PEDS HESI Growth and Development,100% CORRECT
Document Content and Description Below
PEDS HESI Growth and Development
- Client safety is the hallmark of nursing. The fundamental components of nursing practice include nursing process integrated w/ caring, communication, and spirituality, teaching, and le
...
PEDS HESI Growth and Development
- Client safety is the hallmark of nursing. The fundamental components of nursing practice include nursing process integrated w/ caring, communication, and spirituality, teaching, and learning aswell as documentation of the integration of each of these elements
- Erikson (Psychosocial) – TM,AS,IG,II,IRC,II -TMASIGIIIRCII
o Trust vs mistrust (birth-1 year)
Having parents hold their child while in the hospital is an excellent means of building the trust relationship
o Autonomy vs shame and doubt (1-3 year)
o Initiative vs guilt (3-6 year)
o Industry vs inferiority (6-12 year)
Academic performance sense of industry = completing hw, staying on track w/ classmates
o Identity vs role confusion (12-18)
o Intimacy vs isolation (18+)
- Piaget (cognitive) - SPCF
o Sensorimotor period (birth-2 year)
o Preoperational thought (2-4 year)
o Concrete operation (7-11 year)
o Formal operation (11-15 year)
- Kohlberg (moral) NE,PO,IH&CR, GBGG &LO, SC & PP & UP)
o Infancy - Naiveté and egocentricism
o Toddler - Punish-obedience orientation
o Early childhood - Instrumental hedonism and concrete reciprocity
o Middle - childhood Good boy or good girl orientation, Law and order orientation
o Adolescence - Social contract orientation, Personal principle orientation, Universal principle orientation
- Denver developmental test
o Evaluates children from 1mo-6 years: gross motor skills, fine motor skills, language development, and personal/social development
- Infant (birth 1 year)
o Birth weight DOUBLES by 6 months, TRIPLES, by 12 months (if baby was born 9lbs, by 6 months, they would be 12lbs and by 1 y/o they would be 18lbs)
Newborns can lose up to 10% of their weight w/o concern, but should regain their birth weight by 2 weeks of age
o Newborn vaccine: Hep B birth-2 months (usually given prior to discharge)
o Birth length INCREASES by 50%/doubles by 12 months
o Posterior fontanel closes in 2-3 months, anterior fontanel closes in 12-18 months
o Heart rate: 110-160 (birth-1mo)
o Anticipatory guidance
Separation anxiety (begins around 6 months to 30 months): if parents are not able to be w/ the infant (ex: hospitalization), baby may be inconsolable
Aspiration is a common cause if injury/death at this age – often find small things on the floor and put them in their mouths (older siblings often responsible for leaving around small objects)
o Nutrition
Infants should be started on vegetables prior to fruits. The sweetness of fruits may inhibit infants from taking vegetables
Full term infants have iron stores that last approx. 4-6 months
Premature infants have iron stores form the mother that last approx. 2 months, so it is important to introduce an iron supplement by 2 months of age
o Hospitalization/nursing implications
Emerging skills may disappear
Plan & encourage to have parents as part of infant’s care
• Infants are more secure when in proximity to the parents – the parent’s lap = excellent place to assess the child
Prep and teach family, but speak & console infant (esp. during pain/stress)
Toys: mobiles, rattles, squeaking toys, picture books, balls, colored blocks, and activity boxes (ex: musical rattle infants have short attention span and enjoy auditory/visual stimulation
The nurse should not deliver more than 1mL/injection to a 6mo old
Medications should never be mixed in a large amount of food/formula b/c you can’t be sure child will take the entire feeding
Formula decreases the absorption of iron
- Knowledge of normal growth and development Is used to evaluate interventions and therapy
o Ex: what behavior would indicate that thyroid hormone therapy for a 4 month old is effective? (what milestones are accomplished at 4 months?)
o Head control – milestone is met? indicates replacement therapy is adequate for growth
- Toddler (1-3 years)
o Birth weight QUADRUPLES by 30 months, achieves 50% of adult height by 2 y/o
o Varicella vaccine
o Anticipatory guidance
Engage in parallel play play alongside child, but rarely engage in activities w/ the other child
Freud/Erickson toilet training is the essential event that must be mastered by the toddler
Very egocentric, do not consider needs of others (children)
o Hospitalization/Nursing implications
Simple explanations right before procedures (1 y/o vs 3 y/o explanations differ)
Enforced separation from parents (hospitalization) = greatest threat to toddler’s physiological/emotional integrity (teach parents to tell child they’ll be back!)
