobile and at risk for multisystem problems because of inactivity. Beyond these diagnoses, the list of potential diagnoses is extensive because immobility affects multiple body systems. DIF:Understand (comprehension)REF:420 OBJ: Formulate appropriate nursing diagnoses for patients with impaired mobility. TOP:DiagnosisMSC:Management of Care 23. The patient has the nursing diagnosis of Impaired physical mobility related to pain in the left shoulder. Which priority action will the nurse take? a. Encourage the patient to do self-care. b. Keep the patient as mobile as possible. c. Encourage the patient to perform ROM. d. Assist the patient with comfort measures. ANS: D The diagnosis related to pain requires the nurse to assist the patient with comfort measures so that the patient is then willing and more able to move. Pain must be controlled so the patient will not be reluctant to initiate movement. The diagnosis related to reluctance to initiate movement requires interventions aimed at keeping the patient as mobile as possible and encouraging the patient to perform self-care and ROM. DIF:Understand (comprehension)REF:420 OBJ: Develop individualized nursing care plans for patients with impaired mobility. TOP: Implementation MSC: Basic Care and Comfort 24. A nurse is developing an individualized plan of care for a patient. Which action is important for the nurse to take? a. Establish goals that are measurable and realistic. b. Set goals that are a little beyond the capabilities of the patient. c. Use the nurse’s own judgment and not be swayed by family desires. d. Explain that without taking alignment risks, there can be no progress. ANS: A The nurse must develop an individualized plan of care for each nursing diagnosis and must set goals that are individualized, realistic, and measurable. The nurse should set realistic expectations for care and should include the patient and family when possible. The goals focus on preventing problems or risks to body alignment and mobility. DIF:Understand (comprehension)REF:421 OBJ: Develop individualized nursing care plans for patients with impaired mobility. TOP:PlanningMSC:Management of Care 25. Which behavior indicates the nurse is using a team approach when caring for a patient who is experiencing alterations in mobility? a. Delegates assessment of lung sounds to nursing assistive personnel b. Becomes solely responsible for modifying activities of daily living c. Consults physical therapy for strengthening exercises in the extremities d. Involves respiratory therapy for altered breathing from severe anxiety levels ANS: C The nurse should collaborate with other health care team members such as physical or occupational therapists when considering mobility needs. For example, physical therapists are a resource for planning ROM or strengthening exercises. Nurses often delegate some interventions to nursing assistive personnel, but assessment of lung sounds is the nurse’s responsibility. Nursing assistive personnel may turn and position patients, apply elastic stockings, help patients use the incentive spirometer, etc. Occupational therapists are a resource for planning activities of daily living that patients need to modify or relearn. A mental health advanced practice nurse or psychologist should be used for severe anxiety. DIF:Apply (application)REF:421 OBJ: Develop individualized nursing care plans for patients with impaired mobility. TOP:ImplementationMSC:Management of Care 26. The patient is being admitted to the neurological unit with a diagnosis of stroke. When will the nurse begin discharge planning? a. At the time of admission b. The day before the patient is to be discharged c. When outpatient therapy will no longer be needed d. As soon as the patient’s discharge destination is known ANS: A Discharge planning begins when a patient enters the health care system. In anticipation of the patient’s discharge from an institution, the