*NURSING > EXAM > CSE review CRT/RRT Normal Values Exam 444 Questions with Verified Answers,100% CORRECT (All)
CSE review CRT/RRT Normal Values Exam 444 Questions with Verified Answers,100% CORRECT
Document Content and Description Below
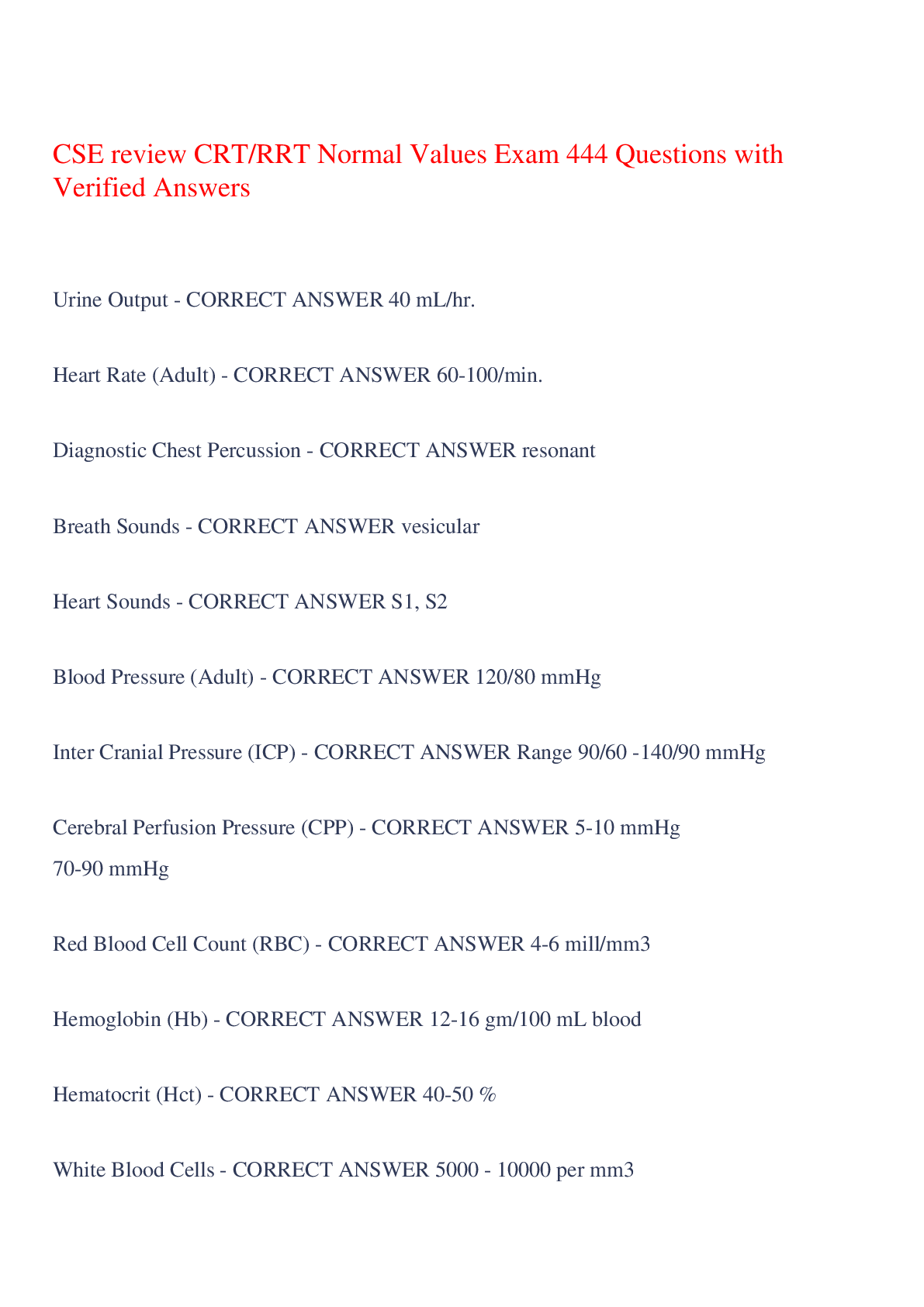
CSE review CRT/RRT Normal Values Exam 444 Questions with Verified Answers Urine Output - CORRECT ANSWER 40 mL/hr. Heart Rate (Adult) - CORRECT ANSWER 60-100/min. Diagnostic Chest Percussion ... - CORRECT ANSWER resonant Breath Sounds - CORRECT ANSWER vesicular Heart Sounds - CORRECT ANSWER S1, S2 Blood Pressure (Adult) - CORRECT ANSWER 120/80 mmHg Inter Cranial Pressure (ICP) - CORRECT ANSWER Range 90/60 -140/90 mmHg Cerebral Perfusion Pressure (CPP) - CORRECT ANSWER 5-10 mmHg 70-90 mmHg Red Blood Cell Count (RBC) - CORRECT ANSWER 4-6 mill/mm3 Hemoglobin (Hb) - CORRECT ANSWER 12-16 gm/100 mL blood Hematocrit (Hct) - CORRECT ANSWER 40-50 % White Blood Cells - CORRECT ANSWER 5000 - 10000 per mm3 Potassium (K+) - CORRECT ANSWER 4.0 mEq/L range 3.5-4.5 mEq/L Sodium (Na+) - CORRECT ANSWER 140 mEq/L range 135 -145 mEq/L Chloride (Cl- - CORRECT ANSWER 90 mEq/L range 80-100 mEq/L Bicarbonate (HCO3) - CORRECT ANSWER 24 mEq/L range 22-26 mEq/L Creatine - CORRECT ANSWER 0.7 -1.3 mg/dl Blood Urea Nitrogen (BUN) - CORRECT ANSWER 8-25 mg/dl Clotting Time - CORRECT ANSWER up to 6 minutes Platelet Count - CORRECT ANSWER 150,000 -400,000 /mm3 Activated Partial Tromboplastin Time (APPT) - CORRECT ANSWER 24-32 sec. Prothrombin Time (PT) - CORRECT ANSWER 12-15 sec. Thrombin Time - CORRECT ANSWER 7-12 sec. Term Infant - CORRECT ANSWER 38 - 42 weeks APGAR Score - CORRECT ANSWER 10-Jul Temperature - CORRECT ANSWER 36.5 0C Heart Rate - CORRECT ANSWER 110 - 160/min. Respiratory Rate - CORRECT ANSWER 30 - 60 breaths /min Blood Pressure - CORRECT ANSWER 60/40 mmHg Birth Weight (Term Infant - CORRECT ANSWER 3000 g Dubositz Score - CORRECT ANSWER 40 New Ballard Score (NBS) - CORRECT ANSWER 40 Blood Glucose (Term Infant) - CORRECT ANSWER > 30mg/dl L/S Ratio - CORRECT ANSWER 2:1 or higher capnography (ETCO2) - CORRECT ANSWER 30 torr 3-5 % pulse oximetry (SpO2) - CORRECT ANSWER 93 - 97% co-oximetry - CORRECT ANSWER 1 - 3% mean arterial pressure (MAP) - CORRECT ANSWER 93 -94 mmHg right arterial pressure - CORRECT ANSWER 2 - 6 mmHg 4 - 12 cmH2O right ventricle pressure - CORRECT ANSWER 25/0 mmHg pulmonary arteries (PAP) - CORRECT ANSWER 25/8 mmHg mean 13 - 14 mmHg pulmonary capillary pressure - CORRECT ANSWER 8-10 mmHg pulmonary capillary wedge pressure (PCWP) - CORRECT ANSWER 4-12 mmHg left atrial pressure - CORRECT ANSWER 2 - 6 mmHg left ventricle pressure - CORRECT ANSWER 120/80 mmHg cardiac output - CORRECT ANSWER 4 - 8 L/min. cardiac index - CORRECT ANSWER 2 - 4 L/min/m2 pulse pressure - CORRECT ANSWER 40 mmHg systemic vascular resistance - CORRECT ANSWER < 20 mmHg/L/min. or 1600 Dynes/sec/m-5 pulmonary vascular resistance - CORRECT ANSWER < 2.5 mmHg/L/min or 200 Dynes/sec/cm-5 Cuff Pressure - CORRECT ANSWER <= 20 mmHg Pre-Term Infant ET tubes size - CORRECT ANSWER 2.5 - 3.0 mm Term Infant ET tubes size - CORRECT ANSWER 3.0 - 3.5 mm Adult Male ET tubes size - CORRECT ANSWER 8.0 - 9.0 mm Adult Female ET tubes size - CORRECT ANSWER 7.0 - 8.0 mm Oral Intubation - CORRECT ANSWER 21 - 25 cm at lips Nasal Intubation - CORRECT ANSWER 26 - 29 cm at nares Body Humidity - CORRECT ANSWER 44 mg/L or 47 mmHg at 370C PAO2 - CORRECT ANSWER Varies directly with patient's FIO2 A-aDO2 - CORRECT ANSWER 5 - 10 mmHg on 21% O2 25 - 65 mmHg on 100% O2 CaO2 - CORRECT ANSWER 17 - 20 vol% CvO2 - CORRECT ANSWER 12 - 16 vol% C(a-v)O2 - CORRECT ANSWER 4 - 5 vol% PaO2/FIO2 - CORRECT ANSWER 380 torr or > Cardiac Output - CORRECT ANSWER 4 - 8 L/min Qs/Qt - CORRECT ANSWER 3 - 5 % SaO2 - CORRECT ANSWER 98% range 95 - 100% VD/VT Ratio - CORRECT ANSWER 20 - 40 % PCO2 - CORRECT ANSWER 40 torr Range 35 - 45 torr PaO2 - CORRECT ANSWER 97 torr Range 80 - 100 torr pH - CORRECT ANSWER 7.4 Range 7.35 -7.45 Newborn Arterial Blood Gas PaCO2 - CORRECT ANSWER < 50 torr Newborn Arterial Blood Gas PaO2 - CORRECT ANSWER >60 torr Calibration syringe - CORRECT ANSWER 3.0 liters Range 2.859 - 3.105 L (+- 3.5%) Maximum Inspiratory Pressure (MIP) - CORRECT ANSWER -80 cmH20 Maximum Expiratory Pressure (MEP) - CORRECT ANSWER + 160 cmH2O Vital Capacity (VC) - CORRECT ANSWER 80% of predicted or higher FEV1 - CORRECT ANSWER 80% of predicted or higher FEV1/FVC - CORRECT ANSWER 70% FEF 200-1200 - CORRECT ANSWER 80% of predicted or higher FEF25-75% - CORRECT ANSWER 80% of predicted or higher Peak Expiratory Flow Rate (PEFR) - CORRECT ANSWER 10 L/sec or 600L/min Airway Resistance - CORRECT ANSWER 0.6 - 2.4 cmH2O/L/sec. Compliance - CORRECT ANSWER 60 - 100 mL/cmH2O DLCO - CORRECT ANSWER 23 mL CO/min/mmHg (STPD) Tidal Volume (VT) - CORRECT ANSWER 5 - 8 mL/kg Vital Capacity (VC) - CORRECT ANSWER 65 -75 mL/kg or 10*Vt Respiratory Rate - CORRECT ANSWER 12 -20 breaths/min Minute Ventilation (VE) - CORRECT ANSWER 5 - 6 L/min Maximum Inspiratory Pressure (MIP) - CORRECT ANSWER -80 cmH2O Static Lung Compliance - CORRECT ANSWER +160 cmH2O Mean Airway Pressure (PAW) - CORRECT ANSWER 5-10 cmH2O Breathing Rate adult - CORRECT ANSWER 10 -12 bpm or every 5-6 sec Breathing Rate child - CORRECT ANSWER 12 -20 bpm or ever 2 sec Breathing Rate infant - CORRECT ANSWER 12 - 20 bpm or ever 2 sec Breathing Rate newborn - CORRECT ANSWER 40 -60 bpm Compression to Ventilation Ratio adult - CORRECT ANSWER 30:2 one and two rescuers Compression to Ventilation Ratio child - CORRECT ANSWER 30:2 one rescuer Compression to Ventilation Ratio child - CORRECT ANSWER 15:2 two rescuers Compression to Ventilation Ratio infant - CORRECT ANSWER 30:2 one rescuer Compression to Ventilation Ratio infant - CORRECT ANSWER 15:2 two rescuers Compression to Ventilation Ratio newborn - CORRECT ANSWER 3:1 one and two rescuers Vd/Vt Ventilator patients - CORRECT ANSWER Up to 60% Vd/Vt - CORRECT ANSWER 20-40% Qs/Qt Shut Normal patients - CORRECT ANSWER 3-5% Qs/Qt Shut Tolerable - CORRECT ANSWER 10-20% Qs/Qt Shut Life-threatening - CORRECT ANSWER 20-30% Parameter VT tidal volume Normal - CORRECT ANSWER 5 to 8 mL per kilogram Parameter Vt Unacceptable - CORRECT ANSWER < 5 mL/ kilogram Parameter Vital capacity Normal - CORRECT ANSWER 65-75 ML/KG Or 10 x VT Parameter Vital capacity Unacceptable - CORRECT ANSWER < 10 ML/KG Or < 2X Vt Parameter Respiratory rate Unacceptable - CORRECT ANSWER > 20 breaths Or < 8 breaths Parameter Minute ventilation Ve Normal - CORRECT ANSWER 5-6L/minute Parameter Ve Minute ventilation Unacceptable - CORRECT ANSWER > 10 L/min Parameter Maximum inspiratory pressure