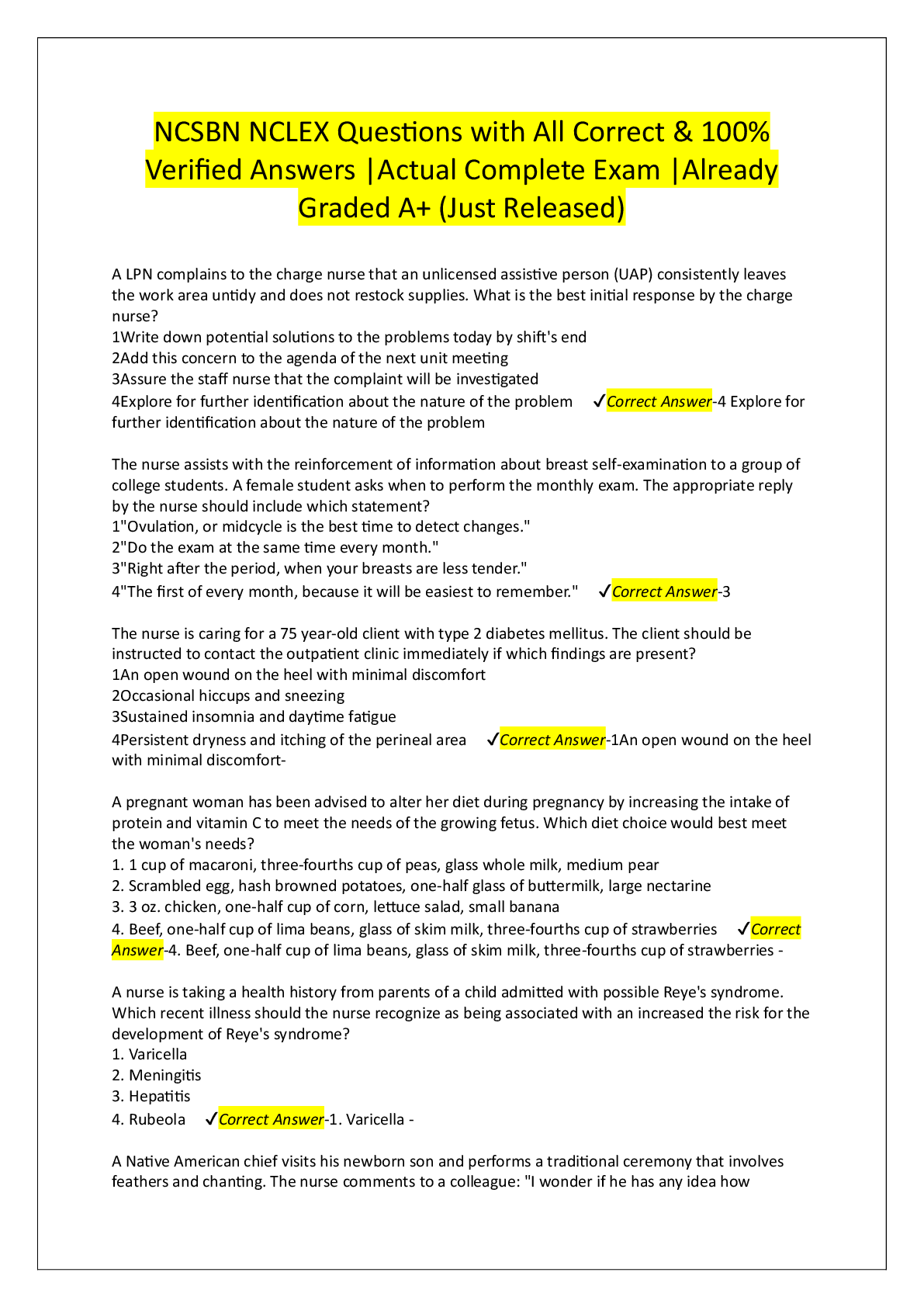
EXAM 2 HEALTH ASSESSMENT STUDY QUESTIONS 2020(LATEST UPDATE)
Document Content and Description Below
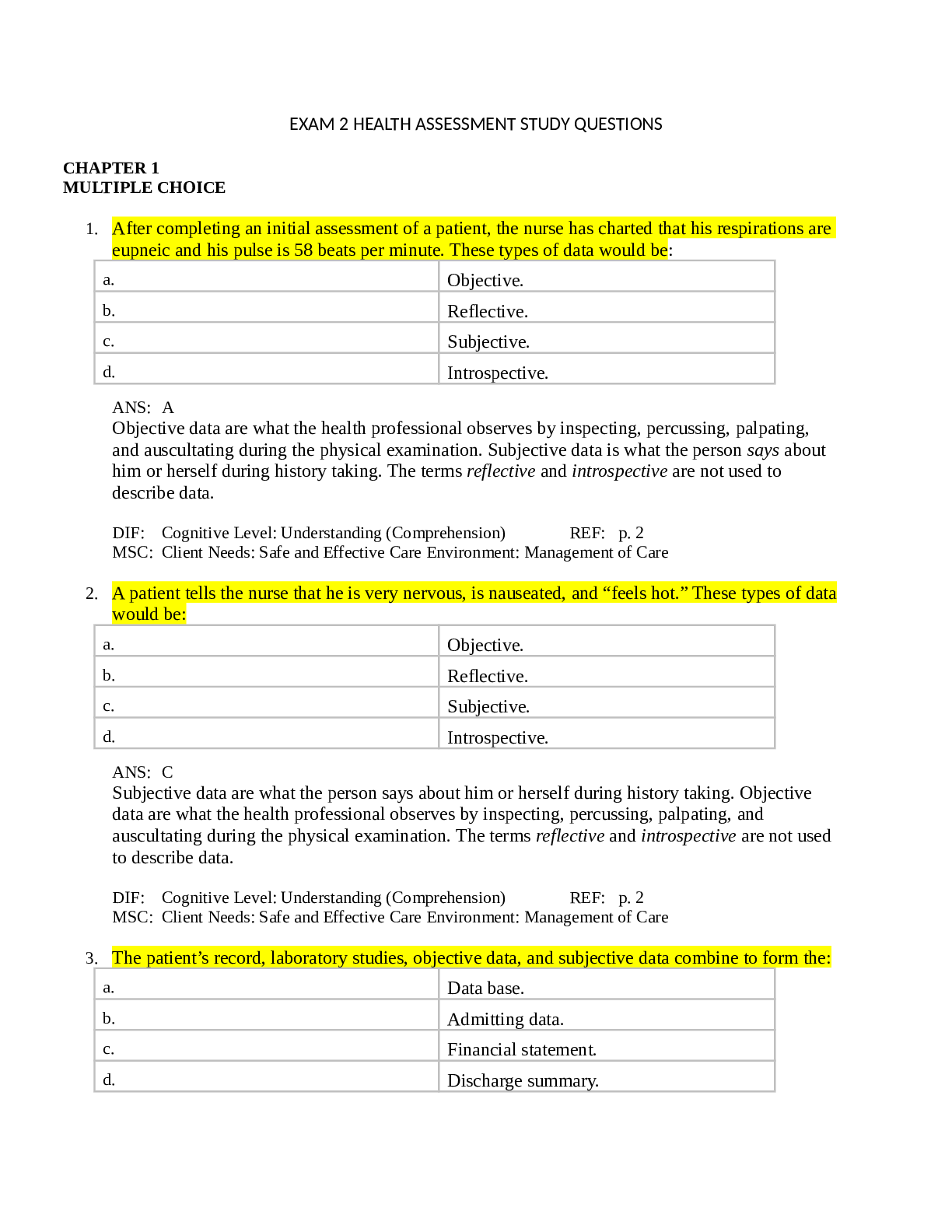
EXAM 2 HEALTH ASSESSMENT STUDY QUESTIONS CHAPTER 1 MULTIPLE CHOICE 1. After completing an initial assessment of a patient, the nurse has charted that his respirations are eupneic and his pulse is 58 b ... eats per minute. These types of data would be: a. Objective. b. Reflective. c. Subjective. d. Introspective. ANS: A Objective data are what the health professional observes by inspecting, percussing, palpating, and auscultating during the physical examination. Subjective data is what the person says about him or herself during history taking. The terms reflective and introspective are not used to describe data. DIF: Cognitive Level: Understanding (Comprehension) REF: p. 2 MSC: Client Needs: Safe and Effective Care Environment: Management of Care 2. A patient tells the nurse that he is very nervous, is nauseated, and “feels hot.” These types of data would be: a. Objective. b. Reflective. c. Subjective. d. Introspective. ANS: C Subjective data are what the person says about him or herself during history taking. Objective data are what the health professional observes by inspecting, percussing, palpating, and auscultating during the physical examination. The terms reflective and introspective are not used to describe data. DIF: Cognitive Level: Understanding (Comprehension) REF: p. 2 MSC: Client Needs: Safe and Effective Care Environment: Management of Care 3. The patient’s record, laboratory studies, objective data, and subjective data combine to form the: a. Data base. b. Admitting data. c. Financial statement. d. Discharge summary. ANS: A Together with the patient’s record and laboratory studies, the objective and subjective data form the data base. The other items are not part of the patient’s record, laboratory studies, or data. DIF: Cognitive Level: Remembering (Knowledge) REF: p. 2 MSC: Client Needs: Safe and Effective Care Environment: Management of Care 8. The nurse is conducting a class on priority setting for a group of new graduate nurses. Which is an example of a first-level priority problem? a. Patient with postoperative pain b. Newly diagnosed patient with diabetes who needs diabetic teaching c. Individual with a small laceration on the sole of the foot d. Individual with shortness of breath and respiratory distress ANS: D First-level priority problems are those that are emergent, life threatening, and immediate (e.g., establishing an airway, supporting breathing, maintaining circulation, monitoring abnormal vital signs) (see Table 1-1). DIF: Cognitive Level: Understanding (Comprehension) REF: p. 4 MSC: Client Needs: Safe and Effective Care Environment: Management of Care 9. When considering priority setting of problems, the nurse keeps in mind that second-level priority problems include which of these aspects? a. Low self-esteem b. Lack of knowledge c. Abnormal laboratory values d. Severely abnormal vital signs ANS: C Second-level priority problems are those that require prompt intervention to forestall further deterioration (e.g., mental status change, acute pain, abnormal laboratory values, risks to safety or security) (see Table 1-1). DIF: Cognitive Level: Understanding (Comprehension) REF: p. 4 MSC: Client Needs: Safe and Effective Care Environment: Management of Care 10. Which critical thinking skill helps the nurse see relationships among the data? a. Validation b. Clustering related cues c. Identifying gaps in data d. Distinguishing relevant from irrelevant ANS: B Clustering related cues helps the nurse see relationships among the data. DIF: Cognitive Level: Understanding (Comprehension) REF: p. 2 MSC: Client Needs: Safe and Effective Care Environment: Management of Care 11. The nurse knows that developing appropriate nursing interventions for a patient relies on the appropriateness of the __________ diagnosis. a. Nursing b. Medical c. Admission d. Collaborative ANS: A An accurate nursing diagnosis provides the basis for the selection of nursing interventions to achieve outcomes for which the nurse is accountable. The other items do not contribute to the development of appropriate nursing interventions. DIF: Cognitive Level: Understanding (Comprehension) REF: p. 6 MSC: Client Needs: Safe and Effective Care Environment: Management of Care 12. The nursing process is a sequential method of problem solving that nurses use and includes which steps? a. Assessment, treatment, planning, evaluation, discharge, and follow-up b. Admission, assessment, diagnosis, treatment, and discharge planning c. Admission, diagnosis, treatment, evaluation, and discharge planning d. Assessment, diagnosis, outcome identification, planning, implementation, and evaluation ANS: D The nursing process is a method of problem solving that includes assessment, diagnosis, outcome identification, planning, implementation, and evaluation. DIF: Cognitive Level: Understanding (Comprehension) REF: p. 3 MSC: Client Needs: Safe and Effective Care Environment: Management of Care 18. When reviewing the concepts of health, the nurse recalls that the components of holistic health include which of these? a. Disease originates from the external environment. b. The individual human is a closed system. c. Nurses are responsible for a patient’s health state. d. Holistic health views the mind, body, and spirit as interdependent. ANS: D Consideration of the whole person is the essence of holistic health, which views the mind, body, and spirit as interdependent. The basis of disease originates from both the external environment and from within the person. Both the individual human and the external environment are open systems, continually changing and adapting, and each person is responsible for his or her own personal health state. DIF: Cognitive Level: Understanding (Comprehension) REF: p. 7 MSC: Client Needs: Safe and Effective Care Environment: Management of Care CHAPTER 5 MULTIPLE CHOICE 1. During an examination, the nurse can assess mental status by which activity? a. Examining the patient’s electroencephalogram b. Observing the patient as he or she performs an intelligence quotient (IQ) test c. Observing the patient and inferring health or dysfunction d. Examining the patient’s response to a specific set of questions ANS: C Mental status cannot be directly scrutinized like the characteristics of skin or heart sounds. Its functioning is inferred through an assessment of an individual’s behaviors, such as consciousness, language, mood and affect, and other aspects. PTS: 1 DIF: Cognitive Level: Understanding (Comprehension) REF: p. 67 MSC: Client Needs: Psychosocial Integrity 2. The nurse is assessing the mental status of a child. Which statement about children and mental status is true? a. All aspects of mental status in children are interdependent. b. Children are highly labile and unstable until the age of 2 years. c. Children’s mental status is largely a function of their parents’ level of functioning until the age of 7 years. d. A child’s mental status is impossible to assess until the child develops the ability to concentrate. ANS: A Separating and tracing the development of only one aspect of mental status is difficult. All aspects are interdependent. For example, consciousness is rudimentary at birth because the cerebral cortex is not yet developed. The infant cannot distinguish the self from the mother’s body. The other statements are not true. PTS: 1 DIF: Cognitive Level: Understanding (Comprehension) REF: p. 68 MSC: Client Needs: Psychosocial Integrity 3. The nurse is assessing a 75-year-old man. As the nurse begins the mental status portion of the assessment, the nurse expects that this patient: a. Will have no decrease in any of his abilities, including response time. b. Will have difficulty on tests of remote memory because this ability typically decreases with age. c. May take a little longer to respond, but his general knowledge and abilities should not have declined. d. Will exhibit had a decrease in his response