nurse makes appropriate referrals or consults a case manager or a discharge planner to ensure that the patient’s needs are met at home. Referrals to home care or outpatient therapy are often needed. Planning the day before discharge, when outpatient therapy is no longer needed, and as soon as the discharge destination is known is too late. DIF:Apply (application)REF:421 OBJ: Develop individualized nursing care plans for patients with impaired mobility. TOP:PlanningMSC:Management of Care 27. Which goal is most appropriate for a patient who has had a total hip replacement? a. The patient will ambulate briskly on the treadmill by the time of discharge. b. The patient will walk 100 feet using a walker by the time of discharge. c. The nurse will assist the patient to ambulate in the hall 2 times a day. d. The patient will ambulate by the time of discharge. ANS: B “The patient will walk 100 feet using a walker by the time of discharge” is individualized, realistic, and measurable. “Ambulating briskly on a treadmill” is not realistic for this patient. The option that focuses on the nurse, not the patient, is not a measurable goal; this is an intervention. “The patient will ambulate by the time of discharge” is not measurable because it does not specify the distance. Even though we can see that the patient will ambulate, this does not quantify how far. DIF:Analyze (analysis)REF:421-422 OBJ: Develop individualized nursing care plans for patients with impaired mobility. TOP:PlanningMSC:Management of Care 28. The nurse is working on an orthopedic rehabilitation unit that requires lifting and positioning of patients. Which personal injury will the nurse most likely try to prevent? a. Arm b. Hip c. Back d. Ankle ANS: C Back injuries are often the direct result of improper lifting and bending. The most common back injury is strain on the lumbar muscle group. While arm, hip, and ankle can occur, they are not as common as back. DIF:Understand (comprehension)REF:421 OBJ: Describe interventions for improving or maintaining patients’ mobility. TOP:PlanningMSC:Health Promotion and Maintenance 29. A nurse is caring for a patient with osteoporosis and lactose intolerance. What will the nurse do? a. Encourage dairy products. b. Monitor intake of vitamin D. c. Increase intake of caffeinated drinks. d. Try to do as much as possible for the patient. ANS: B Encourage patients at risk to be screened for osteoporosis and assess their diets for calcium and vitamin D intake. Patients who have lactose intolerance need dietary teaching about alternative sources of calcium. Caffeine should be decreased. The goal of the patient with osteoporosis is to maintain independence with ADLs. Assistive ambulatory devices, adaptive clothing, and safety bars help the patient maintain independence. DIF:Apply (application)REF:423 OBJ: Develop individualized nursing care plans for patients with impaired mobility. TOP: Implementation MSC: Health Promotion and Maintenance 30. A nurse is providing care to a group of patients. Which patient will the nurse see first? a. A patient with a hip replacement on prolonged bed rest reporting chest pain and dyspnea b. A bedridden patient who has a reddened area on the buttocks who needs to be turned c. A patient on bed rest who has renal calculi and needs to go to the bathroom d. A patient after knee surgery who needs range of motion exercises ANS: A A patient on prolonged bed rest will be prone to deep vein thrombosis, which can lead to an embolus. An embolus can travel through the circulatory system to the lungs and impair circulation and oxygenation, resulting in tachycardia and shortness of breath. Venous emboli that travel to the lungs are sometimes life threatening. While the patient with a reddened area needs to be turned, a patient with renal calculi needing the restroom, and a patient needing range of motion, these are not as life threatening as the chest pain and