Unacceptable - CORRECT ANSWER < - 20 cm h2o Parameter maximum expiratory pressure Unacceptable - CORRECT ANSWER <+40cm H20 Initial ventilator parameters phase 1 What are the two most important settings - CORRECT ANSWER Title volume and rate In phase 1 ventilators where would you set the tidal volume - CORRECT ANSWER 8-12 ML per kilogram of ideal body weight In phase 1 ventilator parameters when would you set the title volume lower - CORRECT ANSWER Patients with lung disease pneumonia ARDS ALI Infant ventilator settings What mode would you use - CORRECT ANSWER IMV/SIMV Infant ventilator settings What rate would you set - CORRECT ANSWER 20-30 breaths per minute Infant ventilator settings Where would you set the peak inspiratory pressure - CORRECT ANSWER 20-30 cm of water Infant ventilator settings Where would you set the Fio2 - CORRECT ANSWER 0.40-0.60 or same FIO2 Infant ventilator settings Where would you set the Peep - CORRECT ANSWER 2-4 cm of water Increased in increments of 1 or 2 cm of water with maximum level of around 8 cm of water Infant ventilator settings Where would you set the flow - CORRECT ANSWER 5-6 L per minute Infant ventilator settings How would you set the I-time - CORRECT ANSWER 0.5-0.6 sec How do you calculate volume lost two chest tubes - CORRECT ANSWER Deliverd Vt - exhaled Vt = loss volume What is the formula to approximate F I O2 with a nasal cannula - CORRECT ANSWER 20+ (4 X liter flow) = approximate FiO2 What is the formula for the duration of flow - CORRECT ANSWER Duration (in minutes) = gage psi X tank factor/liter flow What is the tank factor for E cylinder - CORRECT ANSWER .28 What is the tank factor for h cylinder - CORRECT ANSWER 3.14 If you hear the words lethargic somnolent or sleepy what should you consider - CORRECT ANSWER COPD O2 overdose or sleep apnea If you hear the words stuporous or confused what should you consider - CORRECT ANSWER The patient is responding inappropriately, drug overdose, and detoxification Semi comatose - CORRECT ANSWER Response only to painful stimuli Obtunded - CORRECT ANSWER Drowsy state, may have decreased cough or gag reflex Dyspnea grade V - CORRECT ANSWER Dyspnea at rest, shaving, dressing, etc... When would you see venous distention - CORRECT ANSWER CHF Patients with obstructive lung disease What cheyne Stokes - CORRECT ANSWER Increased intracranial pressure, meningitis, drug overdose Paradoxical pulse/pulses paradoxes - CORRECT ANSWER Pulse/blood-pressure varies with respiration May indicate severe air trapping status asthmaticus or cardiac Tamponade What is plural friction rub associated with - CORRECT ANSWER TB, pneumonia, pulmonary infarction, cancer What is indicated for a plural friction rub - CORRECT ANSWER Steroids in antibiotics Fluffy infiltrates - CORRECT ANSWER Pulmonary Adema Butterfly/batwing pattern - CORRECT ANSWER Pulmonary edema Patchy infiltrates - CORRECT ANSWER Atelectasis Platelike infiltrates - CORRECT ANSWER Atelectasis Honeycomb pattern - CORRECT ANSWER ARDS/IRDS Diffuse bilateral radiopacity - CORRECT ANSWER ARDS/IRDS Air bronchogram - CORRECT ANSWER Pneumonia Peripheral wedge shaped infiltrate - CORRECT ANSWER Pulmonary embolus Concave superior interface border - CORRECT ANSWER Plural effusion CT scan used to diagnose - CORRECT ANSWER Bronchiectasis Is spiral CT scan used to diagnose - CORRECT ANSWER Pulmonary embolus Mucoid - CORRECT ANSWER White gray chronic bronchitis Yellow - CORRECT ANSWER Presence of white blood cells bacterial infection Green - CORRECT ANSWER Stagnant sputum gram-negative bacteria bronchiecstasis pseudomonas Dark brown - CORRECT ANSWER Old blood Anaerobic lung infection does not need oxygen Bright red - CORRECT ANSWER Hemoptysis Bleeding tumor tuberculosis What is the most reliable indicator of pulmonary maturity even with diabetes - CORRECT ANSWER PG A decrease in pet CO2 would indicate - CORRECT ANSWER A increase in ventilation Or decreased perfusion dead space disease pulmonary embolism If you have a positive test what color should the CO2 detection device change to - CORRECT ANSWER Yellow Purple is poor Troubleshooting Loss of pressure What would you suspect - CORRECT ANSWER Leak or insufficient flow Troubleshooting Excessive pressure - CORRECT ANSWER Obstruction Or Excessive flow Troubleshooting Fail to cycle into inspiration - CORRECT ANSWER Adjust sensitivity Tight seal around mouthpiece Troubleshooting Fail to cycle off - CORRECT ANSWER Leak Fenestrated trach tube open Troubleshooting Pressure does not rise normally Needle reads low or negative - CORRECT ANSWER Insufficient flow Interpretation of A-aDO2 25-65 - CORRECT ANSWER Normal value A-aDO2 66-300 - CORRECT ANSWER V/Q mismatch Patient needs oxygen give up to 60% A-aDO2 >300 - CORRECT ANSWER Shunting The patient will not respond the oxygen because oxygen is shunting away. So we need to put them on CPAP if on vent use peep PaO2/Fio2 380 or greater - CORRECT ANSWER Normal value PaO2/Fio2 <200 - CORRECT ANSWER Acute lung injury V/ Q mismatch give oxygen up to 60% PaO2/Fio2 <200 - CORRECT ANSWER ARDS SHUNT use CPAP Factors that control blood pressure What can you use to increase the heart rate and strength which will ultimately increase blood pressure - CORRECT ANSWER Digitalis Digoxin Factors that Control blood pressure What can you use to decrease the heart rate and strength to decrease blood pressure - CORRECT ANSWER Beta blockers to slow the heart down Factors that control blood pressure What can you use two cause vessel constriction to increase blood pressure - CORRECT ANSWER Give epinephrine to constrict the vessels Factors that control blood pressure What can you use two cause vessel dilation to decrease blood pressure - CORRECT ANSWER You can give the patient nitro nitric or nitrous to vasodilate What should the pulmonary artery pressure be? - CORRECT ANSWER 25/8 14 What should the pulmonary wedge pressure be? - CORRECT ANSWER 4-12 Or 8 What should the central venous pressure be? - CORRECT ANSWER 2-6 Or 4 What should the mean arterial pressure be? - CORRECT ANSWER 120/80 Or 93,94 When would you notice pressure dampening - CORRECT ANSWER You would notice this when the monitor does not show the normal dicrotic notch which means the catheter is somehow obstructed What can cause pressure dampening? - CORRECT ANSWER A blood clot or a bubble in the catheter What three things can you do if there was a blood clot or a bubble in the pulmonary artery catheter - CORRECT ANSWER Aspirate Flush the catheter with normal saline Finally rotate the catheter What are for immediate (24 hours) complications of a tracheostomy - CORRECT ANSWER Bleeding