
AQA AS BIOLOGY Biological Molecules and Cells QP and Mark Scheme Version 1.0. 2021 ASSESSMENT RESOURCE
*NURSING > QUESTIONS & ANSWERS > NSG6420 Question Bank for Week 1 to Week 9 Quiz, Final Exam, and Midterm Exam (2020, Latest): South (All)
Question : The major impact of the physiological changes that occur with aging is: Student Answer: Reduced physiological reserve Reduced homeostatic mechanisms Impaired immunologi ... cal response All of the above Instructor Explanation: The major impact of all of these physiological changes can be highlighted with three primary points. First, there is a reduced physiological reserve of most body systems, particularly cardiac, respiratory, and renal. Second, there are reduced homeostatic mechanisms that fail to adjust regulatory systems such as temperature control and fluid and electrolyte balance. Third, there is impaired immunological function: infection risk is greater, and autoimmune diseases are more prevalent. (Kennedy-Malone 3) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 2 of 2 Comments: Question 2. Question : Men have faster and more efficient biotransformation of drugs and this is thought to be due to: Student Answer: Less obesity rates than women Prostate enlargement Testosterone Less estrogen than women Instructor Explanation: Men have faster and more efficient biotransformation, presumably because of serum testosterone. Conditions of increased or decreased liver perfusion alter the overall level of the drug that is absorbed and how it is metabolized. (Kennedy-Malone 5) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 2 of 2 Comments: Question 3. Question : The cytochrome p system involves enzymes that are generally: Student Answer: Inhibited by drugs Induced by drugs Inhibited or induced by drugs Associated with decreased liver perfusion Instructor Explanation: Biotransformation occurs in all body tissues but primarily in the liver, where enzymatic activity (cytochrome P [CYP] system) alters and detoxifies the drug and prepares it for excretion. (Kennedy-Malone 5) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 2 of 2 Comments: Question 4. Question : Functional abilities are best assessed by: Student Answer: Self-report of function Observed assessment of function A comprehensive head-to-toe examination Family report of function Instructor Explanation: Two well-established tools used to evaluate function in older adults are the Katz Activities of Daily Living Scale (Katz et al., 1963) and the Lawton and Brody scale for Instrumental Activities of Daily Living (Lawton & Brody, 1969). It is important to be cautious about self-report of function (rather than direct observation of function) and to ask, “Do you …?” instead of “Can you …?” in order to determine if patients actually perform the activity. (Kennedy-Malone 40) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 2 of 2 Comments: Question 5. Question : Iron Deficiency Anemia (IDA) is classified as a microcytic, hypochromic anemia. This classification refers to which of the following laboratory data? Student Answer: Hemoglobin and Hematocrit Mean Corpuscular Volume (MCV) and Mean Corpuscular Hemoglobin (MCH) Serum ferritin and serum iron Total iron binding capacity and transferrin saturation Instructor Explanation: RBC indices reveal an MCV (mean corpuscular volume/RBC size) that will be decreased to <80 fL in adults; MCH (mean corpuscular hemoglobin/RBC color) will show hypochromia or pale cells; RBC distribution width (RDW)/volume variation will be increased. (Kennedy-Malone page 519) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 0 of 2 Comments: Question 6. Question : When interpreting laboratory data, you would expect to see the following in a patient with Anemia of Chronic Disease (ACD): Student Answer: Hemoglobin <12 g/dl, MCV decreased, MCH decreased Hemoglobin >12 g/dl, MCV increased, MCH increased Hemoglobin <12 g/dl, MCV normal, MCH normal Hemoglobin >12 g/dl, MCV decreased, MCH increased Instructor Explanation: Hemoglobin (Hgb): <12 g/dL (120 g/L) women <13 g/dL (130 g/L) men Rarely <10 g/dL (100 g/L) Mean corpuscular volume: 80–96 mcm3 (normocytic) Mean corpuscular hemoglobin Normochromic (normal color) RBC distribution width: normal (Kennedy-Malone page 517) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 0 of 2 Comments: Question 7. Question : The pathophysiological hallmark of ACD is: Student Answer: Depleted iron stores Impaired ability to use iron stores Chronic uncorrectable bleeding Reduced intestinal absorption of iron Instructor Explanation: The pathophysiological hallmark of ACD is a disregulation of iron homeostasis, characterized by an increased uptake and retention of iron within the cells of the reticuloendothelial system (liver/spleen), resulting in decreased RBC production. Essentially, iron is present but inaccessible for use in the production of Hgb with the erythrocytes (Bross et al., 2010). A shortened RBC survival is also a contributing factor to ACD. (Kennedy-Malone page 516-517) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 0 of 2 Comments: Question 8. Question : The main focus of treatment of patients with ACD is: Student Answer: Replenishing iron stores Providing for adequate nutrition high in iron Management of the underlying disorder Administration of monthly vitamin B12 injections Instructor Explanation: Treatment: Treatment of ACD focuses on management of the underlying disorder. Iron supplementation is of no benefit in ACD, except in cases of coexisting IDA. A therapeutic trial of iron supplementation of no longer than 1 month may be useful in delineating between ACD and IDA. In ACD, there would be no hematological response to iron therapy (Chen & Gandhi, 2004). (Kennedy-Malone page 518) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 2 of 2 Comments: Question 9. Question : In addition to the complete blood count (CBC) with differential, which of the following laboratory tests is considered to be most useful in diagnosing ACD and IDA? Student Answer: Serum iron Total iron binding capacity Transferrin saturation Serum ferritin Instructor Explanation: Treatment: Treatment of ACD focuses on management of the underlying disorder. Iron supplementation is of no benefit in ACD, except in cases of coexisting IDA. A therapeutic trial of iron supplementation of no longer than 1 month may be useful in delineating between ACD and IDA. In ACD, there would be no hematological response to iron therapy (Chen & Gandhi, 2004). (Kennedy-Malone page 518) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 2 of 2 Comments: Question 10. Question : Symptoms in the initial human immunodeficiency virus (HIV) infection include all of the following except: Student Answer: Sore throat Fever Weight loss Headache Instructor Explanation: Signal symptoms: The initial HIV infection is characterized by mononucleosis-like illness with fever, sore throat, lymphadenopathy, headache, and fatigue. A roseola-like rash may also develop. These initial symptoms are followed by an asymptomatic phase, which may last 10 years or more. Later, if untreated, lymphadenopathy, weight loss, myalgias, and diarrhea may develop (Cohen, Kuritzkes, & Sax, 2011). In advanced disease, malignancies and opportunistic infections occur. Co-infection with hepatitis B or C is common (25% to 30%) in IV drug users, so hepatitis symptoms may also appear (Centers for Disease Control and Prevention [CDC], 2010a). (Kennedy-Malone page 521) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 0 of 2 Comments: Question 11. Question : Essential parts of a health history include all of the following except: Student Answer: Chief complaint History of the present illness Current vital signs All of the above are essential history components Instructor Explanation: Vital signs are part of the physical examination portion of patient assessment, not part of the health history. Points Received: 2 of 2 Comments: Question 12. Question : Which of the following clinical reasoning tools is defined as evidence-based resource based on mathematical modeling to express the likelihood of a condition in select situations, settings, and/or patients? Student Answer: Clinical practice guideline Clinical decision rule Clinical algorithm Clinical recommendation Instructor Explanation: Clinical decision (or prediction) rules provide another support for clinical reasoning. Clinical decision rules are evidence-based resources that provide probabilistic statements regarding the likelihood that a condition exists if certain variables are met with regard to the prognosis of patients with specific findings. Decision rules use mathematical models and are specific to certain situations, settings, and/or patient characteristics. Goolsby page 7 Points Received: 2 of 2 Comments: Question 13. Question : The first step in the genomic assessment of a patient is obtaining information regarding: Student Answer: Family history Environmental exposures Lifestyle and behaviors Current medications Instructor Explanation: A critical first step in genomic assessment, including assessment of risk, is the use of family history. Family history is considered the first genetic screen (Berry & Shooner 2004) and is a critical component of care because it reflects shared genetic susceptibilities, shared environment, and common behaviors (Yoon, Scheuner, & Khoury 2003). Goolsby page 18 Points Received: 2 of 2 Comments: Question 14. Question : In autosomal recessive (AR) disorders, individuals need: Student Answer: Only one mutated gene on the sex chromosomes to acquire the disease Only one mutated gene to acquire the disease Two mutated genes to acquire the disease Two mutated genes to become carriers Instructor Explanation: In autosomal recessive (AR) disorders, the offspring inherits the condition by receiving one copy of the gene mutation from each of the parents. Autosomal recessive disorders must be inherited through both parents (Nussbaum et al. 2007). Individuals who have an AR disorder have two mutated genes, one on each locus of the chromosome. Parents of an affected person are called carriers because each carries one copy of the mutation on one chromosome and a normal gene on the other chromosome. Carriers typically are not affected by the disease. Goolsby page 28 Points Received: 0 of 2 Comments: Question 15. Question : In AR disorders, carriers have: Student Answer: Two mutated genes; two from one parent that cause disease A mutation on a sex chromosome that causes a disease A single gene mutation that causes the disease One copy of a gene mutation but not the disease Instructor Explanation: Individuals who have an AR disorder have two mutated genes, one on each allele of the chromosome. Parents of an affected person are called carriers because each parent carries one copy of the mutation on one chromosome and a normal gene on the other chromosome. Carriers typically are not affected by the disease. In pedigrees with an AR inheritance patterns, males and females will be equally affected because the gene mutation is on an autosome. Goolsby page 28 Points Received: 2 of 2 Comments: Question 16. Question : A woman with an X-linked dominant disorder will: Student Answer: Not be affected by the disorder herself Transmit the disorder to 50% of her offspring (male or female) Not transmit the disorder to her daughters Transmit the disorder to only her daughters Instructor Explanation: Everyone born with an X-linked dominant disorder will be affected with the disease. Transmission of the disorder to the next generation varies by gender, however. A woman will transmit the mutation to 50% of all her offspring (male or female). Goolsby page 29 Points Received: 0 of 2 Comments: Question 17. Question : According to the Genetic Information Nondiscrimination Act (GINA): Student Answer: Nurse Practitioners (NPs) should keep all genetic information of patients confidential NPs must obtain informed consent prior to genetic testing of all patients Employers cannot inquire about an employee’s genetic information All of the above Instructor Explanation: On May 21, 2008, President George W. Bush signed the Genetic Information Nondiscrimination Act (GINA) to protect Americans against discrimination based upon their genetic information when it comes to health insurance and employment, paving the way for patient personalized genetic medicine without fear of discrimination (National Human Genome Research Institute 2012). Goolsby page 43 Points Received: 2 of 2 Comments: Question 18. Question : Which of the following would be considered a “red flag” that requires more investigation in a patient assessment? Student Answer: Colon cancer in family member at age 70 Breast cancer in family member at age 75 Myocardial infarction in family member at age 35 All of the above Instructor Explanation: Early onset cancer syndromes, heart disease, or dementia are red flags that warrant further investigation regarding hereditary disorders. Goolsby page 36 Points Received: 0 of 2 Comments: Question 19. Question : Your 2-year-old patient shows facial features, such as epicanthal folds, up-slanted palpebral fissures, single transverse palmar crease, and a low nasal bridge. These are referred to as: Student Answer: Variable expressivity related to inherited disease Dysmorphic features related to genetic disease De novo mutations of genetic disease Different penetrant signs of genetic disease Instructor Explanation: Assessing for dysmorphic features may enable identification of certain syndromes or genetic or chromosomal disorders (Jorde, Carey, & Bamshad 2010; Prichard & Korf 2008). Dysmorphology is defined as “the study of abnormal physical development” (Jorde, Carey, & Bamshad 2010, 302). Goolsby page 37 Points Received: 2 of 2 Comments: Question 20. Question : In order to provide a comprehensive genetic history of a patient, the NP should: Student Answer: Ask patients to complete a family history worksheet Seek out pathology reports related to the patient’s disorder Interview family members regarding genetic disorders All of the above Instructor Explanation: Asking the patient to complete a family history worksheet prior to the appointment saves time in the visit while offering the patient an opportunity to contribute to the collection of an accurate family history. Reviewing the family information can also help establish family rapport while verifying medical conditions in individual family members. If a hereditary condition is being considered but family medical information is unclear or unknown, requesting medical records and pathology or autopsy reports may be warranted. Goolsby page 32 1. Question : An 86-year-old patient who wears a hearing aid complains of poor hearing in the affected ear. In addition to possible hearing aid malfunction, this condition is often due to: Student Answer: Acoustic neuroma Cerumen impaction Otitis media Ménière’s disease Instructor Explanation: Elderly clients frequently present with complaints of hardened cerumen and decreased hearing resulting from cerumen impaction aggravated by hearing aid wear. (Goolsby 137-138) Conductive hearing loss is caused by a lesion involving the outer and middle ear to the level of the oval window. Various structural abnormalities, cerumen impaction, perforation of the tympanic membrane, middle ear fluid, damage to the ossicles from trauma or infection, otosclerosis, tympanosclerosis, cholesteatoma, middle ear tumors, temporal bone fractures, injuries related to trauma, and congenital problems are some of the causes. (Kennedy-Malone 170-171) Points Received: 2 of 2 Comments: Question 2. Question : In examination of the nose, the clinician observes gray, pale mucous membranes with clear, serous discharge. This is most likely indicative of: Student Answer: Bacterial sinusitis Allergic rhinitis Drug abuse Skull fracture Instructor Explanation: When examining the nose, assess the mucosa for integrity, color, moistness, and edema/lesions and the nasal septum for patency. The turbinates should be assessed for color and size. Pale, boggy turbinates suggest allergies; erythematous, swollen turbinates are often seen with infection. Any discharge should be noted. Clear, profuse discharge is often associated with allergies. (Goolsby 128-129) Patients with seasonal allergic rhinitis report rhinorrhea, sneezing, obstructed nasal passages, and pruritic eyes, nose, and oropharynx during the spring and fall. Patients with perennial allergic rhinitis have similar symptoms associated with exposure to environmental allergens typically in their homes. Physical examination may reveal a pale, boggy nasal mucosa, injected conjunctiva, enlarged turbinates, dark discoloration or bags under the eyes, and mouth breathing; absence of pale, boggy nasal mucosa does not rule out allergic rhinitis. (Kennedy-Malone 182-183) Points Received: 2 of 2 Comments: Question 3. Question : A 45 year old patient presents with ‘sore throat’ and fever for one week. After a quick strep screen you determine the patient has Strep throat. You know that streptococcal pharyngitis should be treated with antibiotics to prevent complications and to shorten the course of disease. Which of the following antibiotics should be considered when a patient is allergic to Penicillin? Student Answer: Amoxicillin EES (erythromycin) Bicillin L-A Dicloxacillin Instructor Explanation: MedU Card #1 Points Received: 2 of 2 Comments: Question 4. Question : Presbycusis is the hearing impairment that is associated with: Student Answer: Physiologic aging Ménière’s disease Cerumen impaction Herpes zoster Instructor Explanation: Presbycusis is an age-related cause of gradual sensorineural hearing loss and involves diminished hairy cell function within the cochlea as well as decreased elasticity of the TM. Although the changes associated with presbycusis often start in early adulthood, the decreased hearing acuity is usually not noticed until the individual is older than 65. (Goolsby 138) Because presbycusis is gradual and insidious, hearing loss may go unnoticed until it has progressed significantly. (Kennedy-Malone 170) Points Received: 2 of 2 Comments: Question 5. Question : Epistaxis can be a symptom of: Student Answer: Over-anticoagulation Hematologic malignancy Cocaine abuse All of the above Instructor Explanation: Cocaine abuse, which is more common than might be expected, frequently causes epistaxis. Hematologic disorders likely to cause bleeding include thrombocytopenia, leukemia, aplastic anemia, and hereditary coagulopathies. High doses of anticoagulants can cause epistaxis and bleeding from the gums. (Goolsby 142) Epistaxis results from a spontaneous rupture of a blood vessel in the nose, usually in the anterior septum in Kiesselbach's plexus (Nguyen, 2012). The bleeding may be secondary to local infections, systemic infections, drying of the nasal mucous membrane, trauma, arteriosclerosis, hypertension, or bleeding disorders. Trauma is usually the primary mechanism of disruption of the nasal mucosa. Posterior epistaxis can result in nausea and respiratory compromise. In older adults, nasal and paranasal tumors may be involved (Mäkitie, 2010). (Kennedy-Malone 168-169) Points Received: 2 of 2 Comments: Question 6. Question : Your patient has been using chewing tobacco for 10 years. On physical examination, you observe a white ulceration surrounded by erythematous base on the side of his tongue. The clinician should recognize that very often this is: Student Answer: Malignant melanoma Squamous cell carcinoma Aphthous ulceration Behcet’s syndrome Instructor Explanation: Most oral malignancies are painless until quite advanced, so patients are often unaware of the lesion unless the lip or anterior portion of the tongue is involved. The patient may become aware of the lesion if it bleeds. Squamous cell cancer lesions vary in appearance, from the reddened patches of erythroplakia to areas of induration/thickening, ulceration, or necrotic lesions. Lesions of malignant melanoma have varied pigmentation, including brown, blue, and black. Even lesions that appear flat and smooth may be nodular, indurated, or fixed to adjacent tissue on palpation. Even though patients with squamous cell malignancies often have a history of heavy alcohol and/or tobacco use or poor dentition, these are not risk factors for malignant melanoma. In Behcet’s syndrome, the patient complains of recurrent episodes of oral lesions that are consistent with aphthous ulcers. The number of lesions ranges from one to several; the size of the ulcers varies from less than to greater than 1 cm. Like aphthous ulcers, the lesions are well defined, with a pale yellow or gray base surrounded by erythema. The majority of patients also develop lesions on the genitals and eyes. (Goolsby 153) Tobacco use and heavy alcohol consumption, alone or synergistically, are strongly related to the development of oral cancer. Pipe smoking and sun exposure have been implicated in lip cancer. Leukoplakia and erythroplasia are often precursors to oral cancer. Relationships between oral cancer and Epstein-Barr virus, HPV, herpes simplex virus, and immunodeficiency states also have been found (Stenson, 2011). (Kennedy-Malone 177). Points Received: 2 of 2 Comments: Question 7. Question : A 26 year old patient presents with cough and general malaise for 3 days. They note that their eyes have been watering clear fluid and a ‘runny nose’ since yesterday. They note they ‘feel miserable’ and demand something to make them feel better. What would be the best first plan of treatment? Student Answer: Saline nasal spray for congestion and acetaminophen as needed for pain. Z-pack (azithromycin) for infection and Cromolyn nasal for congestion Hydrococone/acetaminophen as needed for pain and Guaifensin for congestion Cephalexin for infection and Cromolyn ophthalmic for congestion Instructor Explanation: MedU Card #4 Points Received: 0 of 2 Comments: Question 8. Question : Which of the following findings should trigger an urgent referral to a cardiologist or neurologist? Student Answer: History of bright flash of light followed by significantly blurred vision History of transient and painless monocular loss of vision History of monocular severe eye pain, blurred vision, and ciliary flush All of the above Instructor Explanation: Amaurosis fugax is a monocular, transient loss of vision. It stems from transient ischemia of the retina and presents an important warning sign for impending stroke. Depending on the circumstances reported, the patient should be immediately referred to either a cardiovascular or neurological specialist. (Goolsby 108) Points Received: 2 of 2 Comments: Question 9. Question : Dizziness that is described as "lightheaded" or, "like I'm going to faint," is usually caused by inadequate cerebral perfusion and is classified as? Student Answer: Presyncope Disequilibrium Vertigo Syncope Instructor Explanation: MedU Card #5 Points Received: 0 of 2 Comments: Question 10. Question : It is important to not dilate the eye if ____ is suspected. Student Answer: Cataract Macular degeneration Acute closed-angle glaucoma Chronic open-angle glaucoma Instructor Explanation: If the patient has experienced sudden onset of eye pain, it is important not to dilate the eyes before determining whether acute closed-angle glaucoma is present because dilating the eye may increase the intraocular pressure. (Goolsby 108) Acute glaucoma, also known as angle-closure or narrow-angle glaucoma, is an obstruction to the outflow of aqueous humor from the posterior to the anterior chamber through the trabecular meshwork, canal of Schlemm, and associated structures. It results in an elevation of intraocular pressure, damaging the optic nerve and causing loss of peripheral vision, eye pain, and redness. This type of glaucoma is uncommon but may occur as a primary disease or secondary to other conditions and constitutes an ophthalmic emergency (Kennedy-Malone 161) Points Received: 2 of 2 Comments: Question 11. Question : Mr. GC presents to the clinic with nausea and vomiting for 2 days, prior to that time he reports occasional ‘dizziness’ that got better with change in position. He denies a recent history of URI or any history of headaches or migraines. What would the most likely diagnosis be? Student Answer: Vestibular neruitis Benign paroxysmal positional vertigo Vestibular migraine Benign hypertensive central vertigo Instructor Explanation: MedU Card #9 Points Received: 2 of 2 Comments: Question 12. Question : Which of the following patients with vertigo would require neurologic imaging? Student Answer: A 68-year-old woman with a history of hypertension and sudden acute onset constant vertigo. She has right nystagmus that changes direction with gaze and that does not disappear when she focuses. A 45-year-old man with recurrent episodes of brief intense vertigo every time he turns his head rapidly. He has no other neurologic signs or symptoms. He has a positive Dix-Hallpike maneuver. A 66-year-old man with recurrent episodes of vertigo associated with tinnitus and hearing loss. His head thrust test is positive. A 28-year-old otherwise well woman with new onset constant vertigo with no other neurologic symptoms. On physical exam, she has unidirectional nystagmus that disappears when her gaze is fixed. Instructor Explanation: MedU Card #11. There are multiple reasons to be concerned about a central lesion and possible infarct in this patient. Her age puts her at risk as does her hypertension. Her physical exam shows nystagmus that changes direction and that does not inhibit with focus. Both of these findings are consistent with a central lesion. She needs an urgent MRI. Points Received: 0 of 2 Comments: Question 13. Question : A patient presents with eye redness, scant discharge, and a gritty sensation. Your examination reveals the palpable preauricular nodes, which are most likely with: Student Answer: Bacterial conjunctivitis Allergic conjunctivitis Chemical conjunctivitis Viral conjunctivitis Instructor Explanation: Preauricular nodes are nonpalpable and nontender in allergic conjunctivitis, usually nonpalpable in bacterial conjunctivitis, and palpable in viral conjunctivitis. (Goolsby 112) Points Received: 2 of 2 Comments: Question 14. Question : In assessing the eyes, which of the following is considered a “red flag” finding when associated with eye redness? Student Answer: History of prior red-eye episodes Grossly visible corneal defect Exophthalmos Photophobia Instructor Explanation: Red flag warnings for eye redness include pain (not discomfort or irritation), decreased vision, profuse discharge, and corneal defect grossly visible. (Goolsby 112) Points Received: 2 of 2 Comments: Question 15. Question : A 64-year-old male presents with erythema of the sclera, tearing, and bilateral pruritus of the eyes. The symptoms occur intermittently throughout the year and he has associated clear nasal discharge. Which of the following is most likely because of the inflammation? Student Answer: Bacterium Allergen Virus Fungi Instructor Explanation: Patients with seasonal allergic rhinitis report rhinorrhea, sneezing, obstructed nasal passages, and pruritic eyes, nose, and oropharynx during the spring and fall. Patients with perennial allergic rhinitis have similar symptoms associated with exposure to environmental allergens typically in their homes. Physical examination may reveal a pale, boggy nasal mucosa, injected conjunctiva, enlarged turbinates, dark discoloration or bags under the eyes, and mouth breathing; absence of pale, boggy nasal mucosa does not rule out allergic rhinitis. (Kennedy-Malone 182-183) Points Received: 2 of 2 Comments: Question 16. Question : Patients that have atopic disorders are mediated by the production of Immunoglobulin E (IgE) will have histamine stimulated as an immediate phase response. This release of histamine results in which of the following? Student Answer: Sinus pain, increased vascular permeability, and bronchodilation Bronchospasm, vascular permeability, and vasodilatation Contraction of smooth muscle, decreased vascular permeability, and vasoconstriction Vasodilatation, bronchodilation, and increased vascular permeability Instructor Explanation: Rhinitis may be either allergic or nonallergic. Allergic rhinitis results as a response of the nasal mucosa to airborne allergens in atopic genetically prone individuals. This response is mediated by the production of immunoglobulin E (IgE). IgE antibodies produced in response to the initial and subsequent exposure to allergens bind to the nasal mucosa. With repeated exposure, immediate type 1 hypersensitivity reactions may occur (Simoens & Laekeman, 2009). Antigen-specific T cells are activated through the lymphatic system in response to the antigen. The activated antigen-specific T cells activate B cells, and IgE is created in lymphoid tissue and at local tissue sites (Adelman, Casale, & Corren, 2002; Novak, 2009). The newly created antigen-specific IgE is released by plasma cells and binds to high-affinity IgE receptors located on the basophils and mast cells. This leads to the sensitization of the cells in the tissues of the nose, lung, or skin (Adelman et al., 2002; Cirillo, Pistorio, Tosca, & Ciprandi, 2009). IgE also binds with the antigen protein, beginning degranulation of the mast cells and basophils. These actions start the allergic cascade. Mediators are released as a result of the degranulation and include histamine, proteoglycans, enzymes, leukotrienes, cytokines, and many others. The chain in the release of mediators is responsible for the immediate and late phase responses of the cells. Histamine may be fully released within 30 minutes of degranulation, whereas cytokines may be released over many hours (Adelman et al., 2002; Derendorf & Meltzer, 2008). (Kennedy-Malone 181-182) Points Received: 2 of 2 Comments: Question 17. Question : You have a patient complaining of vertigo and want to know what could be the cause. Knowing there are many causes for vertigo, you question the length of time the sensation lasts. She tells you several hours to days and is accompanied by tinnitus and hearing loss. You suspect which of the following conditions? Student Answer: Ménière’s disease Benign paroxysmal positional vertigo Transient ischemic attack (TIA) Migraine Instructor Explanation: Ménière's disease commonly involves a triad of symptoms—severe vertigo, tinnitus, and hearing loss (Goolsby 140) Points Received: 2 of 2 Comments: Question 18. Question : In examining the mouth of an older adult with a history of smoking, the nurse practitioner finds a suspicious oral lesion. The patient has been referred for a biopsy to be sent for pathology. Which is the most common oral precancerous lesion? Student Answer: Fictional keratosis Keratoacanthoma Lichen planus Leukoplakia Instructor Explanation: The cause of most episodes of leukoplakia is not determined. However, this condition, which results in the development of white patches on the oral mucosa, is associated with an increased risk of oral squamous cell cancer. Risk factors for the development of leukoplakia include chronic/recurrent trauma to the affected site and the use of smokeless and smoked tobacco and alcohol. (Goolsby 152) Points Received: 2 of 2 Comments: Question 19. Question : Rheumatic heart disease is a complication that can arise from which type of infection? Student Answer: Epstein-Barr virus Diphtheria Group A beta hemolytic streptococcus Streptococcus pneumoniae Instructor Explanation: Group A beta-hemolytic streptococcal (GABHS) pharyngitis is a bacterial infection of the pharynx, commonly called strep throat. Complications of GABHS pharyngitis, although rare, include rheumatic heart disease and glomerulonephritis, and the condition requires prompt diagnosis and definitive treatment. Most patients with GABHS pharyngitis are children and youths. Other bacterial causes of pharyngitis include mycoplasmal pneumonia, gonorrhea, and diphtheria. (Goolsby 156) Points Received: 2 of 2 Comments: Question 20. Question : A patient complains of fever, fatigue, and pharyngitis. On physical examination there is pronounced cervical lymphadenopathy. Which of the following diagnostic tests should be considered? Student Answer: Mono spot Strep test Throat culture All of the above Instructor Explanation: The physical examination for sore throat should include a comprehensive assessment of the upper and lower respiratory systems, including ears, nose, mouth, throat, and lungs. The neck assessment should include, at a minimum, assessment of the cervical lymph nodes. Strep screens, throat cultures, and mononucleosis screens are common diagnostic studies used to narrow the differential diagnosis of sore throat. A CBC with differential count is helpful in determining the cause of sore throat. (Goolsby 156) 1. Question : Susan P., a 60-year-old woman with a 30 pack year history, presents to your primary care practice for evaluation of a persistent, daily cough with increased sputum production, worse in the morning, occurring over the past three months. She tells you, “I have the same thing, year after year.” Which of the following choices would you consider strongly in your critical thinking process? Student Answer: Seasonal allergies Acute bronchitis Bronchial asthma Chronic bronchitis Instructor Explanation: The pulmonary component includes an abnormal inflammatory response to noxious stimuli, principally tobacco, but also occupational and environmental pollutants. The hallmark of chronic bronchitis is a daily chronic cough with increased sputum production lasting for at least 3 consecutive months in at least 2 consecutive years, usually worse on awakening; this may or may not be associated with COPD (GOLD, 2011). Emphysema is characterized by obstruction to airflow caused by abnormal airspace enlargement distal to terminal bronchioles. Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. (page 206) & Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file. (page 213) Points Received: 2 of 2 Comments: Question 2. Question : A patient presents complaining of a 5 day history of upper respiratory symptoms including nasal congestion and drainage. On the day the symptoms began he had a low-grade fever that has now resolved. His nasal congestion persisted and he has had yellow nasal drainage for three days associated with mild headaches. On exam he is afebrile and in no distress. Examination of his tympanic membranes and throat are normal. Examination of his nose is unremarkable although a slight yellowish-clear drainage is noted. There is tenderness when you lightly percuss his maxillary sinus. What would your treatment plan for this patient be? Student Answer: Observation and reassurance Treatment with an antibiotic such as amoxicillin Treatment with an antibiotic such as a fluoroquinoline or amoxicillin-clavulanate Combination of a low dose inhaled corticosteroid and a long acting beta2 agonist inhaler. Instructor Explanation: MedU Card #4. According to the American Academy of Ortolaryngology—Head and Neck Surgery Foundation guidelines (2007) on sinusitis, making the distinction between a lingering viral upper respiratory infection that affects the nose and sinuses (viral rhinosinusitis) or early acute bacterial sinusitis can be difficult. It is more likely to be a viral rhinosinusitis if the duration of symptoms is less than ten days and they are not worsening. In this case, you can continue to observe the patient and reassure him that antibiotics are not necessary at this time. Points Received: 2 of 2 Comments: Question 3. Question : Emphysematous changes in the lungs produce the following characteristic in COPD patients? Student Answer: Asymmetric chest expansion Increased lateral diameter Increased anterior-posterior diameter Pectus excavatum Instructor Explanation: In COPD, patients commonly develop a barrel-shaped chest due to emphysematous changes in the lungs. A barrel shape is due to an increased anterior-posterior (AP) diameter. In emphysema, there is a 1:1 ratio of AP to lateral diameter; AP diameter equals the lateral diameter. Normally the AP diameter is twice the lateral diameter. Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file( page 213-214) & Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. (page 206) Points Received: 2 of 2 Comments: Question 4. Question : When palpating the posterior chest, the clinician notes increased tactile fremitus over the left lower lobe. This can be indicative of pneumonia. Areas of increased fremitus should raise the suspicion of conditions resulting in increased solidity or consolidation in the underlying lung tissue, such as in pneumonia, tumor, or pulmonary fibrosis. In the instance of an extensive bronchial obstruction: Student Answer: No palpable vibration is felt Decreased fremitus is felt Increased fremitus is felt Vibration is referred to the non-obstructed lobe Instructor Explanation: Areas of increased fremitus should raise the suspicion of conditions resulting in increased solidity or consolidation in the underlying lung tissue, such as in pneumonia, tumor, or pulmonary fibrosis. Conversely, areas of decreased fremitus raise the suspicion of abnormal fluid- or air-filled spaces, such as occurs with pleural effusion, pneumothorax, or emphysema. In the instance of an extensive bronchial obstruction, no palpable vibration is felt in the related field. Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file. (page 209) & Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. (page 193) Points Received: 2 of 2 Comments: Question 5. Question : Your patient presents with complaint of persistent cough. After you have finished obtaining the History of Present Illness, you realize that the patient may be having episodes of wheezing, in addition to his cough. The most common cause of cough with wheezing is asthma. What of the following physical exam findings will support your tentative diagnosis of asthma? Student Answer: Clear, watery nasal drainage with nasal turbinate swelling Pharyngeal exudate and lymphadenopathy Clubbing, cyanosis and edema. Diminished lung sounds with rales in both bases Instructor Explanation: MedU Card #9 Points Received: 2 of 2 Comments: Question 6. Question : Which of the following imaging studies should be considered if a pulmonary malignancy is suspected? Student Answer: Computed tomography (CT) scan Chest X-ray with PA, lateral, and lordotic views Ultrasound Positron emission tomography (PET) scan Instructor Explanation: For pulmonary malignancy, chest films are often nondiagnostic, although they may reveal a nodule, mass, or other abnormality. A CT scan of the chest is typically diagnostic. Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file. (page 217-218) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. (page 251) Points Received: 2 of 2 Comments: Question 7. Question : A 26-year-old, non-smoker, male presented to your clinic with SOB with exertion. This could be due to: Student Answer: Exercise-induced cough Bronchiectasis Alpha-1 deficiency Pericarditis Instructor Explanation: When younger patients or nonsmokers develop findings consistent with COPD, alpha-1 antitrypsin deficiency should be suspected. Currently, the American Thoracic Society (2003) recommends that all individuals with COPD or asthma with chronic obstructive changes be tested for alpha-1 antitrypsin deficiency. If alpha-1 antitrypsin deficit is suspected, a qualitative serum should be performed as a screen, followed by quantitative study, as indicated. Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file. (page 213) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. (page 206) Points Received: 2 of 2 Comments: Question 8. Question : Upon assessment of respiratory excursion, the clinician notes asymmetric expansion of the chest. One side expands greater than the other. This could be due to: Student Answer: Pneumothorax Pleural effusion Pneumonia Pulmonary embolism Instructor Explanation: The respiratory excursion, or expansion, is determined by placing hands around the patient’s posterior rib cage with the thumbs approximately at the level of the 10th rib between the thumbs, and then asking the patient to take a deep breath and observing the movement of the hands. The motion should be symmetrical. Less than anticipated movement occurs with advanced COPD and many restrictive processes, such as interstitial lung disease. Asymmetry of movement occurs with atelectasis, lobar collapse, pneumothorax, and several other conditions. Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file (page 208-209) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. (pages 193 & 227) Points Received: 2 of 2 Comments: Question 9. Question : A 72-year-old woman and her husband are on a cross-country driving vacation. After a long day of driving, they stop for dinner. Midway through the meal, the woman becomes very short of breath, with chest pain and a feeling of panic. Which of the following problems is most likely? Student Answer: Pulmonary edema Heart failure Pulmonary embolism Pneumonia Instructor Explanation: The problem may occur when these symptoms are attributed to aging or existing comorbidities. Dyspnea (acute onset), anxiety or apprehension, pleuritic chest pain, cough, tachypnea, and accentuation of the pul-monic component of S2 are frequently present and may be accompanied by diaphoresis, syncope, tachycardia, S3 or S4 gallop, hypoxemia, or hemoptysis . Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. (page 246) Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file (page 202) Points Received: 2 of 2 Comments: Question 10. Question : A cough is described as chronic if it has been present for: Student Answer: 2 weeks or more 8 weeks or more 3 months or more 6 months or more Instructor Explanation: Cough is classified as acute (less than 3 weeks in duration), subacute (lasting 3 to 8 weeks), and chronic (8 or more weeks in duration), and these distinctions help to narrow the potential differential diagnoses. Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file. (page 211) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. ((page 206) Points Received: 2 of 2 Comments: Question 11. Question : Testing is necessary for the diagnosis of asthma because history and physical are not reliable means of excluding other diagnoses or determining the extent of lung impairment. What is the study that is used to evaluate upper respiratory symptoms with new onset wheeze? Student Answer: Chest X-ray Methacholine challenge test Spirometry, both with and without bronchodilation Ventilation/perfusion scan Instructor Explanation: MedU Card #10 Points Received: 2 of 2 Comments: Question 12. Question : In classifying the severity of your patient presenting with an acute exacerbation of asthma. You determine that they have moderate persistent symptoms based on the report of symptoms and spirometry readings of the last 3 weeks. The findings that support moderate persistent symptoms include: Student Answer: Symptoms daily with nighttime awakening more than 1 time a week. FEV1 >60%, but predicted <80%. FEV1/FVC reduced 5% Symptoms less than twice a week and less than twice a week nighttime awakening. FEV1 >80% predicted. FEV1/FVC normal Symptoms more than 2 days a week, but not daily. Nighttime awakenings 3-4 times a month. FEV1 >80% predicted. FEV1/FVC normal Symptoms throughout the day with nighttime awakenings every night. FEV1< 60% predicted. FEV1/FVC reduced >5% Instructor Explanation: MedU Card #15 Points Received: 2 of 2 Comments: Question 13. Question : The following criterion is considered a positive finding when determining whether a patient with asthma can be safely monitored and treated at home: Student Answer: Age over 40 Fever greater than 101 Tachypnea greater than 30 breaths/minute Productive cough Instructor Explanation: Decision Rule: CURB-65 provides framework for determining whether the patient diagnosed with community-acquired pneumonia can be safely monitored and treated at home. One point is awarded for each of the following factors present: • Confusion of new onset • BUN greater than 20mg/dL • Respiratory rate of ≥ 30 breaths/minute • Blood pressure is less than 90 mmHg systolic or diastolic ≤ 60 mm Hg • Age 65 or older Patients scoring 3 to 5 typically require hospitalization for observation and therapy. Scores of 0 to 1 indicate likelihood that outpatient management is appropriate. A score of 2 is inconclusive. Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file (page 214-216) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file.( page 241) Points Received: 2 of 2 Comments: Question 14. Question : Medications are chosen based on the severity of asthma. Considering the patient that is diagnosed with moderate persistent asthma, the preferred option for maintenance medication is: Student Answer: High-dose inhaled corticosteroid and leukotriene receptor antagonist Oral corticosteroid—high and low dose as appropriate Short acting beta2 agonist inhaler and theophylline Low dose inhaled corticosteroid and long acting beta2 agonist inhaler Instructor Explanation: MedU Card #16 Points Received: 2 of 2 Comments: Question 15. Question : A 75-year-old patient with community-acquired pneumonia presents with chills, productive cough, temperature of 102.1, pulse 100, respiration 18, BP 90/52, WBC 12,000, and blood urea nitrogen (BUN) 22 mg/dl. He has a history of mild dementia and his mental status is unchanged from his last visit. These findings indicate that the patient: Student Answer: Can be treated as an outpatient Requires hospitalization for treatment Requires a high dose of parenteral antibiotic Can be treated with oral antibiotics Instructor Explanation: Decision Rule: CURB-65 provides framework for determining whether the patient diagnosed with community-acquired pneumonia can be safely monitored and treated at home. One point is awarded for each of the following factors present: • Confusion of new onset • BUN is greater than 20mg/dl • Respiratory rate of ≥ 30 breaths/minute • Blood pressure is less than 90 mmHg systolic or diastolic ≤ 60 mm Hg • Age 65 or older Patients scoring 3 to 5 typically require hospitalization for observation and therapy. Scores of 0 to 1 indicate likelihood that outpatient management is appropriate. A score of 2 is inconclusive. Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file (page 214-216) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. (page 241) Points Received: 0 of 2 Comments: Question 16. Question : Which of the following is considered a “red flag” when diagnosing a patient with pneumonia? Student Answer: Fever of 102 Infiltrates on chest X-ray Pleural effusion on chest X-ray Elevated white blood cell count Instructor Explanation: With pneumonia, the chest film typically reveals an area of infiltrate. It is a red flag if a pleural effusion is also visualized, in which case adequate follow-up to exclude development of an empyema is mandatory. This often involves prompt referral to a pulmonologist for possible thoracentesis. Cultures and Gram stains of sputum are usually not ordered for outpatients. The white blood cell count is often elevated. Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file. (page 214) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. (page 240) Points Received: 2 of 2 Comments: Question 17. Question : A 23-year-old patient who has had bronchiectasis since childhood is likely to have which of the following: Student Answer: Barrel-shaped chest Clubbing Pectus excavatum Prolonged capillary refill Instructor Explanation: In bronchiectasis, there is usually a history of chronic, productive cough. Sputum is typically mucopurulent and produced in increased amounts. Other common findings include shortness of breath, wheezing, fatigue, and possibly hemoptysis. Physical examination reveals rhonchi and/or wheezing. In advanced disease, clubbing and cyanosis may be present. Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file (page 216) Points Received: 2 of 2 Comments: Question 18. Question : Your patient has just returned from a 6-month missionary trip to Southeast Asia. He reports unremitting cough, hemoptysis, and an unintentional weight loss of 10 pounds over the last month. These symptoms should prompt the clinician to suspect: Student Answer: Legionnaires' disease Malaria Tuberculosis Pneumonia Instructor Explanation: Many times, patients with active tuberculosis are essentially symptom free. Some complain of malaise and/or fevers but have no significantly disruptive complaints. When respiratory symptoms occur with tuberculosis, cough is common; the cough is nonproductive at first and is later associated with sputum production. Additionally, patients with tuberculosis may experience progressive dyspnea, night sweats, weight loss, and hemoptysis. It is important to suspect tuberculosis when the patient has travelled to a country where TB is endemic, such as Asia. Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file. (page 217) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. (page 249) Points Received: 2 of 2 Comments: Question 19. Question : A 76-year-old patient with a 200-pack year smoking history presents with complaints of chronic cough, dyspnea, fatigue, hemoptysis, and weight loss over the past 2 months. The physical exam reveals decreased breath sounds and dullness to percussion over the left lower lung field. The chest X-ray demonstrates shift of the mediastinum and trachea to the left. These are classic signs of: Student Answer: Lung cancer Tuberculosis Pneumonia COPD Instructor Explanation: Dyspnea is the most common symptom associated with pleural effusion, but effusion may be accompanied by cough, pain, and systemic symptoms, such as malaise and fever. Abnormal physical findings become evident as the effusion increases in volume. These include decreased lung sounds, dullness over the effusion, decreased fremitus, egophony, and whispered pectoriloquy. With extremely large effusions, the mediastinum and trachea may shift to the opposite side. The exception involves effusion related to malignancy, in which case the mediastinum and trachea may be pulled toward the malignancy. Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file (page 217-218) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file.(page 232) Points Received: 2 of 2 Comments: Question 20. Question : A 24-year-old patient presents to the emergency department after sustaining multiple traumatic injuries after a motorcycle accident. Upon examination, you note tachypnea, use of intercostal muscles to breathe, asymmetric chest expansion, and no breath sounds over the left lower lobe. It is most important to suspect: Student Answer: Pulmonary embolism Pleural effusion Pneumothorax Fracture of ribs Instructor Explanation: Pneumothorax involves air in the pleural cavity. A pneumothorax can occur spontaneously in otherwise healthy individuals or be secondary to trauma or intrinsic lung disease. There is history of sudden onset of shortness of breath associated with chest pain. The patient usually presents in great distress, with tachycardia and tachypnea, and is often splinting the chest. There is decreased fremitus and increased hyperresonance on the affected side. Lung sounds are diminished or absent. The trachea may shift away from the affected side if a large pneumothorax is present. Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file (page 221) 1. Question : Which of the following is the most important question to ask during cardiovascular health history? Student Answer: Number of offspring Last physical exam Sudden death of a family member Use of caffeine Instructor Explanation: The sudden death of a family member is an important question to ask in the health history because it reveals the cardiovascular disease risk of the patient. Sudden death is usually due to an acute cardiovascular event, such as myocardial infarction, cardiac dysrhythmia, or stroke. Family history is particularly important for cardiac assessment because CVD, HTN, hyperlipidemia, and other vascular diseases often have a familial association that is not easily ameliorated by lifestyle changes. If there are deaths in the family related to CVD, determine the age and exact cause of death, because CVD at a young age in the immediate family carries an increased risk compared with CVD in an elderly family member. Ask about sudden death, which might indicate a congenital disease such as Marfan's syndrome. This is especially important to ask during pre-sports physicals because sudden death in athletes is often related to congenital or familial heart disease. Familial hyperlipidemia is autosomal dominant and often leads to CAD and MI at a young age. Family history of obesity and type 2 diabetes are also secondary risk factors for heart disease because the familial tendency for these is strong. Ask about smoking in the house, as secondhand smoke is a risk factor for respiratory and cardiac disease. (Goolsby 167-168) Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file. Points Received: 2 of 2 Comments: Question 2. Question : A key symptom of ischemic heart disease is chest pain. However, angina equivalents may include exertional dyspnea. Angina equivalents are important because: Student Answer: Women with ischemic heart disease many times do not present with chest pain Some patients may have no symptoms or atypical symptoms; diagnosis may only be made at the time of an actual myocardial infarction Elderly patients have the most severe symptoms A & B only Instructor Explanation: The key symptom of IHD is chest pain, but other common symptoms include arm pain, lower jaw pain, shortness of breath, and diaphoresis. These symptoms are referred to as angina equivalents and can also include fatigue or breathlessness. Some patients may have no symptoms or atypical ones so that CAD may not be diagnosed until they experience a myocardial infarction. (Kennedy-Malone 227) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 2 of 2 Comments: Question 3. Question : A 55-year-old post-menopausal woman with a history of hypertension complains of jaw pain on heavy exertion. There were no complaints of chest pain. Her ECG indicates normal sinus rhythm without ST segment abnormalities. Your plan may include: Student Answer: Echocardiogram Exercise stress test Cardiac catheterization Myocardial perfusion imaging Instructor Explanation: Once all the results of the initial laboratory and ECG testing are reviewed, a pretest probability of disease can be generated and additional tests can be ordered.2 The probability of CAD can be calculated by considering the chosen noninvasive test's sensitivity and specificity.2 Selection of the proper cardiac test (see Table 115-1) for an individual depends on the person's risk stratification, age, and tolerable level of activity. The most common and least invasive test for diagnosis of CAD is the stress test, also called the exercise tolerance test (ETT) or treadmill exercise. (Buttaro 488) Buttaro, Terry, JoAnn Trybulski, Patricia Bailey, Joanne Sandberg-Cook. Primary Care, 4th Edition. Mosby, 2013. VitalBook file. Points Received: 2 of 2 Comments: Question 4. Question : Jenny is a 24 year old graduate student that presents to the clinic today with complaints of fever, midsternal chest pain and generalized fatigue for the past two days. She denies any cough or sputum production. She states that when she takes Ibuprofen and rest that the chest pain does seem to ease off. Upon examination the patient presents looking very ill. She is leaning forward and states that this is the most comfortable position for her. Temp is 102. BP= 100/70. Heart rate is 120/min and regular. Upon auscultation a friction rub is audible. Her lung sounds are clear. With these presenting symptoms your initial diagnosis would be: Student Answer: Mitral Valve Prolapse Referred Pain from Cholecystitis Pericarditis Pulmonary Embolus Instructor Explanation: Pericarditis Pericarditis, inflammation of the pericardium, is usually not a solo disease process but is seen in conjunction with other diseases or conditions. Pericarditis may occur as a complication of MI (Dressler's syndrome) or coronary artery bypass surgery. It is also more commonly seen in patients with connective tissue disorders such as rheumatoid arthritis, systemic lupus erythematosus (SLE), scleroderma, and sarcoidosis. Bacterial, viral, or fungal infections, including HIV, are risk factors for pericarditis. Pericarditis can occur with kidney failure or metastatic neoplasias or as a reaction to medication, particularly phenytoin, hydralazine, and procainamide. Rarely, it is idiopathic and the cause unknown, although a common viral infection is suspected. Cardiac tamponade can occur as a serious complication, and it is an emergency requiring immediate pericardiocentesis. Constrictive pericarditis can occur over time due to scarring of the pericardial sac. Signs and Symptoms Unlike the symptoms associated with ACS, the pain accompanying pericarditis is sharp and stabbing; it may worsen with inspiration or when lying flat or leaning forward. Associated symptoms may include shortness of breath, fever, chills, and malaise. (Goolsby 179) Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file. Points Received: 2 of 2 Comments: Question 5. Question : Which symptom is more characteristic of Non-Cardiac chest pain? Student Answer: Pain often radiates to the neck, jaw, epigastrium, shoulder, or arm Pain tends to occur with movement, stretching or palpation Pain usually lasts less than 10 minutes and is relieved by nitroglycerine Pain is aggravated by exertion or stress Instructor Explanation: Palpate chest wall for tenderness and swelling. Chest pain present in only one body position is usually not cardiac in origin. (MSN 194) MSN, Jill C. C., FNP-BC. Family Practice Guidelines: Third Edition, 3rd Edition. Springer Publishing Company, 2014-02-01. VitalBook file. Points Received: 2 of 2 Comments: Question 6. Question : What is the most common valvular heart disease in the older adult? Student Answer: Aortic regurgitation Aortic stenosis Mitral regurgitation Mitral stenosis Instructor Explanation: Age: Present in 2% to 9% of persons over age 65, aortic stenosis is the most clinically significant cardiac valve lesion (Faggiano, 2006). Isolated aortic regurgitation is rarely seen and is usually accompanied by some degree of mitral valve involvement. Mitral regurgitation is more common than mitral stenosis in elderly individuals. Mitral valve disease, commonly caused by rheumatic heart disease, is usually acquired by younger patients; however, the effects may not be seen until they are in their forties or fifties. Mitral valve stenosis has a progressively slow course with latent symptoms over 20 to 40 years followed by rapid acceleration in later life. (Kennedy-Malone 259) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 2 of 2 Comments: Question 7. Question : Jeff, 48 years old, presents to the clinic complaining of fleeting chest pain, fatigue, palpitations, lightheadedness, and shortness of breath. The pain comes and goes and is not associated with activity or exertion. Food does not exacerbate or relieve the pain. The pain is usually located under the left nipple. Jeff is concerned because his father has cardiac disease and underwent a CABG at age 65. The ANP examines Jeff and hears a mid-systolic click at the 4th ICS mid-clavicular area. The ANP knows that this is a hallmark sign of: Student Answer: Angina Pericarditis Mitral valve prolapse Congestive heart failure Instructor Explanation: Mitral valve prolapse Sharp left anterior chest pain, generally occurring in response to stress or emotional events Chest discomfort lasting seconds to days Palpitations and dyspnea Mitral valve click may be noted in systole at left lower sternal border (Buttaro 529) Buttaro, Terry, JoAnn Trybulski, Patricia Bailey, Joanne Sandberg-Cook. Primary Care, 4th Edition. Mosby, 2013. VitalBook file. MVP, also termed click-murmur syndrome, is a variant of mitral regurgitation and occurs in approximately 10% of young women. MVP generally is hemodynamically insignificant and characterized by normal heart size and dynamics, although the process can progress to hemodynamically significant mitral regurgitation. Characteristically, a portion of the mitral valve balloons into the left atrium, giving rise to a midsystolic click followed by a soft grade I murmur that crescendos up to S2. It is high-pitched and is heard best at the apex or left sternal border. Some patients with MVP have only a murmur and no click, and others have only a click and no murmur. (Goolsby 185) Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file. Points Received: 2 of 2 Comments: Question 8. Question : The aging process causes what normal physiological changes in the heart? Student Answer: The heart valve thickens and becomes rigid, secondary to fibrosis and sclerosis Cardiology occurs along with prolapse of the mitral valve and regurgitation Dilation of the right ventricle occurs with sclerosis of pulmonic and tricuspid valves Hypertrophy of the right ventricle Instructor Explanation: The aging process can also have an adverse effect on the cardiac valves. The valves tend to become thick and stiff secondary to arteriosclerosis and atherosclerotic plaques. (Kennedy-Malone 201) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. During the past three decades, with the successful treatment of streptococcal pharyngitis, the etiology has shifted away from rheumatic to calcific. All such cases share a history of 20 to 30years of repetitive mechanical trauma of the blood against the valve, resulting in fibrosis, calcification, and eventually stenosis. This progress of calcification within the valve cusps is usually seen during the latter decades of life. An inflammatory process similar to that affecting the development of atherosclerotic plaques in coronaries may be a possible cause of the progression of AS. It has been noted that early lesions and calcification in AS are comparable to those found in coronary plaques.4 (Buttaro 602) Buttaro, Terry, JoAnn Trybulski, Patricia Bailey, Joanne Sandberg-Cook. Primary Care, 4th Edition. Mosby, 2013. VitalBook file. Points Received: 2 of 2 Comments: Question 9. Question : Dan G., a 65-year-old man, presents to your primary care office for the evaluation of chest pain and left-sided shoulder pain. Pain begins after strenuous activity, including walking. Pain is characterized as dull, aching; 8/10 during activity, otherwise 0/10. Began a few months ago, intermittent, aggravated by exercise, and relieved by rest. Has occasional nausea. Pain is retrosternal, radiating to left shoulder, definitely affects quality of life by limiting activity. Pain is worse today; did not go away after he stopped walking. BP 120/80. Pulse 72 and regular. Normal heart sounds, S1 and S2, no murmurs. Which of the following differential diagnoses would be most likely? Student Answer: Musculoskeletal chest wall syndrome with radiation Esophageal motor disorder with radiation Acute cholecystitis with cholelithiasis Coronary artery disease with angina pectoris Instructor Explanation: With a complaint of chest pain, the most life-threatening diagnosis should be ruled out first. A thorough history identifying the quality and quantity of the pain, alleviating and aggravating factors, and associated symptoms assists in raising or lowering your index of suspicion for a myocardial origin of the pain. Age, gender, weight, vital signs, family history, and medical history also assist in diagnosis. Signs and symptoms that are suspicious for myocardial ischemia include substernal chest pain or discomfort that may radiate into the neck or left arm, diaphoresis, nausea, shortness of breath, and perhaps weakness. Chest discomfort that increases with exertion and resolves with rest or nitroglycerin can indicate myocardial ischemia. Chest discomfort that occurs in the early morning or wakes a patient at night can also be cardiac in origin. Chest discomfort or pain at rest is worrisome because it may signify ACS (unstable angina or an acute MI). Atypical symptoms such as jaw pain, fatigue, indigestion, and upper back pain are more common in women, the elderly, and patients with diabetes. (Goolsby 178-179) Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file Points Received: 2 of 2 Comments: Question 10. Question : A common auscultatory finding in advanced CHF is: Student Answer: Systolic ejection murmur S3 gallop rhythm Friction rub Bradycardia Instructor Explanation: Pathological S3, also called a ventricular gallop, is heard in adults and is associated with decreased myocardial contractility, HF, and volume overload conditions, as can occur with mitral or tricuspid regurgitation. The sound is the same as a physiological S3 and is heard just after S2 with the patient supine or in the left lateral recumbent position. The sound is very soft and can be difficult to hear. (Goolsby 165) Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file. Points Received: 2 of 2 Comments: Question 11. Question : Your 35-year-old female patient complains of feeling palpitations on occasion. The clinician should recognize that palpitations are often a sign of: Student Answer: Anemia Anxiety Hyperthyroidism All of the above Instructor Explanation: Occasional palpitations occur physiologically in the majority of the population or as a result of other noncardiac conditions, such as anxiety, exercise, hyperthyroidism, and anemia. They can also occur with VHD, increased or decreased stroke volume, and arrhythmias. The patient may complain of palpitations or skipped beats, or an arrhythmia may be seen on EKG. Patients are often aware if their heart rate is slower or faster than normal or if it is irregular. With some arrhythmias, patients may complain only of fatigue, shortness of breath, weakness, or syncopal episodes. These are common symptoms in patients who have atrial fibrillation, and, if the ventricular response is slow, the patient may be unaware of the arrhythmia. Ask the patient about the frequency and duration of the palpitations and the presence of associated symptoms, such as loss of consciousness, lightheadedness, chest pain, shortness of breath, nausea, or vomiting. (Goolsby 173) Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file. Points Received: 2 of 2 Comments: Question 12. Question : The best way to diagnose structural heart disease/dysfunction non-invasively is: Student Answer: Chest X-ray EKG Echocardiogram Heart catheterization Instructor Explanation: Echocardiography is recommended in patients with ventricular arrhythmias who are suspected of having structural heart disease (Zipes et al., 2006). An echocardiogram is used more commonly than magnetic resonance imaging (MRI) or cardiac computed tomography (CT) because it is inexpensive in comparison. The echocardiogram is a useful tool in assessing for valvular disorders, left ventricular function and wall motion, and the ejection fraction. (Kennedy-Malone 203) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 2 of 2 Comments: Question 13. Question : During auscultation of the chest, your exam reveals a loud grating sound at the lower anterolateral lung fields, at full inspiration and early expiration. This finding is consistent with: Student Answer: Pneumonia Pleuritis Pneumothorax A and B Instructor Explanation: Adventitious Sounds Description Significance Crackles Coarse, medium, or fine; early, mid-, or late inspiratory Atelectasis, bronchiectasis, congestive heart failure, pulmonary fibrosis Rhonchi, Wheezes Low- or high-pitched; inspiratory or expiratory COPD, acute and chronic bronchitis, asthma, bronchiectasis, pneumonia Friction Rub Loud, grating; late inspiratory–early expiratory Inflamed pleura; pneumonia, pleuritis, malignancy (Goolsby 211) Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file. Points Received: 2 of 2 Comments: Question 14. Question : A 75-year-old patient complains of pain and paresthesias in the right foot that worsens with exercise and is relieved by rest. On physical examination you note pallor of the right foot, capillary refill of 4 seconds in the right foot, +1 dorsalis pedis pulse in the right foot, and +2 pulse in left foot. Which of the following is a likely cause of the signs and symptoms? Student Answer: Arterial insufficiency Femoral vein thrombus Venous insufficiency Peripheral neuropathy Instructor Explanation: Intermittent claudication is pain in the leg or foot that becomes worse with exercise and is relieved by rest. The classic signs of peripheral arterial disease include pain, pallor, weak pulse, paresthesias, and palpable coolness. The signs of venous thrombosis are erythema, ropiness, as well as warmth and tenderness along the course of the vein. Edema of the leg and Homan’s sign of the foot are also common. Note any symptoms of intermittent claudication, such as complaints of cramping, aching, or pain in the ankle, calf, or thigh that occur with exercise and are promptly relieved with rest. (Goolsby 200) Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file. Points Received: 2 of 2 Comments: Question 15. Question : Your patient complains of a feeling of heaviness in the lower legs daily. You note varicosities, edema, and dusky color of both ankles and feet. Which of the following is the most likely cause for these symptoms? Student Answer: Femoral vein thrombosis Femoral artery thrombus Venous insufficiency Musculoskeletal injury Instructor Explanation: Chronic venous insufficiency can be a long-term complication of venous thrombosis owing to the destruction of valves in the deep veins. The calf muscle pump that returns blood from the lower legs is damaged, increasing ambulatory pressure in the calf veins. A constellation of symptoms is set up: aching or pain in the lower legs, edema, thinning and hyperpigmentation of the skin, superficial varicosities, venous stasis, and ulceration. Ankle edema is often the earliest sign. Other