dyspnea. DIF:Analyze (analysis)REF:419 OBJ: Develop individualized nursing care plans for patients with impaired mobility. TOP:AssessmentMSC:Management of Care 31. The patient is immobilized after undergoing hip replacement surgery. Which finding will alert the nurse to monitor for hemorrhage in this patient? a. Thick, tenacious pulmonary secretions b. Low-molecular-weight heparin doses c. SCDs wrapped around the legs d. Elastic stockings (TED hose) ANS: B Heparin and low-molecular-weight heparin are the most widely used drugs in the prophylaxis of deep vein thrombosis. Because bleeding is a potential side effect of these medications, continually assess the patient for signs of bleeding. Pulmonary secretions that become thick and tenacious are difficult to remove and are a sign of inadequate hydration or developing pneumonia but not of bleeding. SCDs consist of sleeves or stockings made of fabric or plastic that are wrapped around the leg and are secured with Velcro. They decrease venous stasis by increasing venous return through the deep veins of the legs. They do not usually cause bleeding. Elastic stockings also aid in maintaining external pressure on the muscles of the lower extremities and in promoting venous return. They do not usually cause bleeding. DIF:Apply (application)REF:424 OBJ: Develop individualized nursing care plans for patients with impaired mobility. TOP: Assessment MSC: Reduction of Risk Potential 32. The nurse needs to move a patient up in bed using a drawsheet. The nurse has another nurse helping. In which order will the nurses perform the steps, beginning with the first one? 1. Grasp the drawsheet firmly near the patient. 2. Move the patient and drawsheet to the desired position. 3. Position one nurse at each side of the bed. 4. Place the drawsheet under the patient from shoulder to thigh. 5. Place your feet apart with a forward-backward stance. 6. Flex knees and hips and on count of three shift weight from the front to back leg. a. 1, 4, 5, 6, 3, 2 b. 4, 1, 3, 5, 6, 2 c. 3, 4, 1, 5, 6, 2 d. 5, 6, 3, 1, 4, 2 ANS: C Assisting a patient up in bed with a drawsheet (two or three nurses): (1) Place the patient supine with the head of the bed flat. A nurse stands on each side of the bed. (2) Remove the pillow from under the patient’s head and shoulders and place it at the head of the bed. (3) Turn the patient side to side to place the drawsheet under the patient, extending it from shoulders to thighs. (4) Return the patient to the supine position. (5) Fanfold the drawsheet on both sides, with each nurse grasping firmly near the patient. (6) Nurses place their feet apart with a forward-backward stance. Nurses should flex knees and hips. On the count of three, nurses should shift their weight from front to back leg and move the patient and drawsheet to the desired position in the bed. DIF:Understand (comprehension)REF:433 OBJ: Describe interventions for improving or maintaining patients’ mobility. TOP: Implementation MSC: Basic Care and Comfort 33. The nurse is caring for a patient who needs to be placed in the prone position. Which action will the nurse take? a. Place pillow under the patient’s abdomen after turning. b. Turn head toward one side with large, soft pillow. c. Position legs flat against bed. d. Raise head of bed to 45 degrees. ANS: A Placing a pillow under the patient’s abdomen after turning decreases hyperextension of lumbar vertebrae and strain on lower back; breathing may also be enhanced. Head is turned toward one side with a small pillow to reduce flexion or hyperextension of cervical vertebrae. Legs should be supported with pillows to elevate toes and prevent footdrop. Forty-five degrees is the position for Fowler’s position; prone is on the stomach. DIF:Apply (application)REF:436 OBJ: Describe interventions for improving or maintaining patients’ mobility. TOP: Implementation MSC: Basic Care and Comfort 34. The nurse is caring for a patient