Common stressors of the hospitalized toddler
• Interrupted routine, sleep pattern disturbances, fear of being hurt
Very important to maintain a child’s home routine when parents are present and when not – increase child’s sense of security and decrease anxiety
Provide security objects/favorite toys from home
Respect & implement routine as much as possible
REGRESSION (aka bedwetting)
Toys: board and mallet, push-pull, toy phones, stuffed animals, storybooks w/pictures – playroom if able (mobility is important to development)
Very basic explanations
Toddlers learning to name body parts/concerned about their bodies
Autonomy: provide guided choices when appropriate, allow to participate in actions of which they are capable
- Preschool (3-6 years)
o Gains 5lbs/year and grows 2.5 to 3 inches
o Posture: erect, more slender
o Vision: 22/20
o Respirations: 20-30bpm
o Runs, jumps, skips, hops, establishes handedness, and learns colors and shapes.
o 3 y/o: tricycle
o Falls: common injury
o 4 y/o: use scissors also has aggressiveness
o 5 y/o: ties shoelaces aggressiveness becomes independence)
o Learns sexual identity (curiosity, masturbation – common)
o Imaginary playmates and fears = common
o Literal thinkers (ex: child’s parents say Grandpa is in heaven, so she will think they are in heaven when they are at his funeral)
o Implications/hospitalization
Emphasize understanding of child’s egocentricity
• Believe abuse/illness is their fault and should be reminded they are not bad people
Explain they did not cause illness and pain/procedures are not punishment
Answer child’s questions at child’s level (simple words they understand)
• What is/what is not going to be “fixed”
• Concrete/Simple explanations/basic pictures = helpful
• Understand time in relation to events (ex: nap time)
• Let child handle equipment/models of the equipment
Therapeutic play/medical play helpful for child to act out their experiences
• Enjoy games, good way to elicit their assistance/cooperation during a procedure
Fear of mutilation = common
• Bandaid – helpful in restoring body integrity
• Common response is to cry/protest during an immunization
Toys: coloring books, puzzles, cutting and pasting, dolls, building blocks, clay and toys that allow the preschooler to workout hospitalization procedures
- Use facts and principles related to growth and development in planning teaching interventions
o Ex: what task could a 5 y/o w/ diabetes expect to accomplish by him or herself?
o Let the child choose injection site, gives them a sense of control
- Knowledge of normal growth and developmental milestones are important in the delivery and care of an infant. If there appears to be a discrepancy in the infant’s development, it’ll warrant HCP to further investigate possible cause of delay
- School-age (6-12 y/o)
o Normal for girls to grow taller/gain more weight at this time
o 9/10 years: girls prefer to have friends of the same gender
o Hospitalizations/implications
May need more support from parents than the child wishes to admit
Maintaining contact w/ peers & school activities is important
Explanation of procedures is important
• Verbal explanations, pictures, books, and handling equipment
• Often children will include more detail about their feelings in drawings/express in pictures their feelings
• Understand basic functions of the body
• Understand if explained in basic terms
Privacy and modesty = important and should be respected during hospitalization
• Close curtains during procedures, allow privacy during baths
Participation in care and planning w/ staff sense of involvement and accomplishment
Toys: board games, card games, hobbies (stamp collecting, puzzles, and video games)
- School-age are in Erikson’s stage of industry meaning they like to do and accomplish things. Peers are also becoming important for children of this age
- Tanner Stages of Pubertal Development
o Girls: breast changes, rapid increase in height and weight, growth of pubic hear, appearance of axillary hair, menstruation, abrupt deceleration of linear growth
o Boys: enlargement of testicles, growth of pubic hair, axillary hair, facial hair and body hair, rapid increase in height, changes in larynx and voice, nocturnal emissions, abrupt deceleration of linear growth
- Adolescent
- Girls’ growth spurt (9.5 y/o) before boys, but boys catch up at 14 and continue to grow
- Girls finish growth spurt around 15, boys around 17
- Secondary sex characteristics develop
- 15 y/o: adult light thinking = problem solve and use abstract thinking
- Family conflicts develop
- Erikson’s theory: developing sense of identity (vs role confusion)
- Nursing implications
o Hospitalization: disrupts school/peer activities, need to maintain contact w/ both
o Share room w/ other adolescents
o Will view Illness, tx, & procedures that alter their body image as devastating
o Teaching: include time w/o parents present, direct questions to the adolescent
o 7-14 y/o = Age of assent for medical decisions (parental consent is also needed)
o Maintain identity (prolonged hospitalizations): own clothing, posters, and visitors
Teen room/teen night may be helpful
Adolescent – part of decision regarding parents rooming in
o Some assessment questions asked w/o parent present
o Teaching: focus should be on “here and now” “how will this affect me today?”