Pneumothorax Air embolism Subcutaneous emphysema What are four late complications(24-48) of a tracheostomy - CORRECT ANSWER Hemorrhage Obstruction TE fistula Infection When should you keep the cough inflated - CORRECT ANSWER If a patient is eating Or When the patient is on positive pressure ventilation If you are using a fenestrated tube and decide to plug the tube you should do what three things - CORRECT ANSWER 1 deflate the cough 2 remove the inner cannula 3 plug the tracheostomy tube What are three indications for bronchial hygiene therapy - CORRECT ANSWER 1) accumulated or retained secretions 2) ineffective cough 3) ciliary dysfunction Name 8 types of patients that should receive bronchial hygiene therapy - CORRECT ANSWER 1)Bronchiectasis 2) lung abscess 3) acute atelectasis 4) cystic fibrosis 5) COPD 6) pneumonia 7) postoperative 8) prolonged bed rest When dealing with body positions which position is the best for hypoxic patients - CORRECT ANSWER Fowler Semi-fowler Reverse Trendelenburg When dealing with body positions what 3 positions are best for obese patients - CORRECT ANSWER Fowler Semi-fowler Reverse Trendelenburg When dealing with body positions what 3 positions are best for pulmonary Edema - CORRECT ANSWER Fowler Semi-fowler Reverse Trendelenburg What is the best body position for patients with very low blood pressure - CORRECT ANSWER Transdelenburg What is the best body position to prevent aspiration - CORRECT ANSWER Lateral flat If a patient aspirates during postural drainage what should be done - CORRECT ANSWER First suction Placing opposite position for postural drainage What is the formula to determine catheter size - CORRECT ANSWER (1D size /2)*3 What would be the recommended size for patient with an 8.0 endotracheal tube 12 What are the goals of aerosol therapy - CORRECT ANSWER Relieve bronchospasm in mucosal edema Provide humidity to the respiratory tract Deliver medications Two thin secretions that are thick and tenacious Which device is the least effective when humidifying an artificial airway unless heated - CORRECT ANSWER Passover or blow by humidifier Which type of humidifier device delivers 100% body humidity - CORRECT ANSWER Wick humidifiers When using a blender with a large volume nebulizer you should set the blender at what FI O2 - CORRECT ANSWER You should set the blender at the desired fio2 When using a blender how should you set the air entrainment port A large volume nebulizer - CORRECT ANSWER You should set it at 100%(closed) because you do not want to entrain room air When would you use a SPAG device - CORRECT ANSWER Is used to treat RSV and a delivers the medication ribavirin to treat RSV not to be used with any other substances When do we want to use ultrasonic nebulizers - CORRECT ANSWER For patients with thick and tenacious secretions When using ultrasonic nebulizers how do we go about increasing the mist. Would we increase the amplitude or the frequency - CORRECT ANSWER Increase the amplitude In what sequence would you give the patient with asthma their medications - CORRECT ANSWER Adrenergics Anticholinergics Steroid How would you position the patient with ARDS - CORRECT ANSWER Prone How would you position a patient with CHF - CORRECT ANSWER Fowler How would you position a patient who was obese - CORRECT ANSWER Lateral fowlers How would you position a patient with unilateral lung disease - CORRECT ANSWER Good Lung down If a patient has a pre-op inspiratory capacity of 2600 ML's what should their postop goal be when using an incentives spirometer - CORRECT ANSWER 1300 ML's If I increase the pressure what will happen to the volume - CORRECT ANSWER Volume will increase If I decrease the flow what will happen to the volume - CORRECT ANSWER The volume will increase because I am increasing the inspiratory time If I increase the flow what will happen with the volume - CORRECT ANSWER It will decrease the volume because I am decreasing the inspiratory time What will happen to the expiratory time if I increase the rate - CORRECT ANSWER It will decrease the expiratory time If I have decreased compliance what happens to the volume - CORRECT ANSWER You will have a decreased volume If a patient has increased compliance what will happen to the volume - CORRECT ANSWER You will have a increasing volume Patients with obstructive sleep apnea will find relief with EPAP pressures of what - CORRECT ANSWER 5-10 cm of water Patients on EPAP to treat hypoxemia should be starting WITH what pressures - CORRECT ANSWER 6-8 cm of water What can you measure with a newborn capillary sample - CORRECT ANSWER PH, CO2 What should you not measure with a newborn capillary sample - CORRECT ANSWER Do not measure PO2 instead use the umbilical arterial line What are the advantages of using an umbilical arterial catheter line - CORRECT ANSWER Constant monitoring of blood pressure Arterial samples for ABG And blood replacement therapy What will happen to the displayed blood pressure if the transducer is above the catheter - CORRECT ANSWER The display pressure will be lower What will happen to the display blood pressure if the transducer is below the catheter - CORRECT ANSWER The display pressure will be higher Where should the transducer be for an accurate measurement - CORRECT ANSWER It should be level with the catheter If the patient has their AA gradient performed and received a score of 300 what would this I tell you how would you fix it - CORRECT ANSWER First it would tell me that the patient is shunting. It also tells me that the patient is not responding to oxygen because the oxygen is something away. We need to put this patient on CPAP or Pete to open of your life into PDF of your life from collapsing If a patient has their AA gradient performed and received a score of 66 - 300 what would that tell you - CORRECT ANSWER It would tell me that the patient has v/q mismatch. This also means the patient needs oxygen give the patient oxygen up to 60% What formula would you use to measure exhaled title volume - CORRECT ANSWER Minute ventilation / respirations Formula for alveolar minute ventilation - CORRECT ANSWER (Vt-Vd)*RR Formula to calculate in anatomic dead space - CORRECT ANSWER Approximately 1 mL per pound of ideal body weight 150 pounds equals 150 mL of Vd Formula for physiologic dead space - CORRECT ANSWER Paco2-Peco2/Paco2 What is the formula for dynamic compliance - CORRECT ANSWER Exhaled volume/PIP-PEEP Formula for static compliance - CORRECT ANSWER Exhaled volume/Plateau-PEEP Where would you insert the needle for thoracentesis - CORRECT ANSWER Through the seventh or eighth intercoastal space at the site of