with a spinal cord injury and notices that the patient’s hips have a tendency to rotate externally when the patient is supine. Which device will the nurse use to help prevent injury secondary to this rotation? a. Hand rolls b. A trapeze bar c. A trochanter roll d. Hand-wrist splints ANS: C A trochanter roll prevents external rotation of the hips when the patient is in a supine position. Hand rolls maintain the thumb in slight adduction and in opposition to the fingers. Hand-wrist splints are individually molded for the patient to maintain proper alignment of the thumb and the wrist. The trapeze bar is a triangular device that hangs down from a securely fastened overhead bar that is attached to the bedframe. It allows the patient to pull with the upper extremities to raise the trunk off the bed, to assist in transfer from bed to wheelchair, or to perform upper arm exercises. DIF:Understand (comprehension)REF:428 OBJ: Describe interventions for improving or maintaining patients’ mobility. TOP: Implementation MSC: Basic Care and Comfort 35. The patient is unable to move self and needs to be pulled up in bed. What will the nurse do to make this procedure safe? a. Place the pillow under the patient’s head and shoulders. b. Do by self if the bed is in the flat position. c. Place the side rails in the up position. d. Use a friction-reducing device. ANS: D This is not a one-person task. Helping a patient move up in bed without help from other co-workers or without the aid of an assistive device (e.g., friction-reducing pad) is not recommended and is not considered safe for the patient or the nurse. Remove the pillow from under head and shoulders and place it at the head of the bed to prevent striking the patient’s head against the head of the bed. When pulling a patient up in bed, the bed should be flat to gain gravity assistance, and the side rails should be down. DIF:Apply (application)REF:433 OBJ: Describe interventions for improving or maintaining patients’ mobility. TOP: Implementation MSC: Basic Care and Comfort 36. The nurse is caring for a patient who is immobile and needs to be turned every 2 hours. The patient has poor lower extremity circulation, and the nurse is concerned about irritation of the patient’s toes. Which device will the nurse use? a. Hand rolls b. A foot cradle c. A trapeze bar d. A trochanter roll ANS: B A foot cradle may be used in patients with poor peripheral circulation as a means of reducing pressure on the tips of a patient’s toes. A trochanter roll prevents external rotation of the hips when the patient is in a supine position. Hand rolls maintain the thumb in slight adduction and in opposition to the fingers. The trapeze bar is a triangular device that hangs down from a securely fastened overhead bar that is attached to the bedframe. It allows the patient to pull with the upper extremities to raise the trunk off the bed, to assist in transfer from bed to wheelchair, or to perform upper arm exercises. DIF:Apply (application)REF:434 OBJ: Describe interventions for improving or maintaining patients’ mobility. TOP: Implementation MSC: Basic Care and Comfort 37. A nurse delegates a position change to a nursing assistive personnel. The nurse instructs the NAP to place the patient in the lateral position. Which finding by the nurse indicates a correct outcome? a. Patient is lying on side. b. Patient is lying on back. c. Patient is lying semiprone. d. Patient is lying on abdomen. ANS: A In the side-lying (or lateral) position the patient rests on the side with the major portion of body weight on the dependent hip and shoulder. Patients in the supine position rest on their backs. Sims’ position is semiprone. The patient in the prone position lies face or chest down on the abdomen. DIF:Understand (comprehension)REF:429 | 436 OBJ: Evaluate patient outcomes as a result of a nursing plan for improving or maintaining mobility. TOP:EvaluationMSC:Management