- Accidents are a major cause of death in children and adolescents. Teach parents and children developmentally appropriate safety and accident prevention techniques
- 8 months child sits unsupported
- 15-18 months walking independently
- 18 months throws ball overhand
- 2 years old achieves 50% of adult height, speaks 2-3 word sentences
o Temper tantrums = normal/average behavior
- 4 years old birth length doubles, uses scissors
- 5 years old ties his or her shoes
- 9.5/10 years old female growth spurt before males
- Adolescence: when child forms their identity, rebellion against family is common
- Concepts of bodily injury
o Infants – after 6 months, they can remember pain
o Toddlers – fear intrusive procedures
o Preschoolers—fear body mutilation
o School-age fear loss of control of their bodies
o Adolescence – body image is major concern
Pain assessment and management (the fifth vital sign)
- Pain in peds usually unrecognized/untreated complications
o Delayed recovery, alterations in sleep patterns, and nutrition
o Infant/toddler = unable to verbalize experience of pain may display pain by actions and mannerisms
- Nursing assessment
o Verbal report by child (3 y/o = able to report location and degree of pain)
o Observe:
nonverbal signs of pain (grimacing, irritability, restlessness, difficulty sleeping/feeding)
physiologic responses to pain – usually acute pain (increased heart rate/respiratory rate and blood pressure, diaphoresis, and decreased oxygen levels)
o Include parents
- Nursing plans/interventions
o Use pain rating scale appropriate for the child’s age and developmental level
o Documentation – essential to effectively treat child’s pain
CRIES: infants 32-60 weeks
PRS – pain rating scale = all children of any age
• FACES and POKER CHIP SCALE – preschool age and older
• NUMERIC PAIN SCALE – 9 y/o and older
• OUCHER PAIN SCALE – 3-12 y/o w/ culturally specific photographs showing different levels of pain and discomfort
• FLACC – for the nonverbal child
o Facial expression, Leg Movement, Activity, Crying, & Consolability
o Non-pharmacologic interventions
According to child’s age and developmental level
Infants: pacifiers, holding, rocking
Toddlers/preschoolers: distraction (books, music, TV, blowing bubbles)
School-age/adolescents: guided imagery
Other: massage, hot/cold application, and deep breathing exercises
o Pharmacologic interventions
Before giving pain meds: verify dose is safe (based on weight)
Monitor vitals after giving opioids
5 y/o – may be taught to use PCA
May DENY pain in fear of receiving IM injection
- Child health promotion description
o Immunization of children against communicable disease = great accomplishment of modern medicine (decrease in childhood mortality & morbidity rates)
o Protection against disease should begin in infancy
Communicable diseases of childhood (care is virtually the same for all)
- Rubeola (measles)
• Highly contagious viral disease neuro problems or death
• Transmission: direct contact w/ droplets of the infected person
• Contagious: during prodromal period (fever and URI symptoms)
Photophobia, koplik spots on buccal mucosa
Rash on face, spreads downwards
- Paramyxovirus (mumps)
• Incubation: 14-21 days
• Symptoms: fever, headache, malaise, parotid gland swelling and tenderness
Manifestations: submaxillary/sublingual infection, orchitis, and meningoencephalitis
• Transmission: direct contact or droplet spread
• Tx: analgesics (pain), antiseptics (fever), and bedrest until swelling subsides
- Rubella (German Measles)
• Common viral disease, teratogenic effects on fetus (first trimester)
• Transmission: droplet and direct contact w/ infected person
• Discrete maculopapular rash, disappears in 3 days (starts on face, spreads to entire body)
- Pertussis (whooping cough)
• Acute infectious respiratory disease (usually infancy)
• G (-) bordatella bacillius
• Begins w/ URI symptoms
• Paroxysmal stage: prolonged coughing/crowing/whooping upon inspiration (4-6 weeks)
• Transmission: direct contact/droplet spread or freshly contaminated objects
• Vaccine recommended for all (CDC says doses at 2,4,6, and 15-18 months and then again between 4-6 y/o)
- Varicella (chicken pox)
• Viral disease
• Skin lesions: begin on the trunk and spread to the face and proximal extremities
Macule papule vesicle pustule
• Transmission: direct contact, droplet spread, and freshly contaminated objects
• Communicable: prodromal period until vesicles have crusted
• CDC recommends 2 doses of the varicella vaccine for everyone
First dose: 12-15 months
Second dose: 4-6 y/o
- Nursing care
• Isolation during period of communicability
• Treat fever w/ NONASPIRIN product
• Report occurrence to health dept.