maximal dullness What color is transudate fluid - CORRECT ANSWER Is usually clear and has a light straw color The transudate fluid is also called what - CORRECT ANSWER Serous fluid transudate fluid would be associated with what - CORRECT ANSWER Congestive heart failure What color does empyema pyothorax have - CORRECT ANSWER It has been opaque appearance Empyema and pyothorax is also called what - CORRECT ANSWER Exudate fluid Infections would produce what color on a Exudate fluid - CORRECT ANSWER Yellow or milky What does Purulent Exudate fluid mean - CORRECT ANSWER Pus filled Exudate Serosanguineous is what kind of effusions and they suggest what - CORRECT ANSWER Bloody effusions and will suggest malignancy or cancer What is mucopurulent - CORRECT ANSWER Mucus and pus What is chyle - CORRECT ANSWER The lymphatic exudative fluid What does the term loculated mean - CORRECT ANSWER Very thick For a PH to be considered significant for an Exudate what would the pH have to be less then - CORRECT ANSWER 7.30 If a patient has a pneumothorax where would you place the chest tube - CORRECT ANSWER Anterior chest 2nd intercostal space in the midclavicular line If the tube is to drain the fluid from the plural space where is the tube placed - CORRECT ANSWER Fourth or fifth intercostal space in the midaxillary line. In a three bottle collection device which bottle controls the suction - CORRECT ANSWER Bottle number three How does bottle number three regulate the suction pressure - CORRECT ANSWER It is regulated by the amount of water in the bottle the more water the more suction Which bottle is considered the waterseal bottle preventing air from entering the plural cavity - CORRECT ANSWER It would be the middle bottle or bottle b What happens if there is continuous bubbling in the middle bottle - CORRECT ANSWER It should be reported as this indicates an air leak Since bottle B is the waterseal, if the water seal breaks would you do - CORRECT ANSWER Submerge the chest tube in a glass of water if the patient is receiving mechanical ventilation then leave the tube open to atmosphere air until a new system can be set up Where do you want to set the oxygen for traumatic brain injury tumors aneurysms strokes and seizures - CORRECT ANSWER 100% oxygen What kind of special test do you want to perform for traumatic brain injury tumors aneurysms strokes and seizures - CORRECT ANSWER CT, MRI, pet scans For traumatic brain injury tumors aneurysms strokes and seizures what do you want to do with me and airway pressures and PEEP and peak expiratory pressure - CORRECT ANSWER You would want to minimize Paw by utilizing low PEEP and low peak inspiratory pressures Which medications do you want to use for traumatic brain injury tumors aneurysms strokes and seizures - CORRECT ANSWER Barbiturates for sedation Mannitol to decrease ICP Dilantin for seizures If a neckbrace is in place where would you check the pulse - CORRECT ANSWER You would check the femoral pulse How would you intubate a patient who had traumatic injury or spine deformities - CORRECT ANSWER Use a flexible bronchoscope Prior to any surgeries which type of preop testing should be performed - CORRECT ANSWER Pulmonary function testing or basics Spirometry testing Hyper inflation therapy If it patient has a surgery that involves removal of the vocal chords and the larynx is also removed along with the epiglottitis in thyroid Cartlidge what should you do - CORRECT ANSWER The patient will have a permanent stoma therefore the patient will not be able to be orally or nasally intubated if mechanical ventilation is required insert a endotracheal tube into the laryngectomy opening If it patient has a surgery that involves removal of the vocal chords and the larynx is also removed along with the epiglottitis in thyroid Cartlidge what should you do. What should you do about the secretions - CORRECT ANSWER You would want to use a cool aerosol that will help keep secretions thin in the early postop. What are six causes of ARDS or acute respiratory distress syndrome - CORRECT ANSWER Aspiration Trauma Drug overdose Fluid overload Inhalation of toxins and irritants Shock What kind of cough is produced with ARDS - CORRECT ANSWER Nonproductive cough Which type of breath sounds or heard with ARDS - CORRECT ANSWER Bronchial and crackles What would you see on the chest x-ray for a patient with ARDS - CORRECT ANSWER Diffuse alveolar infiltrates with a honeycomb or groundglass appearance Radiopacity Which type of arterial blood gas will you see on a patient with ARDS - CORRECT ANSWER Refractory hypoxemia Acute alveolar hyperventilation with hypoxia Which type of pulmonary function testing results would you see with ARDS - CORRECT ANSWER Decreased volumes and capacities Tidal volume residual volume FRC and total lung capacity Which type of special tests would you want to perform on a patient with ARDS - CORRECT ANSWER Hemodynamic monitoring reveals elevated pulmonary artery pressure If you were measuring hemodynamics on a patient with ARDS what would be increased - CORRECT ANSWER Pulmonary artery pressure or PAP What is the first rule of thumb to treat ARDS - CORRECT ANSWER Treat the underlying cause With ARDS how much oxygen do you want to use - CORRECT ANSWER Up to 60% With ARDS once you 60% of oxygen what should you do next - CORRECT ANSWER Add CPAP or peep When the ARDS patient starts to improve what do you titrate first oxygen or CPAP/peep - CORRECT ANSWER Oxygen first then CPAP or peep If an ARDS patient develops atelectasis what should you do - CORRECT ANSWER Implement hyperinflation therapy such as SMI IS and IPPB Which modes of mechanical ventilation would you consider for ARDS - CORRECT ANSWER Pressure control ventilation Inverse ratio ventilation Airway pressure release ventilation Pressure regulated volume control High-frequency ventilation What is the ARDS ventilator protocol - CORRECT ANSWER Reduce tidal volume to 6ml/kg Maintain plateau pressure <30 cmH20 Recruitment maneuvers Which neurological disorder contains the neuromuscular junction that interferes with the chemical transmission of acetylcholine - CORRECT ANSWER Myasthenia Gravis For patients with neuromuscular diseases, what 3 things would you look out for in case a patient went into ventilatory failure - CORRECT ANSWER Decreased tidal volumes Decreased vital capacity Decreased maximum inspiratory pressure or MIP Which neurological disease contains drooping eyelids - CORRECT ANSWER Myasthenia Gravis Which neurological disease contains double vision or Dilopia - CORRECT ANSWER Myasthenia Gravis Which special tests do you want to run for Myasthenia