time because of the loss of language and a decrease in general knowledge. ANS: C The aging process leaves the parameters of mental status mostly intact. General knowledge does not decrease, and little or no loss in vocabulary occurs. Response time is slower than in a youth. It takes a little longer for the brain to process information and to react to it. Recent memory, which requires some processing, is somewhat decreased with aging, but remote memory is not affected. PTS: 1 DIF: Cognitive Level: Analyzing (Analysis) REF: p. 68 MSC: Client Needs: Psychosocial Integrity 4. When assessing aging adults, the nurse knows that one of the first things that should be assessed before making judgments about their mental status is: a. Presence of phobias b. General intelligence c. Presence of irrational thinking patterns d. Sensory-perceptive abilities ANS: D Age-related changes in sensory perception can affect mental status. For example, vision loss (as detailed in Chapter 14) may result in apathy, social isolation, and depression. Hearing changes are common in older adults, which produces frustration, suspicion, and social isolation and makes the person appear confused. PTS: 1 DIF: Cognitive Level: Analyzing (Analysis) REF: p. 68 MSC: Client Needs: Psychosocial Integrity 5. The nurse is preparing to conduct a mental status examination. Which statement is true regarding the mental status examination? a. A patient’s family is the best resource for information about the patient’s coping skills. b. Gathering mental status information during the health history interview is usually sufficient. c. Integrating the mental status examination into the health history interview takes an enormous amount of extra time. d. To get a good idea of the patient’s level of functioning, performing a complete mental status examination is usually necessary. ANS: B The full mental status examination is a systematic check of emotional and cognitive functioning. The steps described, however, rarely need to be taken in their entirety. Usually, one can assess mental status through the context of the health history interview. PTS: 1 DIF: Cognitive Level: Applying (Application) REF: p. 68 MSC: Client Needs: Psychosocial Integrity 6. A woman brings her husband to the clinic for an examination. She is particularly worried because after a recent fall, he seems to have lost a great deal of his memory of recent events. Which statement reflects the nurse’s best course of action? a. Perform a complete mental status examination. b. Refer him to a psychometrician. c. Plan to integrate the mental status examination into the history and physical examination. d. Reassure his wife that memory loss after a physical shock is normal and will soon subside. ANS: A Performing a complete mental status examination is necessary when any abnormality in affect or behavior is discovered or when family members are concerned about a person’s behavioral changes (e.g., memory loss, inappropriate social interaction) or after trauma, such as a head injury. PTS: 1 DIF: Cognitive Level: Applying (Application) REF: p. 69 MSC: Client Needs: Psychosocial Integrity 7. The nurse is conducting a patient interview. Which statement made by the patient should the nurse more fully explore during the interview? a. “I sleep like a baby.” b. “I have no health problems.” c. “I never did too good in school.” d. “I am not currently taking any medications.” ANS: C In every mental status examination, the following factors from the health history that could affect the findings should be noted: any known illnesses or health problems, such as alcoholism or chronic renal disease; current medications, the side effects of which may cause confusion or depression; the usual educational and behavioral level, noting this level as the patient’s normal baseline and not expecting a level of performance on the mental status examination to exceed it; and responses to personal history questions, indicating current stress, social interaction patterns, and sleep habits. PTS: 1 DIF: Cognitive Level: Analyzing (Analysis) REF: p. 69 MSC: Client Needs: Psychosocial Integrity 8. A patient is admitted to the unit after an automobile accident. The nurse begins the mental status examination and finds that the patient has dysarthric speech and is lethargic. The nurse’s best approach regarding this examination is to: a. Plan to defer the rest of the mental status examination. b. Skip the language portion of the examination, and proceed onto assessing mood and affect. c. Conduct an in-depth speech evaluation, and defer the mental status examination to another time. d. Proceed with the examination, and assess the patient for suicidal thoughts because dysarthria is often accompanied by severe depression. ANS: A In the mental status examination, the sequence of steps forms a hierarchy in which the most basic functions (consciousness, language) are assessed first. The first steps must be accurately assessed to ensure validity of the steps that follow. For example, if consciousness is clouded, then the person cannot be expected to have full attention and to cooperate with new learning. If language is impaired, then a subsequent assessment of new learning or abstract reasoning (anything that requires language functioning) can give erroneous conclusions. PTS: 1 DIF: Cognitive Level: Analyzing (Analysis) REF: p. 69 MSC: Client Needs: Psychosocial Integrity 9. A 19-year-old woman comes to the clinic at the insistence of her brother. She is wearing black combat boots and a black lace nightgown over the top of her other clothes. Her hair is dyed pink with black streaks throughout. She has several pierced holes in her nares and ears and is wearing an earring through her eyebrow and heavy black makeup. The nurse concludes that: a. She probably does not have any problems. b. She is only trying to shock people and that her dress should be ignored. c. She has a manic syndrome because of her abnormal dress and grooming. d. More information should be gathered to decide whether her dress is appropriate. ANS: D Grooming and hygiene should be noted—the person is clean and well groomed, hair is neat and clean, women have moderate or no makeup, and men are shaved or their beards or moustaches are well groomed. Care should be taken when interpreting clothing that is disheveled, bizarre, or in poor repair because these sometimes reflect the person’s economic status or a deliberate fashion trend. PTS: 1 DIF: Cognitive Level: Applying (Application) REF: p. 70 MSC: Client Needs: Psychosocial Integrity 10. A patient has been in the intensive care unit for 10 days. He has just been moved to the medical-surgical unit, and the admitting nurse is planning to perform a mental status examination. During the tests of cognitive function, the nurse would expect that he: a. May display some disruption in thought content. b. Will state, “I am so relieved to be out of intensive care.” c. Will be oriented to place and person, but the patient may not be certain of the date. d. May show evidence of some clouding of his level of consciousness. ANS: C The nurse can discern the orientation of cognitive function through the course of the interview or can directly and tactfully ask, “Some people have trouble keeping up with the dates while in the hospital. Do you know today’s date?” Many hospitalized people have trouble with the exact date but are fully oriented on the remaining items. PTS: 1 DIF: Cognitive Level: Analyzing (Analysis) REF: pp. 70-71 MSC: Client Needs: Psychosocial Integrity 11. During a mental status examination, the nurse wants to assess a patient’s affect. The nurse should ask the patient which question? a. “How do you feel today?” b. “Would you please repeat the following words?” c. “Have these medications had any effect on your pain?” d. “Has this pain affected your ability to get dressed by yourself?” ANS: A Judge mood and affect by body language and facial expression and by directly asking, “How do you feel today?” or “How do you usually feel?” The mood should be appropriate to the person’s place and condition and should