• Prevent child from scratching skin (cut nail, apply mittens, provide soothing bath)
Diphenhydramine HCL (Benadryl) for itching
Handwashing: care for child/handling secretions or child’s articles
• Administer vaccine as per CDC’s recommendations
- Children w/ German Measles (Rubella) = serious threat to unborn siblings (TERATOGENIC)
- Common childhood problems are encountered by nurses caring for children in the community/hospital setting. Age influences severity & management.
Vaccines
- MMR Vaccine (measles, mumps, and rubella)
• 12-15 mos and repeated at 4-6 y/o or by 11-12 y/o
• Contraindication: hx of anaphylactic reaction to neomycin or eggs, altered immunodeficiency, and pregnant women
- Pertinent history should be obtained before administering certain immunizations b/c reactions to previous immunizations or current health conditions may contraindicate current immunizations
• MMR (Anaphylactic reaction to eggs or neomycin)
• DTAP (reactions, seizures, neuro symptoms after previous vaccine or systematic allergic reactions)
- DTap Vaccine (diphtheria, pertussis, and tetanus)
• At 2 months, begin three doses (at 2 month intervals), boosters given at 15-18 mos and 4-6 y/o
• Contraindications: encephalopathy within 7 days of previous DTap, HX of seizures, neuro symptoms after vaccine, and systemic allergic reactions
- Polio vaccine (inactive polio vaccine)
• Recommended for all <18 y/o, but at 2 mos then again at 4, boosters at 6-18 mos and 4-6 y/o
• Contraindication: hx of anaphylactic reaction to neomycin or streptomycin
- Hib (Haemophilus influenza type B)
• Protects against bacteria that cause epiglottitis, bacterial meningitis, septic arthritis)
• As early as 2 mos
• No contraindications
- Hep B
• Newborns before hospital discharge
• All children up to 18 y/o should be vaccinated
• Contraindications: anaphylactic reactions to common baker’s yeast
- Varicella (Chickenpox)
• 12-18 mos (must be at least 12 mos)
• School entry requirement in most states
• Give MMR and varicella on same day or > 30 days apart
- TB Skin testing
• Mantoux or Tine test
• Screening can be initiated at 12 mos
• Positive reaction = exposure to M. tuberculosis
- Subq injection, rather than intradermal injection, invalidates Mantoux test
- The common cold is not a contraindication for immunization
- Teaching after immunizations
• Normal side effects of DTaP: irritability, fever of 102 F, redness and soreness at site for 2-3 days
• Call HCP if seizures, high fever, or high-pitched crying occurs
• Warm washcloth at thigh injection site and “bicycling” legs w/ each diaper change decreases soreness
• Acetaminophen (Tylenol) admin orally q 4-6h (10-15mg/kg)
- Pertussis fatalities continue to occur in nonimmunized infants in the US
Pediatric Nutritional Assessment (profile of child and family’s eating habits)
- Iron deficiency: most common in children 12-26 months, adolescent females, and females in childbearing years
• Signs of deficiency:
Anemia, pale conjunctiva, pale skin color, atrophy of papillae on tongue, brittle, ridged, spoon-shaped nails, thyroid edema
Food sources: iron-fortified formula, infant high-protein cereal, infant rice cereal, liver, beef, pork, eggs, and green veggies.
