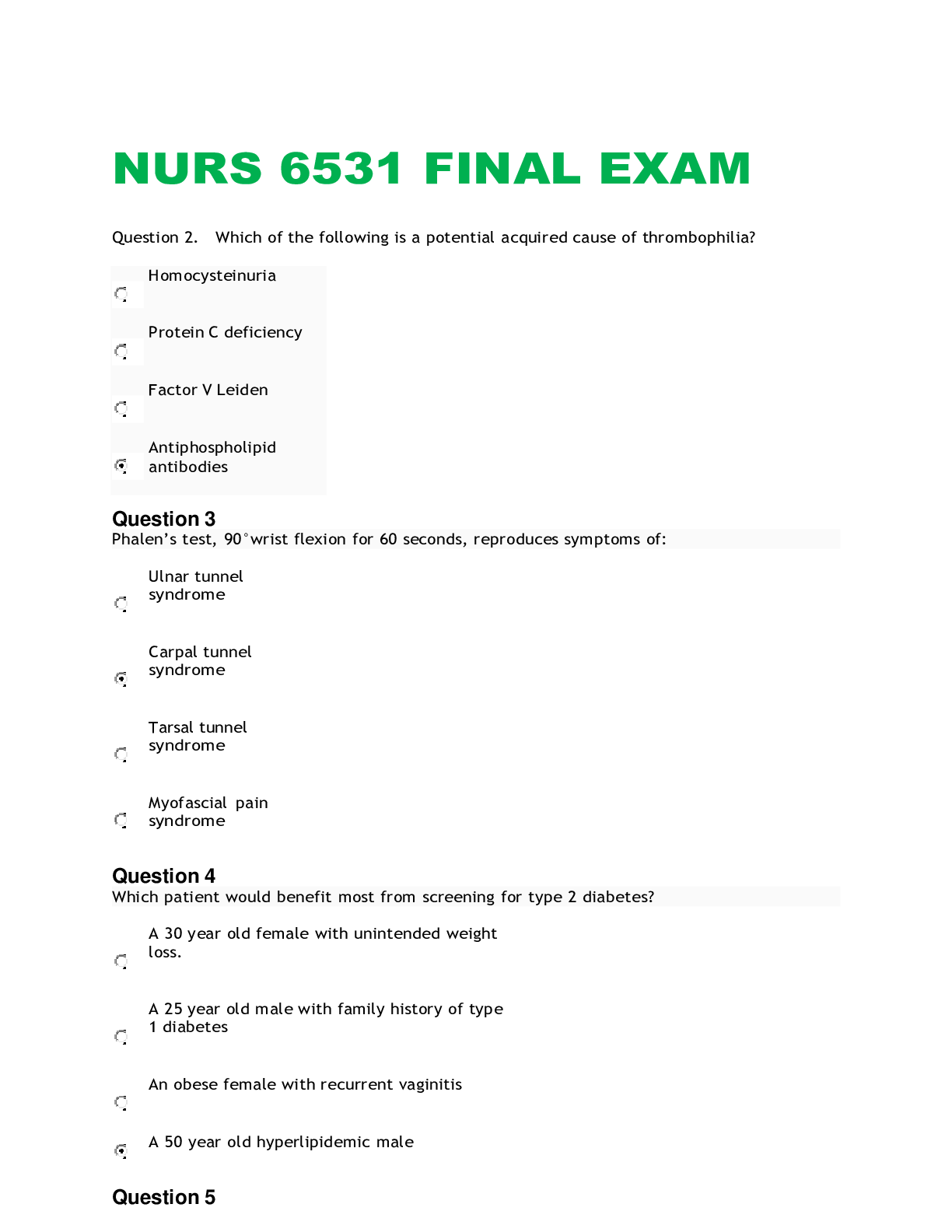
*NURSING > Final Exam Review > NUR 3029: Health Assessment Final Exam: Study Guide (All)
NUR 3029: Health Assessment Final Exam: Study Guide
Document Content and Description Below
The comprehensive examination will contain 100 multiple questions. Please refer to your course syllabus regarding examination policies, the Activities & Assignments for reading assignments, previous s... tudy guides, and class schedule. The following study guide is intended to assist you in preparing for the examination and may not be all-inclusive. Students are expected to apply concepts from pre-requisite courses. Examination preparation should include attending class lectures, reading assignments, and web-based activities. Introduction to Health Assessment • Understanding the components of the Nursing Process • Nurse’s role in environmental assessment • Communication for assessment of multiple populations (adult/elderly) • Cultural sensitivity in Health Assessment Health History • Communication during the physical examination and obtaining health history • Obtaining subjective and objective information during the health history • Components of the Health History Assessment Techniques > Parts of the stethoscope and assessment of sounds (bell vs diaphragm)- the bell is used for soft, low pitched sounds such as extra heart sounds or murmurs and diaphragm used for high-pitched sounds such as, breathe, bowel, and normal heart sounds. > Inspection, palpation, percussion, auscultation (order changes in abdominal assessment. > Appropriate sequence of assessment (infant, child, adult)- the same for each- head to toe General Survey Assessment of vital signs (normal vs abnormal, routes & locations of vital signs) 1) Temperature- > normal oral temp: 96.8 degrees F; normal range: 35.8 to 37.3 degrees C (96.4-99.1 degrees F)- most accurate and convenient > normal rectal temp: 0.4 to 0.5 degrees C higher (0.7 to 1 degree F)- only used when other routes are not practical > TMT- temperature checked by ear (used mostly in children) 2) Pulse- palpating the peripheral pulse gives the rate and rhythm of the heartbeat, as well as local data on the condition of the artery; counting for 30 seconds and multiplying by 2 is the most accurate but if rhythm is irregular, count for the full minute; assess for rate, rhythm, and force > bradycardia- rate less than 50 bpm > tachycardia- rate greater than 90 bpm > 3+ full, bounding; 2+ normal; 1+ weak, thready; 0 absent. 3) Respirations- for a neonate 30-40 breaths per min is normal; for an adult 10-20 is considered normal but 10 should be a concern. 4) Blood pressure- Can be checked in the arm or the thigh (brachial pulse, popliteal pulse) > Normal: 120/80 or less > Prehypertension: 120-139/80-89 > Stage 1 hypertension: 140-159/90-99 > Stage 2 hypertension: >160/>100 Assessment of changes in BP (orthostatic BPS and nurse’s role) > take serial measurements when you suspect volume depletion; when the person is known to have hypertension or is taking antihypertensive medication; or when the person reports fainting or syncope. > have person rest supine for 2 to three minutes and take baseline readings of pulse and BP, and then repeat the measurements with the person sitting, then standing (for person too busy to stand, assess supine and then sitting with legs dangling. Normally when the position is changed from supine to standing, there is a slight decrease (les than 10 mmHg) in systolic pressure. > orthostatic hypotension- drop in systolic pressure of more than 20 mmHg or orthostatic pulse increases in 20 bpm standing position. > nurse must record the BP for each