causes of chronic venous insufficiency include trauma, pelvic neoplasm, and occasionally secondary to superficial venous disease. Prompt treatment of DVT with anticoagulants decreases the risk for chronic venous insufficiency. General measures for symptom management include the following: elevation of the legs intermittently during the day and at night, avoidance of prolonged sitting or standing, and support or compression stockings. Wearing an Unna boot is valuable and successful in the treatment of stasis ulcers. (Goolsby 203-204) Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file. Points Received: 2 of 2 Comments: Question 16. Question : Your 54 year old patient, Mr. A, presents to your clinic with a 2 day history of severe shoulder pain. On initial assessment you note that in addition to shoulder findings his blood pressure on the ‘good’ arm is 162/100. You review his history and on his last visit his blood pressure was 120/70. He has a medical history of sleep apnea and has used anabolic steroids when body building as a younger adult. In addition to caring for Mr. A’s chief complaint of shoulder pain, you also: Student Answer: Start a thiazide diuretic, discussing the importance of adherence Discuss with him his new diagnosis of hypertension and the importance of taking medication. Schedule a follow up appointment after pain has subsided to take additional blood pressure readings Start an ACE inhibitor because with his history he may also be diabetic. Instructor Explanation: MedU Card #3 Points Received: 2 of 2 Comments: Question 17. Question : You decide to order labs today to help with the diagnosis and management of hypertension in Mr. A. Which of the following labs are indicated to assist in the medical management of Mr. A if he meets the diagnostic criteria for hypertension? Student Answer: Serum Sodium Thyroid function tests Fasting serum cholesterol panel Complete liver function enzyme panel Instructor Explanation: MedU Card #14 Points Received: 2 of 2 Comments: Question 18. Question : Lifestyle modifications reduce blood pressure, enhance antihypertensive medication efficacy, and decrease cardiovascular risks. Which lifestyle change will decrease blood pressure the most? Student Answer: Physical activity Dietary sodium reduction DASH diet Weight reduction Instructor Explanation: MedU Card # 15 Points Received: 2 of 2 Comments: Question 19. Question : Mr. A returns to your clinic and a diagnosis of hypertension is made. He is started on a diuretic and counseled on lifestyle modifications including increasing activity and smoking cessation. On his next visit you note that his blood pressure remains elevated. Before referring to a specialist you should do all of the following except: Student Answer: Assure medications are at appropriate dose Identify any underlying medical condition that requires treatment Review diet with Mr. A and refer to dietician if it is diet problematic Determine he has ‘white coat’ hypertension because his home readings are also elevated Instructor Explanation: MedU Card #22 Points Received: 2 of 2 Comments: Question 20. Question : Mr. A has many issues that seem to be interfering with his health outcomes. In order to negotiate and formulate a patient-centered management plan you take the time to gather more information. This can be started by asking the following question: Student Answer: What do you think caused your hypertension and how has it affected your life? I see that you are 20 pounds overweight -- do you exercise? Does you wife help you to manage your diet and medication? Taking your blood pressure everyday is important so that I can see what happens each day. Do you do this? Instructor Explanation: MedU Card #23 MIDTERM 1. Question : Your 2-year-old patient shows facial features, such as epicanthal folds, up-slanted palpebral fissures, single transverse palmar crease, and a low nasal bridge. These are referred to as: Student Answer: Variable expressivity related to inherited disease Dysmorphic features related to genetic disease De novo mutations of genetic disease Different penetrant signs of genetic disease Points Received: 2 of 2 Comments: Question 2. Question : Presbycusis is the hearing impairment that is associated with: Student Answer: Physiologic aging Ménière’s disease Cerumen impaction Herpes zoster Points Received: 2 of 2 Comments: Question 3. Question : The most common etiologic organism for community-acquired pneumonia is: Student Answer: Streptococcus pneumoniae Beta hemolytic streptococcus Mycoplasma Methicillin resistant staphylococcus Points Received: 2 of 2 Comments: Question 4. Question : The first step in the genomic assessment of a patient is obtaining information regarding: Student Answer: Family history Environmental exposures Lifestyle and behaviors Current medications Points Received: 2 of 2 Comments: Question 5. Question : In examination of the nose, the clinician observes gray, pale mucous membranes with clear, serous discharge. This is most likely indicative of: Student Answer: Bacterial sinusitis Allergic rhinitis Drug abuse Skull fracture Points Received: 2 of 2 Comments: Question 6. Question : A cough is described as chronic if it has been present for: Student Answer: 2 weeks or more 8 weeks or more 3 months or more 6 months or more Points Received: 2 of 2 Comments: Question 7. Question : If it has been determined a patient has esophageal reflux, you should tell them: Student Answer: They probably have a hiatal hernia causing reflux They probably need surgery They should avoid all fruit juices Smoking, alcohol, and caffeine can aggravate their problem Points Received: 2 of 2 Comments: Question 8. Question : Which of the following findings should trigger an urgent referral to a cardiologist or neurologist? Student Answer: History of bright flash of light followed by significantly blurred vision History of transient and painless monocular loss of vision History of monocular severe eye pain, blurred vision, and ciliary flush All of the above Points Received: 2 of 2 Comments: Question 9. Question : A 72-year-old woman and her husband are on a cross-country driving vacation. After a long day of driving, they stop for dinner. Midway through the meal, the woman becomes very short of breath, with chest pain and a feeling of panic. Which of the following problems is most likely? Student Answer: Pulmonary edema Heart failure Pulmonary embolism Pneumonia Points Received: 2 of 2 Comments: Question 10. Question : Which of the following is not a contributing factor to the development of esophagitis in older adults? Student Answer: Increased gastric emptying time Regular ingestion of NSAIDs Decreased salivation Fungal infections such as Candida Points Received: 2 of 2 Comments: Question 11. Question : An older patient reports burning pain after ingestion of many foods and large meals. What assessment would assist the nurse practitioner in making a diagnosis of GERD? Student Answer: Identification of a fluid wave Positive Murphy’s sign Palpable spleen Midepigastric pain that is not reproducible with palpation Points Received: 2 of 2 Comments: Question 12. Question : A 26-year-old, non-smoker, male presented to your clinic with SOB with exertion. This could be due to: Student Answer: Exercise-induced cough Bronchiectasis Alpha-1 deficiency Pericarditis Points Received: 2 of 2 Comments: Question 13. Question : Which of the following findings would indicate a need for another endoscopy in clients with peptic ulcer disease? Student Answer: Cases of dyspepsia with constipation Symptoms persisting after six to eight weeks of therapy All clients with dyspepsia who smoke and drink alcohol When a therapeutic response to empiric treatment is obtained Points Received: 2 of 2 Comments: Question 14. Question : Iron Deficiency Anemia (IDA) is classified as a microcytic, hypochromic anemia. This classification refers to which of the following laboratory data? Student Answer: Hemoglobin and Hematocrit Mean Corpuscular Volume (MCV) and Mean Corpuscular Hemoglobin (MCH) Serum ferritin and Serum iron Total iron binding capacity and transferrin saturation Points Received: 2 of 2 Comments: Question 15. Question : A 20-year-old engineering student complains of episodes of abdominal discomfort, bloating, and episodes of diarrhea. The symptoms usually occur after eating, and pain is frequently relieved with bowel movement. She is on a “celiac diet” and the episodic symptoms persist. Physical examination and diagnostic tests are negative. Colonoscopy is negative for any abnormalities. This is a history and physical consistent with: Student Answer: Inflammatory bowel disease Irritable bowel syndrome Giardiasis Norovirus gastroenteritis Points Received: 0 of 2 Comments: Question 16. Question : An obese middle-aged client presents with a month of nonproductive irritating cough without fever. He also reports occasional morning hoarseness. What should the differential include? Student Answer: Atypical pneumonia Peptic ulcer disease Gastroesophageal reflux Mononucleosis (Epstein-Barr) Points Received: 2 of 2 Comments: Question 17. Question : A 55-year-old post-menopausal woman with a history of hypertension complains of jaw pain on heavy exertion. There were no complaints of chest pain. Her ECG indicates normal sinus rhythm without ST segment abnormalities. Your plan may include: Student Answer: Echocardiogram Exercise stress test Cardiac catheterization Myocardial perfusion imaging Points Received: (not graded) Comments: Question 18. Question : Your 35-year-old female patient complains of feeling palpitations on occasion. The clinician should recognize that palpitations are often a sign of: Student Answer: Anemia Anxiety Hyperthyroidism All of the above Points Received: 2 of 2 Comments: Question 19. Question : A 75-year-old patient with community-acquired pneumonia presents with chills, productive cough, temperature of 102.1, pulse 100, respiration 18, BP 90/52, WBC 12,000, and blood urea nitrogen (BUN) 22 mg/dl. He has a history of mild dementia and his mental status is unchanged from his last visit. These findings indicate that the patient: Student Answer: Can be treated as an outpatient Requires hospitalization for treatment Requires a high dose of parenteral antibiotic Can be treated with oral antibiotics Instructor Explanation: Decision Rule: CURB-65 provides framework for determining whether the patient diagnosed with community-acquired pneumonia can be safely monitored and treated at home. One point is awarded for each of the following factors present: Confusion of new onset BUN is greater than 20mg/dl Respiratory rate of ≥ 30 breaths/minute Blood pressure is less than 90 mmHg systolic or diastolic ≤ 60 mm Hg Age 65 or older Patients scoring 3 to 5 typically require hospitalization for observation and therapy. Scores of 0 to 1 indicate likelihood that outpatient management is appropriate. A score of 2 is inconclusive. Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file (page 214-216) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. (page 241) Points Received: 0 of 2 Comments: Question 20. Question : The major impact of the physiological changes that occur with aging is: Student Answer: Reduced physiological reserve Reduced homeostatic mechanisms Impaired immunological response All of the above Points Received: 2 of 2 Comments: Question 21. Question : Aortic regurgitation requires medical treatment for early signs of CHF with: Student Answer: Beta blockers ACE inhibitors Surgery Hospitalization Points Received: 2 of 2 Comments: Question 22. Question : Which of the following symptoms is common with acute otitis media? Student Answer: Bulging tympanic membrane Bright light reflex of tympanic membrane Increased tympanic membrane mobility All of the above Points Received: 2 of 2 Comments: Question 23. Question : A common auscultatory finding in advanced CHF is: Student Answer: Systolic ejection murmur S3 gallop rhythm Friction rub Bradycardia Points Received: 2 of 2 Comments: Question 24. Question : The best way to diagnose structural heart disease/dysfunction non-invasively is: Student Answer: Chest X-ray EKG Echocardiogram Heart catheterization Points Received: 2 of 2 Comments: Question 25. Question : Which disease process typically causes episodic right upper quadrant pain, epigastric pain or chest pain that can last 4-6 hours or less, often radiates to the back (classically under the right shoulder blade) and is often accompanied by nausea or vomiting and often follows a heavy, fatty meal. Student Answer: Acute pancreatitis Duodenal ulcer Biliary colic Cholecystitis Instructor Explanation: MedU Card #7. Biliary colic typically causes right upper quadrant pain, epigastric pain or chest pain that is constant (the term "colic" is a misnomer), typically lasts 4-6 hours or less, and often radiates to the back (classically under the right shoulder blade). It is often accompanied by nausea or vomiting and often follows a heavy, fatty meal. These symptoms are a result of a stimulated gallbladder (e.g., from a fatty meal) contracting when a gallstone obstructs the outlet of the cystic duct. The hallmark of biliary colic is that the stone is mobile and eventually moves away from the outlet allowing resumption of normal gallbladder function and resolution of symptoms. Points Received: (not graded) Comments: Question 26. Question : Which of the following is the most common cause of heartburn-type epigastric pain? Student Answer: Decreased lower esophageal sphincter tone Helicobacter pylori infection of stomach Esophageal spasm Peptic ulcer disease Points Received: 2 of 2 Comments: Question 27. Question : Jeff, 48 years old, presents to the clinic complaining of fleeting chest pain, fatigue, palpitations, lightheadedness, and shortness of breath. The pain comes and goes and is not associated with activity or exertion. Food does not exacerbate or relieve the pain. The pain is usually located under the left nipple. Jeff is concerned because his father has cardiac disease and underwent a CABG at age 65. The ANP examines Jeff and hears a mid-systolic click at the 4th ICS mid-clavicular area. The ANP knows that this is a hallmark sign of: Student Answer: Angina Pericarditis Mitral valve prolapse Congestive heart failure Points Received: 0 of 2 Comments: Question 28. Question : Which of the following statements is true concerning anti-arrhythmic drugs? Student Answer: Amiodarone is the only one not associated with increased mortality and it has a very favorable side effect profile. Both long-acting and short-acting calcium channel blockers are associated with an increased risk of cardiovascular morbidity and mortality. Most anti-arrhythmics have a low toxic/therapeutic ratio and some are exceedingly toxic. Anti-arrhythmic therapy should be initiated in the hospital for all patients. Points Received: 2 of 2 Comments: Question 29. Question : What is the most common valvular heart disease in the older adult? Student Answer: Aortic regurgitation Aortic stenosis Mitral regurgitation Mitral stenosis Points Received: 2 of 2 Comments: Question 30. Question : Which of the following imaging studies should be considered if a pulmonary malignancy is suspected? Student Answer: Computed tomography (CT) scan Chest X-ray with PA, lateral, and lordotic views Ultrasound Positron emission tomography (PET) scan Points Received: 2 of 2 Comments: Question 31. Question : Which of the following is the most important question to ask during cardiovascular health history? Student Answer: Number of offspring Last physical exam Sudden death of a family member Use of caffeine Points Received: 2 of 2 Comments: Question 32. Question : The first assessment to complete related to the eyes is: Student Answer: Eye lids Visual acuity Extraocular movements Peripheral vision Points Received: 2 of 2 Comments: Question 33. Question : Which of the following medications are commonly associated with the side effect of cough? Student Answer: Beta blocker Diuretic ACE inhibitor Calcium antagonist Points Received: 2 of 2 Comments: Question 34. Question : Patients that have atopic disorders are mediated by the production of Immunoglobulin E (IgE) will have histamine stimulated as an immediate phase response. This release of histamine results in which of the following? Student Answer: Sinus pain, increased vascular permeability, and bronchodilation Bronchospasm, vascular permeability, and vasodilatation Contraction of smooth muscle, decreased vascular permeability, and vasoconstriction Vasodilatation, bronchodilation, and increased vascular permeability Points Received: 2 of 2 Comments: Question 35. Question : A nurse practitioner reports that your patient’s abdominal X-ray demonstrates multiple air-fluid levels in the bowel. This is a diagnostic finding found in: Student Answer: Appendicitis Cholecystitis Bowel Obstruction Diverticulitis Points Received: 2 of 2 Comments: Question 36. Question : According to the Genetic Information Nondiscrimination Act (GINA): Student Answer: Nurse Practitioners (NPs) should keep all genetic information of patients confidential NPs must obtain informed consent prior to genetic testing of all patients Employers cannot inquire about an employee’s genetic information All of the above Points Received: 2 of 2 Comments: Question 37. Question : Which of the following would be considered a “red flag” that requires more investigation in a patient assessment? Student Answer: Colon cancer in family member at age 70 Breast cancer in family member at age 75 Myocardial infarction in family member at age 35 All of the above Points Received: 2 of 2 Comments: Question 38. Question : A 59-year-old patient with history of alcohol abuse comes to your office because of ‘throwing up blood”. On physical examination, you note ascites and caput medusa. A likely cause for the hematemesis is: Student Answer: Peptic ulcer disease Barrett’s esophagus Esophageal varices Pancreatitis Points Received: 2 of 2 Comments: Question 39. Question : A 64-year-old male presents with erythema of the sclera, tearing, and bilateral pruritus of the eyes. The symptoms occur intermittently throughout the year and he has associated clear nasal discharge. Which of the following is most likely because of the inflammation? Student Answer: Bacterium Allergen Virus Fungi Points Received: 2 of 2 Comments: Question 40. Question : Your patient complains of lower abdominal pain, anorexia, extreme fatigue, unintentional weight loss of 10 pounds in last 3 weeks, and you find a positive hemoccult on digital rectal examination. Laboratory tests show iron deficiency anemia. The clinician needs to consider: Student Answer: Diverticulitis Colon cancer Appendicitis Peptic ulcer disease 1. Question : Which ethnic group has the highest incidence of prostate cancer? Student Answer: Asians Hispanics African Americans American Indians Instructor Explanation: Ethnicity: African Americans have the highest incidence of prostate cancer in the world, with Asian and Hispanic men at lower risk than white men (Wilbur, 2008). Diagnosis in African Americans tends to be at a more advanced stage, and disease- specific survival is lower in this group (Prostate cancer, 2012). (Kennedy-Malone 378) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 2 of 2 Comments: Question 2. Question : Men with an initial PSA level below 2.5 ng/ml can reduce their screening frequency to what intervals? Student Answer: Every 6 months Yearly Every 2 years Every 2 to 4 years Instructor Explanation: Education: Review risk factors and significance of reporting family history. Encourage screening per health-care providers' recommendations and current guidelines. CLINICAL RECOMMENDATION EVIDENCE RATING REFERENCES Screening, when completed, is recommended with PSA with or without digital rectal examination. A Wolf et al. (2010) Screening should be conducted yearly for men whose PSA levels are ≥2.5 ng/mL. A Wolf et al. (2010) For men whose PSA is <2.5 ng/mL, screening intervals can be extended to every 2 years. A Wolf et al. (2010) A PSA level of ≥4.0 ng/mL historically has been used to recommend referral for further evaluation or biopsy. A Wolf et al. (2010) The USPSTF recommends against PSA screening for prostate cancer. C USPSTF (2012) A = consistent, good-quality, patient-oriented evidence; B = inconsistent or limited-quality, patient-oriented evidence; C = consensus, disease-oriented evidence, usual practice, expert opinion, or case series. For information about the SORT evidence rating system, go to www.aafp.org/afpsort.xml. (Kennedy-Malone 380) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 2 of 2 Comments: Question 3. Question : Your 55-year-old male patient presents to your office with complaints of sudden development of severe right-sided, colicky lower abdominal pain. He cannot sit still on the examining table. The patient has previously been in good health. On physical examination, there are no signs of peritoneal inflammation. A urine sample reveals hematuria and crystalluria. Which is the next diagnostic test that should be done immediately? Student Answer: Ultrasound of the abdomen Abdominal X-ray Digital rectal examination Spiral CT scan Instructor Explanation: The initial study can be a KUB or IVP; however, many facilities can perform a stone protocol spiral CT, a much more definitive test for the evaluation of kidney stones. CT can demonstrate filling defects. CT scan is a highly specific and sensitive test for urinary tract calculi. After the initial evaluation with CT scan, pain reliever can be administered. An IVP can be done at another time when the patient can better prepare for the test. Goolsby. Points Received: 2 of 2 Comments: Question 4. Question : The most common complication of an untreated urinary obstruction due to a ureteral calculus is: Student Answer: Ureteral rupture Hydronephrosis Kidney mass Renal artery stenosis Instructor Explanation: Hydronephrosis is swelling of the renal pelvis caused by an obstructing stone, ureteral stricture, prostatic hyperplasia, or renal or abdominal tumor that prevents the kidney from draining. The obstruction can be unilateral or bilateral, symptoms can be sudden or gradual in onset, and progressive renal damage will occur with time. Goolsby Points Received: 2 of 2 Comments: Question 5. Question : A 43-year-old male patient complains of right-sided abdominal and pain in the back in the right costovertebral angle region, fever, chills, dysuria, and nausea. On physical examination, there is 102 degree fever, tachycardia, and right costovertebral angle tenderness to percussion. The most likely condition is: Student Answer: Lower urinary tract infection Nephrolithiasis Hydronephrosis Pyelonephritis Instructor Explanation: Pyelonephritis is a bacterial infection of the renal pelvis and parenchyma, typically caused by Escherichia coli ascending from the lower urinary tract. The patient will have bilateral or unilateral flank pain, fever, chills, nausea, and vomiting, and LUTS, such as dysuria, may also be present. The patient will appear ill on presentation, with fever and tachycardia commonly noted. Palpation and/or percussion over the infected side is painful. There may be accompanying abdominal discomfort or abdominal distension. Goolsby Points Received: 2 of 2 Comments: Question 6. Question : On a physical examination for employment, a 45-year-old male shows no significant findings and takes no medications. Past medical history and surgery are unremarkable. On urinalysis, hematuria is present. The urinalysis is repeated on another day and still reveals microscopic hematuria. It is important to recognize that painless hematuria can be diagnostic of: Student Answer: Urinary tract infection Bladder cancer Nephrolithiasis Pyelonephritis Instructor Explanation: Approximately 80% to 90% of patients with bladder cancer present with painless gross hematuria. All patients with this classic presentation should be considered to have bladder cancer until proof to the contrary. Patients should be referred to a urologist. They usually undergo cystoscopy to rule out bladder tumor. The majority of patients with bladder cancer present with no urinary tract symptoms or palpable masses. Goolsby Points Received: 2 of 2 Comments: Question 7. Question : On DRE, you note that a 45-year-old patient has a firm, smooth, non-tender but asymmetrically shaped prostate. The patient has no symptoms and has a normal urinalysis. The patient’s PSA is within normal limits for the patient’s age. The clinician should: Student Answer: Refer the patient for transrectal ultrasound guided prostate biopsy Obtain an abdominal X-ray of kidneys, ureter, and bladder Recognize this as a normal finding that requires periodic follow up Obtain urine culture and sensitivity for prostatitis Instructor Explanation: An asymmetric prostate is typically asymptomatic and not necessarily diagnostic of prostate cancer; asymmetry can be a normal finding on DRE but should be followed periodically to monitor for changes. Age-specific reference ranges for PSA (see Table 11.4) should be used as a guide when there is no previous PSA for comparison. A prostatic nodule found on DRE necessitates a referral to a urologist or radiologist for transrectal ultrasound-guided prostate biopsy and may well be the first indication of the presence of a cancer. Goolsby Points Received: 2 of 2 Comments: Question 8. Question : Age-related changes in the bladder, urethra, and ureters include all of the following in older women except: Student Answer: Increased estrogen production’s influence on the bladder and ureter Decline in bladder outlet function Decline in ureteral resistance pressure Laxity of the pelvic muscle Instructor Explanation: Contributing factors: Estrogen-deficient states accompanying metabolic disorders and changes of normal aging create the risk of atrophic vaginitis. Changes in vaginal epithelium and pH caused by estrogen deficiency provide an environment in which pathogenic bacteria and fungi can flourish. Drugs also may alter vaginal secretions and clinical findings (Bachmann & Santen, 2011b). Signs and symptoms: Itching, discomfort, burning, dyspareunia, and, at times, a thin blood-tinged vaginal discharge or bleeding after intercourse as the epithelium thins characterize atrophic vaginitis. As vaginal secretions decrease, vaginal dryness can be another bothersome symptom. Complaints of urinary frequency, urgency, and stress incontinence are common. On physical examination, signs include pale, dry, nonrugated vaginal walls with patches of erythema or petechiae or both. The vaginal canal is short and narrow. A watery white vaginal discharge without foul odor may be found. Estrogen deficiency can lead to loss of uterine support and subsequent uterine descensus (Tan, Bradshaw, & Carr, 2012). (Kennedy-Malone 362) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 2 of 2 Comments: Question 9. Question : Mr. Jones is a 68-year-old retired Air Force pilot that has been diagnosed with prostate cancer in the past week. He has never had a surgical procedure in his life and seeks clarification on the availability of treatments for prostate cancer. He asks the nurse practitioner to tell him the side effects of a radical prostatectomy. Which of the following is not a potential side effect of this procedure? Student Answer: Urinary incontinence Impotence Dribbling urine Selected low back pain Instructor Explanation: Sequelae: Complications of treatment may include incontinence, ED, mild colitis, and radiation cystitis. After nerve-sparing prostatectomy, urinary continence returns in under 6 months in about 50% of men. The rate of ED after external beam radiation ranges from 10% to 80%, and with brachytherapy approximately 15% to 60% (Ali & Walsh, 2011). (Kennedy-Malone 379) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 2 of 2 Comments: Question 10. Question : Your 77-year-old patient complains of frequent urination, hesitation in getting the stream started, and nocturnal frequency of urination that is bothersome. On DRE, there is an enlarged, firm, non-tender, smooth prostate. The clinician should recognize these as symptoms of: Student Answer: Urethritis Benign prostatic hyperplasia Prostatitis Prostate cancer Instructor Explanation: BPH is an enlargement of the transition zone of the prostate gland which occurs as men age. An enlarged prostate causes symptoms that include urinary urgency, frequency, hesitation in getting the stream started, decreased caliber and force of stream, and nocturnal frequency of urination that is bothersome. This collection of symptoms has also been termed prostatism. A patient with BPH shows symmetric or asymmetric enlargement and a firm, smooth, non-tender gland. Goolsby Points Received: 2 of 2 Comments: Question 11. Question : Your 24-year-old female patient complains of dysuria as well as frequency and urgency of urination that develops the day after she uses her diaphragm. Urine culture reveals a bacterial count of 100 CFU/mL. These signs and symptoms indicate: Student Answer: Upper urinary tract infection Normal bacteriuria Lower urinary tract infection Urethritis Instructor Explanation: In women whose symptoms suggest uncomplicated UTI, a culture of greater than 102 CFU/mL of a specific bacterium is indicative of cystitis. However, this CFU number is controversial. Infectious disease specialists recommend use of 103 CFU / mL as diagnostic of UTI. In the past, a bacterial count of 105 CFU/mL was regarded as significant for UTI. UTI diagnosis relies on the patient’s subjective report of symptoms of UTI, not only the number of bacteria. Patients with asymptomatic bacteriuria can have bacterial counts as high as 10 5 CFU/mL. Asymptomatic bacteriuria is not treated. Risk factors for the development of a UTI include increasing age, recent sexual intercourse, a history of UTI, use of a diaphragm or cervical cap, and anatomic abnormalities. Goolsby Points Received: 2 of 2 Comments: Question 12. Question : A 79-year-old man is being evaluated for frequent urinary dribbling without burning. Physical examination reveals a smooth but slightly enlarged prostate gland. His PSA level is 3.3 ng/ml. The patient undergoes formal urodynamic studies, and findings are as follows: a decreased bladder capacity of 370 ml; a few involuntary detrusor contractions at a low bladder volume of 246 mL; an increased postvoid residual urine volume of 225 ml; and a slightly decreased urinary flow rate. Which of the following is not consistent with a normal age-associated change? Student Answer: PSA level of 3.3 ng/ml Decreased bladder capacity Involuntary detrusor contradictions Increased postvoid residual urine volume Instructor Explanation: Signs and symptoms: Symptoms are lower urinary tract symptoms (LUTS), occur on a continuum, and do not necessarily reflect the degree of prostatic enlargement. The onset of symptoms is gradual and includes increased frequency of urination, nocturia, hesitancy, urgency, and weak urinary stream. These symptoms are not specific for BPH and progress gradually over a period of years. (Kennedy-Malone 373) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 2 of 2 Comments: Question 13. Question : Mrs. L. Billings is a 77-year-old Caucasian female who has a history of breast cancer. She has been in remission for 6 years. As her primary care provider, you are seeing her for follow-up of her recent complaint of intermittent abdominal pain of a 3-month duration and some general malaise. Given the brief history above, what will you direct your assessment at during physical examination? Student Answer: Examination of her thyroid to rule out thyroid nodules that may contribute to her feeling fatigued. Auscultation of her abdomen for abnormal bowel sounds to rule out peritonitis. Thorough abdominal and gynecological exam to rule out masses and identify any tenderness. A rectal examination to rule out colon cancer as a secondary site for breast cancer. Instructor Explanation: Signs and symptoms: Ovarian cancer may be totally asymptomatic. The woman may experience pelvic or abdominal pain or pressure, bloating, early satiety, or urinary symptoms (frequency/urgency). Because many of these symptoms are nonspecific and occur with other health conditions, they are frequently overlooked by patient and health-care professional alike (Vaughan et al., 2011). Diagnostic tests: Pelvic examination is recommended in all sexually active women on the schedule determined by the American College of Obstetricians and Gynecologists. Rectovaginal examination may be necessary to detect ovarian enlargement. Ovarian enlargement cannot always be palpated, making pelvic examination a limited diagnostic test. (Kennedy-Malone 371) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 2 of 2 Comments: Question 14. Question : A 27-year-old male comes in to the clinic for symptoms of dysuria, urinary frequency, as well as urgency and perineal pain. Transrectal palpation of the prostate reveals a very tender, boggy, swollen prostate. The clinician should recognize these as signs of: Student Answer: Prostatitis Prostate cancer Urethritis Benign prostatic hyperplasia Instructor Explanation: Prostatitis is an acute or chronic infection of the prostate gland. Acute bacterial prostatitis is usually the result of infection by aerobic gram-negative rods (coliform bacteria or Pseudomonas). Enterococcus faecalis, an aerobic gram-positive bacteria, can also cause prostatitis. Routes of infection are ascent from the urethra, reflux of infected urine into the prostatic ducts, direct extension of bacteria, and migration via the lymphatic and vascular system. Acute symptoms commonly include fever, low back and perineal pain, possible penis pain, urinary urgency and frequency, nocturia, dysuria, and muscle and joint aches. Transrectal palpation of the prostate reveals a very tender, boggy, swollen prostate. Goolsby Points Received: 2 of 2 Comments: Question 15. Question : Which of the following males would be at greatest risk for testicular cancer? Student Answer: John, a 52-year-old, married African American Attorney who lives in Detroit, MI Jacob, a 22-year-old, homosexual male, who works as an accountant, resides in Cumming GA, and has a history of cryptorchidism Andy, a 27-year-old, Caucasian, single male who resides in Waukesha, WI and works as a maintenance mechanic Ryan, a 34-year-old healthy, married man from Sweden, who works as a Registered Nurse in Boston, MA Instructor Explanation: Malignant tumors of the testes are uncommon, usually present between the ages of 15 and 35, are slightly more common on the right side, and arise from germ cells. The greatest risk factor for the development of a testicular tumor is cryptorchidism, with an overall incidence of 7% to 10% in the patient with a history of unilateral or bilateral undescended testes. Increased screening and early detection have significantly decreased the mortality from this malignancy, but up to 10% of patients present with pain and/or constitutional or pulmonary complaints