- Vitamin D: recommended 400 IU/Day
• If mother is not taking enough, infant is recommended to receive oral dose of 400IU/day
- Preschool and school-age children most lack:
• Vitamin A, C, B6, and B12
Vitamin B2 (riboflavin) – signs of deficiency:
• Redness, fissuring of eyelid corners, burning, itching, tearing, eyes (photophobia), magenta-colored tongue, glossitis, seborrheic dermatitis, delayed wound healing
• Food sources: prepared infant formula, liver, cow’s milk, cheddar cheese, some green leafy vegetables, and enriched cereals
Vitamin A (retinol) – signs of deficiency:
• Dry, rough skin, dull cornea, soft cornea, bitot spots, night blindness, defective tooth enamel, retarted growth, impaired bone formation, decreased thyroxine formation
• Food sources: liver, sweet potatoes, carrots, spinach, peaches, and apricots
Vitamin C (ascorbic acid) – signs of deficiency
• Scurvy, receding gums that are spongy and prone to bleeding, dry, rough skin, petechiae, decreased wound healing, increased susceptibility to infection, irritability, anorexia, apprehension
• Food sources: strawberries, oranges/orange juice, tomatoes, broccoli, cabbage, cauliflower, spinach
Vitamin B6 (pyridoxine) – signs of deficiency
• Scaly dermatitis, weight loss, anemia, irritability, convulsions, and peripheral neuritis
• Food sources: meat (esp liver), cereals (wheat and corn), years, soybeans, peanuts, tuna, chicken, and bananas)
- Teach proper cooking and storage methods to preserve potency (cook veggies in small amounts of liquid, store milk in opaque container)
- Nursing plans and interventions
• Determine dietary history
24 hr recall: family recall all food/liquid intake during the past 24 hours
Food diary: 3-day record (2 weekdays and 1 weekend day) of all food/liquid intake and the amount of each
Food frequency record: questionnaire – ask family to record info about number of times/day or month child consumes items from the four food groups
• Perform clinical exam
Assess skin, hair, teeth, lips, tongue and yes
Measure: height, weight, BMI, head circumference, proportion, skinfold thickness, and arm circumference
• Height and weight – reflect past nutrition
• Weight, skinfold thickness, and arm circumference reflect present nutritional status (protein and fat reserves)
• Skinfold thickness = body’s fat content (half of fat = directly beneath skin)
Obtain biochemical analysis
• Plasma, blood cells, urine, or tissues from liver, bone, hair, fingernails = can determine nutritional status
• Labs: Hgb, Hct, albumin, creatinine, and nitrogen = can determine nutritional status
• Implement appropriate nursing interventions – teaching to correct nutritional deficits
- Diarrhea
• Increased number or decreased consistency of stools
• Can be serious or fatal symptom (especially in infancy)
• Causes (include, but not limited to)
Infections (bacterial, viral, parasitic)
Malabsorption problems
Inflammatory diseases
Dietary factors
• Conditions assoc. w/ diarrhea
Dehydration
Metabolic acidosis
Shock
• Nursing assessment
Usually occurs in infants
Hx of exposure to pathogens, contaminated food, dietary changes
Signs of dehydration
• Poor skin turgor/tenting of skin
• Absence of tears – dry and sticky mucus membranes
• Weight loss 5-15%
• Depressed fontanel
• Decreased urinary output, increased specific gravity
• Acidotic state
Lab signs of acidosis
• Loss of bicarbonate (serum pH <7.35)
• Loss of sodium and potassium through stools
• Elevated hematocrit and BUN
Signs of shock
• Decreased BP, rapid/weak pulse
• Skin = mottled to gray color, cool/clammy to touch
• Because the infant’s hands may be acrocyanotic, the best place to check cap refill is on the infant’s sternum
• Delayed cap refill (>4 seconds)
• Changes in mental state
• Nursing plans/interventions
Assess hydration status and vitals frequently, monitor I&O
Do NOT take rectal temperature
Rehydrate as prescribed, calculate IV hydration to include maintenance and replacement fluids
Collect specimens diagnose cause
Check stools for PH, glucose, and blood
Administer AB as prescribed
Check urine for specific gravity
Institute careful isolation precautions – WASH HANDS
Teach home care of child w/ diarrhea
• Oral rehydration solution (pedialyte or lytren)
• May need lactose-free diet (temporarily)
• SHOULD NOT RECEIVE antidiarrheals (Imodium)
• DO NOT give grape, orange, apple juice, cola or ginger ale (high osmolality)
- Important to document method used to take temperature. Ensure tympanic probe fits properly in the ear canal. Ensure client does not have otitis media
- Antibiotics are not recommended for diarrhea – only prescribed if caused by bacterial, fungal, or parasitic infection
- Add potassium to IV fluids only when client has adequate urine ouput
- Standard IV fluids used to treat pediatric dehydration: isotonic – LR, or NS. (20ml/kg)
Burns
- Tissue injuries caused by heat, electricity, chemicals or radiation
- Major cause of accidental death in children <15 (second to MV accidents)
- 75% are preventable
- Children >2 have a higher mortality rate
• Greater central body surface area – greatest part of body surface area is in the head and trunk = more serious effects from burns to trunk and head
• Greater fluid volume (proportionate to body size)
• Less effective cardio responses to fluid volume shifts
- Partial thickness burn – major if more than 25% of body surface
- Full thickness burn – major if more than 10% body surface
- Rule of nines can’t be used to assess the percentage of burn
- Lund-browder chart – takes into account the changing proportions of the child (THIS IS WHAT IS USED)
- Fluid needs should be calculated from the time of the burn
• Parkland formula – commonly used guideline for calculating fluid replacement and maintenance (based on child’s body surface area and should include vol. for losses and maintenance)
• Adequacy of fluid replacement is determined by evaluating urine output
- Urine output for infants and children should be 1-2 ml/kg/hr
Child Abuse
- Intentional or nonintentional physical and mental injury, sexual abuse, and emotional and physical neglect of a child under the age of 18 years old who is under the care of an adult.