of Care 38. A nurse is evaluating care of an immobilized patient. Which action will the nurse take? a. Focus on whether the interdisciplinary team is satisfied with the care. b. Compare the patient’s actual outcomes with the outcomes in the care plan. c. Involve primarily the patient’s family and health care team to determine goal achievement. d. Use objective data solely in determining whether interventions have been successful. ANS: B From your perspective as the nurse, you are to evaluate outcomes and response to nursing care and compare the patient’s actual outcomes with the outcomes selected during planning. Ask if the patient’s expectations (subjective data) of care are being met, and use objective data to determine the success of interventions. Just as it was important to include the patient during the assessment and planning phase of the care plan, it is essential to have the patient’s evaluation of the plan of care, not just the patient’s family and health care team. DIF:Understand (comprehension)REF:431 OBJ: Evaluate patient outcomes as a result of a nursing plan for improving or maintaining mobility. TOP:EvaluationMSC:Management of Care 39. A nurse is supervising the logrolling of a patient. To which patient is the nurse most likely providing care? a. A patient with neck surgery b. A patient with hypostatic pneumonia c. A patient with a total knee replacement d. A patient with a Stage IV pressure ulcer ANS: A A nurse supervises and aids personnel when there is a health care provider’s order to logroll a patient. Patients who have suffered from spinal cord injury or are recovering from neck, back, or spinal surgery often need to keep the spinal column in straight alignment to prevent further injury. Hypostatic pneumonia, total knee replacement, and Stage IV ulcers do not have to be logrolled. DIF:Understand (comprehension)REF:437 OBJ: Develop individualized nursing care plans for patients with impaired mobility. TOP:ImplementationMSC:Management of Care 40. The nurse is providing teaching to an immobilized patient with impaired skin integrity about diet. Which diet will the nurse recommend? a. High protein, high calorie b. High carbohydrate, low fat c. High vitamin A, high vitamin E d. Fluid restricted, bland ANS: A Because the body needs protein to repair injured tissue and rebuild depleted protein stores, give the immobilized patient a high-protein, high-calorie diet. A high-carbohydrate, low-fat diet is not beneficial for an immobilized patient. Vitamins B and C are needed rather than A and E. Fluid restriction can be detrimental to the immobilized patient; this can lead to dehydration. A bland diet is not necessary for immobilized patients. DIF:Understand (comprehension)REF:423 OBJ: Describe interventions for improving or maintaining patients’ mobility. TOP: Implementation MSC: Basic Care and Comfort 41. The nurse is caring for a patient who has had a stroke causing total paralysis of the right side. To help maintain joint function and minimize the disability from contractures, passive ROM will be initiated. When should the nurse begin this therapy? a. After the acute phase of the disease has passed b. As soon as the ability to move is lost c. Once the patient enters the rehab unit d. When the patient requests it ANS: B Passive ROM exercises should begin as soon as the patient’s ability to move the extremity or joint is lost. The nurse should not wait for the acute phase to end. It may be some time before the patient enters the rehab unit or the patient requests it, and contractures could form by then. DIF:Understand (comprehension)REF:430 OBJ: Compare and contrast active and passive range-of-motion exercises. TOP: Planning MSC: Basic Care and Comfort 42. The nurse is admitting a patient who has been diagnosed as having had a stroke. The health care provider writes orders for “ROM as needed.” What should the nurse do next? a. Restrict patient’s mobility as