that indicate metastasis. (Goolsby 337) Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file. Points Received: 2 of 2 Comments: Question 16. Question : A 43-year-old male patient complains of right-sided abdominal and pain in the back in the right costovertebral angle region, fever, chills, dysuria, and nausea. On physical examination, there is 102 degree fever, tachycardia, and right costovertebral angle tenderness to percussion. The most likely condition is: Student Answer: Lower urinary tract infection Pyelonephritis Nephrolithiasis Hydonephrosis Points Received: 2 of 2 Comments: Question 17. Question : Which of the following disorders can cause urinary incontinence? Student Answer: Cystocele Overactive bladder Uterine prolapse All of the above Instructor Explanation: Cystocele and prolapse of the uterus can affect pelvic floor anatomy and cause urinary changes, including incontinence and changes to the quality of the urinary stream. Overactive bladder is a cause of incontinence due to atrophic changes of the pelvic floor muscles. Goolsby Points Received: 2 of 2 Comments: Question 18. Question : Your 18 year old sexually active patient presents with sudden right sided groin pain that is sharp and constant. Inspection of his genitals reveals a swollen and erythematous right scrotum. His right testicle is exquisitely tender, swollen and has no palpable masses. Elevation of the testis results in no reduction in pain. The left scrotum and the testicle are normal. Epididymis and other scrotal contents were within normal limits. The scrotum does not transilluminate. Cremasteric reflex is present on the left side but absent on the right. There is no penile discharge, inguinal lymphadenopathy, or hernias. Based on the history and physical exam your immediate concern is for: Student Answer: Torsion Infection Cancer Rupture Instructor Explanation: MedU Card #11 Points Received: 2 of 2 Comments: Question 19. Question : The Prehn sign is utilized to distinguish epididymitis from testicular torsion. Epididymitis is considered when the Prehn sign is positive. When is the Prehn sign determined to be positive? Student Answer: Pain is relieved by lifting of the testicle. Tenderness is limited to the upper pole of the testis. Lightly stroking or pinching the superior medial aspect of the thigh causes testicular retraction. A small bluish discoloration is visible through the skin in the upper pole. Instructor Explanation: MedU Card # 6. Prehn reported that physical lifting of the testicles relieves the pain caused by epididymitis but not pain caused by testicular torsion. A positive Prehn sign is pain that is relieved by lifting of the testicle; if present this can help distinguish epididymitis from testicular torsion. Points Received: 2 of 2 Comments: Question 20. Question : Which of the following exam findings makes the diagnosis of testicular tumor more likely? Student Answer: A scrotal mass that is accompanied by exquisite tenderness. Testicular swelling is mostly fluid and transilluminates easily A testicular mass that is non-tender to palpation Dilated and tortuous veins in the pampiniform plexus Instructor Explanation: MedU Card #9. Testicular tumor presents as scrotal mass that is rarely accompanied by tenderness. The swelling is solid so should not transilluminate. A testicular tumor is usually non-tender to palpation. Points Received: 2 of 2 Comments: 1. Question : Which ethnic group has the highest incidence of prostate cancer? Student Answer: Asians Hispanics African Americans American Indians Instructor Explanation: Ethnicity: African Americans have the highest incidence of prostate cancer in the world, with Asian and Hispanic men at lower risk than white men (Wilbur, 2008). Diagnosis in African Americans tends to be at a more advanced stage, and disease- specific survival is lower in this group (Prostate cancer, 2012). (Kennedy-Malone 378) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 2 of 2 Comments: Question 2. Question : Men with an initial PSA level below 2.5 ng/ml can reduce their screening frequency to what intervals? Student Answer: Every 6 months Yearly Every 2 years Every 2 to 4 years Instructor Explanation: Education: Review risk factors and significance of reporting family history. Encourage screening per health-care providers' recommendations and current guidelines. CLINICAL RECOMMENDATION EVIDENCE RATING REFERENCES Screening, when completed, is recommended with PSA with or without digital rectal examination. A Wolf et al. (2010) Screening should be conducted yearly for men whose PSA levels are ≥2.5 ng/mL. A Wolf et al. (2010) For men whose PSA is <2.5 ng/mL, screening intervals can be extended to every 2 years. A Wolf et al. (2010) A PSA level of ≥4.0 ng/mL historically has been used to recommend referral for further evaluation or biopsy. A Wolf et al. (2010) The USPSTF recommends against PSA screening for prostate cancer. C USPSTF (2012) A = consistent, good-quality, patient-oriented evidence; B = inconsistent or limited-quality, patient-oriented evidence; C = consensus, disease-oriented evidence, usual practice, expert opinion, or case series. For information about the SORT evidence rating system, go to www.aafp.org/afpsort.xml. (Kennedy-Malone 380) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 2 of 2 Comments: Question 3. Question : Your 55-year-old male patient presents to your office with complaints of sudden development of severe right-sided, colicky lower abdominal pain. He cannot sit still on the examining table. The patient has previously been in good health. On physical examination, there are no signs of peritoneal inflammation. A urine sample reveals hematuria and crystalluria. Which is the next diagnostic test that should be done immediately? Student Answer: Ultrasound of the abdomen Abdominal X-ray Digital rectal examination Spiral CT scan Instructor Explanation: The initial study can be a KUB or IVP; however, many facilities can perform a stone protocol spiral CT, a much more definitive test for the evaluation of kidney stones. CT can demonstrate filling defects. CT scan is a highly specific and sensitive test for urinary tract calculi. After the initial evaluation with CT scan, pain reliever can be administered. An IVP can be done at another time when the patient can better prepare for the test. Goolsby. Points Received: 2 of 2 Comments: Question 4. Question : The most common complication of an untreated urinary obstruction due to a ureteral calculus is: Student Answer: Ureteral rupture Hydronephrosis Kidney mass Renal artery stenosis Instructor Explanation: Hydronephrosis is swelling of the renal pelvis caused by an obstructing stone, ureteral stricture, prostatic hyperplasia, or renal or abdominal tumor that prevents the kidney from draining. The obstruction can be unilateral or bilateral, symptoms can be sudden or gradual in onset, and progressive renal damage will occur with time. Goolsby Points Received: 2 of 2 Comments: Question 5. Question : A 43-year-old male patient complains of right-sided abdominal and pain in the back in the right costovertebral angle region, fever, chills, dysuria, and nausea. On physical examination, there is 102 degree fever, tachycardia, and right costovertebral angle tenderness to percussion. The most likely condition is: Student Answer: Lower urinary tract infection Nephrolithiasis Hydronephrosis Pyelonephritis Instructor Explanation: Pyelonephritis is a bacterial infection of the renal pelvis and parenchyma, typically caused by Escherichia coli ascending from the lower urinary tract. The patient will have bilateral or unilateral flank pain, fever, chills, nausea, and vomiting, and LUTS, such as dysuria, may also be present. The patient will appear ill on presentation, with fever and tachycardia commonly noted. Palpation and/or percussion over the infected side is painful. There may be accompanying abdominal discomfort or abdominal distension. Goolsby Points Received: 2 of 2 Comments: Question 6. Question : On a physical examination for employment, a 45-year-old male shows no significant findings and takes no medications. Past medical history and surgery are unremarkable. On urinalysis, hematuria is present. The urinalysis is repeated on another day and still reveals microscopic hematuria. It is important to recognize that painless hematuria can be diagnostic of: Student Answer: Urinary tract infection Bladder cancer Nephrolithiasis Pyelonephritis Instructor Explanation: Approximately 80% to 90% of patients with bladder cancer present with painless gross hematuria. All patients with this classic presentation should be considered to have bladder cancer until proof to the contrary. Patients should be referred to a urologist. They usually undergo cystoscopy to rule out bladder tumor. The majority of patients with bladder cancer present with no urinary tract symptoms or palpable masses. Goolsby Points Received: 2 of 2 Comments: Question 7. Question : On DRE, you note that a 45-year-old patient has a firm, smooth, non-tender but asymmetrically shaped prostate. The patient has no symptoms and has a normal urinalysis. The patient’s PSA is within normal limits for the patient’s age. The clinician should: Student Answer: Refer the patient for transrectal ultrasound guided prostate biopsy Obtain an abdominal X-ray of kidneys, ureter, and bladder Recognize this as a normal finding that requires periodic follow up Obtain urine culture and sensitivity for prostatitis Instructor Explanation: An asymmetric prostate is typically asymptomatic and not necessarily diagnostic of prostate cancer; asymmetry can be a normal finding on DRE but should be followed periodically to monitor for changes. Age-specific reference ranges for PSA (see Table 11.4) should be used as a guide when there is no previous PSA for comparison. A prostatic nodule found on DRE necessitates a referral to a urologist or radiologist for transrectal ultrasound-guided prostate biopsy and may well be the first indication of the presence of a cancer. Goolsby Points Received: 2 of 2 Comments: Question 8. Question : Age-related changes in the bladder, urethra, and ureters include all of the following in older women except: Student Answer: Increased estrogen production’s influence on the bladder and ureter Decline in bladder outlet function Decline in ureteral resistance pressure Laxity of the pelvic muscle Instructor Explanation: Contributing factors: Estrogen-deficient states accompanying metabolic disorders and changes of normal aging create the risk of atrophic vaginitis. Changes in vaginal epithelium and pH caused by estrogen deficiency provide an environment in which pathogenic bacteria and fungi can flourish. Drugs also may alter vaginal secretions and clinical findings (Bachmann & Santen, 2011b). Signs and symptoms: Itching, discomfort, burning, dyspareunia, and, at times, a thin blood-tinged vaginal discharge or bleeding after intercourse as the epithelium thins characterize atrophic vaginitis. As vaginal secretions decrease, vaginal dryness can be another bothersome symptom. Complaints of urinary frequency, urgency, and stress incontinence are common. On physical examination, signs include pale, dry, nonrugated vaginal walls with patches of erythema or petechiae or both. The vaginal canal is short and narrow. A watery white vaginal discharge without foul odor may be found. Estrogen deficiency can lead to loss of uterine support and subsequent uterine descensus (Tan, Bradshaw, & Carr, 2012). (Kennedy-Malone 362) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 2 of 2 Comments: Question 9. Question : Mr. Jones is a 68-year-old retired Air Force pilot that has been diagnosed with prostate cancer in the past week. He has never had a surgical procedure in his life and seeks clarification on the availability of treatments for prostate cancer. He asks the nurse practitioner to tell him the side effects of a radical prostatectomy. Which of the following is not a potential side effect of this procedure? Student Answer: Urinary incontinence Impotence Dribbling urine Selected low back pain Instructor Explanation: Sequelae: Complications of treatment may include incontinence, ED, mild colitis, and radiation cystitis. After nerve-sparing prostatectomy, urinary continence returns in under 6 months in about 50% of men. The rate of ED after external beam radiation ranges from 10% to 80%, and with brachytherapy approximately 15% to 60% (Ali & Walsh, 2011). (Kennedy-Malone 379) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 2 of 2 Comments: Question 10. Question : Your 77-year-old patient complains of frequent urination, hesitation in getting the stream started, and nocturnal frequency of urination that is bothersome. On DRE, there is an enlarged, firm, non-tender, smooth prostate. The clinician should recognize these as symptoms of: Student Answer: Urethritis Benign prostatic hyperplasia Prostatitis Prostate cancer Instructor Explanation: BPH is an enlargement of the transition zone of the prostate gland which occurs as men age. An enlarged prostate causes symptoms that include urinary urgency, frequency, hesitation in getting the stream started, decreased caliber and force of stream, and nocturnal frequency of urination that is bothersome. This collection of symptoms has also been termed prostatism. A patient with BPH shows symmetric or asymmetric enlargement and a firm, smooth, non-tender gland. Goolsby Points Received: 2 of 2 Comments: Question 11. Question : Your 24-year-old female patient complains of dysuria as well as frequency and urgency of urination that develops the day after she uses her diaphragm. Urine culture reveals a bacterial count of 100 CFU/mL. These signs and symptoms indicate: Student Answer: Upper urinary tract infection Normal bacteriuria Lower urinary tract infection Urethritis Instructor Explanation: In women whose symptoms suggest uncomplicated UTI, a culture of greater than 102 CFU/mL of a specific bacterium is indicative of cystitis. However, this CFU number is controversial. Infectious disease specialists recommend use of 103 CFU / mL as diagnostic of UTI. In the past, a bacterial count of 105 CFU/mL was regarded as significant for UTI. UTI diagnosis relies on the patient’s subjective report of symptoms of UTI, not only the number of bacteria. Patients with asymptomatic bacteriuria can have bacterial counts as high as 10 5 CFU/mL. Asymptomatic bacteriuria is not treated. Risk factors for the development of a UTI include increasing age, recent sexual intercourse, a history of UTI, use of a diaphragm or cervical cap, and anatomic abnormalities. Goolsby Points Received: 2 of 2 Comments: Question 12. Question : A 79-year-old man is being evaluated for frequent urinary dribbling without burning. Physical examination reveals a smooth but slightly enlarged prostate gland. His PSA level is 3.3 ng/ml. The patient undergoes formal urodynamic studies, and findings are as follows: a decreased bladder capacity of 370 ml; a few involuntary detrusor contractions at a low bladder volume of 246 mL; an increased postvoid residual urine volume of 225 ml; and a slightly decreased urinary flow rate. Which of the following is not consistent with a normal age-associated change? Student Answer: PSA level of 3.3 ng/ml Decreased bladder capacity Involuntary detrusor contradictions Increased postvoid residual urine volume Instructor Explanation: Signs and symptoms: Symptoms are lower urinary tract symptoms (LUTS), occur on a continuum, and do not necessarily reflect the degree of prostatic enlargement. The onset of symptoms is gradual and includes increased frequency of urination, nocturia, hesitancy, urgency, and weak urinary stream. These symptoms are not specific for BPH and progress gradually over a period of years. (Kennedy-Malone 373) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 2 of 2 Comments: Question 13. Question : Mrs. L. Billings is a 77-year-old Caucasian female who has a history of breast cancer. She has been in remission for 6 years. As her primary care provider, you are seeing her for follow-up of her recent complaint of intermittent abdominal pain of a 3-month duration and some general malaise. Given the brief history above, what will you direct your assessment at during physical examination? Student Answer: Examination of her thyroid to rule out thyroid nodules that may contribute to her feeling fatigued. Auscultation of her abdomen for abnormal bowel sounds to rule out peritonitis. Thorough abdominal and gynecological exam to rule out masses and identify any tenderness. A rectal examination to rule out colon cancer as a secondary site for breast cancer. Instructor Explanation: Signs and symptoms: Ovarian cancer may be totally asymptomatic. The woman may experience pelvic or abdominal pain or pressure, bloating, early satiety, or urinary symptoms (frequency/urgency). Because many of these symptoms are nonspecific and occur with other health conditions, they are frequently overlooked by patient and health-care professional alike (Vaughan et al., 2011). Diagnostic tests: Pelvic examination is recommended in all sexually active women on the schedule determined by the American College of Obstetricians and Gynecologists. Rectovaginal examination may be necessary to detect ovarian enlargement. Ovarian enlargement cannot always be palpated, making pelvic examination a limited diagnostic test. (Kennedy-Malone 371) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 2 of 2 Comments: Question 14. Question : A 27-year-old male comes in to the clinic for symptoms of dysuria, urinary frequency, as well as urgency and perineal pain. Transrectal palpation of the prostate reveals a very tender, boggy, swollen prostate. The clinician should recognize these as signs of: Student Answer: Prostatitis Prostate cancer Urethritis Benign prostatic hyperplasia Instructor Explanation: Prostatitis is an acute or chronic infection of the prostate gland. Acute bacterial prostatitis is usually the result of infection by aerobic gram-negative rods (coliform bacteria or Pseudomonas). Enterococcus faecalis, an aerobic gram-positive bacteria, can also cause prostatitis. Routes of infection are ascent from the urethra, reflux of infected urine into the prostatic ducts, direct extension of bacteria, and migration via the lymphatic and vascular system. Acute symptoms commonly include fever, low back and perineal pain, possible penis pain, urinary urgency and frequency, nocturia, dysuria, and muscle and joint aches. Transrectal palpation of the prostate reveals a very tender, boggy, swollen prostate. Goolsby Points Received: 2 of 2 Comments: Question 15. Question : Which of the following males would be at greatest risk for testicular cancer? Student Answer: John, a 52-year-old, married African American Attorney who lives in Detroit, MI Jacob, a 22-year-old, homosexual male, who works as an accountant, resides in Cumming GA, and has a history of cryptorchidism Andy, a 27-year-old, Caucasian, single male who resides in Waukesha, WI and works as a maintenance mechanic Ryan, a 34-year-old healthy, married man from Sweden, who works as a Registered Nurse in Boston, MA Instructor Explanation: Malignant tumors of the testes are uncommon, usually present between the ages of 15 and 35, are slightly more common on the right side, and arise from germ cells. The greatest risk factor for the development of a testicular tumor is cryptorchidism, with an overall incidence of 7% to 10% in the patient with a history of unilateral or bilateral undescended testes. Increased screening and early detection have significantly decreased the mortality from this malignancy, but up to 10% of patients present with pain and/or constitutional or pulmonary complaints that indicate metastasis. (Goolsby 337) Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file. Points Received: 2 of 2 Comments: Question 16. Question : A 43-year-old male patient complains of right-sided abdominal and pain in the back in the right costovertebral angle region, fever, chills, dysuria, and nausea. On physical examination, there is 102 degree fever, tachycardia, and right costovertebral angle tenderness to percussion. The most likely condition is: Student Answer: Lower urinary tract infection Pyelonephritis Nephrolithiasis Hydonephrosis Points Received: 2 of 2 Comments: Question 17. Question : Which of the following disorders can cause urinary incontinence? Student Answer: Cystocele Overactive bladder Uterine prolapse All of the above Instructor Explanation: Cystocele and prolapse of the uterus can affect pelvic floor anatomy and cause urinary changes, including incontinence and changes to the quality of the urinary stream. Overactive bladder is a cause of incontinence due to atrophic changes of the pelvic floor muscles. Goolsby Points Received: 2 of 2 Comments: Question 18. Question : Your 18 year old sexually active patient presents with sudden right sided groin pain that is sharp and constant. Inspection of his genitals reveals a swollen and erythematous right scrotum. His right testicle is exquisitely tender, swollen and has no palpable masses. Elevation of the testis results in no reduction in pain. The left scrotum and the testicle are normal. Epididymis and other scrotal contents were within normal limits. The scrotum does not transilluminate. Cremasteric reflex is present on the left side but absent on the right. There is no penile discharge, inguinal lymphadenopathy, or hernias. Based on the history and physical exam your immediate concern is for: Student Answer: Torsion Infection Cancer Rupture Instructor Explanation: MedU Card #11 Points Received: 2 of 2 Comments: Question 19. Question : The Prehn sign is utilized to distinguish epididymitis from testicular torsion. Epididymitis is considered when the Prehn sign is positive. When is the Prehn sign determined to be positive? Student Answer: Pain is relieved by lifting of the testicle. Tenderness is limited to the upper pole of the testis. Lightly stroking or pinching the superior medial aspect of the thigh causes testicular retraction. A small bluish discoloration is visible through the skin in the upper pole. Instructor Explanation: MedU Card # 6. Prehn reported that physical lifting of the testicles relieves the pain caused by epididymitis but not pain caused by testicular torsion. A positive Prehn sign is pain that is relieved by lifting of the testicle; if present this can help distinguish epididymitis from testicular torsion. Points Received: 2 of 2 Comments: Question 20. Question : Which of the following exam findings makes the diagnosis of testicular tumor more likely? Student Answer: A scrotal mass that is accompanied by exquisite tenderness. Testicular swelling is mostly fluid and transilluminates easily A testicular mass that is non-tender to palpation Dilated and tortuous veins in the pampiniform plexus Instructor Explanation: MedU Card #9. Testicular tumor presents as scrotal mass that is rarely accompanied by tenderness. The swelling is solid so should not transilluminate. A testicular tumor is usually non-tender to palpation. Points Received: 2 of 2 Comments: 1. Question : When a patient presents with a skin-related complaint, it is important to first: Student Answer: Fully inspect all skin lesions before asking the patient how the lesion in question developed Obtain a full history about the development of the skin lesion prior to the physical examination Complete a full physical examination of the body prior to inspecting the skin lesion Examine the skin lesion without hearing a health history in order to not prejudice the diagnosis Instructor Explanation: When a patient presents with a skin-related complaint, there is an inclination to immediately examine the skin, as the lesion or change is often readily observable. However, it is crucial to obtain a history before proceeding to the examination in order to understand the background of the problem. A thorough symptom analysis is essential. Goolsby Points Received: 2 of 2 Comments: Question 2. Question : Which of the following dermatological conditions results from reactivation of the dormant varicella virus? Student Answer: Tinea versicolor Seborrheic keratosis Verruca Herpes zoster Instructor Explanation: Description: Herpes zoster is an acute vesicular eruption caused by a virus histologically identical to the varicella (chickenpox) virus. Herpes zoster is human (alpha) herpes virus 3 (varicella-zoster virus [VZV]), a member of the herpes virus group. Etiology: Recurrent VZV infection causes herpes zoster. The patient has initial contact with VZV in the form of chickenpox. The DNA virus resides within the neurons. During reactivation, the virus spreads across the sensory ganglion to other neurons, which causes a cutaneous eruption of a dermatome distribution (Fashner & Bell, 2011). Older adults have a decrease in cell-mediated immunity, which contributes to the risk of developing herpes zoster and postherpetic neuralgia (Barakzai & Fraser, 2008). (Kennedy-Malone 132-133) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 2 of 2 Comments: Question 3. Question : An older adult male presents with pain in his right chest wall for the past 48 hours. Upon examination, the nurse practitioner notices a vesicular eruption along the dermatome and identifies this as herpes zoster. The NP informs the gentleman that: Student Answer: All symptoms should disappear within three days Oral medications can dramatically reduce the duration and intensity of his symptoms He has chickenpox and can be contagious to his grandchildren He has a sexually transmitted disease Instructor Explanation: Treatment: Antiviral agents are recommended in the presence of significant pain, serious herpes zoster, or involvement near the eye. Postherpetic neuralgia is not reduced by antiviral therapy, but these agents may help with healing in the acute phase by reducing viral shredding (Cadogan, 2010). Give acyclovir, 800 mg 5 times a day for 7 to 10 days; famciclovir, 500 mg orally every 8 hours for 7 days; or valacyclovir, 1000 mg orally every 8 hours for 7 days (Fashner & Bell, 2011). These drugs must be given within 72 hours after onset of rash to be effective, and their use must be monitored in patients with reduced renal function (Tyring, Beutner, Tucker, Anderson, & Crooks, 2000). Patients should be encouraged to stay hydrated and to avoid scratching (Cadogan, 2010). Patients with disseminated disease and those who are immunocompromised may need IV antiviral medications (Cadogan, 2010). Topical agents are also effective in treating herpes zoster. The use of cool compresses with 1:20 Burow's solution, calamine lotion, and topical lidocaine (Xylocaine) is recommended for the soothing local effect. Analgesics may be necessary for the initial prodromal pain associated with herpes zoster. Acetaminophen is recommended initially. Tramadol, NSAIDs, and opiates can be used as recommended for severe pain. Gabapentin is recommended for the treatment of PHN. Initial dose is 300 mg on the first day and is titrated up gradually until pain relief is safely reached. The maximum does of gabapentin is 3600 mg/day. Pregabalin is also recommended for the treatment of postherpetic neuralgia and can be administered 50 mg 3 times a day or 75 mg twice a day. The dosage can be increased to 300 mg daily after 3 to 7 days as tolerated, followed by 150 mg every 3 to 7 days. The maximum recommended dose is 600 mg/day. Caution is advised when prescribing gabapentin and pregabalin to older adults given the side effects of dizziness and ataxia (Christo, Hobelmann, & Maine, 2007). The secondary amine tricyclic antidepressants, nortriptyline 10 mg orally or desipramine 10 to 25 mg orally both given at bedtime, may be helpful, and it may be necessary to gradually increase the dosage until reduction of pain occurs; however, because of the anticholinergic side effects, caution is warranted (Ahmad & Goucke,2002). The use of opioids in the treatment of PHN alone or in combination with other therapies has also been studied; greater pain relief was experienced by patients when a combined regimen was prescribed over a single agent (Gilron et al., 2005). The 5% lidocaine patch has been shown to be effective in treating the pain of PHN; 1 to 3 patches are applied in a 24-hour period. For PHN pain, capsaicin (Zostrix cream) can be applied topically. The capsaicin 8% patch can be applied by a health-care professional to the most painful skin areas (Christo et al., 2007). In cases of severe pain, a transcutaneous electrical nerve stimulator unit may be tried (Christo et al., 2007). (Kennedy-Malone 134) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 2 of 2 Comments: Question 4. Question : A 70-year-old white male comes to the clinic with a slightly raised, scaly, pink, and irregular lesion on his scalp. He is a farmer and works outside all day. You suspect actinic keratosis, but cannot rule out other lesions. What recommendation would you give him? Student Answer: Ignore the lesion, as it is associated with aging. Instruct him to use a nonprescription hydrocortisone cream to dry up the lesion. Perform a biopsy or refer to a dermatologist. Advise him to use a dandruff shampoo and return in one month if the lesion has not gone away. Instructor Explanation: Patients may be concerned about a new, pigmented lesion or a change in an already existing one. Patients may report associated itching, burning, or pain in a mole. Superficial spreading melanoma is a flat to slightly raised pigmented lesion with irregular borders, commonly found on the backs of men and the lower legs of women. Lentigo maligna melanoma, an irregularly pigmented macula with notched borders, occurs on sun-exposed areas, especially on the faces of older adults. Nodular melanoma, brown or black papules usually located on the trunk, head, and neck, is characterized by rapid growth. Acral lentiginous melanomas, a rare melanoma subtype, is found proportionally higher in people of color. Acral lentiginous melanoma occurs on the palms, soles, fingers, and toes; a pigmented streak of the cuticle is diagnostic (Hutchinson's sign) (Bradford, Goldstein, McMaster, & Tucker, 2009; Bristow, de Berker, Acland, Turner, & Bowling, 2010). Clinical evaluation for skin cancer also includes a total body skin examination and palpation of regional lymph nodes, liver, and spleen (Rubin, 2010a). Diagnostic tests: Skin cancer is diagnosed through biopsy. Biopsy of the suspected lesion is necessary to confirm the diagnosis via histological examination of the tissue; an adequate tissue sample should be excised, and an elliptical excision generally is necessary for larger lesions. Excisional biopsy is recommended for any pigmented lesion (Nolen et al., 2011). (Kennedy-Malone 145) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 2 of 2 Comments: Question 5. Question : The appearance of a 2-10 cm. herald patch with subsequent development of parallel oval lesions on the trunk in a christmas tree distribution involving the upper arms and upper legs are common in: Student Answer: Pityriasis Rosea Shingles Psoriasis Lymes Disease Instructor Explanation: The patient is usually asymptomatic, although some complain of a prodromal period of malaise preceding the emergence of the rash. The rash is often pruritic. The first sign is typically a “herald patch,” which is a 2- to 10-cm annular pink patch that, similar to tinea, has an area of central clearing with a fine scale. The herald patch is most commonly located on the trunk. The herald patch is followed several days later by a more diffuse set of smaller pink, salmon, or fawn-colored lesions, which, at 0.5 to 1.5 cm, are much smaller than the herald patch. The distribution of the smaller lesions is described as “Christmas tree distribution” because the lesions have a slightly diagonal axis and are distributed along the skin tension lines. (Goolsby 73) Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file. Points Received: 2 of 2 Comments: Question 6. Question : Mr. Fitzgerald is a 68-year-old previously healthy man with a history of significant sun exposure who presents with a progressively enlarging 18 x 16 mm erythematous pruritic oval patch on his left forearm that has been present for three to four years. Your differential would include all of the following EXCEPT: Student Answer: Fungal skin infection Eczema Seborrheic Keratosis Squamous cell carcinoma of the skin Instructor Explanation: MedU Card #7 Points Received: 2 of 2 Comments: Question 7. Question : What kind of lesions are caused by the herpes simplex virus? Student Answer: Scales Vesicles Plaques Urticaria Instructor Explanation: The skin lesions of herpes consist of multiple vesicles, which cluster and are usually preceded by an area of tender erythema. The vesicles erode, forming ulcerations. Goolsby Points Received: 2 of 2 Comments: Question 8. Question : Among the following conditions, which needs to be treated with systemic antifungal agents? Student Answer: Tinea pedis/tinea magnum Tinea corporis/tinea cruris Tinea capitis/Tinea unguium (onychomycosis) Tinea pedis /tinea faciale Instructor Explanation: MedU Card #9 Points Received: 2 of 2 Comments: Question 9. Question : Which lesions are typically located along the distribution of dermatome? Student Answer: Scabies Herpes zoster Tinea Dyshidrosis Instructor Explanation: Signal symptoms: Cutaneous eruption of a dermatome distribution, burning or tingling skin sensation. Description: Herpes zoster is an acute vesicular eruption caused by a virus histologically identical to the varicella (chickenpox) virus. Herpes zoster is human (alpha) herpes virus 3 (varicella-zoster virus [VZV]), a member of the herpes virus group. Etiology: Recurrent VZV infection causes herpes zoster. The patient has initial contact with VZV in the form of chickenpox. The DNA virus resides within the neurons. During reactivation, the virus spreads across the sensory ganglion to other neurons, which causes a cutaneous eruption of a dermatome distribution (Fashner & Bell, 2011). Older adults have a decrease in cell-mediated immunity, which contributes to the risk of developing herpes zoster and postherpetic neuralgia (Barakzai & Fraser, 2008). (Kennedy-Malone 132-133) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 2 of 2 Comments: Question 10. Question : A smooth round nodule with a pearly gray border and central induration best describes which skin lesion? Student Answer: Seborrheic keratosis Malignant melanoma Herpes zoster Basal cell carcinoma Instructor Explanation: There are three specific types of basal cell carcinoma: nodular, morpheaform, and superficial. Nodular BCC generally presents first as a dome-shaped, white-to-pink papule or nodule having a raised pearly border with prominent telangiectasia. BCC tumors can also have a brown to glossy black appearance (Gloster & Neal, 2006). Patients may describe this lesion as a pimple that did not heal. As the nodule enlarges, scaling, crusting, or central ulceration may become noticeable. It is