- Children <1 – greatest risk of being abuse
- Child neglect = most common form of abuse
- Risk factors
- <4 y/o
- Children of special needs
- Abused individuals at risk of becoming perpetrator of abuse
- Nursing assessment
• Injuries not congruent w/ developmental age or skill
• Injuries not correlated w/ stated cause
Unusual places, different stages of healing, caused by belts, cords, cigarettes, iron, being shaken, bald patches, fractures at different healing stages
• Delay in seeking medical care
• FTT, unattended to physical problems, torn, stained, bloody undergarmends
• Lacerations of genitalia
• Child w/ STD
• Older child bedwetting or soiling
• Child = frightened and withdrawn
- Plans/interventions
• Nurses = legally required to report all cases of suspected child abuse
• Take color photographs, document factual, objective statements
• Establish trust and care for child’s physical problems – primary and immediate needs of these children
• Recognize own feelings of anger toward the parents
- Abused children have difficulty establishing trust. Select only one nurse to care for an abused child because the child will be less anxious w/ a consistent caregiver.
Poisonings
- Ingesting, inhaling, or absorbing a toxic substance
- Poison (particularly ingestion) = a common cause of childhood injury and illness
- > 6yr, peak at 2 yr
• Exploratory behavior, curiosity and oral motor activity of early childhood place the child at risk for poisonings
- 90% occur at home
- Nursing assessment
• Child fond near source of poison
• GI disturbances )nausea, abdominal pain, diarrhea, vomiting)
• Burns of mouth, pharynx
• Respiratory distress
• Seizures, changes in LOV
• Cyanosis, shock
- Use of syrup of ipecac is no longer recommended by the AAP. Teach parents that it is NOT recommended to induce vomiting in any way because it may cause more damage.
- Plans/interventions
• ID poisonous agent quickly
• Asses respiratory, cardiac, and neuro status
• Instruct parent to bring any emesis, stool, etc
• Gastric lavage, activated charcoal, N-acetylcysteine or naloxone HCL
• Teach home safety
Poison proof/childproof – ID locations of poisons
Put locks on cabinets
Use safety containers
Discard unused meds
• Make sure child is always under adult supervisipon
• Have local poison control # next to phone
• Examine environment from child’s POV, be aware of changes in the child’s environment
- Common household products that are poisonous to children if ingested: perfume and aftershave, sunburn relief products, alcohol, cigarettes or any type of tobacco product, and mouthwash
Lead poisoning
- There is no established “safe” level of lead for children – every system of the bod can be affected by lead exposure
- Lead exposure and elevated levels have been linked to decreased IQ’s
- <6 yr and younger = most vulnerable to the effects of lead b/c children tend to put things into their mouths
- Major cause of lead poisoning is lead-based paint
- Enters body thru ingestion, inhalation, or placental transfer.