much as possible. b. Realize the patient is unable to move extremities. c. Move all the patient’s extremities. d. Further assess the patient. ANS: D Further assessment of the patient is needed to determine what the patient is able to perform. Some patients are able to move some joints actively, whereas the nurse passively moves others. With a weak patient, the nurse may have to support an extremity while the patient performs the movement. In general, exercises need to be as active as health and mobility allow. DIF:Apply (application)REF:414 OBJ: Compare and contrast active and passive range-of-motion exercises. TOP: Implementation MSC: Basic Care and Comfort 43. A nurse is assessing pressure points in a patient placed in the Sims’ position. Which areas will the nurse observe? a. Chin, elbow, hips b. Ileum, clavicle, knees c. Shoulder, anterior iliac spine, ankles d. Occipital region of the head, coccyx, heels ANS: B In the Sims’ position pressure points include the ileum, humerus, clavicle, knees, and ankles. The lateral position pressure points include the ear, shoulder, anterior iliac spine, and ankles. The prone position pressure points include the chin, elbows, female breasts, hips, knees, and toes. Supine position pressure points include the occipital region of the head, vertebrae, coccyx, elbows, and heels. DIF:Apply (application)REF:429 OBJ:Assess for correct and impaired body alignment and mobility. TOP: Assessment MSC: Reduction of Risk Potential 44. The patient is admitted to a skilled care unit for rehabilitation after the surgical procedure of fixation of a fractured left hip. The patient’s nursing diagnosis is Impaired physical mobility related to musculoskeletal impairment from surgery and pain with movement. The patient is able to use a walker but needs assistance ambulating and transferring from the bed to the chair. Which nursing intervention is most appropriate for this patient? a. Obtain assistance and physically transfer the patient to the chair. b. Assist with ambulation and measure how far the patient walks. c. Give pain medication after ambulation so the patient will have a clear mind. d. Bring the patient to the cafeteria for group instruction on ambulation. ANS: B Assist with walking and measure how far the patient walks to quantify progress. The nurse should allow the patient to do as much for self as possible. Therefore, the nurse should observe the patient transferring from the bed to the chair using the walker and should provide assistance as needed. The patient should be encouraged to use adequate pain medication to decrease the effects of pain and to increase mobility. The patient should be instructed on safe transfer and ambulation techniques in an environment with few distractions, not in the cafeteria. DIF: Analyze (analysis) REF: 413-414 | 428 | 431-432 | 438 OBJ: Develop individualized nursing care plans for patients with impaired mobility. TOP: Implementation MSC: Basic Care and Comfort 45. The patient has been diagnosed with a spinal cord injury and needs to be repositioned using the logrolling technique. Which technique will the nurse use for logrolling? a. Use at least three people. b. Have the patient reach for the opposite side rail when turning. c. Move the top part of the patient’s torso and then the bottom part. d. Do not use pillows after turning. ANS: A At least three to four people are needed to perform this skill safely. Have the patient cross the arms on the chest to prevent injury to the arms. Move the patient as one unit in a smooth, continuous motion on the count of three. Gently lean the patient as a unit back toward pillows for support. DIF:Apply (application)REF:437 OBJ: Describe interventions for improving or maintaining patients’ mobility. TOP: Implementation MSC: Basic Care and Comfort MULTIPLE RESPONSE 1. Upon assessment a nurse discovers that a patient has erythema. Which actions will the nurse take? (Select