position, the arm used, and the cuff size if different from standard adult; also record the pulse rate and rhythm. * If BP cuff is too narrow for the arm, it will result in a false high BP reading and if it is too loose or uneven it will result in a false low reading. Pain Assessment and Vital Signs interpretation >infants and children use the face pain scale >PQRSTU - Provocative/palliative - Quality - Region/Radiation - Severity, 0-10 - Time - Understands * BP tends to be higher when a person is in acute pain; in persons with chronic pain BP is not normally affected. Integumentary Assessment Normal vs abnormal changes in the skin (infant, child, adult, older adults) > test for skin turgor (tenting), which signifies dehydration- abdomen on infant, hand on an adult > newborns nail beds may be cyanotic for the first few hours of life, then turn pink. > adolescents experience acne; appear in children 7 to 8 years of age but usually peak at age 14 to 16 years in girls, and at 16 to 19 years in boys. > skin for aging adult is much thinner > acrochordons or “skin tags” occur frequently on eyelids, back, and axillae and trunk. > hair growth decreases in aging adult and the amount of decrease in axillae and pubic areas. After menopause, women develop brisk hair on chin or upper lip; in men coarse terminal hairs develop in ears nose and eyebrows but beard is unchanged; male pattern alopecia is a genetic trait (gradual receding in a symmetric W shape); in males and females, hair begins to change white due to loss of melanocyte function. > with aging the nail growth rate decreases and surface may be brittle and sometimes yellowed; toe nails are thickened- make sure it is normal and not due to peripheral vascular disease Abnormal skin and hair changes and descriptions > pallor occurs with anemia, shock, arterial insufficiency, albinism (absence of melanin), and vitiligo (destruction of melanocytes) > cyanosis in light skinned people- blue, in dark skinned- check conjuctiva, oral mucosa, and nail beds > jaundice – yellow in sclera, hard palate, mucous membranes, skin; check palms and soft palate in dark persons; light gray colored stool and dark golden urine. > skin smooth with hyperthyroidism, skin dry in hypothyroidism > in endocrine disorders cause excessive hair or hair loss > tinea capitis- brittle scalp hair, dull, and coarse > jagged nails- nervous picking habits; chronically dirty- poor self-care; clubbing of nails occurs with congenital cyanotic heart disease and pulmonary disorders (nail is > 180 degrees with a spongy nail base) > nails are thickened and rigid with arterial insufficiency > alopecia- a condition in which hair is lost from some or all areas of the body, usually from the scalp. > wheal- superficial, raised, transient, and erythematous; slightly irregular shaped due to edema; (ie. mosquito bite, allergic reaction; dermographism). > bulla- larger than 1 cm diameter; usually single chambered; superficial in epidermis; thin walled so it ruptures easily; (ie. friction burn, dermatitis, burns). > papules- solid, elevated, and circumscribed, less than 1 cm in diamete, caused by superficial thickening in the epidermis (ie. mole, wart). > nodule- solid, elevated, hard or soft, larger than 1 cm. May extend deeper into dermis than a papule. ……………………………..CONTINUED……………………………………….. [Show More]
Last updated: 2 years ago
Preview 1 out of 32 pages
.png)
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$12.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Feb 23, 2021
Number of pages
32
Written in
Additional information
This document has been written for:
Uploaded
Feb 23, 2021
Downloads
0
Views
103