Gravis - CORRECT ANSWER Edrophonium(tension Challenge test) Electromyography When looking at a Myasthenia Gravis patient. which type of arterial blood gas would you see and when would the PaCO2 have a ventilatory failure - CORRECT ANSWER Look cute ventilatory failure with hypoxemia. Watch for ventilatory failure PaCO2 > 45 If the Vt VC and MIP and weakness improve with tensilon. what does this tell you - CORRECT ANSWER This is referred to as a myasthenic crisis indicating more of this type of drug needs to be given What is the name of the drug that is given for myasthenic crisis - CORRECT ANSWER Niostigmine or prostigmine If the Vt VC and MIP and weakness worsens with tensilon. what does this tell you - CORRECT ANSWER This would be called a cholinergic crisis indicating too much of this type of drug has been given If the patient goes into cholinergic crisis which type of drug should be used to reverse tensilon - CORRECT ANSWER Atropine While trying to treat a patient with myasthenia gravis what are some things that you should do - CORRECT ANSWER Bed rest restriction Oxygen therapy for hypoxemia Hyper inflation therapy Pulmonary hygiene What are some other treatment modalities for myasthenia gravis which would include drugs and other special procedures - CORRECT ANSWER Corticosteroids in severe cases Adrenocoeticotropic hormone Thymectomy Plasmapheresis Which neuromuscular disease contains the peripheral nervous system - CORRECT ANSWER Guillain barre Which neurological disease frequently occurs after a febrile illness 1-4 weeks - CORRECT ANSWER Guillain barre What is the precise cause of Guillain barre - CORRECT ANSWER The precise causes is unknown What special test would you do for a patient with Guillain barre - CORRECT ANSWER A lumbar puncture- high protein level in CSF, abnormal electromyograph What are some treatment options for a patient with Guillain barre - CORRECT ANSWER Oxygen therapy Hyperinflation therapy Pulmonary hygiene Anticoagulant therapy Physical therapy Corticosteroids In severe cases only what are some treatment options for Guillain barre - CORRECT ANSWER Plasmapheresis For a stroke patient will kind of picture do you want to take of the brain - CORRECT ANSWER A CT scan or MRI How will that intracranial pressure look with a patient with a stroke - CORRECT ANSWER Increased What is the treatment therapy for a stroke patient within six hours of symptom onset drug therapy - CORRECT ANSWER Anticoagulation therapy Vasodilaters Thrombolytic therapy for acute machine stroke When would you use mechanical ventilation for a stroke patient - CORRECT ANSWER 1 for ventilatory failure 2 reduce intracranial pressure What kind of electrolytes will you see with a patient with myocardial infarction - CORRECT ANSWER Hyperkalemia Or Hypokalemia What kind of special tests would you perform on a patient with a myocardial infarction. I am not talking about scans. - CORRECT ANSWER Cardiac enzymes CPK, LVH, SGOT and also troponin How will the electrocardiogram look with a patient that has a myocardial infarction - CORRECT ANSWER Arrhythmias with significant Q waves in ST segment changes How much oxygen are you going to give the patient with a myocardial infarction - CORRECT ANSWER 100% What is the drug therapy for a myocardial infarction - CORRECT ANSWER Atropine for bradycardia Defibrillate for pulseless ventricular tachycardia or fibrillation Nitrates for chest pain Aspirin anti rhythmic agents What do you do for a patient that has pulseless ventricular tachycardia - CORRECT ANSWER Defibrillated How much oxygen do you give to a patient with CHF or pulmonary Edema - CORRECT ANSWER 100% oxygen Besides drug therapy what other decision-making protocols will you decide to use for CHF or pulmonary EDema - CORRECT ANSWER Oxygen at 100% Closely monitor vital signs in place the patient in fowlers IPPB with 100% oxygen Which type of drugs will you use for CHF or pulmonary edema - CORRECT ANSWER Diuretics such as Lasix Positive inotropic agents such as: digitalis digoxin dopamine and low-dose amiodarone Name some positive inotropic drugs - CORRECT ANSWER digitalis digoxin dopamine Which type of electrolyte replacements will be added to the IV bag for CHF patient or pulmonary E Dema - CORRECT ANSWER Potassium and sodium What will you do for ventricular fibrillation and pulseless ventricular tachycardia - CORRECT ANSWER Defibrillate at 360 jewels What will you do for atrial flutter fibrillation and ventricular tachycardia with a pulse that are not life-threatening - CORRECT ANSWER Perform synchronized cardioversion starting at 50 to 100 jewels A patient that is in shock what will the drug therapy include - CORRECT ANSWER Vasopressors for vasogenic hypovolemia Positive inotropic drugs such as digitalis digoxin for heart failure Antibiotics for infection At what age will a child most likely get croup - CORRECT ANSWER Six months to six years Which child infection supports a viral infection that can cause an obstruction in the airway - CORRECT ANSWER Croup For croup what will you do for mild cases - CORRECT ANSWER Temperature control cool the environment Adequate hydration and humidification of inspired air How much oxygen will you give to a patient with croup during a mild case - CORRECT ANSWER 30 to 40% oxygen How will you apply cool aerosol mist to a patient with croup - CORRECT ANSWER Facemask or tent The patient has croup what will the drug therapy include during mild cases - CORRECT ANSWER Racemic epinephrine Corticosteroids but only for patients who do not respond to cool aerosol in racemic epinephrine therapy When would you use corticosteroids for a patient that is having a mild case of croup - CORRECT ANSWER only for patients who do not respond to cool aerosol in racemic epinephrine therapy How will you know a child is having a severe case of croup - CORRECT ANSWER The child will have severe respiratory distress and or marked inspiratory stridor What is the criteria for intubation for a child with a severe case of croup - CORRECT ANSWER The patient would appear extremely lethargic Severe stridor or at rest Diminished breath sounds Extreme accessory muscle usage What six things will you do for a child that is having a severe case of croup. No drug therapy - CORRECT ANSWER Temperature control cool environment Adequate hydration in humidification of inspired air Transfer patient to the ICU sedate if necessary Place on TPiece CPAP For a child that has croup what is the criteria for extubation - CORRECT ANSWER Child's condition is stable Air leak around the tube which means swelling has gone down What childhood condition has a