• Ingestion by hand to mouth or contaminated hands, fingers, toys, or pacifiers = most common route
- Renal, neuro, and heme systems are the most seriously affected by lead
- BLL = currently used for screening and dx
- Erythrocyte protoporphyrin (EP) = good indicator of early toxic effects of lead, help est. the total potential body burden of lead in a child
- Nursing assessment
• Screen for lead poisoning/Universal screening
All children should have BLL at 1 and 2 yr
Any child between 3-6 yr that has not been screened should also be tested
• Physical assessment
General signs: anemia, acute cramping, abdominal pain, vomiting, constipation, anorexia, headache, lethargy, impaired growth
CNS signs (early): hyperactivity, aggression, impulsiveness, decreased interest in play, irritability, short attention span
CNS signs (late): mental retardation, paralysis, blindness, convulsions, coma, death
- Plans/interventions
• ID source
• Administer prescribed chelating agents to reduce high BLL levels
Children w/ peanut allergies should not be given chelating agents such as dimercaprol (BAL), d-penicillamine, or calcium disodium EDTA
• IM/IV administration
Calcium disodium EDTA (IM)
Dimercaprol in conjunction w/ calcium disodium EDTA to help efficacy of tx
• Considerations for admin
Rotate injection sites (chelating agents given IM)
Reassure child that injections are tx, not punishment
Administer the local anesthetic procaine w/ IM injection of calcium disodium EDTA to reduce discomfort
Apply EMLA cream over puncture site 2.5 hr before injection to reduce discomfort
Avoid giving iron during chelation – possible interactive effects
Cleansing enemas or cathartic for acute lead ingestion
Do not vaccum hard-surfaced floors or windowsills or window wells in homes built before 1960 (spreads dust)
Wash and dry child’s hands and face – toys and pacifiers frequently
- More lead is absorbed on an empty stomach. Hot water can contain higher levels of lead b/c it dissolves lead more quickly than cold water, so use only cold water for consumption (drinking, cooking, and esp for making infant formula)
Respiratory disorders
Important signs in children
- Cardinal signs of respiratory distress
• Restlessness, increased respiratory rate, increased pulse rate, diaphoresis
- Other signs of respiratory distress
• Flaring nostrils, retractions, grunting, adventitious breath sounds (or absent breath sounds), use of accessory muscles, head bobbing, alterations in blood gases – decreased PO2, elevated PCO2, cyanosis and pallor, alterations in mental status
- Symptoms of hypoxia
• Early: restlessness, anxiety, tachycardia/tachypnea
• Late: bradycardia, extreme restlessness, severe dyspnea
• Pediatrics: difficulty feeding, inspiratory stridor, nares, flaring, grunting w/ expirations, sternal retractions
- Nursing implications
• Pediatric client often goes into respiratory failure before cardiac failure
• KNOW THE SIGNS OF RESPIRATORY DISTRESS
Asthma
- Inflammatory reactive airway disease that is commonly chronic
• Airways edematous, congested w/ mucus
• Smooth muscles of bronchi and bronchioles construct
• Air trapping in the alveoli
- Nursing assessment
• Hx of asthma in the family, allergies, or eczema
• Home environment w/ pets/other allergents
• Tight (nonproductive) cough – usually/worsens at night
• Breath sounds: coarse, expiratory wheezing, rales, crackles
• Chest diameter enlarges (late s/s)
• Increased # of school days missed in past 6 months
• SIGNS OF RESPIRATORY DISTRESS
- Plans/interventions
• Monitor carefully for increasing respiratory distress
• Admin: rapid acting bronchodilators and steroids for acute attacks
• Maintain hydration (oral IV fluids)
• Monitor blood gas values (respiratory acidosis), pulse ox as prescribed
• Oxygen/nebulizer therapy as prescribed
• Monitor beta-adrenergic agonists and anti-inflammatory corticosteroids – commonly used medications
• Home care program (factors, triggers, allergens, use, monitoring peak flow, breathing exercises, monitoring drug (actions, doses, side effects), managing acute episodes)
- Epinephrine – rapid acting bronchodilator, drug of choice for acute asthma attack
• Adverse reactions: tachycardia, hypertensions, tremors, nausea
• Implications: give subq, IV via nebulizer – may be repeated after 20 minutes
- Calculating pediatric dosage - Change the weight from lb to kg (1kg=2.2lbs)
Cystic Fibrosis
- An autosomal-recessive disease that is causes dysfunction of the exocrine glands
• Lung insufficiency (most critical problem), pancreatic insufficiency, increased loss of sodium and chloride in sweat
• Nursing assessment
Most often found in white people
Meconium ileus at birth (10%-20%)
Recurrent respiratory infection, pulmonary congestion
Steatorrhea (excessive fat, greasy stools), foul smelling, bulky stools
Delayed growth, poor weight gain, salty skin when kissed (excessive sweating)
End stages: cyanosis, nail-bed clubbing, congestive heart failure
• Plans/interventions
Monitor respiratory status
Administer AB, pancreatic enzymes (cotazym-S, Pancrease), fat soluble vitamins (A,D,E, and K), oxygen & nebulizer treatments
• Oxygen hood: infants
• Nasal prongs: low-moderate concentrations of o2, up to 4-6L
• Tents: provide mist and oxygen. Monitor child’s temperature and keep edges tucked in, child dry
• Measurements of oxygen
o Pulse ox = oxygen saturation (SAO2) – attached to finger or toe, nurse should be aware of alarm parameters
o Blood gas evaluation monitored also
NORMAL PO2 = 80-100mmHg
NORMAL PCO2 = 35-45 mmHg
Evaluate effectiveness of respiratory treatments
Teach dietary recommendations: high in calories, high protein, moderate-high fat, moderate-low carbs
Age-appropriate activities, refer family for genetic counseling
- A child needs 150% of the usual calorie intake for normal growth and development
- Cystic fibrosis is now screened w/ tests performed after birth. The dx is made in the child’s first month of life before signs and symptoms occur.