appropriately change with the topics. PTS: 1 DIF: Cognitive Level: Applying (Application) REF: p. 70 MSC: Client Needs: Psychosocial Integrity 12. The nurse is planning to assess new memory with a patient. The best way for the nurse to do this would be to: a. Administer the FACT test. b. Ask him to describe his first job. c. Give him the Four Unrelated Words Test. d. Ask him to describe what television show he was watching before coming to the clinic. ANS: C Ask questions that can be corroborated, which screens for the occasional person who confabulates or makes up answers to fill in the gaps of memory loss. The Four Unrelated Words Test tests the person’s ability to lay down new memories and is a highly sensitive and valid memory test. PTS: 1 DIF: Cognitive Level: Applying (Application) REF: p. 71 MSC: Client Needs: Psychosocial Integrity 13. A 45-year-old woman is at the clinic for a mental status assessment. In giving her the Four Unrelated Words Test, the nurse would be concerned if she could not ____ four unrelated words ____. a. Invent; within 5 minutes b. Invent; within 30 seconds c. Recall; after a 30-minute delay d. Recall; after a 60-minute delay ANS: C The Four Unrelated Words Test tests the person’s ability to lay down new memories. It is a highly sensitive and valid memory test. It requires more effort than the recall of personal or historic events. To the person say, “I am going to say four words. I want you to remember them. In a few minutes I will ask you to recall them.” After 5 minutes, ask for the four words. The normal response for persons under 60 years is an accurate three- or four-word recall after a 5-, 10-, and 30-minute delay. PTS: 1 DIF: Cognitive Level: Analyzing (Analysis) REF: p. 71 MSC: Client Needs: Psychosocial Integrity 14. During a mental status assessment, which question by the nurse would best assess a person’s judgment? a. “Do you feel that you are being watched, followed, or controlled?” b. “Tell me what you plan to do once you are discharged from the hospital.” c. “What does the statement, ‘People in glass houses shouldn’t throw stones,’ mean to you?” d. “What would you do if you found a stamped, addressed envelope lying on the sidewalk?” ANS: B A person exercises judgment when he or she can compare and evaluate the alternatives in a situation and reach an appropriate course of action. Rather than testing the person’s response to a hypothetical situation (as illustrated in the option with the envelope), the nurse should be more interested in the person’s judgment about daily or long-term goals, the likelihood of acting in response to delusions or hallucinations, and the capacity for violent or suicidal behavior. PTS: 1 DIF: Cognitive Level: Applying (Application) REF: p. 74 MSC: Client Needs: Psychosocial Integrity 15. Which of these individuals would the nurse consider at highest risk for a suicide attempt? a. Man who jokes about death b. Woman who, during a past episode of major depression, attempted suicide c. Adolescent who just broke up with her boyfriend and states that she would like to kill herself d. Older adult man who tells the nurse that he is going to “join his wife in heaven” tomorrow and plans to use a gun ANS: D When the person expresses feelings of sadness, hopelessness, despair, or grief, assessing any possible risk of physical harm to him or herself is important. The interview should begin with more general questions. If the nurse hears affirmative answers, then he or she should continue with more specific questions. A precise suicide plan to take place in the next 24 to 48 hours with use of a lethal method constitutes high risk. PTS: 1 DIF: Cognitive Level: Applying (Application) REF: p. 74 MSC: Client Needs: Psychosocial Integrity 16. The nurse is performing a mental status assessment on a 5-year-old girl. Her parents are undergoing a bitter divorce and are worried about the effect it is having on their daughter. Which action or statement might lead the nurse to be concerned about the girl’s mental status? a. She clings to her mother whenever the nurse is in the room. b. She appears angry and will not make eye contact with the nurse. c. Her mother states that she has begun to ride a tricycle around their yard. d. Her mother states that her daughter prefers to play with toddlers instead of kids her own age while in daycare. ANS: D The mental status assessment of infants and children covers behavioral, cognitive, and psychosocial development and examines how the child is coping with his or her environment. Essentially, the nurse should follow the same Association for Behavioral and Cognitive Therapies (ABCT) guidelines as those for the adult, with special consideration for developmental milestones. The best examination technique arises from a thorough knowledge of the developmental milestones (described in Chapter 2). Abnormalities are often problems of omission (e.g., the child does not achieve a milestone as expected). PTS: 1 DIF: Cognitive Level: Applying (Application) REF: p. 75 MSC: Client Needs: Psychosocial Integrity 17. The nurse is assessing orientation in a 79-year-old patient. Which of these responses would lead the nurse to conclude that this patient is oriented? a. “I know my name is John. I couldn’t tell you where I am. I think it is 2010, though.” b. “I know my name is John, but to tell you the truth, I get kind of confused about the date.” c. “I know my name is John; I guess I’m at the hospital in Spokane. No, I don’t know the date.” d. “I know my name is John. I am at the hospital in Spokane. I couldn’t tell you what date it is, but I know that it is February of a new year—2010.” ANS: D Many aging persons experience social isolation, loss of structure without a job, a change in residence, or some short-term memory loss. These factors affect orientation, and the person may not provide the precise date or complete name of the agency. You may consider aging persons oriented if they generally know where they are and the present period. They should be considered oriented to time if the year and month are correctly stated. Orientation to place is accepted with the correct identification of the type of setting (e.g., hospital) and the name of the town. PTS: 1 DIF: Cognitive Level: Applying (Application) REF: p. 76 MSC: Client Needs: Psychosocial Integrity 18. The nurse is performing the Denver II screening test on a 12-month-old infant during a routine well-child visit. The nurse should tell the infant’s parents that the Denver II: a. Tests three areas of development: cognitive, physical, and psychological b. Will indicate whether the child has a speech disorder so that treatment can begin. c. Is a screening instrument designed to detect children who are slow in development. d. Is a test to determine intellectual ability and may indicate whether problems will develop later in school. ANS: C The Denver II is a screening instrument designed to detect developmental delays in infants and preschoolers. It tests four functions: gross motor, language, fine motor-adaptive, and personal-social. The Denver II is not an intelligence test; it does not predict current or future intellectual ability. It is not diagnostic; it does not suggest treatment regimens. PTS: 1 DIF: Cognitive Level: Applying (Application) REF: p. 75 MSC: Client Needs: Psychosocial Integrity 19. A patient drifts off to sleep when she is not being stimulated. The nurse can easily arouse her by calling her name, but the patient remains drowsy during the conversation. The best description of this patient’s level of consciousness would be: a. Lethargic b. Obtunded c. Stuporous d. Semialert ANS: A Lethargic (or somnolent) is when the person is not fully alert, drifts off to sleep when not stimulated, and can be aroused when called by name in a normal voice but looks drowsy. He or she appropriately responds to questions or commands, but thinking seems slow and fuzzy. He or she is inattentive and loses the train of thought. Spontaneous movements are decreased. (See Table 5-3 for the definitions of the other terms.) PTS: 1 DIF: Cognitive Level: Understanding (Comprehension) REF: p. 79 MSC: Client Needs: Psychosocial Integrity 20. A patient has had a cerebrovascular accident (stroke). He is trying very hard to communicate. He seems driven to speak and says, “I buy obie get spirding and take my train.” What is the best description of this patient’s problem? a. Global aphasia b. Broca’s aphasia c. Echolalia d. Wernicke’s aphasia ANS: D This type of communication illustrates Wernicke’s or receptive aphasia. The person can hear sounds and words but cannot relate them to previous experiences. Speech is fluent, effortless, and well articulated, but it has many paraphasias (word substitutions that are malformed or wrong) and neologisms (made-up words) and often lacks substantive words. Speech can be totally incomprehensible. Often, a great urge to speak is present. Repetition, reading, and writing also are impaired. Echolalia is an imitation or the repetition of another person’s words or phrases. (See Table 5-4 for the definitions of the other disorders.) PTS: 1 DIF: Cognitive Level: Applying (Application) REF: p. 80 MSC: Client Needs: Psychosocial Integrity 21. A patient repeatedly seems to have difficulty coming up with a word. He says, “I was on my way to work, and when I got there, the thing that you step into that goes up in the air was so full that I decided to take the stairs.” The nurse will note on his chart that he is using or experiencing: a. Blocking b. Neologism c. Circumlocution d. Circumstantiality ANS: C Circumlocution is a roundabout expression, substituting a phrase when one cannot think of the name of the object. PTS: 1 DIF: Cognitive Level: Understanding (Comprehension) REF: p. 84 MSC: Client Needs: Psychosocial Integrity 22. During an examination, the nurse notes that a patient is exhibiting flight of ideas. Which statement by the patient is an example of flight of ideas? a. “My stomach hurts. Hurts, spurts, burts.” b. “Kiss, wood, reading, ducks, onto, maybe.” c. “Take this pill? The pill is red. I see red. Red velvet is soft, soft as a baby’s bottom.” d. “I wash my hands, wash them, wash them. I usually go to the sink and wash my hands.” ANS: C Flight of ideas is demonstrated by an abrupt change, rapid skipping from topic to topic, and practically continuous flow of accelerated speech. Topics usually have recognizable associations or are plays on words. PTS: 1 DIF: Cognitive Level: Understanding (Comprehension) REF: p. 84 MSC: Client Needs: Psychosocial Integrity 23. A patient describes feeling an unreasonable, irrational fear of snakes. His fear is so persistent that he can no longer comfortably look at even pictures of snakes and has made an effort to identify all the places he might encounter a snake and avoids them. The nurse recognizes that he: a. Has a snake phobia. b. Is a hypochondriac; snakes are usually harmless. c. Has an obsession with snakes. d. Has a delusion that snakes are harmful, which must stem from an early traumatic incident involving snakes. ANS: A A phobia is a strong, persistent, irrational fear of an object or situation; the person feels driven to avoid it. (See Table 5-7 for the definitions of the other terms.) PTS: 1 DIF: Cognitive Level: Applying (Application) REF: p. 85 MSC: Client Needs: Psychosocial Integrity 24. A patient has been diagnosed with schizophrenia. During a recent interview, he shows the nurse a picture of a man holding a decapitated head. He describes this picture as horrifying but then laughs loudly at the content. This behavior is a display of: a. Confusion b. Ambivalence c. Depersonalization d. Inappropriate affect ANS: D An inappropriate affect is an affect clearly discordant with the content of the person’s speech. (See Table 5-5 for the definitions of the other terms.) PTS: 1 DIF: Cognitive Level: Analyzing (Analysis) REF: p. 81 MSC: Client Needs: Psychosocial Integrity 25. During reporting, the nurse hears that a patient is experiencing hallucinations. Which is an example of a hallucination? a. Man believes that his dead wife is talking to him. b. Woman hears the doorbell ring and goes to answer it, but no one is there. c. Child sees a man standing in his closet. When the lights are turned on, it is only a dry cleaning bag. d. Man believes that the dog has curled up on the bed, but when he gets closer he sees that it is a blanket. ANS: A Hallucinations are sensory perceptions for which no external stimuli exist. They may strike any sense: visual, auditory, tactile, olfactory, or gustatory. PTS: 1 DIF: Cognitive Level: Remembering (Knowledge) REF: p. 85 MSC: Client Needs: Psychosocial Integrity 26. A 20-year-old construction worker has been brought into the emergency department with heat stroke. He has delirium as a result of a fluid and electrolyte imbalance. For the mental status examination, the nurse should first assess the patient’s: a. Affect and mood b. Memory and affect c. Language abilities d. Level of consciousness and cognitive abilities ANS: D Delirium is a disturbance of consciousness (i.e., reduced clarity of awareness of the environment) with reduced ability to focus, sustain, or shift attention. Delirium is not an alteration in mood, affect, or language abilities. PTS: 1 DIF: Cognitive Level: Understanding (Comprehension) REF: p. 69 MSC: Client Needs: Psychosocial Integrity 27. A patient states, “I feel so sad all of the time. I can’t feel happy even doing things I used to like to do.” He also states that he is tired, sleeps poorly, and has no energy. To differentiate between a dysthymic disorder and a major depressive disorder, the nurse should ask which question? a. “Have you had any weight changes?” b. “Are you having any thoughts of suicide?” c. “How long have you been feeling this way?” d. “Are you having feelings of worthlessness?” ANS: C Major depressive disorder is characterized by one or more major depressive episodes, that is, at least 2 weeks of depressed mood or loss of interest accompanied by at least four additional symptoms of depression. Dysthymic disorder is characterized by at least 2 years of depressed mood for more days than not, accompanied by additional depressive symptoms. PTS: 1 DIF: Cognitive Level: Analyzing (Analysis) REF: p. 73 MSC: Client Needs: Psychosocial Integrity 28. A 26-year-old woman was robbed and beaten a month ago. She is returning to the clinic today for a follow-up assessment. The nurse will want to ask her which one of these questions? a. “How are things going with the trial?” b. “How are things going with your job?” c. “Tell me about your recent engagement!” d. “Are you having any disturbing dreams?” ANS: D In posttraumatic stress disorder, the person has been exposed to a traumatic event. The traumatic event is persistently reexperienced by recurrent and intrusive, distressing recollections of the event, including images, thoughts, or perceptions; recurrent distressing dreams of the event; and acting or feeling as if the traumatic event were recurring. PTS: 1 DIF: Cognitive Level: Applying (Application) REF: p. 82 MSC: Client Needs: Psychosocial Integrity 29. The nurse is performing a mental status examination. Which statement is true regarding the assessment of mental status? a. Mental status assessment diagnoses specific psychiatric disorders. b. Mental disorders occur in response to everyday life stressors. c. Mental status functioning is inferred through the assessment of an individual’s behaviors. d. Mental status can be directly assessed, similar to other systems of the body (e.g., heart sounds, breath sounds). ANS: C Mental status functioning is inferred through the assessment of an individual’s behaviors. It cannot be directly assessed like the characteristics of the skin or heart sounds. PTS: 1 DIF: Cognitive Level: Understanding (Comprehension) REF: p. 67 MSC: Client Needs: Psychosocial Integrity 30. A 23-year-old patient in the clinic appears anxious. Her speech is rapid, and she is fidgety and in constant motion. Which of these questions or statements would be most appropriate for the nurse to use in this situation to assess attention span? a. “How do you usually feel? Is this normal behavior for