sudden onset within 6 to 8 hours - CORRECT ANSWER Epiglottitis What kind of retractions will you see any patient with epiglottitis - CORRECT ANSWER Sub sternal and intercoastal retractions What is the typical age of the child with epiglottitis - CORRECT ANSWER 2-6 years of age With a child with epiglottitis have a fever - CORRECT ANSWER Yes How will you measure a child's fever - CORRECT ANSWER Axillary or tympanic to avoid stimulating the child you do not want to increase their heart rate blood pressure or cardiac output How will the CBC appear on a child with epiglottitis - CORRECT ANSWER Increased white blood cells In your decision-making for a child with epiglottitis what will be the first thing you would want to do - CORRECT ANSWER Endotracheal tube Or perform a tracheostomy if unable to intubate Transfer patient to the ICU Today if necessary Place on TPiece or CPAP What drug therapy will be used for a patient with epiglottitis - CORRECT ANSWER AntiBiotics For a pediatric poisoning what kinds of decisions will you make to support care - CORRECT ANSWER Maintain an airway intubate when aspiration is possible Monitoring Full resuscitation Venous access for drug administration Appropriate weight measurement Toxicology screen Once a child has been stabilized who has pediatric poisoning what are the treatment goals - CORRECT ANSWER Prohibit further drug absorption Improve elimination of those drugs Manage complications What would you do to decontaminate the gastrointestinal tract - CORRECT ANSWER What did minister activated charcoal. However this cannot be used to absorb alcohols hydrocarbons organic solvents What is the anecdote for acetaminophen - CORRECT ANSWER Acetylcysteine What is the anecdote for narcotics - CORRECT ANSWER Narcan The patient that has cystic fibrosis how many times per day will you perform air clearance - CORRECT ANSWER Four times per day What types of things will you do for excessive secretions in a patient with cystic fibrosis - CORRECT ANSWER Chest percussion and postural drainage High-frequency chest wall compression Would you recommend exercise for a patient with cystic fibrosis - CORRECT ANSWER Yes For cystic fibrosis name three types of forced expiration techniques - CORRECT ANSWER Active cycle of breathing Autogenic drainage Huff coughing When making decisions on a patient with cystic fibrosis what will the aerosol drug therapy include - CORRECT ANSWER Bronchodilator therapy Mucolytic's such as pulmozyme Anti-inflammatory such as Advair Flovent and Pulmicort Which type of mucolytic will you use for a patient with cystic fibrosis - CORRECT ANSWER pulmozyme Which type of anti-inflammatories will you use for a patient with cystic fibrosis - CORRECT ANSWER Advair Flovent and Pulmicort And hydrating a patient with cystic fibrosis in which type of saline would you use - CORRECT ANSWER Hypertonic When treating a patient with cystic fibrosis which type of inhaled antibiotics would you prefer - CORRECT ANSWER Tobramycin What virus is connected to bronchiolitis - CORRECT ANSWER RSV Respiratory syncytial virus What age is RSV or bronchiolitis usually acquired - CORRECT ANSWER 1 in 10 infants younger than two years of age Is there any discharge with bronchiolitis if there is where would you see it - CORRECT ANSWER Nasal How was a diagnosis of RSV determined - CORRECT ANSWER The virus is determined by its antigens in the patient's oropharyngeal or nasopharyngeal secretions with bronchiolitis which infants are recommended for prophylaxis - CORRECT ANSWER -Less than two years of age who require therapy for chronic lung disease -less then 32 weeks gestation -infants with congenital heart disease with cardiovascular compromise I need to know the drug therapy for Bronchiolitis. Drug therapy -what is the antibodies against RSV Intravenous and intramuscular - CORRECT ANSWER Intravenous respigam Intramuscular-synagis Bronchiolitis most severe cases are For patients with apne, treated at the hospital, director at relieving the airway obstruction and hypoxia by utilizing what - CORRECT ANSWER Systemic hydration Oxygen therapy Airway clearance Ribavirin aerosol For bronchiolitis when would you use mechanical ventilation - CORRECT ANSWER Impending acute vent failure For bronchiolitis what is important to know about the mechanical ventilation in regards to the respiratory rate and expiratory time - CORRECT ANSWER Low respiratory rates and long expiratory times What would the action be based on this Apgar score 0-3 - CORRECT ANSWER Resuscitatr, CPR What would the action be based on this Apgar score 4-6 - CORRECT ANSWER Support Stimulate, warm, administer oxygen, assist ventilation What would the action be based on this Apgar score 7-10 - CORRECT ANSWER Routine care What kind of special test would you do want a patient with apnea of prematurity - CORRECT ANSWER Polysomnogram How will the vital signs look when treating a patient with apnea of prematurity - CORRECT ANSWER You will see periods s of bradycardia, variations in thermal regulation when treating a patient with apnea of prematurity what are some risk factors - CORRECT ANSWER Prone positioning Maternal smoking Bottlefeeding when treating a patient with apnea of prematurity how would you treat and manage these newborns - CORRECT ANSWER Oxygen therapy 30 to 50% as indicated by oximetry -Methylxanthine -Teach family CPR -Send infant home with them at the monitor Infants or newborns with meconium aspiration syndrome does it occur in full-term or postterm infants or pre-term - CORRECT ANSWER Full-term in postterm infants How will the appearance of the chest look with meconium aspiration syndrome - CORRECT ANSWER Sub sternal retractions abdominal distention see saw movement Patients with meconium aspiration syndrome what type of breath sounds were you hear - CORRECT ANSWER Wheezes, rhonchi, crackles, expiratory grunting How will the chest x-ray appear on a new born with meconium - CORRECT ANSWER Atelectasis consolidation What is the first thing you should do for an infant with meconium - CORRECT ANSWER Suction the nasopharynx and the oropharynx thoroughly when amniotic fluid is stained A patient that has meconium aspiration syndrome what would you do if the infant is: vigorous, active and crying. (Pulse > 100, strong RR and a good muscle tone)? - CORRECT ANSWER -suction mouth and nose to clear pharynx -warm dry and observe the infant -apply blow by oxygen as needed A patient that has meconium aspiration syndrome, what would you do if the infant is not vigorous (pulse<100, limp, depressed, poor tone, absent or gasping respirations) are you going to use positive pressure