all that apply.) a. Consult a dietitian. b. Increase fiber in the diet. c. Place on chest physiotherapy. d. Increase frequency of turning. e. Place on pressure-relieving mattress. ANS: A, D, E If skin shows areas of erythema and breakdown, increase the frequency of turning and repositioning; place the turning schedule above the patient’s bed; implement other activities per agency skin care policy or protocol (e.g., assess more frequently, consult dietitian, place patient on pressure-relieving mattress). Increased fiber will help constipation. Chest physiotherapy is for respiratory complications. DIF:Apply (application)REF:438 OBJ: Describe interventions for improving or maintaining patients’ mobility. TOP: Implementation MSC: Reduction of Risk Potential 2. The nurse is caring for a patient with impaired physical mobility. Which potential complications will the nurse monitor for in this patient? (Select all that apply.) a. Footdrop b. Somnolence c. Hypostatic pneumonia d. Impaired skin integrity e. Increased socialization ANS: A, C, D Immobility leads to complications such as hypostatic pneumonia. Other possible complications include footdrop and impaired skin integrity. Interruptions in the sleep-wake cycle and social isolation are more common complications than somnolence or increased socialization. DIF:Understand (comprehension)REF:410-411 | 419 OBJ: Identify changes in physiological and psychosocial function associated with immobility. TOP: Assessment MSC: Reduction of Risk Potential 3. The nurse is caring for a patient who has had a recent stroke and is paralyzed on the left side. The patient has no respiratory or cardiac issues but cannot walk. The patient cannot button a shirt and cannot feed self due to being left-handed and becomes frustrated very easily. The patient has been eating very little and has lost 2 lbs. The patient asks the nurse, “How can I go home like this? I’m not getting better.” Which health care team members will the nurse need to consult? (Select all that apply.) a. Dietitian b. Physical therapist c. Respiratory therapist d. Cardiac rehabilitation therapist e. Occupational therapist f. Psychologist ANS: A, B, E, F Physical therapists are a resource for planning ROM or strengthening exercises, and occupational therapists are a resource for planning ADLs that patients need to modify or relearn. Because of the loss of 2 lbs and eating very little, a dietitian will also be helpful. Referral to a mental health advanced practice nurse, a licensed social worker, or a physiologist to assist with coping or other psychosocial issues is also wise. Because the patient exhibits good cardiac and respiratory function, respiratory therapy and cardiac rehabilitation probably are not needed at this time. DIF:Analyze (analysis)REF:421 OBJ: Develop individualized nursing care plans for patients with impaired mobility. TOP:ImplementationMSC:Management of Care MATCHING Upon assessment a nurse discovers postural abnormalities on several patients. Match the abnormalities to the findings the nurse observed. a. Lateral-S- or C-shaped spinal column with vertebral rotation b. Legs curved inward so knees come together as person walks c. One or both legs bent outward at knee d. Inclining of head to affected side e. Exaggeration of anterior convex curve of lumbar spine f. Increased convexity in curvature of thoracic spine 1. Lordosis 2. Kyphosis 3. Scoliosis 4. Genu valgum 5. Genu varum 6. Torticollis 1.ANS:EDIF:Understand (comprehension)REF:409 OBJ:Discuss physiological and pathological influences on mobility. [Show More]
Last updated: 2 years ago
Preview 1 out of 56 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$17.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Feb 13, 2021
Number of pages
56
Written in
Additional information
This document has been written for:
Uploaded
Feb 13, 2021
Downloads
0
Views
110




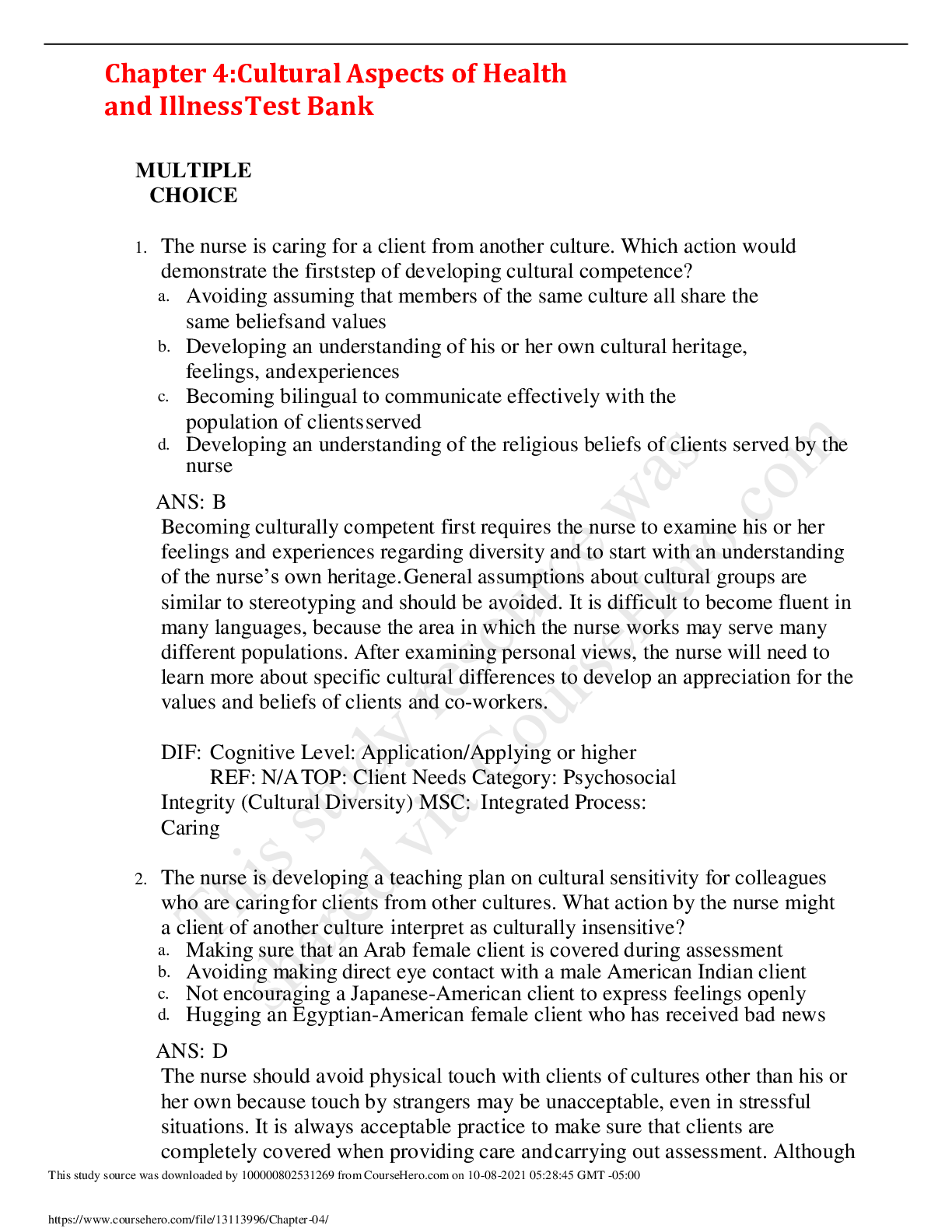


.png)