you?” b. “I am going to say four words. In a few minutes, I will ask you to recall them.” c. “Describe the meaning of the phrase, ‘Looking through rose-colored glasses.’” d. “Pick up the pencil in your left hand, move it to your right hand, and place it on the table.” ANS: D Attention span is evaluated by assessing the individual’s ability to concentrate and complete a thought or task without wandering. Giving a series of directions to follow is one method used to assess attention span. PTS: 1 DIF: Cognitive Level: Applying (Application) REF: p. 71 MSC: Client Needs: Psychosocial Integrity 31. The nurse is planning health teaching for a 65-year-old woman who has had a cerebrovascular accident (stroke) and has aphasia. Which of these questions is most important to use when assessing mental status in this patient? a. “Please count backward from 100 by seven.” b. “I will name three items and ask you to repeat them in a few minutes.” c. “Please point to articles in the room and parts of the body as I name them.” d. “What would you do if you found a stamped, addressed envelope on the sidewalk?” ANS: C Additional tests for persons with aphasia include word comprehension (asking the individual to point to articles in the room or parts of the body), reading (asking the person to read available print), and writing (asking the person to make up and write a sentence). PTS: 1 DIF: Cognitive Level: Applying (Application) REF: p. 71 MSC: Client Needs: Psychosocial Integrity CHAPTER 18 MULTIPLE CHOICE 1. Which of these statements is true regarding the vertebra prominens? The vertebra prominens is: a. The spinous process of C7. b. Usually nonpalpable in most individuals. c. Opposite the interior border of the scapula. d. Located next to the manubrium of the sternum. ANS: A The spinous process of C7 is the vertebra prominens and is the most prominent bony spur protruding at the base of the neck. Counting ribs and intercostal spaces on the posterior thorax is difficult because of the muscles and soft tissue. The vertebra prominens is easier to identify and is used as a starting point in counting thoracic processes and identifying landmarks on the posterior chest. DIF: Cognitive Level: Remembering (Knowledge) REF: p. 414 MSC: Client Needs: General 2. When performing a respiratory assessment on a patient, the nurse notices a costal angle of approximately 90 degrees. This characteristic is: a. Observed in patients with kyphosis. b. Indicative of pectus excavatum. c. A normal finding in a healthy adult. d. An expected finding in a patient with a barrel chest. ANS: C The right and left costal margins form an angle where they meet at the xiphoid process. Usually, this angle is 90 degrees or less. The angle increases when the rib cage is chronically overinflated, as in emphysema. DIF: Cognitive Level: Understanding (Comprehension) REF: p. 414 MSC: Client Needs: Safe and Effective Care Environment: Management of Care 3. When assessing a patient’s lungs, the nurse recalls that the left lung: a. Consists of two lobes. b. Is divided by the horizontal fissure. c. Primarily consists of an upper lobe on the posterior chest. d. Is shorter than the right lung because of the underlying stomach. ANS: A The left lung has two lobes, and the right lung has three lobes. The right lung is shorter than the left lung because of the underlying liver. The left lung is narrower than the right lung because the heart bulges to the left. The posterior chest is almost all lower lobes. DIF: Cognitive Level: Remembering (Knowledge) REF: p. 415 MSC: Client Needs: General 4. Which statement about the apices of the lungs is true? The apices of the lungs: a. Are at the level of the second rib anteriorly. b. Extend 3 to 4 cm above the inner third of the clavicles. c. Are located at the sixth rib anteriorly and the eighth rib laterally. d. Rest on the diaphragm at the fifth intercostal space in the midclavicular line (MCL). ANS: B The apex of the lung on the anterior chest is 3 to 4 cm above the inner third of the clavicles. On the posterior chest, the apices are at the level of C7. DIF: Cognitive Level: Remembering (Knowledge) REF: p. 415 MSC: Client Needs: General 5. During an examination of the anterior thorax, the nurse is aware that the trachea bifurcates anteriorly at the: a. Costal angle. b. Sternal angle. c. Xiphoid process. d. Suprasternal notch. ANS: B The sternal angle marks the site of tracheal bifurcation into the right and left main bronchi; it corresponds with the upper borders of the atria of the heart, and it lies above the fourth thoracic vertebra on the back. DIF: Cognitive Level: Remembering (Knowledge) REF: p. 416 MSC: Client Needs: Safe and Effective Care Environment: Management of Care 6. During an assessment, the nurse knows that expected assessment findings in the normal adult lung include the presence of: a. Adventitious sounds and limited chest expansion. b. Increased tactile fremitus and dull percussion tones. c. Muffled voice sounds and symmetric tactile fremitus. d. Absent voice sounds and hyperresonant percussion tones. ANS: C Normal lung findings include symmetric chest expansion, resonant percussion tones, vesicular breath sounds over the peripheral lung fields, muffled voice sounds, and no adventitious sounds. DIF: Cognitive Level: Understanding (Comprehension) REF: p. 426 |p. 431 MSC: Client Needs: Safe and Effective Care Environment: Management of Care 7. The primary muscles of respiration include the: a. Diaphragm and intercostals. b. Sternomastoids and scaleni. c. Trapezii and rectus abdominis. d. External obliques and pectoralis major. ANS: A The major muscle of respiration is the diaphragm. The intercostal muscles lift the sternum and elevate the ribs during inspiration, increasing the anteroposterior diameter. Expiration is primarily passive. Forced inspiration involves the use of other muscles, such as the accessory neck muscles—sternomastoid, scaleni, and trapezii muscles. Forced expiration involves the abdominal muscles. DIF: Cognitive Level: Remembering (Knowledge) REF: p. 418 MSC: Client Needs: General 8. A 65-year-old patient with a history of heart failure comes to the clinic with complaints of “being awakened from sleep with shortness of breath.” Which action by the nurse is most appropriate? a. Obtaining a detailed health history of the patient’s allergies and a history of asthma b. Telling the patient to sleep on his or her right side to facilitate ease of respirations c. Assessing for other signs and symptoms of paroxysmal nocturnal dyspnea d. Assuring the patient that paroxysmal nocturnal dyspnea is normal and will probably resolve within the next week ANS: C The patient is experiencing paroxysmal nocturnal dyspnea—being awakened from sleep with shortness of breath and the need to be upright to achieve comfort. DIF: Cognitive Level: Applying (Application) REF: p. 421 MSC: Client Needs: Safe and Effective Care Environment: Management of Care 9. When assessing tactile fremitus, the nurse recalls that it is normal to feel tactile fremitus most intensely over which location? a. Between the scapulae b. Third intercostal space, MCL c. Fifth intercostal space, midaxillary line (MAL) d. Over the lower lobes, posterior side ANS: A Normally, fremitus is most prominent between the scapulae and around the sternum. These sites are where the major bronchi are closest to the chest wall. Fremitus normally decreases as one progresses down the chest because more tissue impedes sound transmission. DIF: Cognitive Level: Understanding (Comprehension) REF: p. 426 MSC: Client Needs: Safe and Effective Care Environment: Management of Care 10. The nurse is reviewing the technique of palpating for tactile fremitus with a new graduate. Which statement by the graduate nurse reflects a correct understanding of tactile fremitus? “Tactile fremitus: a. “Is caused by moisture in the alveoli.” b. “Indicates that air is present in the subcutaneous tissues.” c. “Is caused by sounds generated from the larynx.” d. “Reflects the blood flow through the pulmonary arteries.” ANS: C Fremitus is a palpable vibration. Sounds