ventilation? - CORRECT ANSWER No A patient that has meconium aspiration syndrome, what would you do if the infant is not vigorous (pulse<100, limp, depressed, poor tone, absent or gasping respirations). What are you going to visualize - CORRECT ANSWER Vocal chords with the laryngoscope A patient that has meconium aspiration syndrome, what would you do if the infant is not vigorous (pulse<100, limp, depressed, poor tone, absent or gasping respirations). What would you do if you see meconium in the airway? - CORRECT ANSWER Intubate with the meconium aspirator and suctioned trachea A patient that has meconium aspiration syndrome, what would you do if the infant is not vigorous (pulse<100, limp, depressed, poor tone, absent or gasping respirations). How many times will you intubate with the meconium aspirator suction the trachea? - CORRECT ANSWER Repeat until airways clear even if pulses low A patient that has meconium aspiration syndrome, what would you do if the infant is not vigorous (pulse<100, limp, depressed, poor tone, absent or gasping respirations). After you have finished intubating with the meconium aspiration suctioning the trachea what's a last thing you will do? - CORRECT ANSWER Intubate provide airway A patient that has meconium aspiration syndrome, what would you do if the infant is not vigorous (pulse<100, limp, depressed, poor tone, absent or gasping respirations). List the five things that you are going to do in order!!! - CORRECT ANSWER -No positive pressure ventilation because you will send the meconium aspirate further down the airways -visualize vocal chords with the laryngoscope -intubate with the meconium aspirator suctioned trachea -repeat until airway is clear - even if pulses low -intubate provide airway Once you stabilize infant with meconium aspiration syndrome and transfer to the ICU which steps will you take to keep the infant healthy? (4) - CORRECT ANSWER -vigorous pulmonary hygiene(postural drainage percussion and suctioning) -oxygen therapy -mechanical ventilation for ventilatory failure -drug therapy(steroids,antibiotics) When you have a congenital heart defect, how does a right to left shunt present? - CORRECT ANSWER Cyanotic (hypoxemia) If you have a congenital heart defect how does a left to right shunt present? - CORRECT ANSWER Acyanotic (pulmonary congestion) With congenital heart defects what are the two causes of right to left shunts? - CORRECT ANSWER Tetralogy of Fallot Transposition of the great vessels What are the three causes of left to right shunts - CORRECT ANSWER -atrial septal defect -ventricular septal defect -Patent ductus arteriosus With congenital heart defects what will you here on the breath sounds? - CORRECT ANSWER Heart murmur What is the physical appearance of an infant with congenital heart defect - CORRECT ANSWER Respiratory distress With congenital heart defects which newborn has an egg shaped heart - CORRECT ANSWER Transposition of the great vessels With congenital heart defects which newborn will have a boot shaped heart - CORRECT ANSWER Tetralogy of fallot What is the most important diagnostic test to identify cardiac defects - CORRECT ANSWER Echocardiogram With congenital heart defects, where would you maintain the oxygen level? - CORRECT ANSWER Maintain the PaO2 levels between 60-80 torr For congenital heart defects do you want to use mechanical ventilation - CORRECT ANSWER Yes if the new born has ventilatory failure What is the cause of infant respiratory distress syndrome IRDS - CORRECT ANSWER Insufficient amount of pulmonary surfactant or depressed surfactant activity that leads to massive atelectasis in hypoxemia What is the gestational age for a newborn that has IRDS - CORRECT ANSWER Less than 38 weeks For a newborn that has IRDS how will The LS ratio appear - CORRECT ANSWER <2:1 newborn that has IRDS what will you see on the appearance of the chest? - CORRECT ANSWER Intercoastal retractions How will the respiratory pattern appear for a newborn that has IRDS - CORRECT ANSWER Tachypnea and possible apnea What will you hear for the breath sounds for a newborn that has IRDS - CORRECT ANSWER Bronchial or harsh, fine crackles/rales, expiratory grunting Physical appearance for a newborn that has IRDS - CORRECT ANSWER -Nasal flaring -grunting -retractions How will the vital signs appear for a newborn that has IRDS - CORRECT ANSWER -Increased heart rate -Increased blood pressure -Increased cardiac output How will the chest x-ray appear on a newborn that has IRDS - CORRECT ANSWER -Increased opacity -Groundglass appearance -Air bronchograms How will you correct hypoxemia for a newborn that has IRDS - CORRECT ANSWER -Oxygen with oxyhood or nasal cannula -CPAP (4-6) -Maintain PaO2 between 60-80 torr For a newborn that has IRDS what kind of environment do you want to keep them in - CORRECT ANSWER Maintain a neutral thermal environment For a newborn that has IRDS when should you administer surfactant - CORRECT ANSWER -Immediately after birth (prophylactic) in neonates 35 weeks gestation age -Or once IRDS has been diagnosed (rescue) Name four types of surfactant - CORRECT ANSWER Survanta Infasurf Curosurf Pulmactant How will you administer surfactant in a newborn that has IRDS - CORRECT ANSWER Instilled directly into the trachea through a 5 Fr. catheter placed into the endotracheal tube The solution of surfactant is administered in how many portions? - CORRECT ANSWER 4 One at a time While administering surfactant when is the catheter removed - CORRECT ANSWER After each administration During each administration of surfactant what is performed in a newborn that has IRDS - CORRECT ANSWER Infant or newborn is manually ventilated for 30 seconds After the surfactant therapy is given for anewborn that has IRDS what will you be observing for as far as adverse reactions - CORRECT ANSWER -Barotrauma -Apnea -bradycardia For a newborn that has IRDS how will you increase distribution of surfactant in the lungs - CORRECT ANSWER Change patient position to increase distribution of surfactant in the lungs What kind of mechanical ventilation will you use for a newborn that has IRDS - CORRECT ANSWER Time cycled pressure limited ventilation with Peep for ventilatory failure What is bronchopulmonary dysplasia - CORRECT ANSWER A chronic lung disease that develops in newborns as a consequence of treatment of IR DS with oxygen and positive pressure ventilation List for common factors of bronchopulmonary dysplasia - CORRECT ANSWER -Low gestational age and low birth weight -mechanical ventilation with high airway pressure -hi oxygen concentrations -history of IRDS what is the appearance