important to note that the ulcerated areas can heal over with new scar tissue; however, the tumor grows deeper and the cycle of ulceration and healing begins again (Habif, 2004). Superficial BCC often appears on the trunk and extremities. Characteristic of the superficial BCC is the presence of a well-circumscribed translucent or bright pink to red patch of skin surrounded often by telangiectasia. This type of BCC resembles other chronic skin conditions such as psoriasis, eczema, discoid lupus erythematous, and Bowen's disease. The least common type of BCC is the sclerosing or morpheaform tumor. Found on the head and neck and occasionally the trunk of the body, the lesion appears to be a hypopigmented tumor that eventually is surrounded by irregular telangiectasia with atrophic scarlike appearance (Nolen et al., 2011). (Kennedy-Malone 144-145) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 2 of 2 Comments: Question 11. Question : Cellulitis is a deep skin infection involving the dermis and subcutaneous tissues. The nurse practitioner suspects cellulitis in a 70-year-old Asian diabetic male presenting with reddened edematous skin around his nares. Which statement below will the nurse practitioner use in her decision-making process for the differential diagnosis pertaining to reddened edematous skin? Student Answer: Cellulitis is two times more common in women Facial cellulitis is more common in people >55 There is low incidence of cellulitis in patients with diabetes Cellulitis is only a disease of the lower extremities of patients with known arterial insufficiency Instructor Explanation: Age: Cellulitis can occur at any age. Facial cellulitis is most common in people 50 years and older. (Kennedy-Malone 128) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 2 of 2 Comments: Question 12. Question : Folliculitis is most commonly due to: Student Answer: Contact dermatitis Varicella zoster Dermatophytes Staphylococcal infection Instructor Explanation: Folliculitis is an inflammation of the hair follicles and is typically associated with staphylococci. Other microorganisms and causes include pseudomonas (associated with hot tubs), Candida, tinea barbae, and herpes. Goolsby Points Received: 2 of 2 Comments: Question 13. Question : The anti-inflammatory properties of topical corticosteroids result in part from their ability to induce vasoconstriction to the small blood vessels in the upper dermis. Of the following, which is the most potent topical corticosteroid? Student Answer: Hydrocortisone 2.5% Triamcinolone acetonide 0.1% Betamethasone dipropionate 0.05% Alclometasone dipropionate 0.05% Instructor Explanation: MedU Card #8 Points Received: 2 of 2 Comments: Question 14. Question : Which of the following descriptions accurately documents cellulitis? Student Answer: Cool, erythematous, shiny hairless extremity with decreased pulse Scattered, erythematous ring-like lesions with clear centers Clearly demarcated, raised erythematous area of face Diffusely inflamed skin that is warm and tender to palpation Instructor Explanation: Signs and symptoms: Patients may complain of localized pain, fever, chills, rigors, malaise, anorexia, nausea, or headache, and, in severe cases, patients may have tachycardia, hypotension, and delirium (Nazarko, 2008b). Cellulitis most often appears on the lower extremities after a skin aberration, such as dermatitis, ulceration, trauma, or tinea pedis. Cellulitis can develop on the arms and the face as well. Scars from previous cardiovascular surgery are common sites for recurrent cellulitis (Price, 2009). Examine for skin temperature, note any breaks in the skin and ulcerations, and determine presence of pulses and sensation. Local erythema with edema and tenderness elicited by palpation are presenting signs of cellulitis. The skin can appear to look stretched, later taking on the appearance of an orange peel when the surface is infiltrated (Price, 2009). Depending on the organism of origin, large hemorrhagic bullae may be present. (Kennedy-Malone 128-129) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 2 of 2 Comments: Question 15. Question : Asymmetrical bi-color lesion with irregular border measuring 8 mm is found on the right lower arm of an adult patient. This assessment finding is consistent with: Student Answer: Melanoma Basal cell carcinoma Leukoplakia Senile lentigines Instructor Explanation: For patients with suspected melanoma, the mnemonic ABCDE guides the clinician in determining if the clinical characteristics of a suspicious lesion warrant close surveillance and/or biopsy for histological evaluation: • Asymmetry • Border irregularity • Color variation • Diameter >6 mm • Elevation of a previously flat lesion, evolving and enlarging (Halpern, Marghoob, & Sober, 2009; Rubin, 2010b). It is important to note, however, than only one-third of melanoma cases follow the classic ABCDE pattern of development, and many forms of melanoma mimic benign lesions (Rubin, 2009). (Kennedy-Malone 145) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 2 of 2 Comments: Question 16. Question : Which of the following descriptions best illustrates assessment findings consistent with tinea capitis? Student Answer: Circular erythematous patches with papular, scaly annular borders and clear discharge Inflamed scaly dry patches with broken hairs Web lesions with erythema and scaling borders Scaly pruritic erythematous lesions on inguinal creases Instructor Explanation: Signs and symptoms: Dry scaling is a hallmark of each of the superficial fungal infections. Tinea capitis presents as hair loss (alopecia). Grey patch tinea capitis often is circular in shape with the presence of many broken-off hairs and the scalp assumes a dull grey color due to the arthrospores that are formed by the fungi. Black dot tinea capitis occurs when hairs break off near the surface and give the appearance of dots. The dots may be scattered over the scalp and not form a classic round patch. A kerion is an inflammatory mass on the scalp that is painful and may include pustules and result in cervical or occipital adenopathy. (Kennedy-Malone 150) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 2 of 2 Comments: Question 17. Question : A patient has a tender, firm, nodular cystic lesion on his scalp that produces cheesy discharge with foul odor. This is most likely a: Student Answer: Bacterial folliculitis Basal cell carcinoma Bullous impetigo Epidermoid cyst Instructor Explanation: With an epidermoid cyst, the patient complains of a cystic lesion that produces cheesy discharge with foul odor. The lesion is sometimes tender or painful. The lesion is nodular, round and firm, and subcutaneous; thus, it is flesh colored. The most common sites include the face, scalp, neck, upper trunk, and extremities. Goolsby Points Received: 2 of 2 Comments: Question 18. Question : Patient presents with complaint of a “swollen node” under his arm. The area is tender and the node has progressed in size over the past few days. Which of the following should be included in your differential diagnosis? Student Answer: Hidradenitis suppurativa Epidermoid cyst Furuncle Both A and C Instructor Explanation: Hidradenitis suppurativa involves occlusions of hair follicles, which causes a red, fluctuant tender lesion. The site is commonly under the breast or in the axillae or groin. The clinician must differentiate this skin condition from an enlarged lymph node, which can appear similar. An enlarged lymph node is usually painless, whereas hidradenitis is usually tender. Furuncles are staphylococcal infections of hair follicles or sebaceous glands. Patients complain of pain, redness, and swelling at the affected site, commonly the axillae and groin. Goolsby Points Received: 2 of 2 Comments: Question 19. Question : A patient suffered a laceration of the shin three days ago, and today presents with a painful, warm, red swollen region around the area. The laceration has a purulent exudate. The clinician should recognize that the infected region is called: Student Answer: Contact dermatitis Folliculitis Hidradenitis suppurativa Cellulitis Instructor Explanation: In cellulitis, a patient often describes a history of a break in the skin from an injury, insect bite or sting, or previous procedure preceding the onset of redness, swelling, and pain at the site. The affected area is tender, swollen, reddened, and warm. Streptococcus or staphylococcal commonly causes the infection. The lower leg is a common site, usually unilateral. Goolsby Points Received: 2 of 2 Comments: Question 20. Question : A woman complains of malaise and arthralgias. You note a butterfly-shaped, macular, erythematous rash across her cheeks and nose. These conditions are common in: Student Answer: Psoriasis Lichen planus Systemic lupus erythematosus Erythema nodosum Instructor Explanation: In systemic lupus erythematosus, the patient will have a range of symptoms relevant to the diagnosis, depending on the affected organs. There is often coexisting arthralgia and malaise. The rash is macular and erythematous. It is described as a “butterfly rash” because the distribution resembles a butterfly’s wings overlying the forehead and cheeks. Goolsby 1. Question : Which of the following best describes the pain associated with osteoarthritis? Student Answer: Constant, burning, and throbbing with an acute onset Dull and primarily affected by exposure to cold and barometric pressure Begins upon arising and after prolonged weight bearing and/or use of the joint Begins in the morning and limits continued ambulation Instructor Explanation: Signs and symptoms: Complaints of morning stiffness lasting <30 minutes or stiffness that improves with activity and accompanying muscle spasms may indicate OA. Persistent pain and limitation of motion in the affected joint may be reported. (Kennedy-Malone 402) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 2 of 2 Comments: Question 2. Question : Your 63-year-old Caucasian woman with polymyalgia rheumatica (PMR) will begin treatment with corticosteroids until the condition has resolved. You look over her records and it has been 2 years since her last physical examination and any laboratory or diagnostic tests as she relocated and had not yet identified a health-care provider. In prioritizing your management plan, your first orders should include: Student Answer: Recommending she increase her dietary intake of Calcium and Vitamin D Ordering once a year bisphosphonate and a proton pump inhibitor Participate in a fall prevention program Dual-energy X-ray (DEXA) scan and updating immunizations Instructor Explanation: Follow-up: Assess the patient for proximal pain, morning stiffness, resolution of constitutional symptoms, and adverse reaction to corticosteroids (Dasgupta et al., 2010). For patients with PMR, the ESR and/or C-reactive protein need monitoring until the levels decrease and previously reported symptoms are alleviated. The CBC can be repeated to determine if the anemia has resolved. Initially, the patients will need to return every couple of weeks to evaluate the clinical response to therapy; this is followed by approximately an every-3-month surveillance to determine response to treatment and any adverse reactions to the long-term corticosteroids. Additional monitoring of urea and electrolytes and glucose should continue every 3 months while on corticosteroids (Dasgupta et al., 2010). Follow up on the results of the dual-energy x-ray absorptiometry scan. Consider prophylactic therapy to prevent osteoporosis with bisphosphonates with calcium and vitamin D supplementation. Patients also presenting with GCA need to be monitored in the same way, with repeated eye examinations as warranted, including examination for cataracts resulting from corticosteroid therapy (Paget & Spiera, 2006). Because patients with GCA are at risk for developing aortic aneurysm, follow-up abdominal examination for aortic aneurysm is needed. This complication is of great concern especially with patients who are at high risk for developing aortic aneurysms such as patients who smoke, are hypertensive, and have arteriosclerotic heart disease (Unwin et al., 2006). (Kennedy-Malone 407) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 2 of 2 Comments: Question 3. Question : In providing health teaching related to dietary restrictions, the nurse practitioner should advise a patient with gout to avoid which of the following dietary items: Student Answer: Green leafy vegetables Beer, sausage, fried seafood Sugar Gluten and bread items Instructor Explanation: Contributing factors: Factors associated with primary gout in men include positive family history, obesity, trauma, hypertension, hyperlipidemia, hypertriglyceridemia, diets high in purine (especially organ meats, anchovies, sardines, scallops, oatmeal), alcohol consumption (especially beer and moonshine whiskey), dietary intake of high-fructose corn syrup products, lead intoxication, dehydration, fasting (which causes ketosis), binge eating, analgesic nephropathy, nephrolithiasis, urolithiasis, and polycystic kidney disease (Choi & Curhan, 2008; Neogi, 2011) (Kennedy-Malone 394) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 2 of 2 Comments: Question 4. Question : A 33-year-old female reports general malaise, fatigue, stiffness, and pain in multiple joints of the body. There is no history of systemic disease and no history of trauma. On physical examination, the patient has no swelling or decreased range of motion in any of the joints. She indicates specific points on the neck and shoulders that are particularly affected. She complains of tenderness upon palpation of the neck, both shoulders, hips, and medial regions of the knees. The clinician should include the following disorder in the list of potential diagnoses: Student Answer: Osteoarthritis Rheumatoid arthritis Fibromyalgia Polymyalgia rheumatica Instructor Explanation: In fibromyalgia, the most common symptoms are generalized pain, stiffness, and decreased ROM, with multiple-point tenderness. The diagnostic criteria currently rest on a patient reporting point tenderness in at least 11 of 18 specified sites (Fig. 14.1) in addition to the presence of widespread pain for at least 3 months. The most common tender sites are in the neck, shoulders, spine, and hips. Other common symptoms include morning stiffness, anxiety, depression, sleep disturbances, “brain fog,” and irritable bowel syndrome. Goolsby Points Received: 2 of 2 Comments: Question 5. Question : A 46-year-old female complains of fatigue, general malaise, and pain and swelling in her hands that has gradually worsened over the last few weeks. She reports that pain, stiffness, and swelling of her hands are most severe in the morning. On physical examination, you note swelling of the metacarpophalangeal joints bilaterally. These are common signs of: Student Answer: Osteoarthritis Rheumatoid arthritis Scleroderma Sarcoidosis Instructor Explanation: RA typically affects the joints symmetrically. Symptoms may wax and wane, but the effects are cumulative and progressive. Although RA can affect any joint, it commonly affects the small joints of the hands and feet, and this is often helpful in diagnosis. There is often history of prolonged morning stiffness and fatigue. Affected joints are often tender, swollen with effusions, warm, and inflamed. The disease most commonly affects metacarpophalangeal and proximal interphalangeal joints. Goolsby Points Received: 2 of 2 Comments: Question 6. Question : Which of the following statements about osteoarthritis is true? Student Answer: It affects primarily weight-bearing joints It is a systemic inflammatory illness The metacarpal phalangeal joints are commonly involved Prolonged morning stiffness is common Instructor Explanation: Osteoarthritis (OA), still also referred to as degenerative joint disease, is a degenerative disease of the joint cartilage. It is the leading cause of disability in older adults in the United States (Lawrence et al., 2008). OA most commonly affects the hips, knees, and cervical and lumbar spine. Joint deformity with minimal pain is found in the DIP and PIP joints of the hand, the first carpometacarpal joint, and the first metatarsophalangeal joint (Shelton, 2013). OA is a complex active disease process involving the wearing away (degradation) and, to a lesser extent, the repair of the cartilage surface. It is now understood that there is both a mechanical (wearing away) and a biological (abnormal joint biology) part of the osteoarthritis (Ling & Rudolph, 2006). Besides the cartilage degeneration, patients often experience neurological and mechanical dysfunction (Chao & Kalunian, 2010). (Kennedy-Malone 402) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 2 of 2 Comments: Question 7. Question : The most appropriate first-line treatment for an acute gout flare is (assuming no kidney disease or elevated bleeding risk): Student Answer: Indomethacin 50 mg thrice daily for 2 days; then 25 mg thrice daily for 3 days Doxycycline 100 mg twice daily for 5 days Prednisolone 35 mg four times a day for 5 days Ice therapy Instructor Explanation: Treatment: NSAIDs, corticosteroids, and oral colchicine are acceptable first-line options for treatment of acute gout with treatment started within 24 hours of attack onset. Management of the older adult with gout requires careful monitoring. Older adults are susceptible to renal insufficiency, may have other concomitant diseases, and experience hypersensitivity to some of the medications used to treat younger patients with gout. NSAIDs should be used cautiously in the treatment of gout in older adults who have a history of heart failure, renal failure, and gastrointestinal conditions (Fravel & Ernst, 2011). As with any NSAID, renal function must be monitored. NSAIDs can endanger existing renal function, especially when the creatinine clearance is ≤30 mL/min. Additional concern with NSAID use in older adults is the potential for gastrointestinal bleeding due to NSAID-induced peptic ulcers. An exacerbation of hypertension can occur with excessive use of NSAIDs in older adults. Extensive use of NSAIDs can lead to fluid retention and antagonism of diuretic therapy, which may precipitate heart failure (Fravel & Ernst, 2011). Indomethacin is effective in the treatment of acute gout; the usual dose is 25 to 50 mg orally 2 to 3 times daily until the symptoms cease, then begin to taper the dose for 5 to 7 days. Liquid indomethacin is available for patient use. Although indomethacin has been traditionally favored in the treatment of gout, there has been no research documenting the advantage to its use over other NSAIDs such as naproxen (Zychowicz et. al, 2010). As with any NSAID, renal function must be monitored. NSAIDs can endanger existing renal function, especially when the creatinine clearance is ≤30 mL/min. Cyclooxygenase-2 inhibitors may be better tolerated in older adults with history of peptic ulcer. Colchicine can be given for acute gout attacks orally. It is most effective if given within 24 hours of an attack. The oral colchicine dose is 1.2 mg followed by a single 0.6 mg dose 1 hour later. Dose should not exceed 1.8 mg a day for an acute flare. Consensus guidelines indicate that colchicine is not to be used in patients with a creatinine clearance of <10 mL/min. (Hanlon et al., 2009). (Kennedy-Malone 395-396) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 2 of 2 Comments: Question 8. Question : A 34-year-old female presents with fever, general malaise, fatigue, arthralgias and rash for the last 2 weeks. On physical examination, you note facial erythema across the nose and cheeks. Serum diagnostic tests reveal positive antinuclear antibodies, anti-DNA antibodies, elevated C-reactive protein and erythrocyte sedimentation rate. The clinician should include the following disorder in the list of potential problems: Student Answer: Fibromyalgia Sarcoidosis Systemic lupus erythematosus Rheumatoid arthritis Instructor Explanation: SLE has many potential symptoms. The classic findings include a malar rash. Patients often have arthralgias, myalgias, fever, fatigue, Raynaud’s syndrome, and neuropathy. SLE effects depend on the organs involved and diagnosis can be difficult. A positive ANA occurs at some point in the condition in the majority of patients but is neither consistent nor specific for SLE. Positive anti-DNA and lupus erythematosus prep are also common to SLE. Goolsby Points Received: 2 of 2 Comments: Question 9. Question : Your 66-year-old male patient has recently started treatment for metabolic syndrome and is currently taking the following medications: an ACE inhibitor and beta blocker for treatment of hypertension. He is also taking a statin medication, simvastatin for hyperlipidemia, and a biguanide, metformin, for type 2 diabetes. The patient complains of myalgias of the legs bilaterally and blood work shows elevated serum creatine kinase. Which of the medications can cause such a side effect? Student Answer: Beta blocker ACE inhibitor Statin medication Metformin Instructor Explanation: Myalgias are a side effect of lipid-lowering medications called “statins.” If the myalgia is related to rhabdomyolysis, the urine is often reddish-brown. When drug- induced myalgia is present, there is often eosinophilia. For rhabdomyolysis myalgia, the serum creatine kinase is significantly elevated. Goolsby Points Received: 2 of 2 Comments: Question 10. Question : A 20-year-old male construction worker is experiencing new onset of knee pain. He complains of right knee pain when kneeling, squatting, or walking up and down stairs. On physical examination, there is swelling and crepitus of the right knee and obvious pain with resisted range of motion of the knee. He is unable to squat due to pain. Which of the following disorders should be considered in the differential diagnosis? Student Answer: Joint infection Chondromalacia patella Prepatellar bursitis All of the above Instructor Explanation: Prepatellar bursitis is also called housemaid’s knee, which is common to persons whose occupation requires extended periods of kneeling, such as plumbers and carpet layers. This bursitis can also be caused by an infection. The patient complains of pain in the area inferior to and over the patella, and there is swelling and inflammation of the bursa. Chondromalacia patella is seen in young active persons of either gender. The condition is also commonly called patella-femoral syndrome and runner’s knee. The pain involves the anterior knee, often develops gradually, and is moderate in intensity. Pain can be reproduced by pressing the patella against the femoral condyles, and there is tenderness around the patella. Other maneuvers that reproduce the pain include applying pressure against the patella as the patient extends the lower leg, flexing the quadriceps, and moving the patella from side to side. Crepitus and effusion are often present. Decision Rule in Chondromalacia Patella: Two or more of the following symptoms (pain reported on muscle contraction, squatting, or kneeling) is associated with 60% sensitivity and 85% specificity for patellofemoral pain syndrome. Of these, the one maneuver with greatest diagnostic strength is pain on resisted contraction (Cook et al., 2010). Goolsby Points Received: 2 of 2 Comments: Question 11. Question : A 17-year-old male complains of severe right knee pain. He was playing football when he heard a “pop” at the moment of being tackled and his knee “gave away” from under him. On physical examination, there is right knee swelling and decreased range of motion. There is a positive anterior drawer sign. These findings indicate: Student Answer: Knee ligament injury Osgood-Schlatter disease Prepatellar bursitis Chondromalacia patella Instructor Explanation: The anterior, medial, and lateral knee ligaments are vulnerable to injury in athletic activities. The mechanism through which the anterior cruciate ligament (ACL) is typically injured involves deceleration combined with sudden turning or pivoting. The medial collateral ligament (MCL) is most prone to injury through motions that place valgus stress on the knee. Compared with ACL and MCL injury, damage to the lateral collateral ligament (LCL) is much rarer but typically occurs when sudden varus stress is placed on the knee. The patient often relates history of an acute trauma followed by the onset of pain, swelling, and limited mobility. Often patients recall hearing or feeling a “pop” at the moment of injury and/or “give-away” sense. ACL injury is identified through a positive drawer (Fig. 14.9) and/or Lachman’s test (Fig. 14.10). Laxity of the LCL is assessed by placing varus stress on the knee with the leg both extended and flexed. Goolsby Points Received: 2 of 2 Comments: Question 12. Question : A 55-year-old patient complains of lower back pain due to heavy lifting at work yesterday. He reports weakness of the left leg and paresthesias in the left foot. On physical examination, the patient has diminished ability to dorsiflex the left ankle. Which of the following symptoms should prompt the clinician to make immediate referral to a neurosurgeon? Student Answer: Straight leg raising sign Lumbar herniated disc on X-ray Loss of left sided patellar reflex Urinary incontinence Instructor Explanation: With low back pain in a patient, it is important to obtain a detailed history of the onset and progression of the pain. A thorough pain history should be completed, noting its quality, location, radiation, and intensity as well as any exacerbating and relieving factors. A thorough review of systems is necessary to identify any associated symptoms that may indicate an urgent problem. These include altered bowel and/or bladder function, fever, weight loss, and/or weakness. The physical examination should begin by noting the patient’s posture and apparent level of comfort. The standing patient should be directed through a series of maneuvers to assess the back motion, including flexion, hyperextension, lateral flexion, and rotation, as the smoothness of motion, ROM, and any obvious signs of discomfort are noted. Observe the patient walking on heels and on toes, noting any signs of weakness. Next, with the patient resting supine on the examination table, the straight leg maneuver should be performed. As the patient rests supine with both legs extended, the examiner should passively elevate one leg at a time. A positive test is indicated if the patient experiences discomfort with the initial elevation rather than once the hip has been hyperflexed beyond 50 degrees. If the results indicate nerve impingement or disk injury, further radiographic testing is then indicated. Goolsby Points Received: 2 of 2 Comments: Question 13. Question : Your patient is a 43-year-old female golfer who complains of arm pain. On physical examination, there is point tenderness on the elbow and pain when the patient is asked to flex the wrist against the clinician’s resistance. These are typical signs of: Student Answer: Carpal tunnel syndrome Osteoarthritis of the wrist Epicondylitis Cervical osteoarthritis Instructor Explanation: Carpal tunnel syndrome causes a range of neurological symptoms, including pain, paresthesia, and weakness. Frequently, nighttime pain is an early symptom. There may be a swelling at the wrist related to inactivity or flexion at night. The pain and/or paresthesias typically involve the anterior aspects of wrist, medial palm, and first three digits on the affected hand. However, pain may radiate up the forearm to the shoulder with numbness and tingling along the median nerve. Over time, hand weakness often develops. Pain and paresthesia are often relieved by the patient “shaking” the affected hand in a downward fashion; this is called the flicking sign. A positive Tinel’s sign is elicited by tapping on the median nerve at the carpal tunnel, causing pain and tingling along the median nerve. Phalen’s maneuver reproduces the pain after 1 minute of wrist flexion against resistance. Goolsby Points Received: 2 of 2 Comments: Question 14. Question : Which of the following describes the pathology of De Quervain’s tenosynovitis? Student Answer: Irritation of a tendon located on the radial side of the wrist, near the thumb Impingement of the median nerve, causing pain in the palm and fingers Fluid-filled cyst that typically develops adjacent to a tendon sheath in the wrist Ulnar nerve compression at the olecranon process Instructor Explanation: De Quervain’s tenosynovitis involves irritation of a tendon located on the radial side of the wrist, near the thumb. With overuse, the tissues surrounding the tendon sheath hypertrophy, causing pressure on the tendon and making it difficult to move. The pain is usually limited to the radial aspect of the wrist and area immediately around the base of the thumb. Pain increases with use of the hand, such as with gripping maneuvers. Other symptoms include swelling, decreased sensation, and limited ROM with a locking sensation with thumb motion. The Finkelstein maneuver (Fig. 14.7) is used to diagnose De Quervain’s disease. A positive test results in pain, which is often severe. Patients who can repeatedly open and close the fist with smooth thumb motion are unlikely to have De Quervain’s. Goolsby Points Received: 2 of 2 Comments: Question 15. Question : What is the most common cause of hip pain in older adults? Student Answer: Osteoporosis Osteoarthritis Trauma due to fall Trochanteric bursitis Instructor Explanation: There are many potential causes of hip pain. Among adults, the most common cause is OA with degenerative changes. In younger patients, the cause is often strain of the muscles or tendons. In comparison to other joints, the hip is often difficult to assess, in part because much of the joint and its periarticular structures lie deeper than those of other joints. Goolsby Points Received: 2 of 2 Comments: Question 16. Question : A 43-year-old female was in a bicycling accident and complains of severe pain of the right foot. The patient limps into the emergency room. On physical examination, there is no point tenderness over the medial or lateral ankle malleolus. There is no foot tenderness except at the base of the fifth metatarsal bone. According to the Ottawa foot rules, should an X-ray of the feet be ordered? Student Answer: Yes, there is tenderness over the fifth metatarsal No, there is not tenderness over the navicular bone Yes, the patient cannot bear weight on the foot A and C Instructor Explanation: Foot Rule: Order film if one of the following is met: Inability to bear weight for four steps (both immediately and in emergency department) Bone tenderness at navicular or base of fifth metatarsal Sensitivity = 100% Specificity = 79% Goolsby. And FYI: The following Ottawa rules recommend x-ray of the ankle if either one of the following conditions exist: Inability to bear weight for four steps (both immediately and in emergency department) Bone tenderness at posterior edge or tip of either malleolus Points Received: 2 of 2 Comments: Question 17. Question : 38-year-old Asian male, Mr. Chen, with past medical history significant for prehypertension who has recently taken up softball presents with three to five weeks of shoulder pain when throwing overhead. Ice minimally alleviates pain. Medications: Naproxen minimally alleviates shoulder pain. Allergies: Penicillin-associated rash. Family history: Brother has rheumatoid arthritis. Which of the following musculoskeletal causes of shoulder pain would merit urgent diagnosis and management? Student Answer: Adhesive capsulitis Septic subacromial bursitis Impingement of the supraspinatus tendon Calcific tendinopathy Instructor Explanation: MedU Card #3 Delay in recognition and treatment of a septic subacromial bursitis may lead to local tissue destruction and loss of function, extension of infection locally to deeper spaces such as bone (osteomyelitis) or more distant sites by way of bacteremia and that may progress to sepsis. Points Received: 2 of 2 Comments: Question 18. Question : If Mr. Chen had restricted passive as well as active ROM of the shoulder, what problems involving the shoulder might you consider? Student Answer: Adhesive capsulitis Rotator cuff tear Tendinopathy of the long head of the biceps Rotator cuff impingment Instructor Explanation: MedU Card #7 A patient with loss of active and passive ROM is more likely to have joint disease; whereas a patient with loss of only active ROM is more likely to have an issue with muscle tissue. The following joint diseases will produce restricted active and passive ROM of the shoulder: • Adhesive capsulitis, a condition common in patients with metabolic diseases such as diabetes and hypothyroidism in which there is contracture of the joint capsule • Glenohumeral arthritis, a much less common site of osteoarthritis than the primary weight-bearing joints of the lower extremity • Points Received: 2 of 2 Comments: Question 19. Question : What is the essential dynamic stabilizer of the shoulder joint? Student Answer: Labrum Rotator muscle group Glenohumeral ligaments Teres major muscle Instructor Explanation: MedU Card #10 Points Received: 2 of 2 Comments: Question 20. Question : Given Mr. Chen’s repetitive overhead activities, some injury to his rotator cuff muscle group is most likely. Of the following exam findings, which one would not support the diagnosis of rotator cuff tendinopathy? Student Answer: Positive Apley’s Scratch test Weakness and pain with empty can testing Limited active ROM Inability to raise arm above his head Instructor Explanation: MedU Card #15 Limited ROM with significant pain is a hallmark of the physical exam in the patient with a partial or complete rotator cuff tear. In a complete tear, the patient will likely not be able to raise his arm above his head. 1. Question : When assessing a patient who complains of a tremor, the nurse practitioner must differentiate essential tremor from the tremor of Parkinson’s disease. Which of the following findings are consistent with essential tremor? Student Answer: The handwriting is not affected by the tremor The tremor occurs with purposeful movements The tremor occurs at rest The tremor gets worse with alcohol ingestion Instructor Explanation: Unilateral pill-rolling tremor at rest is usually the first symptom. The tremor is maximal at rest but absent during sleep and can be differentiated from essential tremor, which is absent at rest and worsens with voluntary movement. The bradykinesia of PD affects gross and fine motor movement, speech volume, swallowing, and blinking. There is generally no muscle weakness, and deep tendon reflexes are normal. Although Alzheimer's disease can manifest with rigidity, bradykinesia, and gait disorders, no resting tremor is seen with Alzheimer's. Nonspecific secondary manifestations include cognitive dysfunction, sleep disturbances, constipation, dysphagia, blurred or double vision, nocturia, frequency, urgency, autonomic dysfunction (e.g., erectile