generated from the larynx are transmitted through patent bronchi and the lung parenchyma to the chest wall where they are felt as vibrations. Crepitus is the term for air in the subcutaneous tissues. DIF: Cognitive Level: Understanding (Comprehension) REF: p. 426 MSC: Client Needs: Safe and Effective Care Environment: Management of Care 11. During percussion, the nurse knows that a dull percussion note elicited over a lung lobe most likely results from: a. Shallow breathing. b. Normal lung tissue. c. Decreased adipose tissue. d. Increased density of lung tissue. ANS: D A dull percussion note indicates an abnormal density in the lungs, as with pneumonia, pleural effusion, atelectasis, or a tumor. Resonance is the expected finding in normal lung tissue. DIF: Cognitive Level: Understanding (Comprehension) REF: p. 427 MSC: Client Needs: General 12. The nurse is observing the auscultation technique of another nurse. The correct method to use when progressing from one auscultatory site on the thorax to another is _______ comparison. a. Side-to-side b. Top-to-bottom c. Posterior-to-anterior d. Interspace-by-interspace ANS: A Side-to-side comparison is most important when auscultating the chest. The nurse should listen to at least one full respiration in each location. The other techniques are not correct. DIF: Cognitive Level: Understanding (Comprehension) REF: p. 435 MSC: Client Needs: Safe and Effective Care Environment: Management of Care 13. When auscultating the lungs of an adult patient, the nurse notes that low-pitched, soft breath sounds are heard over the posterior lower lobes, with inspiration being longer than expiration. The nurse interprets that these sounds are: a. Normally auscultated over the trachea. b. Bronchial breath sounds and normal in that location. c. Vesicular breath sounds and normal in that location. d. Bronchovesicular breath sounds and normal in that location. ANS: C Vesicular breath sounds are low-pitched, soft sounds with inspiration being longer than expiration. These breath sounds are expected over the peripheral lung fields where air flows through smaller bronchioles and alveoli. DIF: Cognitive Level: Applying (Application) REF: p. 430 MSC: Client Needs: Safe and Effective Care Environment: Management of Care 14. The nurse is auscultating the chest in an adult. Which technique is correct? a. Instructing the patient to take deep, rapid breaths b. Instructing the patient to breathe in and out through his or her nose c. Firmly holding the diaphragm of the stethoscope against the chest d. Lightly holding the bell of the stethoscope against the chest to avoid friction ANS: C Firmly holding the diaphragm of the stethoscope against the chest is the correct way to auscultate breath sounds. The patient should be instructed to breathe through his or her mouth, a little deeper than usual, but not to hyperventilate. DIF: Cognitive Level: Understanding (Comprehension) REF: p. 429 MSC: Client Needs: Safe and Effective Care Environment: Management of Care 19. When assessing the respiratory system of a 4-year-old child, which of these findings would the nurse expect? a. Crepitus palpated at the costochondral junctions b. No diaphragmatic excursion as a result of a child’s decreased inspiratory volume c. Presence of bronchovesicular breath sounds in the peripheral lung fields d. Irregular respiratory pattern and a respiratory rate of 40 breaths per minute at rest ANS: C Bronchovesicular breath sounds in the peripheral lung fields of the infant and young child up to age 5 or 6 years are normal findings. Their thin chest walls with underdeveloped musculature do not dampen the sound, as do the thicker chest walls of adults; therefore, breath sounds are loud and harsh. DIF: Cognitive Level: Applying (Application) REF: p. 437 MSC: Client Needs: Safe and Effective Care Environment: Management of Care 20. When inspecting the anterior chest of an adult, the nurse should include which assessment? a. Diaphragmatic excursion b. Symmetric chest expansion c. Presence of breath sounds d. Shape and configuration of the chest wall ANS: D Inspection of the anterior chest includes shape and configuration of the chest wall; assessment of the patient’s level of consciousness and the patient’s skin color and condition; quality of respirations; presence or absence of retraction and bulging of the intercostal spaces; and use of accessory muscles. Symmetric chest expansion is assessed by palpation. Diaphragmatic excursion is assessed by percussion of the posterior chest. Breath sounds are assessed by auscultation. DIF: Cognitive Level: Understanding (Comprehension) REF: p. 432 MSC: Client Needs: Safe and Effective Care Environment: Management of Care 21. The nurse knows that auscultation of fine crackles would most likely be noticed in: a. A healthy 5-year-old child. b. A pregnant woman. c. The immediate newborn period. d. Association with a pneumothorax. ANS: C Fine crackles are commonly heard in the immediate newborn period as a result of the opening of the airways and a clearing of fluid. Persistent fine crackles would be noticed with pneumonia, bronchiolitis, or atelectasis. DIF: Cognitive Level: Applying (Application) REF: p. 438 MSC: Client Needs: Safe and Effective Care Environment: Management of Care 24. The nurse is reviewing the characteristics of breath sounds. Which statement about bronchovesicular breath sounds is true? Bronchovesicular breath sounds are: a. Musical in quality. b. Usually caused by a pathologic disease. c. Expected near the major airways. d. Similar to bronchial sounds except shorter in duration. ANS: C Bronchovesicular breath sounds are heard over major bronchi where fewer alveoli are located posteriorly—between the scapulae, especially on the right; and anteriorly, around the upper sternum in the first and second intercostal spaces. The other responses are not correct. DIF: Cognitive Level: Understanding (Comprehension) REF: p. 430 MSC: Client Needs: Safe and Effective Care Environment: Management of Care 35. During auscultation of breath sounds, the nurse should correctly use the stethoscope in which of the following ways? a. Listening to at least one full respiration in each location b. Listening as the patient inhales and then going to the next site during exhalation c. Instructing the patient to breathe in and out rapidly while listening to the breath sounds d. If the patient is modest, listening to sounds over his or her clothing or hospital gown ANS: A During auscultation of breath sounds with a stethoscope, listening to one full respiration in each location is important. During the examination, the nurse should monitor the breathing and offer times for the person to breathe normally to prevent possible dizziness. DIF: Cognitive Level: Applying (Application) REF: p. 429 MSC: Client Needs: Safe and Effective Care Environment: Management of Care 38. The nurse is auscultating the lungs of a patient who had been sleeping and notices short, popping, crackling sounds that stop after a few breaths. The nurse recognizes that these breath sounds are: a. Atelectatic crackles that do not have a pathologic cause. b. Fine crackles and may be a sign of pneumonia. c. Vesicular breath sounds. d. Fine wheezes. ANS: A One type of adventitious sound, atelectatic crackles, does not have a pathologic cause. They are short, popping, crackling sounds that sound similar to fine crackles but do not last beyond a few breaths. When sections of alveoli are not fully aerated (as in people who are asleep or in older adults), they deflate slightly and accumulate secretions. Crackles are heard when these sections are expanded by a few deep breaths. Atelectatic crackles are heard only in the periphery, usually in dependent portions of the lungs, and disappear after the first few breaths or after a cough. DIF: Cognitive Level: Analyzing (Analysis) REF: p. 431 MSC: Client Needs: Safe and Effective Care Environment: Management of Care 39. A patient has been admitted to the emergency department for a suspected drug overdose. His respirations are shallow, with an irregular pattern, with a rate