of the chest for bronchopulmonary dysplasia - CORRECT ANSWER Intercoastal retractions What is the respiratory pattern for bronchopulmonary dysplasia - CORRECT ANSWER Increased > 60/ minute What type of breath sounds will you here with bronchopulmonary dysplasia - CORRECT ANSWER -Wheezes -Rhonchi -Crackles --Expiratory grunting What will the physical appearance be for bronchopulmonary dysplasia - CORRECT ANSWER -Nasal flaring -Substernal retractions/abdominal distention (seesaw movement) Does a premature infant who has bronchopulmonary dysplasia improve with mechanical ventilation - CORRECT ANSWER No Do bronchopulmonary dysplasia patients have a continued need for high oxygen concentrations? - CORRECT ANSWER Yes How will the chest x-Ray appear on bronchopulmonary dysplasia patient - CORRECT ANSWER -Groundglass pattern -Air broncograms -Small lung volumes --Cardiomegaly and pleural effusion may be present Name 14 treatments for bronchopulmonary dysplasia - CORRECT ANSWER -Drug therapy bronchodilators -Avoid endotracheal CPAP because of the increased airway resistance -M V for vent failure -Pulmonary hygiene -Surgical ligation of PDA -Extubation can be done at ventilator rates between 5 & 15 breaths / min -Monitor fluid balance -Supportive care to relieve symptoms of respiratory distress in heart failure -Hyperinflation therapy -Maintain PaO2 55-70 CO2 45-60 pH 725 -740 -minimize mean airway pressure -Ventilation in oxygenation should be maintained at lowest possible level -Oxygen therapy -Weaning from mechanical ventilation should be a slow gradual process that involves high concentrations of oxygen for prolonged periods of time after extubation infants may go home with oxygen therapy When does transient tachypnea of the newborn occur - CORRECT ANSWER 24-48 hours after birth What symptoms does transient tachypnea have similarities with - CORRECT ANSWER It has similar symptoms to the early stages of IRDS Why is When does transient tachypnea thought to be caused? - CORRECT ANSWER Believed to be caused by slow absorption of fetal lung fluid transient tachypnea is commonly seen in which type of infants - CORRECT ANSWER Near-term or full-term infants of normal size and gestational age With transient tachypnea what happens with the Apgar scores - CORRECT ANSWER At birth the infant shows good Apgar scores and then develops respiratory distress in the next 12 hours How is the cough in transient tachypnea - CORRECT ANSWER Depressed effort, excessive secretions and mucus What is the appearance of the chest for transient tachypnea - CORRECT ANSWER Intercoastal retractions, nasal flaring What is the respiratory pattern for transient tachypnea - CORRECT ANSWER Increased rate > than 60 What type of breath sounds will you hear in transient Tachypnea pts - CORRECT ANSWER -Wheezes -Rhonchi -Crackles -Respiratory grunting Describe what you will see on a chest x-ray for transient tachypnea - CORRECT ANSWER -Initially appears normal -Pulmonary congestion develops 12 hours after birth -Patchy infiltrates -Cardiomegaly -pleural effusion maybe present What is the treatment and management for transient tachypnea Cops mu - CORRECT ANSWER -CPAP to offset pulmonary congestion in interested she will edema -Oxygen therapy for hypoxemia -Pulmonary hygiene -Supportive care to relieve signs of respiratory distress -Mechanical ventilation for vent failure which is rare Usually self-limiting. anatomical alterations in the lungs usually begin to resolve in about 24-48 hours after birth What type of pulmonary hygiene do you want to perform on transient tachypnea - CORRECT ANSWER -Suctioning -Increased bronchial hydration -Postural drainage and percussion For Congenital diaphragmatic hernia, are the newborns typically mature or immature - CORRECT ANSWER Mature Congenital diaphragmatic hernia. Is it more common in nale or female - CORRECT ANSWER Males Congenital diaphragmatic hernia appearance of the chest - CORRECT ANSWER -Intercoastal and substernal retractions -Nasal flaring -Expiratory grunting Congenital diaphragmatic hernia Respiratory pattern - CORRECT ANSWER > 60/min Congenital diaphragmatic hernia Breath sounds - CORRECT ANSWER Absent on affected side -bowel sounds on the affected side Congenital diaphragmatic hernia Physical appearance - CORRECT ANSWER -Scaphoid abdomen -Barrel chest Congenital diaphragmatic hernia Chest x-ray - CORRECT ANSWER -Atelectasis and complete lung collapse -Shift of the heart and mediastinum toward unaffected side -Hypo-plastic left lung -Fluid and air filled loops of intestine in the chest Congenital diaphragmatic hernia Treatment and medical decision-making Aid pimp - CORRECT ANSWER -Always an emergency -Immediate oxygen therapy -Do not ventilate with mask -Prompt surgical repair is crucial -Insert orogastric tube to decrease gas in the bowel -May require intubation and mechanical ventilation -Please infant on -affected side Congenital diaphragmatic hernia Where do you want to keep the pressures for mechanical ventilation - CORRECT ANSWER Use Low Peak inspiratory pressures < 30 Do you want a high-frequency or low-frequency ventilation for Congenital diaphragmatic hernia - CORRECT ANSWER Hi Congenital diaphragmatic hernia Severe cases - CORRECT ANSWER Ecmo What is the temperature of Accidental hypothermia - CORRECT ANSWER Below 35°C in below 95°F How are the vital signs in a Accidental hypothermia patient - CORRECT ANSWER Decreased heart rate respiratory rate cardiac output temperature -Peripheral vasoconstriction Accidental hypothermia Arterial blood gas - CORRECT ANSWER Moderate to severe acidosis with hypoxemia Accidental hypothermia Treatment mild cases - CORRECT ANSWER Passive rewarming may be sufficient -warm, dry clothes -warm drinks -isometric exercises to increased heat production Accidental hypothermia Treatment moderate Core temperature >30°C - CORRECT ANSWER Active rewarming may be required -warm water bath -warm blankets -heating pads -warm oral fluids with patient is alert Accidental hypothermia Severe cases <30°C - CORRECT ANSWER Active rewarming required Administration of: -warm intravenous solutions -warm gastric lavage or peritoneal lavage -inhalation of warm gases Accidental hypothermia Re-warming should proceed no faster then - CORRECT ANSWER A few degrees per hour to avoid complications [Show More]
Last updated: 2 years ago
Preview 1 out of 48 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$9.50
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Nov 23, 2023
Number of pages
48
Written in
All
Additional information
This document has been written for:
Uploaded
Nov 23, 2023
Downloads
0
Views
118