dysfunction), dizziness, and drooling. (Goolsby 463) Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file. Points Received: 2 of 2 Comments: Question 2. Question : An older adult client with a history of a seizure disorder comes into the clinic for a routine check-up. Although seizure free, the client continues on long-term phenytoin treatment. The nurse practitioner would assess for which of the following long-term effects? Student Answer: Lid lag and nystagmus Gingival hyperplasia and nystagmus Nystagmus and microcytic anemia Gingival hyperplasia and iron deficiency anemia Instructor Explanation: Swallowing certain medications such as aspirin, antibiotics, ferrous sulfate, certain chemotherapeutic agents, NSAIDs, quinidine, steroids, alendronate, alprenolol, vitamin C, phenytoin, calcium preparations, theophylline, and potassium chloride contributes to pill esophagitis due to chemical irritation of the esophageal mucosa. (Kennedy-Malone 323) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 2 of 2 Comments: Question 3. Question : An elderly patient is maintained on phenytoin therapy for a history of a seizure disorder. In addition to periodic serum drug concentrations, which of the following are needed for annual evaluation? Student Answer: Complete blood count, liver function tests, and renal function tests Complete blood count, liver function tests, and platelet count Renal function and calculated creatinine clearance Serum albumin, liver function tests, and renal function tests Instructor Explanation: Goolsby Points Received: 2 of 2 Comments: Question 4. Question : An elderly patient has had a CVA in the anterior cerebral circulatory system (frontal lobe). What symptoms are most likely expressed? Student Answer: Neglect of body and difficulty organizing space Wernicke’s aphasia (difficulty understanding speech) Disorders of behavior and cognition Bilateral motor and sensory problem Instructor Explanation: Focal neurological changes are related to the area of the brain invaded by tumor. Frontal and parietal lobe tumors may cause changes in memory, behavior, and cognitive function. Memory, hearing, vision, and emotions are affected most often by temporal lobe tumors. Symptoms of temporal lobe tumors may mimic symptoms of affective or psychotic thought disorders. Visual changes can occur with occipital lobe tumors, in addition to speech, motor, and sensory changes for left-sided occipital masses and an inability to grasp abstract concepts for right-sided occipital masses. Lesions in the cerebellum affect balance and coordination. Pituitary tumors may present with the symptoms of hypothyroidism, hypercortisolism, diabetes insipidus, or visual changes (Chandana et al., 2008; Wong & Wu, 2010). (Kennedy-Malone 421) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 2 of 2 Comments: Question 5. Question : The most common neurological cause of seizures in an older adult is: Student Answer: Alzheimer’s disease Multiple sclerosis Stroke Peripheral neuropathy Instructor Explanation: A common cause of epilepsy in the elderly is stroke, which accounts for up to 50% of cases in whom a cause can be identified. The risk of epilepsy increases up to 20-fold in the first year after a stroke. Individuals with a brain tumor, bacterial meningitis, or Alzheimer's disease are up to 10 times more likely to develop epilepsy than those without the diseases. (Kennedy-Malone 438) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 2 of 2 Comments: Question 6. Question : Mr. Andrews experienced a brief onset of right-sided weakness, slurred speech, and confusion yesterday. The symptoms have resolved. What should the nurse practitioner do? Student Answer: Assure the patient that he will not experience the symptoms again Identify modifiable cardiovascular risk factors Do a thorough medication review and a CT scan Order a stat EEG and administer O2 by mask Instructor Explanation: Stroke is one of the leading causes of death in the United States. Patients with stroke often have a history of hypertension, diabetes, cardiac disease, hyperlipidemia, smoking, drug or alcohol abuse, and family history of stroke. Strokes are divided into two main categories: thrombotic and hemorrhagic; however, the two can be difficult to differentiate using clinical signs and symptoms. (Goolsby 462) Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file. Points Received: 2 of 2 Comments: Question 7. Question : An older male patient is experiencing acute onset of right-sided weakness, slurred speech, and confusion. What should the nurse practitioner do promptly? Student Answer: Administer an aspirin by mouth Evaluate for stroke and arrange transport to the hospital right away Do a thorough medication review and stat blood sugar Order an EKG and administer O2 by cannula immediately Instructor Explanation: Stroke Stroke is one of the leading causes of death in the United States. Patients with stroke often have a history of hypertension, diabetes, cardiac disease, hyperlipidemia, smoking, drug or alcohol abuse, and family history of stroke. Strokes are divided into two main categories: thrombotic and hemorrhagic; however, the two can be difficult to differentiate using clinical signs and symptoms. Signs and Symptoms The onset is usually an abrupt altered level of consciousness accompanied by hemiparesis or hemiplegia. Patients may experience confusion, memory impairment, and aphasia. Signs and symptoms vary with the location and severity of the stroke. Mentation and cognitive changes may be temporary or permanent, depending on the extent of injury. Communication alterations stemming from fluent or receptive aphasia may be mistaken as dementia. Diagnostic Studies A CT scan, without contrast, is the preferred imaging study in early stroke because hemorrhage may be difficult to determine on an MRI in the first 48 hours. In studies of ischemic stroke patients, researchers have shown the reversibility of abnormalities on CT or MRI through the use of thrombolytic therapy within a 3-hour window. Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 2 of 2 Comments: Question 8. Question : When assessing an elderly client who reports a tremor, which assessment findings would be most reliable in identifying Parkinson’s disease? Student Answer: Any presence of tremor Symptoms of slowed movement, unstable angina, and tremor Resting tremor, slow unsteady gait, and cogwheel resistance Cogwheel rigidity, bradykinesia, and amnesia Instructor Explanation: Description: Parkinson's disease (PD) is a chronic progressive neurodegenerative disorder resulting in the loss of dopamine-producing cells in the substantia nigra, located in the basal ganglia. The loss of the inhibitory neurotransmitter dopamine results in an imbalance with the neurotransmitter acetylcholine, which is primarily responsible for worsening symptoms leading to immobility. Symptoms of PD include resting tremor, rigidity, akinesia, bradykinesia, and impaired postural reflexes (resulting in postural instability) (Vernon, 2009). Subtle motor impairments may precede the development of overt clinical signs and symptoms by many years. The Braak hypothesis (Burke, Dauer, & Vonsattel, 2008) indicates six pathological stages of PD, but clinical symptoms do not appear until stage 4 to 6. This stage correlates with 60% to 80% loss of substantia nigra neurons and striatal dopamine. It is the second most common neurodegenerative disease. It affects motor and autonomic function, mood, and cognition. (Kennedy-Malone 423-424) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 2 of 2 Comments: Question 9. Question : A middle-aged patient has been diagnosed with Parkinson’s disease. What influences the nurse practitioner’s decision to begin pharmacological treatment for this patient? Student Answer: Intentional tremors Gait instability requiring use of a cane Symptoms interfering with functional ability Medications initiated at first sign of unilateral involvement Instructor Explanation: Treatment: Drug therapy focuses on correcting the imbalance of dopamine and acetylcholine. • Patients with mild disease and no interference with ADLs may not require treatment. • With tremors and rigidity causing impairment of the patient's ability to perform ADLs and a disability level that is mild-to-moderate, treatment may include amantadine, which is thought to augment dopamine release from presynaptic nerve terminals or to inhibit dopamine reuptake. Initial dose is usually 100 mg with breakfast. In 5 to 7 days, add amantadine 100 mg with lunch, then increase daily dose to 300 mg. (Kennedy-Malone 425-426) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 2 of 2 Comments: Question 10. Question : A female patient presents to the clinic with complaints of a severe, throbbing, unilateral headache. She complains of seeing flashes of light prior to the headache. She complains of sound and light sensitivity as well as nausea. The clinician should recognize these as symptoms of: Student Answer: Epilepsy with aura Cluster headache Migraine headache Normal pressure hydrocephalus Instructor Explanation: Typical migraine pain begins unilaterally but may become generalized and may lateralize to the opposite side and/or radiate to the face or neck. The pain ranges from a dull ache to a throbbing or pulsatile pain. The pain is often severe and/or incapacitating and is often aggravated by movement, light, and noise. Accompanying symptoms may include nausea, vomiting, photophobia, phonophobia, osmophobia, dizziness, chills, and/or ataxia. There may be tenderness to palpation of the temporal arteries. Auras, if experienced, may include blurred vision and scotoma and/or other prodromal symptoms, such as anorexia, irritability, restlessness, or paresthesias lasting from 30 minutes to 3 hours before the onset of migraine pain. Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file. Points Received: 2 of 2 Comments: Question 11. Question : Which of the following is a common trigger of migraine headache? Student Answer: Missed meals Menses Alcohol All of the above Instructor Explanation: Common Migraine Triggers: • Stress • Caffeine • Altered sleep • Specific foods, missed meals • Menses • Alcohol • Hormone supplements Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file. Points Received: 2 of 2 Comments: Question 12. Question : A 65-year-old woman is accompanied by her daughter for a physical examination. She has mild heart failure and takes digitalis and an ACE inhibitor. As you examine the patient, you note flat affect, hand tremor, and slowed movements. The tremor is worsened at rest. There are no neurologic deficits. Hand grip, sensation of face and extremities, and lower extremity muscle strength are within normal limits and bilaterally equal. DTRs are equal bilaterally. CN II to XII are intact. The mental status exam is normal. These are key signs of: Student Answer: Chiari malformation Normal pressure hydrocephalus Parkinson’s disease Drug toxicity Instructor Explanation: Parkinson’s disease occurs with approximately equal sex distribution, and usually begins between 45 and 65 years of age. Unilateral pill-rolling tremor at rest is usually the first symptom. The tremor is maximal at rest but absent during sleep and can be differentiated from essential tremor, which is absent at rest and worsens with voluntary movement. There is a flattened affect and blank stare. There is bradykinesia of gross and fine motor movement, speech volume, swallowing, and blinking. There is generally no muscle weakness, and deep tendon reflexes are normal. Although Alzheimer’s disease can manifest with rigidity, bradykinesia, and gait disorders, no resting tremor is seen with Alzheimer’s. Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file. Points Received: 2 of 2 Comments: Question 13. Question : A 65-year-old male complains of a headache that feels “like a knife is cutting into his head.” He also reports feeling right-sided scalp and facial pain and “seeing double” at times. He has a history of hypertension and hyperlipidemia. His medications include beta blocker, statin drug, and an ACE inhibitor. On physical examination, you note palpable tenderness over the right side of the forehead. There are no neurological deficits. Vision is 20/20 with lenses. No weakness of extremities. CN II to XII are intact. The history corresponds to which of the following disorders? Student Answer: Drug toxicity Giant cell arteritis Cluster headache Migraine headache Instructor Explanation: Temporal arteritis is also referred to as giant cell arteritis or cranial arteritis. It is characterized by chronic inflammation and the presence of giant cells in large arteries, usually the temporal artery, but can occur in the cranial arteries, the aorta, and coronary and peripheral arteries. It affects the arteries containing elastic tissue, resulting in narrowing and eventual occlusion of the lumen. It occurs more among persons over 50 years of age and is slightly more common in females than in males. The cause is unknown, but there seems to be a genetic predisposition. If left untreated, arteritis can rapidly lead to blindness that is often irreversible. The most common chief complaint is head pain that is lancinating, sharp, or “ice pick” in nature. Patients often complain of visual changes, including amaurosis, diplopia, blurred vision, visual field cuts, eye pain, periorbital edema, and intermittent unilateral blindness. Other common presenting symptoms include scalp and/or jaw tenderness, facial pain, and tenderness to palpation over the affected artery. The pain is generally hemicranial but can be bilateral or diffuse. There may be eye pain, which is usually bilateral; periorbital edema may be present. Other potential associated symptoms include an intermittent fever (generally low grade), nausea, and/or weight loss. Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file. Points Received: 2 of 2 Comments: Question 14. Question : Which type of seizure is involved following a head injury or febile event? Student Answer: Epileptic Isolated Atonic Clonic-tonic Instructor Explanation: Subdural hematomas can be either acute or chronic. Acute subdural hematomas are usually associated with an acute head injury and can cause a range of symptoms, including headache and loss of consciousness. A chronic subdural hematoma in the elderly population may enlarge significantly before the patient begins to notice head pain. The headache associated with subdural hematoma is generally dull and aching in nature and may be transient. The history often includes a blow to the head, fall, or other injury, which preceded the pain. The physical findings vary depending on the severity of the trauma but may include progressive neurological deterioration, which may advance to include coma. The elderly patient with head trauma and anticoagulants should raise suspicion of subdural hematoma. Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file. Points Received: 2 of 2 Comments: Question 15. Question : M. L. is a 40-year-old female that has been recently diagnosed with Multiple Sclerosis (MS). As you provide primary care for your patient you inform her that: Student Answer: MS presents with a classis triad of symptoms, which are blurred vision, vertigo, and tinnitus MS has a predictable course and can easily be managed MS has a predictable course and can easily be managed Often MS has a varying pattern of exacerbation and remissions Instructor Explanation: Multiple sclerosis (MS) is a degenerative, demyelinating disease that is usually diagnosed in the second to fourth decades of life. It occurs more often in women than in men. The presentation of MS is often vague and transient, with episodic remission and exacerbation. Patients may have relapsing-remitting or primary/ secondary progressive MS. The etiology is unknown, but it is thought to be autoimmune. A genetic susceptibility is suspected since it is seen more in those of western European lineage who live in temperate zones. (Goolsby 481) Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file. Points Received: 2 of 2 Comments: Question 16. Question : Ms. Smith, 37-year-old, comes to the clinic today complaining of dull, throbbing bilateral headaches almost every evening. You suspect she is experiencing: Student Answer: cluster headaches migraine headaches tension headaches benign intracranial hypertension Instructor Explanation: Tension Headache Tension headaches are quite common. Whereas many people with episodic tension headaches do not seek treatment, those who suffer from frequent or chronic tension headaches may enlist the help of their provider. Other terms to describe tension headache include stress headache, essential headache, idiopathic headache, and muscle contraction headache. Tension headaches can occur with equal frequency among men and women, in any age group, and within any socioeconomic group. Signs and Symptoms Typical symptoms of tension headache include mild to moderate, nonthrobbing pressure or squeezing pain that can occur anywhere in the head or neck. The pain often starts slowly as a dull and aching discomfort that progresses to holocranial pain and pressure. The pain can recur intermittently, lasting from minutes to hours and usually remitting with rest or removal of the stressful trigger. There is usually no associated nausea and vomiting. Although patients may report photophobia and phonophobia, it is less severe than those associated with migraines. Tension headaches are not aggravated by movement or activity. The neck muscles are often tight to palpation. Tension headache triggers are listed in Table 15.2. (Goolsby 453) Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file. Points Received: 2 of 2 Comments: Question 17. Question : The FNP is seeing Mr. Smith a 78-year-old gentleman accompanied by his wife to the health clinic. His wife reports that he has been falling down, tripping and stumbling. The FNP suspects a problem in: Student Answer: Peripheral nervous system Brainstem Cerebrum Cerebellum Instructor Explanation: Focal neurological changes are related to the area of the brain invaded by tumor. Frontal and parietal lobe tumors may cause changes in memory, behavior, and cognitive function. Memory, hearing, vision, and emotions are affected most often by temporal lobe tumors. Symptoms of temporal lobe tumors may mimic symptoms of affective or psychotic thought disorders. Visual changes can occur with occipital lobe tumors, in addition to speech, motor, and sensory changes for left-sided occipital masses and an inability to grasp abstract concepts for right-sided occipital masses. Lesions in the cerebellum affect balance and coordination. Pituitary tumors may present with the symptoms of hypothyroidism, hypercortisolism, diabetes insipidus, or visual changes (Chandana et al., 2008; Wong & Wu, 2010). (Kennedy-Malone 421) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 2 of 2 Comments: Question 18. Question : Educating your patient about headache management should include information about all but: Student Answer: Headache diary Rebound headaches Trigger identification Common laboratory testing for diagnosis Instructor Explanation: For recurrent headaches, a headache diary is helpful in arriving at a definitive diagnosis. Although details can be simply recorded on a calendar, a number of headache diaries are available and downloadable via the Internet. Regardless of the format used, the diary should provide a space for the patient to identify daily whether a headache was experienced. When headache is experienced, the form should allow the patient to identify the type, severity, and duration of pain experienced; accompanying symptoms; treatment and response; and any suspected triggers. (Goolsby 450) Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file. A careful history of symptoms is invaluable. Complete physical examination should include skin survey for stigmata of neurocutaneous syndromes or melanoma, lymph node examination, abdominal examination for hepatomegaly or splenomegaly, and rectal examination with guaiac stool testing. Breast and pelvic examinations in women and cardiopulmonary examination are recommended. The neurological evaluation should include a mental status evaluation, testing for cognitive deficits or memory loss, and assessment for personality changes. Family members may be able to provide clues about subtle personality changes. Ophthalmic examination is essential to assess for papilledema, although this may not be present in patients 55 years old and older. Test also for asymmetry of strength, sensation, visual fields, reflex activity, cranial nerve function, and radicular signs. (Kennedy-Malone 422) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Points Received: 2 of 2 Comments: Question 19. Question : Mr. Marshall is a 72-year-old man, with a history of hypertension, COPD and moderate dementia, who presents with 4 days of increased confusion, nighttime restlessness, visual hallucinations, and urinary incontinence. His physical exam is unremarkable except for tachypnea, a mildly enlarged prostate, inattentiveness, and a worsening of his MMSE score from a baseline of 18 to 12 today. Mr. Marshall's presentation is most consistent with an acute delirium (acute change in cognition, perceptual derangement, waxing and waning consciousness, and inattention). What is the most likely diagnosis to frequently cause acute delirium in patients with dementia? Student Answer: Adverse drug effects Urinary tract infection Depression Acute cerebrovascular event Instructor Explanation: MedU Card #10 Points Received: 2 of 2 Comments: Question 20. Question : Mr. Marshall was administered the Mini-Mental State Exam (MMSE). Which of the following statements pertaining to this tool is a true statement? Student Answer: Mr. Marshall’s baseline score of 18 on the MMSE demonstrates severe impairment. The test takes 45 minutes to administer and will detect subtle memory losses, particularly in well-educated patients Because Mr. Marshall has symptoms of change of mental status you are not screening; you are doing the MMSE for diagnosis. In interpreting MMSE test scores, allowance does not have to be made for education and ethnicity Instructor Explanation: MedU Card #8 1. Question : Which of the following statements is true concerning anti-arrhythmic drugs? Student Answer: Amiodarone is the only one not associated with increased mortality and it has a very favorable side effect profile. Both long-acting and short-acting calcium channel blockers are associated with an increased risk of cardiovascular morbidity and mortality. Most anti-arrhythmics have a low toxic/therapeutic ratio and some are exceedingly toxic. Anti-arrhythmic therapy should be initiated in the hospital for all patients. Points Received: 2 of 2 Comments: Question 2. Question : What is the most common cause of hip pain in older adults? Student Answer: Osteoporosis Osteoarthritis Trauma due to fall Trochanteric bursitis Points Received: 2 of 2 Comments: Question 3. Question : Which patient is most likely to have osteoporosis? Student Answer: An 80-year-old underweight male who smokes and has been on steroids for psoriasis A 90-year-old female with no family history of osteoporosis who is on hormone replacement therapy A 68-year-old overweight female who drinks 1-2 drinks alcohol/day An 82-year-old female with a normal BMI takes calcium and performs weight-bearing exercise daily Points Received: 2 of 2 Comments: Question 4. Question : A 68-year-old male reports painless rectal bleeding occasionally noted with thin pencil-like stools, but no pain with defection. He has a history of colon polyp removal 10 years ago but was lost to follow-up. The nurse practitioner’s appropriate intervention is: Student Answer: Digital rectal exam and send home with 3 hemoccult to return Immediate referral to gastroenterologist and colonoscopy Order a screening sigmoidoscopy Order a colonoscopy and barium enema and refer based on results Points Received: 2 of 2 Comments: Question 5. Question : An older adult male presents with pain in his right chest wall for the past 48 hours. Upon examination, the nurse practitioner notices a vesicular eruption along the dermatome and identifies this as herpes zoster. The NP informs the gentleman that: Student Answer: All symptoms should disappear within three days Oral medications can dramatically reduce the duration and intensity of his symptoms He has chickenpox and can be contagious to his grandchildren He has a sexually transmitted disease Points Received: 2 of 2 Comments: Question 6. Question : According to the Genetic Information Nondiscrimination Act (GINA): Student Answer: Nurse Practitioners (NPs) should keep all genetic information of patients confidential NPs must obtain informed consent prior to genetic testing of all patients Employers cannot inquire about an employee’s genetic information All of the above Points Received: 2 of 2 Comments: Question 7. Question : Emphysematous changes in the lungs produce the following characteristic in COPD patients? Student Answer: Asymmetric chest expansion Increased lateral diameter Increased anterior-posterior diameter Pectus excavatum Points Received: 2 of 2 Comments: Question 8. Question : A 43-year-old female was in a bicycling accident and complains of severe pain of the right foot. The patient limps into the emergency room. On physical examination, there is no point tenderness over the medial or lateral ankle malleolus. There is no foot tenderness except at the base of the fifth metatarsal bone. According to the Ottawa foot rules, should an X-ray of the feet be ordered? Student Answer: Yes, there is tenderness over the fifth metatarsal No, there is not tenderness over the navicular bone Yes, the patient cannot bear weight on the foot A and C Points Received: 2 of 2 Comments: Question 9. Question : A key symptom of ischemic heart disease is chest pain. However, angina equivalents may include exertional dyspnea. Angina equivalents are important because: Student Answer: Women with ischemic heart disease many times do not present with chest pain Some patients may have no symptoms or atypical symptoms; diagnosis may only be made at the time of an actual myocardial infarction Elderly patients have the most severe symptoms A & B only Points Received: 2 of 2 Comments: Question 10. Question : Your 63-year-old Caucasian woman with polymyalgia rheumatica (PMR) will begin treatment with corticosteroids until the condition has resolved. You look over her records and it has been 2 years since her last physical examination and any laboratory or diagnostic tests as she relocated and had not yet identified a health-care provider. In prioritizing your management plan, your first orders should include: Student Answer: Recommending she increase her dietary intake of Calcium and Vitamin D Ordering once a year bisphosphonate and a proton pump inhibitor Participate in a fall prevention program Dual-energy X-ray (DEXA) scan and updating immunizations Points Received: 2 of 2 Comments: Question 11. Question : During physical examination of a patient, you note resonance on percussion in the upper lung fields. This is consistent with: Student Answer: COPD Pneumothorax A normal finding Pleural effusion Points Received: 2 of 2 Comments: Question 12. Question : The major impact of the physiological changes that occur with aging is: Student Answer: Reduced physiological reserve Reduced homeostatic mechanisms Impaired immunological response All of the above Points Received: 2 of 2 Comments: Question 13. Question : The Mini-Cog is a short screening tool used to assess cognition. Which of the following statements pertaining to the test is a true statement? Student Answer: The patient will be asked to repeat five words immediately following the directions by the practitioner. The patient is asked to draw the hour and minute hands on a picture of an analog clock. A score of 0-2 is a positive screen for dementia. The patient is asked to recall five images from picture cards following the drawing of the clock hands. Points Received: 2 of 2 Comments: Question 14. Question : Which of the following is considered a “red flag” when diagnosing a patient with pneumonia? Student Answer: Fever of 102 Infiltrates on chest X-ray Pleural effusion on chest X-ray Elevated white blood cell count Points Received: 2 of 2 Comments: Question 15. Question : The cytochrome p system involves enzymes that are generally: Student Answer: Inhibited by drugs Induced by drugs Inhibited or induced by drugs Associated with decreased liver perfusion Points Received: 2 of 2 Comments: Question 16. Question : In differentiating a gastric ulcer from a duodenal ulcer, you know that each type of ulcer can present with distinct signs and symptoms. Which of the following pieces of information from the patient’s history is the least useful for you to determine that the patient has a duodenal ulcer? Student Answer: Pain occurs on an empty stomach Diffuse epigastric pain Rarely associated with non-steroidal use Occurs in patients under 40 years of age Points Received: 2 of 2 Comments: Question 17. Question : During a routine physical examination of a 62-year-old female patient, the nurse practitioner identifies xanthelasma around both his eyes. What is the significance of this finding? Student Answer: High potential for future blindness and requires immediate referral None, normal variant of aging process Abnormal lipid metabolism requiring medical management Hereditary variant that is of no consequence but requires watchful waiting Points Received: 2 of 2 Comments: Question 18. Question : Which of the following is generally not a first-line treatment for post herpetic neuralgia? Student Answer: Intrathecal methylprednisolone Gabapentin 5% lidocaine patch Topical capsaicin Points Received: 2 of 2 Comments: Question 19. Question : A 66-year-old patient presents to the clinic complaining of dyspnea and wheezing. The patient reports a smoking history of 2 packs of cigarettes per day since age 16. This would be recorded in the chart as: Student Answer: 50 x 2-pack years 100-pack years 50-year, 2-pack history 100-pack history Points Received: 2 of 2 Comments: Question 20. Question : A common auscultatory finding in advanced CHF is: Student Answer: Systolic ejection murmur S3 gallop rhythm Friction rub Bradycardia Points Received: 2 of 2 Comments: Question 21. Question : The most common neurological cause of seizures in an older adult is: Student Answer: Alzheimer’s disease Multiple sclerosis Stroke Peripheral neuropathy Points Received: 2 of 2 Comments: Question 22. Question : A patient has a tender, firm, nodular cystic lesion on his scalp that produces cheesy discharge with foul odor. This is most likely a: Student Answer: Bacterial folliculitis Basal cell carcinoma Bullous impetigo Epidermoid cyst Points Received: 2 of 2 Comments: Question 23. Question : The most common cause of eye redness is: Student Answer: Conjunctivitis Acute glaucoma Head trauma Corneal abrasion Points Received: 2 of 2 Comments: Question 24. Question : Epistaxis can be a symptom of: Student Answer: Over-anticoagulation Hematologic malignancy Cocaine abuse All of the above Points Received: 2 of 2 Comments: Question 25. Question : A 33-year-old female reports general malaise, fatigue, stiffness, and pain in multiple joints of the body. There is no history of systemic disease and no history of trauma. On physical examination, the patient has no swelling or decreased range of motion in any of the joints. She indicates specific points on the neck and shoulders that are particularly affected. She complains of tenderness upon palpation of the neck, both shoulders, hips, and medial regions of the knees. The clinician should include the following disorder in the list of potential diagnoses: Student Answer: Osteoarthritis Rheumatoid arthritis Fibromyalgia Polymyalgia rheumatica Points Received: 2 of 2 Comments: Question 26. Question : Which symptom is more characteristic of Non-Cardiac chest pain? Student Answer: Pain often radiates to the neck, jaw, epigastrium, shoulder, or arm Pain tends to occur with movement, stretching or palpation Pain usually lasts less than 10 minutes and is relieved by nitroglycerine Pain is aggravated by exertion or stress Points Received: 2 of 2 Comments: Question 27. Question : Which type of seizure is involved following a head injury or febile event? Student Answer: Epileptic Isolated Atonic Clonic-tonic Points Received: 2 of 2 Comments: Question 28. Question : The best way to diagnose structural heart disease/dysfunction non-invasively is: Student Answer: Chest X-ray EKG Echocardiogram Heart catheterization Points Received: 2 of 2 Comments: Question 29. Question : A woman with an X-linked dominant disorder will: Student Answer: Not be affected by the disorder herself Transmit the disorder to 50% of her offspring (male or female) Not transmit the disorder to her daughters Transmit the disorder to only her daughters Points Received: 2 of 2 Comments: Question 30. Question : In assessing the eyes, which of the following is considered a “red flag” finding when associated with eye redness? Student Answer: History of prior red-eye episodes Grossly visible corneal defect Exophthalmos Photophobia Points Received: 2 of 2 Comments: Question 31. Question : Presbycusis is the hearing impairment that is associated with: Student Answer: Physiologic aging Ménière’s disease Cerumen impaction Herpes zoster Points Received: 2 of 2 Comments: Question 32. Question : In examination of the nose, the clinician observes gray, pale mucous membranes with clear, serous discharge. This is most likely indicative of: Student Answer: Bacterial sinusitis Allergic rhinitis Drug abuse Skull fracture Points Received: 2 of 2 Comments: Question 33. Question : When a patient presents with a skin-related complaint, it is important to first: Student Answer: Fully inspect all skin lesions before asking the patient how the lesion in question developed Obtain a full history about the development of the skin lesion prior to the physical examination Complete a full physical examination of the body prior to inspecting the skin lesion Examine the skin lesion without hearing a health history in order to not prejudice the diagnosis Points Received: 2 of 2 Comments: Question 34. Question : In providing health teaching related to dietary restrictions, the nurse practitioner should advise a patient with gout to avoid which of the following dietary items: Student Answer: Green leafy vegetables Beer, sausage, fried seafood Sugar Gluten and bread items Points Received: 2 of 2 Comments: Question 35. Question : A patient complains of fever, fatigue, and pharyngitis. On physical examination there is pronounced cervical lymphadenopathy. Which of the following diagnostic tests should be considered? Student Answer: Mono spot Strep test Throat culture All of the above Points Received: 2 of 2 Comments: Question 36. Question : In order to provide a comprehensive genetic history of a patient, the NP should: Student Answer: Ask patients to complete a family history worksheet Seek out pathology reports related to the patient’s disorder Interview family members regarding genetic disorders All of the above Points Received: 2 of 2 Comments: Question 37. Question : Which of the following imaging studies should be considered if a pulmonary malignancy is suspected? Student Answer: Computed tomography (CT) scan Chest X-ray with PA, lateral, and lordotic views Ultrasound Positron emission tomography (PET) scan Points Received: 2 of 2 Comments: Question 38. Question : A 75-year-old patient with community-acquired pneumonia presents with chills, productive cough, temperature of 102.1, pulse 100, respiration 18, BP 90/52, WBC 12,000, and blood urea nitrogen (BUN) 22 mg/dl. He has a history of mild dementia and his mental status is unchanged from his last visit. These findings indicate that the patient: Student Answer: Can be treated as an outpatient Requires hospitalization for treatment Requires a high dose of parenteral antibiotic Can be treated with oral antibiotics Instructor Explanation: Decision Rule: CURB-65 provides framework for determining whether the patient diagnosed with community-acquired pneumonia can be safely monitored and treated at home. One point is awarded for each of the following factors present: Confusion of new onset BUN is greater than 20mg/dl Respiratory rate of ≥ 30 breaths/minute Blood pressure is less than 90 mmHg systolic or diastolic ≤ 60 mm Hg Age 65 or older Patients scoring 3 to 5 typically require hospitalization for observation and therapy. Scores of 0 to 1 indicate likelihood that outpatient management is appropriate. A score of 2 is inconclusive. Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file (page 214-216) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. (page 241) Points Received: 2 of 2 Comments: Question 39. Question : Symptoms in the initial human immunodeficiency virus (HIV) infection include all of the following except: Student Answer: Sore throat Fever Weight loss Headache Points Received: 2 of 2 Comments: Question 40. Question : During auscultation of the chest, your exam reveals a loud grating sound at the lower anterolateral lung fields, at full inspiration and early expiration. This finding is consistent with: Student Answer: Pneumonia Pleuritis Pneumothorax A and B Points Received: 2 of 2 Comments: Question 41. Question : Helicobacter pylori is implicated as a causative agent in the development of duodenal or gastric ulcers. What teaching should the nurse practitioner plan for a patient who has a positive Helicobacter pylori test? Student Answer: It is highly contagious and a mask should be worn at home. Treatment regimen is multiple lifetime medications. Treatment regimen is multiple medications taken daily for a few weeks. Treatment regimen is complicated and is not indicated unless the patient is symptomatic. Points Received: 2 of 2 Comments: Question 42. Question : Your patient complains of lower abdominal pain, anorexia, extreme fatigue, unintentional weight loss of 10 pounds in last 3 weeks, and you find a positive hemoccult on digital rectal examination. Laboratory tests show iron deficiency anemia. The clinician needs to consider: Student Answer: Diverticulitis Colon cancer Appendicitis Peptic ulcer disease Points Received: 2 of 2 Comments: Question 43. Question : What is the most common valvular heart disease in the older adult? Student Answer: Aortic regurgitation Aortic stenosis Mitral regurgitation Mitral stenosis Points Received: 2 of 2 Comments: Question 44. Question : An 86-year-old patient who wears a hearing aid complains of poor hearing in the affected ear. In addition to possible hearing aid malfunction, this condition is often due to: Student Answer: Acoustic neuroma Cerumen impaction Otitis media Ménière’s disease Points Received: 2 of 2 Comments: Question 45. Question : Your patient is a 78-year-old female with a smoking history of 120-pack years. She complains of hoarseness that has developed over the last few months. It is important to exclude the possibility of: Student Answer: Thrush Laryngeal cancer Carotidynia Thyroiditis Points Received: 2 of 2 Comments: Question 46. Question : The aging process causes what normal physiological changes in the heart? Student Answer: The heart valve thickens and becomes rigid, secondary to fibrosis and sclerosis Cardiology occurs along with prolapse of the mitral valve and regurgitation Dilation of the right ventricle occurs with sclerosis of pulmonic and tricuspid valves Hypertrophy of the right ventricle Points Received: 2 of 2 Comments: Question 47. Question : Functional abilities are best assessed by: Student Answer: Self-report of function Observed assessment of function A comprehensive head-to-toe examination Family report of function Points Received: 2 of 2 Comments: Question 48. Question : An 18-year-old female patient presents with repeated urinary tract infections. She has no risk factors in her history, and her physical examination is unremarkable. She also has a normal pelvic exam. Which of the following should be obtained if anatomic abnormalities are suspected? Student Answer: Ultrasound of the kidneys Intravenous pyelogram Cystoscopy Transvaginal ultrasound of the bladder Points Received: 2 of 2 Comments: Question 49. Question : Which of the following disorders can cause urinary incontinence? Student Answer: Cystocele Overactive bladder Uterine prolapse All of the above Points Received: 2 of 2 Comments: Question 50. Question : A 57-year-old female complains of fatigue, muscle weakness, palpitations, nervousness, and insomnia for the last few weeks. She thought she was just experiencing stress from her husband’s recent stroke 1 month ago. There are no current medications. Past medical history includes cholecystecomy at age 45, D & C, age 50. On physical examination, the patient is afebrile, pulse 102, 18 breaths/min, BP 156/ 98. Physical examination reveals tremulousness and quadriceps weakness bilaterally +4/5. Which of the following diagnostic tests is a priority in the work-up? Student Answer: ACTH challenge test TSH Atrial fibrillation Fasting blood glucose Points Received: 2 of 2 Comments: Question 51. Question : A careful history of a female client with a chief complaint of intermittent diarrhea reveals that she also experiences bouts of constipation. She has no known allergies and experienced no unintentional weight loss. What is the most likely condition? Student Answer: Inflammatory bowel disease Irritable bowel syndrome Giardiasis Lactose intolerance Points Received: 2 of 2 Comments: Question 52. Question : When counseling clients regarding the use of antidiarrheal drugs such as Imodium anti-diarrheal and Kaopectate, the nurse practitioner advises patients to: Student Answer: Use all the medication Do not use for possible infectious diarrhea Use should exceed one week for effectiveness These drugs provide exactly the same pharmaceutical effects Points Received: 2 of 2 Comments: Question 53. Question : A 23-year-old patient who has had bronchiectasis since childhood is likely to have which of the following: Student Answer: Barrel-shaped chest Clubbing Pectus excavatum Prolonged capillary refill Points Received: 2 of 2 Comments: Question 54. Question : An older patient reports burning pain after ingestion of many foods and large meals. What assessment would assist the nurse practitioner in making a diagnosis of GERD? Student Answer: Identification of a fluid wave Positive Murphy’s sign Palpable spleen Midepigastric pain that is not reproducible with palpation Points Received: 2 of 2 Comments: Question 55. Question : Which ethnic group has the highest incidence of prostate cancer? Student Answer: Asians Hispanics African Americans American Indians Points Received: 2 of 2 Comments: Question 56. Question : The nurse practitioner orders bilateral wrist X-rays on a 69-year-old gentleman complaining of pain in both wrists for the past 6 weeks not related to any known trauma. The nurse practitioner suspects elderly onset rheumatoid arthritis. The initial radiographic finding in a patient with elderly onset rheumatoid arthritis would be: Student Answer: Symmetric joint space narrowing Soft tissue swelling Subluxations of the joints Joint erosions Points Received: 2 of 2 Comments: Question 57. Question : A 74-year-old obese female presents complaining of persistent right upper quadrant pain. She reports that she has not had any prior abdominal surgeries. Which of the following laboratory studies would be most indicative of acute cholecystitis? Student Answer: C-reactive protein level of 3 mg White blood cell count of 11,000 Direct serum bilirubin level of 0.3 mg/dl Serum amylase level of 145 U/L Points Received: 2 of 2 Comments: Question 58. Question : Which of the following is the most common cause of heartburn-type epigastric pain? Student Answer: Decreased lower esophageal sphincter tone Helicobacter pylori infection of stomach Esophageal spasm Peptic ulcer disease Points Received: 2 of 2 Comments: Question 59. Question : Your 70-year-old patient has gastroesophageal reflux disease (GERD). After a trial of lifestyle modifications and antacids, the patient continues to have occasional mild heartburn after occasional meals and at night. The most appropriate next action is: Student Answer: Prokinetic agents H2 antagonists Proton pump inhibitors Sucralfate Points Received: 2 of 2 Comments: Question 60. Question : The first step in the genomic assessment of a patient is obtaining information regarding: Student Answer: Family history Environmental exposures Lifestyle and behaviors Current medications Points Received: 2 of 2 Comments: Question 61. Question : Asymmetrical bi-color lesion with irregular border measuring 8 mm is found on the right lower arm of an adult patient. This assessment finding is consistent with: Student Answer: Melanoma Basal cell carcinoma Leukoplakia Senile lentigines Points Received: 2 of 2 Comments: Question 62. Question : Whenever a patient presents with acute non-traumatic shoulder pain, the clinician should make sure to exclude a: Student Answer: Cardiac origin of symptoms Gastrointestinal condition Cervical spine disorder All of the above Points Received: 2 of 2 Comments: Question 63. Question : Folliculitis is most commonly due to: Student Answer: Contact dermatitis Varicella zoster Dermatophytes Staphylococcal infection Points Received: 2 of 2 Comments: Question 64. Question : The three cardinal features of Parkinson’s disease are: Student Answer: Essential tremor, postural rigidity, and infarcts of the basal ganglion Bradykinesia, rigidity, and tremor Shuffling gait, constipation, positional freezing. Dementia, incontinence, and infarcts of the basal ganglion Points Received: 2 of 2 Comments: Question 65. Question : In AR disorders, carriers have: Student Answer: Two mutated genes; one from each parent that cause disease A mutation on a sex chromosome that causes a disease A single gene mutation that causes the disease One copy of a gene mutation but not the disease Points Received: 2 of 2 Comments: Question 66. Question : A 20-year-old male construction worker is experiencing new onset of knee pain. He complains of right knee pain when kneeling, squatting, or walking up and down stairs. On physical examination, there is swelling and crepitus of the right knee and obvious pain with resisted range of motion of the knee. He is unable to squat due to pain. Which of the following disorders should be considered in the differential diagnosis? Student Answer: Joint infection Chondromalacia patella Prepatellar bursitis All of the above Points Received: 0 of 2 Comments: Question 67. Question : When teaching a group of older adults regarding prevention of gastroesophageal reflux disease symptoms, the nurse practitioner will include which of the following instructions? Student Answer: Raise the head of the bed with pillows at night and chew peppermints when symptoms of heartburn begins. Raise the head of the bed on blocks and take the proton pump inhibitor medication at bedtime. Sit up for an hour after taking any medication and restrict fluid intake. Avoid food intolerances, raise head of bed on blocks, and take a proton pump inhibitor before a meal. Points Received: 2 of 2 Comments: Question 68. Question : You have a patient complaining of vertigo and want to know what could be the cause. Knowing there are many causes for vertigo, you question the length of time the sensation lasts. She tells you several hours to days and is accompanied by tinnitus and hearing loss. You suspect which of the following conditions? Student Answer: Ménière’s disease Benign paroxysmal positional vertigo Transient ischemic attack (TIA) Migraine Points Received: 2 of 2 Comments: Question 69. Question : Your patient has just returned from a 6-month missionary trip to Southeast Asia. He reports unremitting cough, hemoptysis, and an unintentional weight loss of 10 pounds over the last month. These symptoms should prompt the clinician to suspect: Student Answer: Legionnaires' disease Malaria Tuberculosis Pneumonia Points Received: 2 of 2 Comments: Question 70. Question : Which of the following is not a contributing factor to the development of esophagitis in older adults? Student Answer: Increased gastric emptying time Regular ingestion of NSAIDs Decreased salivation Fungal infections such as Candida Points Received: 2 of 2 Comments: Question 71. Question : Your 55-year-old male patient presents to your office with complaints of sudden development of severe right-sided, colicky lower abdominal pain. He cannot sit still on the examining table. The patient has previously been in good health. On physical examination, there are no signs of peritoneal inflammation. A urine sample reveals hematuria and crystalluria. Which is the next diagnostic test that should be done immediately? Student Answer: Ultrasound of the abdomen Abdominal X-ray Digital rectal examination Spiral CT scan Points Received: 2 of 2 Comments: Question 72. Question : The best evidence rating drugs to consider in a post myocardial infarction patient include: Student Answer: ASA, ACE/ARB, beta-blocker, aldosterone blockade ACE, ARB, Calcium channel blocker, ASA Long-acting nitrates, warfarin, ACE, and ARB ASA, clopidogrel, nitrates Points Received: 2 of 2 Comments: Question 73. Question : A 65-year-old woman is accompanied by her daughter for a physical examination. She has mild heart failure and takes digitalis and an ACE inhibitor. As you examine the patient, you note flat affect, hand tremor, and slowed movements. The tremor is worsened at rest. There are no neurologic deficits. Hand grip, sensation of face and extremities, and lower extremity muscle strength are within normal limits and bilaterally equal. DTRs are equal bilaterally. CN II to XII are intact. The mental status exam is normal. These are key signs of: Student Answer: Chiari malformation Normal pressure hydrocephalus Parkinson’s disease Drug toxicity Points Received: 2 of 2 Comments: Question 74. Question : A 26-year-old female who gave birth 1 month ago presents with sudden development of fever, neck pain, sore throat with dysphagia, and radiation of pain to the ear. Which of the following conditions is most important to consider? Student Answer: Diphtheria Epiglottitis Thyroiditis Otitis media Points Received: 2 of 2 Comments: Question 75. Question : A 17-year-old male complains of severe right knee pain. He was playing football when he heard a “pop” at the moment of being tackled and his knee “gave away” from under him. On physical examination, there is right knee swelling and decreased range of motion. There is a positive anterior drawer sign. These findings indicate: Student Answer: Knee ligament injury Osgood-Schlatter disease Prepatellar bursitis Chondromalacia patella Points Received: 2 of 2 Comments: Question 76. Question : An elderly patient has had a CVA in the anterior cerebral circulatory system (frontal lobe). What symptoms are most likely expressed? Student Answer: Neglect of body and difficulty organizing space Wernicke’s aphasia (difficulty understanding speech) Disorders of behavior and cognition Bilateral motor and sensory problem Points Received: 2 of 2 Comments: Question 77. Question : Which of the following medications are commonly associated with the side effect of cough? Student Answer: Beta blocker Diuretic ACE inhibitor Calcium antagonist Points Received: 2 of 2 Comments: Question 78. Question : Cellulitis is a deep skin infection involving the dermis and subcutaneous tissues. The nurse practitioner suspects cellulitis in a 70-year-old Asian diabetic male presenting with reddened edematous skin around his nares. Which statement below will the nurse practitioner use in her decision-making process for the differential diagnosis pertaining to reddened edematous skin? Student Answer: Cellulitis is two times more common in women Facial cellulitis is more common in people >55 There is low incidence of cellulitis in patients with diabetes Cellulitis is only a disease of the lower extremities of patients with known arterial insufficiency Points Received: 2 of 2 Comments: Question 79. Question : A 55-year-old patient complains of lower back pain due to heavy lifting at work yesterday. He reports weakness of the left leg and paresthesias in the left foot. On physical examination, the patient has diminished ability to dorsiflex the left ankle. Which of the following symptoms should prompt the clinician to make immediate referral to a neurosurgeon? Student Answer: Straight leg raising sign Lumbar herniated disc on X-ray Loss of left sided patellar reflex Urinary incontinence Points Received: 2 of 2 Comments: Question 80. Question : A patient presents with eye redness, scant discharge, and a gritty sensation. Your examination reveals the palpable preauricular nodes, which are most likely with: Student Answer: Bacterial conjunctivitis Allergic conjunctivitis Chemical conjunctivitis Viral conjunctivitis Points Received: 2 of 2 Comments: Question 81. Question : A 60-year-old obese male client has type 2 diabetes mellitus and a lipid panel of TC = 250, HDL = 32, LDL = 165. The nurse practitioner teaches the patient about his modifiable cardiac risk factors, which include: Student Answer: Advancing age, diabetes, hyperlipidemia, and male gender Diabetes, obesity, and hyperlipidemia Hyperlipidemia, smoking, and family history of heart disease Male with age > 45, diabetes mellitus, and hyperlipidemia Points Received: 2 of 2 Comments: Question 82. Question : A patient has been prescribed metformin (Glucophage). One week later he returns with lowered blood sugars but complains of some loose stools during the week. How should the nurse practitioner respond? Student Answer: Discontinue the medication immediately Reassure the patient that this is an anticipated side effect Double the dosage of medication and have patient return in 1 week Order a chem. 7 to check for lactic acidosis Points Received: 2 of 2 Comments: Question 83. Question : Men have faster and more efficient biotransformation of drugs and this is thought to be due to: Student Answer: Less obesity rates than women Prostate enlargement Testosterone Less estrogen than women Points Received: 2 of 2 Comments: Question 84. Question : Which of the following conditions is the most common cause of nausea, vomiting, and diarrhea? Student Answer: Viral gastroenteritis Staphylococcal food poisoning Acute hepatitis A E coli gastroenteritis Points Received: 2 of 2 Comments: Question 85. Question : Alteration in micturition is the hallmark symptom for abdominal pain of genitourinary origin. Symptoms in alteration in micturition would include: Student Answer: Fever Dysuria Nausea/vomiting Right lower quadrant pain Points Received: 2 of 2 Comments: Question 86. Question : Mr. Jones is a 68-year-old retired Air Force pilot that has been diagnosed with prostate cancer in the past week. He has never had a surgical procedure in his life and seeks clarification on the availability of treatments for prostate cancer. He asks the nurse practitioner to tell him the side effects of a radical prostatectomy. Which of the following is not a potential side effect of this procedure? Student Answer: Urinary incontinence Impotence Dribbling urine Selected low back pain Points Received: 2 of 2 Comments: Question 87. Question : Which of the following symptoms is common with acute otitis media? Student Answer: Bulging tympanic membrane Bright light reflex of tympanic membrane Increased tympanic membrane mobility All of the above Points Received: 2 of 2 Comments: Question 88. Question : Rheumatic heart disease is a complication that can arise from which type of infection? Student Answer: Epstein-Barr virus Diphtheria Group A beta hemolytic streptococcus Streptococcus pneumoniae Points Received: 2 of 2 Comments: Question 89. Question : Which of the following drugs would be useful for the nurse practitioner to prescribe for an older adult to prevent gastric ulcers when a nonsteroidal anti-inflammatory drug is used for chronic pain management? Student Answer: Misoprostol (Cytotec) Cimetidine (Tagamet) Metronidazole (Flagyl) Bismuth subsalicylate (Pepto bismol) Points Received: 2 of 2 Comments: Question 90. Question : The most common complication of an untreated urinary obstruction due to a ureteral calculus is: Student Answer: Ureteral rupture Hydronephrosis Kidney mass Renal artery stenosis Points Received: 2 of 2 Comments: Question 91. Question : Jenny is a 24 year old graduate student that presents to the clinic today with complaints of fever, midsternal chest pain and generalized fatigue for the past two days. She denies any cough or sputum production. She states that when she takes Ibuprofen and rest that the chest pain does seem to ease off. Upon examination the patient presents looking very ill. She is leaning forward and states that this is the most comfortable position for her. Temp is 102. BP= 100/70. Heart rate is 120/min and regular. Upon auscultation a friction rub is audible. Her lung sounds are clear. With these presenting symptoms your initial diagnosis would be: Student Answer: Mitral Valve Prolapse Referred Pain from Cholecystitis Pericarditis Pulmonary Embolus Points Received: 2 of 2 Comments: Question 92. Question : If it has been determined a patient has esophageal reflux, you should tell them: Student Answer: They probably have a hiatal hernia causing reflux They probably need surgery They should avoid all fruit juices Smoking, alcohol, and caffeine can aggravate their problem Points Received: 2 of 2 Comments: Question 93. Question : Your 2-year-old patient shows facial features, such as epicanthal folds, up-slanted palpebral fissures, single transverse palmar crease, and a low nasal bridge. These are referred to as: Student Answer: Variable expressivity related to inherited disease Dysmorphic features related to genetic disease De novo mutations of genetic disease Different penetrant signs of genetic disease Points Received: 2 of 2 Comments: Question 94. Question : Asymptomatic 1+ bacteriuria is found in a nursing home resident with an indwelling catheter. The nurse practitioner’s initial intervention includes: Student Answer: Assessing resident’s cognitive status and last change of the catheter/bag Prescribing prophylactic Bactrim 1 tablet at bedtime Ordering a urine culture and sensitivity and prescribing empiric treatment until results obtained Ordering an X-ray of the kidney, urine, and bladder Points Received: 2 of 2 Comments: Question 95. Question : The nurse practitioner is discussing lifestyle changes with a patient diagnosed with gastroesophageal reflux. What are the nonpharmacological management interventions that should be included? Student Answer: Weight reduction and rest 30 minutes after each meal in the supine position Elevation of head of the bed 4-6 inches on blocks and weight reduction Encouraged to wear restrictive clothing to add support for diaphragmatic breathing Using oral mints to relieve gastric distress Points Received: 2 of 2 Comments: Question 96. Question : An obese middle-aged client presents with a month of nonproductive irritating cough without fever. He also reports occasional morning hoarseness. What should the differential include? Student Answer: Atypical pneumonia Peptic ulcer disease Gastroesophageal reflux Mononucleosis (Epstein-Barr) Points Received: 2 of 2 Comments: Question 97. Question : What kind of lesions are caused by the herpes simplex virus? Student Answer: Scales Vesicles Plaques Urticaria Points Received: 2 of 2 Comments: Question 98. Question : Fifth Disease is a slapped cheek rash that is caused by: Student Answer: Coxsackievirus Varicella Parvovirus B19 None of the above Points Received: 2 of 2 Comments: Question 99. Question : Which of the following descriptions accurately documents cellulitis? Student Answer: Cool, erythematous, shiny hairless extremity with decreased pulse Scattered, erythematous ring-like lesions with clear centers Clearly demarcated, raised erythematous area of face Diffusely inflamed skin that is warm and tender to palpation Points Received: 2 of 2 Comments: Question 100. Question : A clinical clue for suspected renal artery stenosis would be: Student Answer: Decreased urine output Development of resistant hypertension in a previously well-controlled patient Retroperitoneal pain on the affected side Rising BUN level with normal creatinine level Points Received: 2 of 2 Comments: * Times are displayed in (GMT-07:00) Mountain Time (US & Canada) 1. Question : You are beginning the examination of the skin on a 25-year-old teacher. You have previously elicited that she came to the office for evaluation of fatigue, weight gain, and hair loss. You strongly suspect that she has hypothyroidism. What is the expected moisture and texture of the skin of a patient with hypothyroidism? Student Answer: Moist and smooth Moist and rough Dry and smooth Dry and rough Points Received: 1 of 1 Comments: Question 2. Question : You are assessing a patient with joint pain and are trying to decide whether it is inflammatory or noninflammatory in nature. Which one of the following symptoms is consistent with an inflammatory process? Student Answer: Tenderness Cool temperature Ecchymosis Nodules Points Received: 1 of 1 Comments: Question 3. Question : A 68-year-old retired farmer comes to your office for evaluation of a skin lesion. On the right temporal area of the forehead, you see a flattened papule the same color as his skin, covered by a dry scale that is round and feels hard. He has several more of these scattered on the forehead, arms, and legs. Based on this description, what is your most likely diagnosis? Student Answer: Actinic keratosis Seborrheic keratosis Basal cell carcinoma Squamous cell carcinoma Points Received: 0 of 1 Comments: Question 4. Question : A 28-year-old graduate student comes to your clinic for evaluation of pain “all over.” With further questioning, she is able to relate that the pain is worse in the neck, shoulders, hands, low back, and knees. She denies swelling in her joints. She states that the pain is worse in the morning. There is no limitation in her range of motion. On physical examination, she has several points on the muscles of the neck, shoulders, and back that are tender to palpation. Muscle strength and range of motion are normal. Which one of the following is likely the cause of her pain? Student Answer: Rheumatoid arthritis Osteoarthritis Fibromyalgia Polymyalgia rheumatica Points Received: 1 of 1 Comments: Question 5. Question : Heberden’s nodes are commonly found in which one of the following diseases? Student Answer: Rheumatoid arthritis Degenerative joint disease Psoriatic arthritis Septic arthritis Points Received: 1 of 1 Comments: Question 6. Question : A new patient is complaining of severe pruritus that is worse at night. Several family members also have the same symptoms. Upon examination, areas of excoriated papules are noted on some of the interdigital webs of both hands and on the axillae. This finding is most consistent with: Student Answer: Contact dermatitis Impetigo Larva migrans Scabies Points Received: 1 of 1 Comments: Question 7. Question : An obese 55-year-old woman went through menarche at age 16 and menopause 2 years ago. She is concerned because an aunt had severe osteoporosis. Which one of the following is a risk factor for osteoporosis? Student Answer: Obesity Late menopause Having an aunt with osteoporosis Delayed menarche Points Received: 0 of 1 Comments: Question 8. Question : Ms. Whiting is a 68-year-old female who comes in for her usual follow-up visit. You notice a few flat red and purple lesions, about 6 centimeters in diameter, on the ulnar aspect of her forearms but nowhere else. She doesn't mention them. They are tender when you examine them. What should you do? Student Answer: Conclude that these are lesions she has had for a long time. Wait for her to mention them before asking further questions. Ask how she acquired them. Conduct the visit as usual for the patient. Points Received: 1 of 1 Comments: Question 9. Question : A 58-year-old man comes to your office complaining of bilateral back pain that now awakens him at night. This has been steadily increasing for the past 2 months. Which one of the following is the most reassuring in this patient with back pain? Student Answer: Age over 50 Pain at night Pain lasting more than 1 month or not responding to therapy Pain that is bilateral Points Received: 1 of 1 Comments: Question 10. Question : The Phalen’s test is used to evaluate: Student Answer: Inflammation of the median nerve Rheumatoid arthritis Degenerative joint changes Chronic tenosynovitis 1. Question : Which of the following would lead you to suspect a hydrocele versus other causes of scrotal swelling? Student Answer: The presence of bowel sounds in the scrotum Being unable to palpate superior to the mass A positive transillumination test Normal thickness of the skin of the scrotum Comments: Question 2. Question : You are examining a newborn and note that the right testicle is not in the scrotum. What should you do next? Student Answer: Refer to urology Recheck in six months Tell the parent the testicle is absent but that this should not affect fertility Attempt to bring down the testis from the inguinal canal Comments: Question 3. Question : A 50-year-old truck driver comes to your clinic for a work physical. He has had no upper respiratory, cardiac, pulmonary, gastrointestinal, urinary, or musculoskeletal system complaints. His past medical history is significant for mild arthritis and prior knee surgery in college. He is married and just changed jobs, working for a different trucking company. He smokes one pack of cigarettes a day, drinks less than six beers a week, and denies using any illegal drugs. His mother has high blood pressure and arthritis and his father died of lung cancer in his sixties. On examination, his blood pressure is 130/80 and his pulse is 80. His cardiac, lung, and abdominal examinations are normal. He has no inguinal hernia, but on his digital rectal examination you palpate a soft, smooth, and nontender pedunculated mass on the posterior wall of the rectum. What anal, rectal, or prostate disorder best fits his presentation? Student Answer: Internal hemorrhoid Prostate cancer Anorectal cancer Rectal polyp Comments: Question 4. Question : A 15-year-old high school football player is brought to your office by his mother. He is complaining of severe testicular pain since exactly 8:00 this morning. He denies any sexual activity and states that he hurts so bad he can't even urinate. He is nauseated and is throwing up. He denies any recent illness or fever. His past medical history is unremarkable. He denies any tobacco, alcohol, or drug use. His parents are both in good health. On examination, you see a young teenager lying on the bed with an emesis basin. He is very uncomfortable and keeps shifting his position. His blood pressure is 150/100, his pulse is 110, and his respirations are 24. On visualization of the penis, he is circumcised and there are no lesions and no discharge from the meatus. His scrotal skin is tense and red. Palpation of the left testicle causes severe pain and the patient begins to cry. His prostate examination is unremarkable. His cremasteric reflex is absent on the left but is normal on the right. By catheter you get a urine sample and the analysis is unremarkable. You send the boy with his mother to the emergency room for further workup. Student Answer: Acute orchitis Acute epididymitis Torsion of the spermatic cord Prostatitis Comments: Question 5. Question : Which is true of prostate cancer? Student Answer: It is commonly lethal. It is one of the less common forms of cancer. Family history does not appear to be a risk factor. Ethnicity is a risk factor. Comments: Question 6. Question : Which of the following conditions involves a tight prepuce which, once retracted, cannot be returned? Student Answer: Phimosis Paraphimosis Balanitis Balanoposthitis Comments: Question 7. Question : A 12-year-old is brought to your clinic by his father. He was taught in his health class at school to do monthly testicular self-examinations. Yesterday, when he felt his left testicle, it was enlarged and tender. He isn't sure if he has had burning with urination and he says he has never had sexual intercourse. He has had a sore throat, cough, and runny nose for the last three days. His past medical history is significant for a tonsillectomy as a small child. His father has high blood pressure and his mother is healthy. On examination, you see a child in no acute distress. His temperature is 100.8 and his blood pressure and pulse are unremarkable. On visualization of his penis, he is uncircumcised and has no lesions or discharge. His scrotum is red and tense on the left and normal appearing on the right. Palpating his left testicle reveals a mildly sore swollen testicle. The right testicle is unremarkable. An examining finger is put through both inguinal rings, and there are no bulges with bearing down. His prostate examination is unremarkable. Urine analysis is also unremarkable. What abnormality of the testes does this child most likely have? Student Answer: Acute orchitis Acute epididymitis Torsion of the spermatic cord Prostatitis Comments: Question 8. Question : The most common cause of cancer deaths in males is: Student Answer: Lung cancer Prostate cancer Colon cancer Skin cancer Comments: Question 9. Question : Important techniques in performing the rectal examination include which of the following? Student Answer: Lubrication Waiting for the sphincter to relax Explaining what the patient should expect with each step before it occurs All of the above Comments: Question 10. Question : Jim is a 47-year-old man who is having difficulties with sexual function. He is recently separated from his wife of 20 years. He notes that he has early morning erections