of 12 respirations per minute. The nurse interprets this respiration pattern as which of the following? a. Bradypnea b. Cheyne-Stokes respirations c. Hypoventilation d. Chronic obstructive breathing ANS: C Hypoventilation is characterized by an irregular, shallow pattern, and can be caused by an overdose of narcotics or anesthetics. Bradypnea is slow breathing, with a rate less than 10 respirations per minute. (See Table 18-4 for descriptions of Cheyne-Stokes respirations and chronic obstructive breathing.) DIF: Cognitive Level: Analyzing (Analysis) REF: p. 444 MSC: Client Needs: Safe and Effective Care Environment: Management of Care 40. A patient with pleuritis has been admitted to the hospital and complains of pain with breathing. What other key assessment finding would the nurse expect to find upon auscultation? a. Stridor b. Friction rub c. Crackles d. Wheezing ANS: B A patient with pleuritis will exhibit a pleural friction rub upon auscultation. This sound is made when the pleurae become inflamed and rub together during respiration. The sound is superficial, coarse, and low-pitched, as if two pieces of leather are being rubbed together. Stridor is associated with croup, acute epiglottitis in children, and foreign body inhalation. Crackles are associated with pneumonia, heart failure, chronic bronchitis, and other diseases (see Table 18-6). Wheezes are associated with diffuse airway obstruction caused by acute asthma or chronic emphysema. DIF: Cognitive Level: Applying (Application) REF: p. 449 MSC: Client Needs: Safe and Effective Care Environment: Management of Care MULTIPLE RESPONSE 1. The nurse is assessing voice sounds during a respiratory assessment. Which of these findings indicates a normal assessment? Select all that apply. a. Voice sounds are faint, muffled, and almost inaudible when the patient whispers “one, two, three” in a very soft voice. b. As the patient repeatedly says “ninety-nine,” the examiner clearly hears the words “ninety-nine.” c. When the patient speaks in a normal voice, the examiner can hear a sound but cannot exactly distinguish what is being said. d. As the patient says a long “ee-ee-ee” sound, the examiner also hears a long “ee-ee-ee” sound. e. As the patient says a long “ee-ee-ee” sound, the examiner hears a long “aaaaaa” sound. ANS: A, C, D As a patient repeatedly says “ninety-nine,” normally the examiner hears voice sounds but cannot distinguish what is being said. If a clear “ninety-nine” is auscultated, then it could indicate increased lung density, which enhances the transmission of voice sounds, which is a measure of bronchophony. When a patient says a long “ee-ee-ee” sound, normally the examiner also hears a long “ee-ee-ee” sound through auscultation, which is a measure of egophony. If the examiner hears a long “aaaaaa” sound instead, this sound could indicate areas of consolidation or compression. With whispered pectoriloquy, as when a patient whispers a phrase such as “one-two-three,” the normal response when auscultating voice sounds is to hear sounds that are faint, muffled, and almost inaudible. If the examiner clearly hears the whispered voice, as if the patient is speaking through the stethoscope, then consolidation of the lung fields may exist. DIF: Cognitive Level: Applying (Application) REF: p. 449 MSC: Client Needs: Safe and Effective Care Environment: Management of Care CHAPTER 19 MULTIPLE CHOICE 1. The sac that surrounds and protects the heart is called the: a. Pericardium. b. Myocardium. c. Endocardium. d. Pleural space. ANS: A The pericardium is a tough, fibrous double-walled sac that surrounds and protects the heart. It has two layers that contain a few milliliters of serous pericardial fluid. DIF: Cognitive Level: Remembering (Knowledge) REF: p. 460 MSC: Client Needs: General 2. The direction of blood flow through the heart is best described by which of these? a. Vena cava right atrium right ventricle lungs pulmonary artery left atrium left ventricle b. Right atrium right ventricle pulmonary artery lungs pulmonary vein left atrium left ventricle c. Aorta right atrium right ventricle lungs pulmonary vein left atrium left ventricle vena cava d. Right atrium right ventricle pulmonary vein lungs pulmonary artery left atrium left ventricle ANS: B Returning blood from the body empties into the right atrium and flows into the right ventricle and then goes to the lungs through the pulmonary artery. The lungs oxygenate the blood, and it is then returned to the left atrium through the pulmonary vein. The blood goes from there to the left ventricle and then out to the body through the aorta. DIF: Cognitive Level: Remembering (Knowledge) REF: p. 461|p. 463 MSC: Client Needs: General 3. The nurse is reviewing the anatomy and physiologic functioning of the heart. Which statement best describes what is meant by atrial kick? a. The atria contract during systole and attempt to push against closed valves. b. Contraction of the atria at the beginning of diastole can be felt as a palpitation. c. Atrial kick is the pressure exerted against the atria as the ventricles contract during systole. d. The atria contract toward the end of diastole and push the remaining blood into the ventricles. ANS: D Toward the end of diastole, the atria contract and push the last amount of blood (approximately 25% of stroke volume) into the ventricles. This active filling phase is called presystole, or atrial systole, or sometimes the atrial kick. DIF: Cognitive Level: Remembering (Knowledge) REF: p. 463 MSC: Client Needs: General 4. When listening to heart sounds, the nurse knows the valve closures that can be heard best at the base of the heart are: a. Mitral and tricuspid. b. Tricuspid and aortic. c. Aortic and pulmonic. d. Mitral and pulmonic. ANS: C The second heart sound (S2) occurs with the closure of the semilunar (aortic and pulmonic) valves and signals the end of systole. Although it is heard over all the precordium, the S2 is loudest at the base of the heart. DIF: Cognitive Level: Understanding (Comprehension) REF: p. 464 MSC: Client Needs: General 5. Which of these statements describes the closure of the valves in a normal cardiac cycle? a. The aortic valve closes slightly before the tricuspid valve. b. The pulmonic valve closes slightly before the aortic valve. c. The tricuspid valve closes slightly later than the mitral valve. d. Both the tricuspid and pulmonic valves close at the same time. ANS: C Events occur just slightly later in the right side of the heart because of the route of myocardial depolarization. As a result, two distinct components to each of the heart sounds exist, and sometimes they can be heard separately. In the first heart sound, the mitral component (M1) closes just before the tricuspid component (T1). DIF: Cognitive Level: Understanding (Comprehension) REF: p. 463 MSC: Client Needs: General 6. The component of the conduction system referred to as the pacemaker of the heart is the: a. Atrioventricular (AV) node. b. Sinoatrial (SA) node. c. Bundle of His. d. Bundle branches. ANS: B Specialized cells in the SA node near the superior vena cava initiate an electrical impulse. Because the SA node has an intrinsic rhythm, it is called the pacemaker of the heart. DIF: Cognitive Level: Remembering (Knowledge) REF: p. 464 MSC: Client Needs: General 7. The electrical stimulus of the cardiac cycle follows which sequence? a. AV node SA node bundle of His b. Bundle of His AV node SA node c. SA node AV node bundle of His bundle branches d. AV node SA node bundle of His bundle branches ANS: D Specialized cells in the SA node near the superior vena cava initiate an electrical impulse. The current flows in an orderly sequence, first across the atria to the AV node low in the atrial septum. There it is delayed slightly, allowing the atria the time to contract before the ventricles are stimulated. Then the impulse travels to the bundle of His, the right and left bundle branches, and then through the ventricles. DIF: Cognitive Level: Understanding (Comprehension) REF: p. 464 MSC: Client Needs: General 9. When assessing a newborn infant who is 5 minutes old, the nurse knows which of these statements to be true? a. The left ventricle is larger and weighs more than the right ventricle. b. The circulation of a newborn is identical to that of an adult. c. Blood can flow into the left side of the heart through an opening in the atrial septum. d. The foramen ovale closes just minutes before birth, and the ductus arteriosus closes immediately after. ANS: C First, approximately two thirds of the blood is shunted through an opening in the atrial septum, the foramen ovale, into the left side of the heart, where it is pumped out through the aorta. The foramen ovale closes within the first hour after birth because the pressure in the right side of the heart is now lower than in the left side. DIF: Cognitive Level: Applying (Application) REF: p. 467 MSC: Client Needs: Health Promotion and Maintenance 11. In assessing a 70-year-old man, the nurse finds the following: blood pressure 140/100 mm Hg; heart rate 104 beats per minute and slightly irregular; and the split S2 heart sound. Which of these findings can be explained by expected hemodynamic changes related to age? a. Increase in resting heart rate b. Increase in systolic blood pressure c. Decrease in diastolic blood pressure d. Increase in diastolic blood pressure ANS: B With aging, an increase in systolic blood pressure occurs. No significant change in diastolic pressure and no change in the resting heart rate occur with aging. Cardiac output at rest is does not changed with aging. DIF: Cognitive Level: Analyzing (Analysis) REF: p. 469 MSC: Client Needs: Health Promotion and Maintenance 15. In assessing the carotid arteries of an older patient with cardiovascular disease, the nurse would: a. Palpate the artery in the upper one third of the neck. b. Listen with the bell of the stethoscope to assess for bruits. c. Simultaneously palpate both arteries to compare amplitude. d. Instruct the patient to take slow deep breaths during auscultation. ANS: B If cardiovascular disease is suspected, then the nurse should auscultate each carotid artery for the presence of a bruit. The nurse should avoid compressing the artery, which could create an artificial bruit and compromise circulation if the carotid artery is already narrowed by atherosclerosis. Excessive pressure on the carotid sinus area high in the neck should be avoided, and excessive vagal stimulation could slow down the heart rate, especially in older adults. Palpating only one carotid artery at a time will avoid compromising arterial blood to the brain. DIF: Cognitive Level: Applying (Application) REF: p. 476 MSC: Client Needs: Safe and Effective Care Environment: Management of Care 16. During an assessment of a 68-year-old man with a recent onset of right-sided weakness, the nurse hears a blowing, swishing sound with the bell of the stethoscope over the left carotid artery. This finding would indicate: a. Valvular disorder. b. Blood flow turbulence. c. Fluid volume overload. d. Ventricular hypertrophy. ANS: B A bruit is a blowing, swishing sound indicating blood flow turbulence; normally, none is present. DIF: Cognitive Level: Analyzing (Analysis) REF: p. 476 MSC: Client Needs: Safe and Effective Care Environment: Management of Care 17. During an inspection of the precordium of an adult patient, the nurse notices the chest moving in a forceful manner along the sternal border. This finding most likely suggests a(n): a. Normal heart. b. Systolic murmur. c. Enlargement of the left ventricle. d. Enlargement of the right ventricle. ANS: D Normally, the examiner may or may not see an apical impulse; when visible, it occupies the fourth or fifth intercostal space at or inside the midclavicular line. A heave or lift is a sustained forceful thrusting of the ventricle during systole. It occurs with ventricular hypertrophy as a result of increased workload. A right ventricular heave is seen at the sternal border; a left ventricular heave is seen at the apex. DIF: Cognitive Level: Applying (Application) REF: p. 479 MSC: Client Needs: Safe and Effective Care Environment: Management of Care 18. During an assessment of a healthy adult, where would the nurse expect to palpate the apical impulse? a. Third left intercostal space at the midclavicular line b. Fourth left intercostal space at the sternal border c. Fourth left intercostal space at the anterior axillary line d. Fifth left intercostal space at the midclavicular line ANS: D The apical impulse should occupy only one intercostal space, the fourth or fifth, and it should be at or medial to the midclavicular line. DIF: Cognitive Level: Remembering (Knowledge) REF: p. 479 MSC: Client Needs: Safe and Effective Care Environment: Management of Care 19. The nurse is examining a patient who has possible cardiac enlargement. Which statement about percussion of the heart is true? a. Percussion is a useful tool for outlining the heart’s borders. b. Percussion is easier in patients who are obese. c. Studies show that percussed cardiac borders do not correlate well with the true cardiac border. d. Only expert health care providers should attempt percussion of the heart. ANS: C Numerous comparison studies have shown that the percussed cardiac border correlates only moderately with the true cardiac border. Percussion is of limited usefulness with the female breast tissue, in a person who is obese, or in a person with a muscular chest wall. Chest x-ray images or echocardiographic examinations are significantly more accurate in detecting heart enlargement. DIF: Cognitive Level: Understanding (Comprehension) REF: p. 480 MSC: Client Needs: Safe and Effective Care Environment: Management of Care 20. The nurse is preparing to auscultate for heart sounds. Which technique is correct? a. Listening to the sounds at the aortic, tricuspid, pulmonic, and mitral areas b. Listening by inching the stethoscope in a rough Z pattern, from the base of the heart across and down, then over to the apex c. Listening to the sounds only at the site where the apical pulse is felt to be the strongest d. Listening for all possible sounds at a time at each specified area ANS: B Auscultation of breath sounds should not be limited to only four locations. Sounds produced by the valves may be heard all over the precordium. The stethoscope should be inched in a rough Z pattern from the base of the heart across and down, then over to the apex; or, starting at the apex, it should be slowly worked up (see Figure 19-22). Listening selectively to one sound at a time is best. DIF: Cognitive Level: Understanding (Comprehension) REF: p. 481 MSC: Client Needs: Safe and Effective Care Environment: Management of Care 21. While counting the apical pulse on a 16-year-old patient, the nurse notices an irregular rhythm. His rate speeds up on inspiration and slows on expiration. What would be the nurse’s response? a. Talk with the patient about his intake of caffeine. b. Perform an electrocardiogram after the examination. c. No further response is needed because sinus arrhythmia can occur normally. d. Refer the patient to a cardiologist for further testing. ANS: C The rhythm should be regular, although sinus arrhythmia occurs normally in young adults and children. With sinus arrhythmia, the rhythm varies with the person’s breathing, increasing at the peak of inspiration and slowing with expiration. DIF: Cognitive Level: Analyzing (Analysis) REF: p. 481 MSC: Client Needs: Health Promotion and Maintenance 22. When listening to heart sounds, the nurse knows that the S1: a. Is louder than the S2 at the base of the heart. b. Indicates the beginning of diastole. c. Coincides with the carotid artery pulse. d. Is caused by the closure of the semilunar valves. ANS: C The S1 coincides with the carotid artery pulse, is the start of systole, and i [Show More]
Last updated: 3 years ago
Preview 1 out of 167 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$12.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Feb 19, 2021
Number of pages
167
Written in
All
Additional information
This document has been written for:
Uploaded
Feb 19, 2021
Downloads
0
Views
168