but otherwise cannot function. Which of the following is a likely cause for his problem? Student Answer: Decreased testosterone levels Psychological issues Abnormal hypogastric arterial circulation Impaired neural innervation Question : Which of the following is true of human papilloma virus (HPV) infection? Student Answer: Pap smear is a relatively ineffective screening method. It commonly resolves spontaneously in one to two years. It is the second most common STI in the United States. HPV infections cause a small but important number of cervical cancers. Points Received: 1 of 1 Comments: Question 2. Question : Which of the following is the most effective pattern of palpation for breast cancer? Student Answer: Beginning at the nipple, make an ever-enlarging spiral. Divide the breast into quadrants and inspect each systematically. Examine in lines resembling the back and forth pattern of mowing a lawn. Beginning at the nipple, palpate vertically in a stripe pattern. Points Received: 0 of 1 Comments: Question 3. Question : A 14-year-old junior high school student is brought in by his mother and father because he seems to be developing breasts. The mother is upset because she read on the Internet that smoking marijuana leads to breast enlargement in males. The young man adamantly denies using any tobacco, alcohol, or drugs. He has recently noticed changes in his penis, testicles, and pubic hair pattern. Otherwise, his past medical history is unremarkable. His parents are both in good health. He has two older brothers who never had this problem. On examination, you see a mildly overweight teenager with enlarged breast tissue that is slightly tender on both sides. Otherwise, his examination is normal. He is agreeable to taking a drug test. What is the most likely cause of his gynecomastia? Student Answer: Breast cancer Imbalance of hormones of puberty Drug use Points Received: 1 of 1 Comments: Question 4. Question : Which of the following represents metrorrhagia? Student Answer: Fewer than 21 days between menses Excessive flow Infrequent bleeding Bleeding between periods Points Received: 1 of 1 Comments: Question 5. Question : What does a KOH (potassium hydroxide) prep help the nurse practitioner diagnose? Student Answer: Herpes zoster infections Yeast infections Herpes simplex infections Viral infections Points Received: 1 of 1 Comments: Question 6. Question : Abby is a newly married woman who is unable to have intercourse because of vaginismus. Which of the following is true? Student Answer: This is most likely due to lack of lubrication. This is most likely due to atrophic vaginitis. This is most likely due to pressure on an ovary. Psychosocial reasons may cause this condition. Points Received: 1 of 1 Comments: Question 7. Question : A 30-year-old man notices a firm, 2-cm mass under his areola. He has no other symptoms and no diagnosis of breast cancer in his first-degree relatives. What is the most likely diagnosis? Student Answer: Breast tissue Fibrocystic disease Breast cancer Lymph node Points Received: 0 of 1 Comments: Question 8. Question : Which of the following is true regarding breast self-examination? Student Answer: It has been shown to reduce mortality from breast cancer. It is recommended unanimously by organizations making screening recommendations. A high proportion of breast masses are detected by breast self-examination. The undue fear caused by finding a mass justifies omitting instruction in breast self-examination. Points Received: 0 of 1 Comments: Question 9. Question : A 23-year-old computer programmer comes to your office for an annual examination. She has recently become sexually active and wants to be placed on birth control. Her only complaint is that the skin in her armpits has become darker. She states it looks like dirt, and she scrubs her skin nightly with soap and water but the color stays. Her past medical symptoms consist of acne and mild obesity. Her periods have been irregular for 3 years. Her mother has type 2 diabetes, and her father has high blood pressure. The patient denies using tobacco but has four to five drinks on Friday and Saturday nights. She denies any illegal drug use. On examination, you see a mildly obese female who is breathing comfortably. Her vital signs are unremarkable. Looking under her axilla, you see dark, velvet-like skin. Her annual examination is otherwise unremarkable. What disorder of the breast or axilla is she most likely to have? Student Answer: Peau d'orange Acanthosis nigricans Hidradenitis suppurativa Points Received: 1 of 1 Comments: Question 10. Question : Which of the following is true of women who have had a unilateral mastectomy? Student Answer: They no longer require breast examination. They should be examined carefully along the surgical scar for masses. Lymphedema of the ipsilateral arm usually suggests recurrence of breast cancer. Women with breast reconstruction over their mastectomy site no longer require examination. Question : A 76-year-old retired farmer comes to your office complaining of abdominal pain, constipation, and a low-grade fever for about three days. He denies any nausea, vomiting, or diarrhea. The only unusual thing he remembers eating is two bags of popcorn at the movies with his grandson, three days before his symptoms began. He denies any other recent illnesses. His past medical history is significant for coronary artery disease and high blood pressure. He has been married for over fifty years. He denies any tobacco, alcohol, or drug use. His mother died of colon cancer and his father had a stroke. On examination, he appears his stated age and is in no acute distress. His temperature is 100.9 degrees and his other vital signs are unremarkable. His head, cardiac, and pulmonary examinations are normal. He has normal bowel sounds and is tender over the left lower quadrant. He has no rebound or guarding. His rectal examination is unremarkable and his fecal occult blood test is negative. His prostate is slightly enlarged but his testicular, penile, and inguinal examinations are all normal. Blood work is pending. What diagnosis for abdominal pain best describes his symptoms and signs? Student Answer: Acute diverticulitis Acute cholecystitis Acute appendicitis Mesenteric ischemia Points Received: 1 of 1 Comments: Question 2. Question : Jim is a 60-year-old man who presents with vomiting. He denies seeing any blood with emesis, which has been occurring for two days. He does note a dark, granular substance resembling the coffee left in the filter after brewing. What do you suspect? Student Answer: Bleeding from a diverticulum Bleeding from a peptic ulcer Bleeding from a colon cancer Bleeding from cholecystitis Points Received: 1 of 1 Comments: Question 3. Question : A 26-year-old sports store manager comes to your clinic, complaining of severe right-sided abdominal pain for twelve hours. He began having a stomachache yesterday, with a decreased appetite, but today the pain seems to be just on the lower right side. He has had some nausea and vomiting but no constipation or diarrhea. His last bowel movement was the night before and was normal. He has had no fever or chills. He denies any recent illnesses or injuries. His past medical history is unremarkable. He is engaged. He denies any tobacco or drug use and drinks four to six beers per week. His mother has breast cancer and his father has coronary artery disease. On examination, he appears ill and is lying on his right side. His temperature is 100.4 degrees and his heart rate is 110. His bowel sounds are decreased and he has rebound and involuntary guarding, one-third of the way between the anterior superior iliac spine and the umbilicus in the right lower quadrant (RLQ). His rectal, inguinal, prostate, penile, and testicular examinations are normal. What is the most likely cause of his pain? Student Answer: Acute appendicitis Acute mechanical intestinal obstruction Acute cholecystitis Mesenteric ischemia Points Received: 1 of 1 Comments: Question 4. Question : Josh is a 14-year-old boy who presents with a sore throat. On examination, you notice dullness in the last intercostal space in the anterior axillary line on his left side with a deep breath. What does this indicate? Student Answer: His spleen is definitely enlarged and further workup is warranted. His spleen is possibly enlarged and close attention should be paid to further examination. His spleen is possibly enlarged and further workup is warranted. His spleen is definitely normal. Points Received: 0 of 1 Comments: Question 5. Question : Diminished radial pulses may be seen in patients with which of the following? Student Answer: Aortic insufficiency Hyperthyroidism Arterial emboli Early “warm” septic shock Points Received: 0 of 1 Comments: Question 6. Question : A 42-year-old florist comes to your office, complaining of chronic constipation for the last six months. She has had no nausea, vomiting, or diarrhea, and no abdominal pain or cramping. She denies any recent illnesses or injuries. She denies any changes to her diet or exercise program. She is on no new medications. During the review of systems (ROS), you note that she has felt fatigued, had some weight gain, has irregular periods, and has cold intolerance. Her past medical history is significant for one vaginal delivery and two cesarean sections. She is married, has three children, and owns a flower shop. She denies tobacco, alcohol, or drug use. Her mother has type 2 diabetes and her father has coronary artery disease. There is no family history of cancers. On examination, she appears her stated age. Her vital signs are normal. Her head, eyes, ears, nose, throat, and neck examinations are normal. Her cardiac, lung, and abdominal examinations are also unremarkable. Her rectal occult blood test is negative. Her deep tendon reflexes are delayed in response to a blow with the hammer, especially the Achilles tendons. What is the best choice for the cause of her constipation? Student Answer: Large bowel obstruction Irritable bowel syndrome Rectal cancer Hypothyroidism Points Received: 1 of 1 Comments: Question 7. Question : A 57-year-old maintenance worker comes to your office for evaluation of pain in his legs. He has smoked two packs per day since the age of sixteen, but is otherwise healthy. You are concerned that he may have peripheral vascular disease. Which of the following is part of common or concerning symptoms for the peripheral vascular system? Student Answer: Intermittent claudication Chest pressure with exertion Shortness of breath Knee pain Points Received: 1 of 1 Comments: Question 8. Question : You are assessing a 59-year-old gas station owner for atherosclerosis in the lower extremities. In which of the following locations would the patient's pain make you concerned for this disease process? Student Answer: Thigh Knee Calf Ankle Points Received: 1 of 1 Comments: Question 9. Question : A 55-year-old secretary with a recent history of breast cancer, for which she underwent surgery and radiation therapy, and a history of hypertension comes to your office for a routine checkup. Which of the following aspects of the physical are important to note when assessing the patient for peripheral vascular disease in the arms? Student Answer: Femoral pulse, popliteal pulse Dorsalis pedis pulse, posterior tibial pulse Carotid pulse Radial pulse, brachial pulse Points Received: 1 of 1 Comments: Question 10. Question : Cody is a teenager with a history of leukemia and an enlarged spleen. Today he presents with fairly significant left upper quadrant (LUQ) pain. On examination of this area, a rough grating noise is heard. What is this sound? Student Answer: It is a splenic rub. It is a variant of bowel noise. It represents borborygmi. It is a vascular noise. Question : A 30-year-old woman with a history of mitral valve problems states that she has been “very tired.” She has started waking up at night and feels like her “heart is pounding.” During the assessment, the nurse practitioner palpates a thrill and lift at the fifth left intercostal space midclavicular line. In the same area the nurse practitioner also auscultates a blowing, swishing sound right after S1. These findings would be most consistent with: Student Answer: heart failure. aortic stenosis. pulmonary edema. mitral regurgitation. Instructor Explanation: Mitral regurgitation subjective findings include fatigue, palpitation, and orthopnea. Objective findings are (1) a thrill in systole at apex, (2) lift at apex, (3) apical impulse displaced down and to the left, (4) S1 diminished, S2 accentuated, S3 at apex often present, and (5) murmur: pansystolic, often loud, blowing, best heard at apex, radiating well to the left axilla. Points Received: 4 of 4 Comments: Question 2. Question : A patient presents with excruciating headache pain on one side of his head, especially around his eye, forehead, and cheek that lasts about 1/2 to 2 hours, occurring once or twice each day. The nurse practitioner suspects: Student Answer: hypertension. cluster headaches. tension headaches. migraine headaches. Instructor Explanation: Cluster headaches produce pain around the eye, temple, forehead, and cheek and are unilateral and always on the same side of the head. They are excruciating and occur once or twice per day and last 1/2 to 2 hours each. Points Received: 4 of 4 Comments: Question 3. Question : A patient complains that while studying for an examination he began to notice a severe headache in the frontotemporal area of his head that is throbbing and is somewhat relieved when he lies down. He tells the nurse practitioner that his mother also had these headaches. The nurse practitioner suspects that he may be suffering from: Student Answer: hypertension. cluster headaches. tension headaches. migraine headaches. Instructor Explanation: Migraine headaches tend to be supraorbital, retro-orbital, or frontotemporal with a throbbing quality. They are of a severe quality and are relieved by lying down. Migraines are associated with family history of migraine. Points Received: 4 of 4 Comments: Question 4. Question : A patient tells the nurse practitioner that he is very nervous, that he is nauseated, and that he “feels hot.” This type of data would be: Student Answer: objective. reflective. subjective. introspective Instructor Explanation: Subjective data are what the person says about himself or herself during history taking. Points Received: 4 of 4 Comments: Question 5. Question : The most important reason to share information and offer brief teaching while performing the physical examination is to help: Student Answer: the examiner feel more comfortable and gain control of the situation. build rapport and increase the patient’s confidence in the examiner. the patient understand his or her disease process and treatment modalities. the patient identify questions about his or her disease and potential areas of patient education. Instructor Explanation: Sharing of information builds rapport and increases the patient’s confidence in you as an examiner. It also gives the patient a little more control in a situation in which it’s easy to feel completely helpless. Points Received: 4 of 4 Comments: Question 6. Question : A patient says that she has recently noticed a lump in the front of her neck below her “Adam’s apple” that seems to be getting bigger. During the assessment, the finding that reassures the nurse practitioner that this may not be a cancerous thyroid nodule is that the lump (nodule): Student Answer: is tender. is mobile and not hard. disappears when the patient smiles. is hard and fixed to the surrounding structures. Instructor Explanation: Suspect any painless, rapidly growing nodule, especially the appearance of a single nodule in a young person. Cancerous nodules tend to be hard and are fixed to surrounding structures. Points Received: 4 of 4 Comments: Question 7. Question : A patient visits the clinic because he has recently noticed that the left side of his mouth is paralyzed. He states that he cannot raise his eyebrow or whistle. The nurse practitioner suspects that he has: Student Answer: Cushing’s syndrome. Parkinson’s syndrome. Bell’s palsy. had a cerebrovascular accident (stroke). Instructor Explanation: With an upper motor neuron lesion (as with CVA) the patient will have paralysis of lower facial muscles, but the upper half of the face is not affected owing to the intact nerve from the unaffected hemisphere. The person is still able to wrinkle the forehead and close the eyes. Points Received: 4 of 4 Comments: Question 8. Question : The temporomandibular joint is just below the temporal artery and anterior to the: Student Answer: hyoid. vagus. tragus. mandible. Instructor Explanation: The temporomandibular joint is just below the temporal artery and anterior to the tragus. Points Received: 4 of 4 Comments: Question 9. Question : During an examination of a patient’s abdomen, the nurse practitioner notes that the abdomen is rounded and firm to the touch. During percussion, the nurse practitioner notes a drum-like quality of the sound across the quadrants. This type of sound indicates: Student Answer: constipation. air-filled areas. the presence of a tumor. the presence of dense organs. Instructor Explanation: A musical or drum-like sound (tympany) is the sound heard when percussion occurs over air-filled viscus, such as the stomach or intestines. Points Received: 4 of 4 Comments: Question 10. Question : A patient tells the nurse that he is allergic to penicillin. What would be the nurse practitioner’s best response to this information? Student Answer: “Are you allergic to any other drugs?” “How often have you received penicillin?” “I’ll write your allergy on your chart so you won’t receive any.” “Please describe what happens to you when you take penicillin.” Instructor Explanation: Note both the allergen (medication, food, or contact agent, such as fabric or environmental agent) and the reaction (rash, itching, runny nose, watery eyes, difficulty breathing). With a drug, this symptom should not be a side effect but a true allergic reaction. Points Received: 4 of 4 Comments: Question 11. Question : A patient’s thyroid is enlarged, and the nurse practitioner is preparing to auscultate the thyroid for the presence of a bruit. A bruit is a: Student Answer: low gurgling sound best heard with the diaphragm of the stethoscope. loud, whooshing, blowing sound best heard with the bell of the stethoscope. soft, whooshing, pulsatile sound best heard with the bell of the stethoscope. high-pitched tinkling sound best heard with the diaphragm of the stethoscope. Instructor Explanation: If the thyroid gland is enlarged, auscultate it for the presence of a bruit, which is a soft, pulsatile, whooshing, blowing sound heard best with the bell of the stethoscope. Points Received: 4 of 4 Comments: Question 12. Question : After completing an initial assessment on a patient, the nurse practitioner has documented that his respirations are eupneic and his pulse is 58. This type of data would be: Student Answer: objective. reflective. subjective. introspective. Instructor Explanation: Objective data are what the health professional observes by inspecting, percussing, palpating, and auscultating during the physical exam. Points Received: 4 of 4 Comments: Question 13. Question : A patient tells the nurse that she has had abdominal pain for the past week. What would be the best response by the nurse? Student Answer: “Can you point to where it hurts?” “We’ll talk more about that later in the interview.” “What have you had to eat in the last 24 hours?” “Have you ever had any surgeries on your abdomen?” Instructor Explanation: A final summary of any symptom the person has should include, along with seven other critical characteristics, “Location: specific.” Ask the person to point to the location. Points Received: 4 of 4 Comments: Question 14. Question : A teenage patient comes to the emergency department with complaints of an inability to “breathe and a sharp pain in my left chest.” The assessment findings include the following: cyanosis, tachypnea, tracheal deviation to the right, decreased tactile fremitus on the left, hyperresonance on the left, and decreased breath sounds on the left. This description is consistent with: Student Answer: bronchitis. a pneumothorax. acute pneumonia. an asthmatic attack. Instructor Explanation: With a pneumothorax, free air in the pleural space causes partial or complete lung collapse. If the pneumothorax is large, tachypnea and cyanosis are seen. Unequal chest expansion, decreased or absent tactile fremitus, tracheal deviation to the unaffected side, decreased chest expansion, hyperresonant percussion tones, and decreased or absent breath sounds are assessed. Points Received: 4 of 4 Comments: Question 15. Question : The inspection phase of the physical assessment: Student Answer: yields little information. takes time and reveals a surprising amount of information. may be somewhat uncomfortable for the expert practitioner. requires a quick glance at the patient’s body systems before proceeding on with palpation. Instructor Explanation: A focused inspection takes time and yields a surprising amount of data. Initially, the examiner may feel uncomfortable “staring” at the person without also “doing something.” Points Received: 4 of 4 Comments: Question 16. Question : The mother of a 2-year-old is concerned because her son has had three ear infections in the past year. What would be an appropriate response by the nurse practitioner? Student Answer: “It is unusual for a small child to have frequent ear infections unless there is something else wrong.” “We need to check the immune system of your son to see why he is having so many ear infections.” “Ear infections are not uncommon in infants and toddlers because they tend to have more cerumen in the external ear.” “Your son’s eustachian tube is shorter and wider than yours because of his age, which allows for infections to develop more easily.” Instructor Explanation: The infant’s eustachian tube is relatively shorter and wider, and its position is more horizontal than the adult’s, so it is easier for pathogens from the nasopharynx to migrate through to the middle ear. Points Received: 4 of 4 Comments: Question 17. Question : The nurse practitioner would use bimanual palpation technique in which situation? Student Answer: Palpating the thorax of an infant Palpating the kidneys and uterus Assessing pulsations and vibrations Assessing the presence of tenderness and pain Instructor Explanation: Bimanual palpation requires the use of both hands to envelop or capture certain body parts or organs such as the kidneys, uterus, or adnexa. Points Received: 4 of 4 Comments: Question 18. Question : The patient’s record, laboratory studies, objective data, and subjective data combine to form the: Student Answer: database. admitting data. financial statement. discharge summary. Instructor Explanation: Together with the patient’s record and laboratory studies, the objective and subjective data form the database. Points Received: 4 of 4 Comments: Question 19. Question : When preparing to perform a physical examination on an infant, the examiner should: Student Answer: have the parent remove all clothing except the diaper on a boy. instruct the parent to feed the infant immediately before the exam. encourage the infant to suck on a pacifier during the abdominal exam. ask the parent to briefly leave the room when assessing the infant’s vital signs. Instructor Explanation: The parent should always be present for the child’s feeling of security and to understand normal growth and development. Timing of the examination should be 1 to 2 hours after feeding when the baby is not too drowsy nor too hungry. Infants do not object to being nude; clothing should be removed and a diaper left on a boy. Points Received: 4 of 4 Comments: Question 20. Question : The nurse practitioner notices that an infant has a large, soft lump on the side of his head and that his mother is very concerned. She tells the nurse practitioner that she noticed the lump about 8 hours after her baby’s birth, and that it seems to be getting bigger. One possible explanation for this is: Student Answer: hydrocephalus. craniosynostosis. cephalhematoma. caput succedaneum. Instructor Explanation: A cephalhematoma is a subperiosteal hemorrhage that is the result of birth trauma. It is soft, fluctuant, and well defined over one cranial bone. It appears several hours after birth and gradually increases in size. Points Received: 4 of 4 Comments: Question 21. Question : When examining an infant, the nurse practitioner should examine which area first? Student Answer: Ear Nose Throat Abdomen Instructor Explanation: Perform the least distressing steps first. Save the invasive steps of examination of the eye, ear, nose, and throat until last. Points Received: 4 of 4 Comments: Question 22. Question : When preparing to examine a 6-year-old child, which action is most appropriate? Student Answer: Start with the thorax, abdomen, and genitalia before examining the head. Avoid talking about the equipment being used because it may increase the child’s anxiety. Keep in mind that a child this age will have a sense of modesty. Have the child undress from the waist up. Instructor Explanation: A 6-year-old child has a sense of modesty. The child should undress himself or herself, leaving underpants on, and use a gown or drape. A school-age child is curious to know how equipment works, and the sequence should progress from head to toes. Points Received: 4 of 4 Comments: Question 23. Question : The nurse practitioner is assessing a patient’s skin during an office visit. What is the best technique to use to best assess the patient’s skin temperature? Student Answer: Use the fingertips because they’re more sensitive to small changes in temperature. Use the dorsal surface of the hand because the skin is thinner than on the palms. Use the ulnar portion of the hand because there is increased blood supply that enhances temperature sensitivity. Use the palmar surface of the hand because it is most sensitive to temperature variations because of increased nerve supply in this area. Instructor Explanation: The dorsa (backs) of hands and fingers are best for determining temperature because the skin there is thinner than on the palms. Points Received: 4 of 4 Comments: Question 24. Question : Percussion notes heard during the abdominal assessment may include: Student Answer: flatness, resonance, and dullness. resonance, dullness, and tympany. tympany, hyperresonance, and dullness. resonance, hyperresonance, and flatness. Instructor Explanation: Percussion notes normally heard during the abdominal assessment may include tympany, which should predominate because air in the intestines rises to the surface when the person is supine; hyperresonance, which may be present with gaseous distention; and dullness, which may be palpated over a distended bladder or enlarged spleen or liver. Points Received: 4 of 4 Comments: Question 25. Question : The nurse practitioner is assessing a patient for possible peptic ulcer disease and knows that which condition often causes this problem? Student Answer: Hypertension Streptococcus infections History of constipation and frequent laxative use Frequent use of nonsteroidal anti-inflammatory drugs Instructor Explanation: Peptic ulcer disease occurs with frequent use of nonsteroidal anti-inflammatory drugs, alcohol use, smoking, and Helicobacter pylori infection. Question : You are participating in a health fair and performing cholesterol screens. One person has a cholesterol level of 225. She is concerned about her risk for developing heart disease. Which of the following factors is used to estimate the 10-year risk of developing coronary heart disease? Student Answer: Ethnicity Alcohol intake Gender Asthma Comments: Question 2. Question : You are concerned that a patient has an aortic regurgitation murmur. Which is the best position to accentuate the murmur? Student Answer: Upright Upright, but leaning forward Supine Left lateral decubitus Comments: Question 3. Question : You are screening people at the mall as part of a health fair. The first person who comes for screening has a blood pressure of 132/85. How would you categorize this? Student Answer: Normal Prehypertension Stage 1 hypertension Stage 2 hypertension Comments: Question 4. Question : How should you determine whether a murmur is systolic or diastolic? Student Answer: Palpate the carotid pulse. Palpate the radial pulse. Judge the relative length of systole and diastole by auscultation. Correlate the murmur with a bedside heart monitor. Comments: Question 5. Question : A 78-year-old retired seamstress comes to the office for a routine check-up. You obtain an electrocardiogram (ECG) because of her history of hypertension. You diagnose a previous myocardial infarction and ask her if she had any symptoms related to this. Which of the following symptoms would be more common in this patient’s age group for an AMI? Student Answer: Chest pain Syncope Pain radiating into the left arm Pain radiating into the jaw Comments: Question 6. Question : On examination, you find a bounding carotid pulse on a 62-year-old patient. Which murmur should you suspect? Student Answer: Mitral valve prolapse Pulmonic stenosis Tricuspid insufficiency Aortic insufficiency Comments: Question 7. Question : Which of the following correlates with a sustained, high-amplitude point of maximal impulse (PMI)? Student Answer: Hyperthyroidism Anemia Fever Hypertension Comments: Question 8. Question : A 68-year-old woman with hypertension and diabetes is seen by the nurse practitioner for a dry cough that worsens at night when she lies in bed. She has shortness of breath, which worsens when she exerts herself. The patient’s pulse rate is 90/min and regular. The patient has gained 6 lbs over the past two months. She is on a nitroglycerine patch and furosemide daily. The explanation for her symptoms is: Student Answer: Kidney failure Congestive heart failure Angiotensin-converting enzyme (ACE) inhibitor induced coughing Thyroid disease Comments: Question 9. Question : When listening to a soft murmur or bruit, which of the following may be necessary? Student Answer: Asking the patient to hold their breath. Asking the patient in the next bed to turn down the TV. Checking your stethoscope for air leaks. All of the above. Comments: Question 10. Question : You notice a patient has a strong pulse and then a weak pulse. This pattern continues. Which of the following is likely? Student Answer: Emphysema Asthma exacerbation Severe left heart failure Cardiac tamponade uestion : A patient complains of shortness of breath for the past few days. On examination, you note late inspiratory crackles in the lower third of the chest that were not present a week ago. What is the most likely explanation for these? Student Answer: Asthma COPD Bronchiectasis Heart failure Comments: Question 2. Question : A sixty-year-old baker presents to your clinic, complaining of increasing shortness of breath and nonproductive cough over the last month. She feels like she can’t do as much activity as she used to do without becoming tired. She even has to sleep upright in her recliner at night to be able to breathe comfortably. She denies any chest pain, nausea, or sweating. Her past medical history is significant for high blood pressure and coronary artery disease. She had a hysterectomy in her 40s for heavy vaginal bleeding. She is married and is retiring from the local bakery soon. She denies any tobacco, alcohol, or drug use. Her mother died of a stroke, and her father died from prostate cancer. She denies any recent upper respiratory illness, and she has had no other symptoms. On examination, she is in no acute distress. Her blood pressure is 160/100, and her pulse is 100. She is afebrile, and her respiratory rate is 16. With auscultation, she has distant air sounds and she has late inspiratory crackles in both lower lobes. On cardiac examination, the S1 and S2 are distant and an S3 is heard over the apex. Student Answer: Pneumonia COPD Pleural pain Left-sided heart failure Comments: Question 3. Question : A patient with long-standing COPD was told by another practitioner that his liver was enlarged and this needed to be assessed. Which of the following would be reasonable to do next? Student Answer: Percuss the lower border of the liver. Measure the span of the liver. Order a hepatitis panel. Obtain an ultrasound of the liver. Comments: Question 4. Question : Which of the following is not considered an adventitious sound heard in the lung fields? Student Answer: Rhonchi Wheezes Rales Atelectatic crackles Comments: Question 5. Question : A fifty-five-year-old smoker complains of chest pain and gestures with a closed fist over her sternum to describe it. Which of the following diagnoses should be considered because of her gesture? Student Answer: Bronchitis Costochondritis Pericarditis Angina pectoris Comments: Question 6. Question : When crackles, wheezes, or rhonchi clear with a cough, which of the following is a likely etiology? Student Answer: Bronchitis Simple asthma Cystic fibrosis Heart failure Comments: Question 7. Question : Is the following information subjective or objective? Mr. Mazz has shortness of breath that has persisted for the past ten days; it is worse with activity and relieved by rest. Student Answer: Subjective Objective Comments: Question 8. Question : All of the following are implicated in causing chronic cough except: Student Answer: Chronic bronchitis Allergic rhinitis Acute viral upper respiratory infection Gastroesophageal reflux disease Comments: Question 9. Question : A mother brings her infant to you because of a “rattle” in his chest with breathing. Which of the following would you hear if there is a problem in the upper airway? Student Answer: Different sounds from the nose and the chest Asymmetric sounds Inspiratory sounds Sounds louder in the lower chest Comments: Question 10. Question : Which of the following is consistent with good percussion technique? Student Answer: Allow all of the fingers to touch the chest while performing percussion. Maintain a stiff wrist and hand. Leave the plexor finger on the pleximeter after each strike. Strike the pleximeter over the distal interphalangeal joint. [Show More]
Last updated: 3 years ago
Preview 1 out of 232 pages
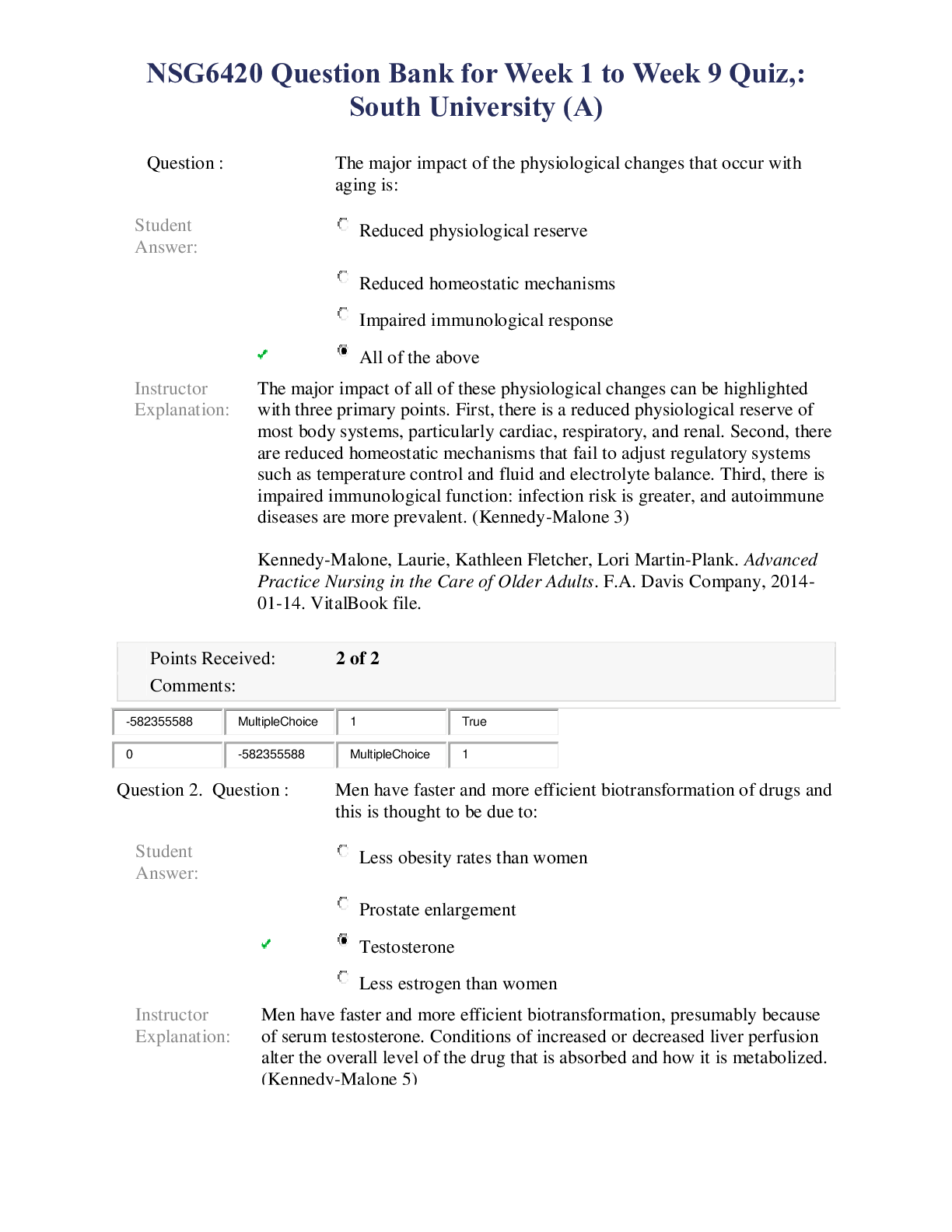
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Can't find what you want? Try our AI powered Search
Connected school, study & course
About the document
Uploaded On
Apr 09, 2020
Number of pages
232
Written in
All
This document has been written for:
Uploaded
Apr 09, 2020
Downloads
0
Views
167
Scholarfriends.com Online Platform by Browsegrades Inc. 651N South Broad St, Middletown DE. United States.
We're available through e-mail, Twitter, Facebook, and live chat.
FAQ
Questions? Leave a message!
Copyright © Scholarfriends · High quality services·