Epiglottitis (usually H. influenzae)
- MEDICAL EMERGENCY: Severe, life-threatening infection of the epiglottis
- Progresses rapidly, causing acute airway obstruction
- nursing assessment
• sudden onset
• restlessness, high fever, sore throat, dysphagia
• drooling, muffled voice
• tripod position – child assuming upright, sitting position w/ chin out and tongue protruding
- plans/interventions encourage prevention w/ HiB vaccine, maintain child in tripod position
- prepare for intubation or trach, administer IV AB
- prepare for ICU, restrain to prevent extubation
- employ measures to decrease agitation and crying
Bronchiolitis
- viral infection of the bronchioles that is characterized by thick secretions
• usually caused by RSV, found to be readily transmitted by close contact w/ hospital personnel, families, and other children
• primarily in young infants
- assessment
• hx of URI, irritable, distressed infant
• paroxysmal coughing, poor eating, nasal congestion and flaring
• prolonged expiratory phase of respiration
• wheezing, rales can be auscultated
• deteriorating condition shallow, rapid respirations
- plans/interventions
• isolate child (contact if RSV), assign nurse to client w/ RSV who have no other client
• clear airway using bulb syringe, provide care in mist tent (oxygen)
maintain hydration, evaluate response to respiratory tx
administer palivizumab passive immunity against RSH in high risk children (<2 yr w/ hx of prematurity, lung disease, or CHD)
- in planning and providing nursing care, a patent airway is always the priority regardless of age
otitis media
- inflammatory disorder of the middle ear (suppurative or serous)
- anatomic structure of the ear predisposes young child to ear infections
- risk for conductive hearing loss if untreated or incompletely treated
- assessment
• fever, pain, infant may pull at ear, enlarged lymph nodes, discharge from ear (if drum ruptured)
• URI symptoms, vomiting, diarrhea
- Plans/interventions
• AB, reduce body temperature (tepid baths, acetaminophen)
• Position child on affected side
• Provide comfort measures (warm compress on affected ear)
• Teach home care – finish all AB, encourage follow-up, monitor for hearing loss, teach preventive care (avoid secondhand smoke, discourage bottle feeding when child = supine)
• Tympanostomy tubes placement
- Respiratory disorders are the primary reason most children and their families seek medical care. Therefore these disorders are frequently tested on the NCLEX-RN. Knowing the normal parameters of respiratory rates and the key signs of respiratory distress in children is essential
Tonsillitis
- Inflammation of the tonsils (viral or bacterial) may be streptococcus species
• If strep-related tx = VERY IMPORTANT, risk for developing AGN or rheumatic heart disease
- Assessment
• Sore throat, difficulty swallowing > 48 hrs
• Fever, enlarged tonsils (may have purulent discharge on tonsils)
• Breathing = may be obstructed tonsils touching, called kissing tonsils
• Throat culture to determine cause (bacteria or virus)
- Plans/interventions
• Collect throat culture – if prescribed
• Instruct parents in home care (warm saline gargles, ice chips, antibiotics, fever – acetaminophen)
• Tonsillectomy? preop teaching/assessment, monitor for signs of post op bleeding (Frequent swallowing, vomiting fresh blood, clearing throat)
Encourage soft foods, oral fluids (avoid red fluids mimics signs of bleeding)
DO NOT USE STRAW
Teach highest risk of hemorrhage – first 24 hrs and 5-10 days after surgery
- Teach parents why it is important to administer pain meds as prescribed (usually cough suppressant for tonsillectomy – coughing may loosen sutures, create clots, active bleeding)
- Removal of ingested sharp object is a medical emergency
Cardiovascular Disorders (IVC/SVC RA RV PA LUNGS PV LA LV AV BODY!)
Congenital Heart Disorders
- Heart anomalies that develop in utero and manifest at birth or shortly after
- Categories
• Acyanotic: increased fatigue, murmur, increased risk of endocarditis, CHD, growth retardation
Left-to-right shunts or increased pulmonary blood flow
• ASD
• VSD
• PDA
Obstructive pulmonary blood flow defects
• Coarctation/stenosis of the aorta
• Cyanotic: squatting, cyanosis, clubbing, and syncope
Right-to-left shunts or decreased pulmonary blood flow
• Tetralogy of fallot
Mixed pulmonary blood flow
• TGA,TA
Acyanotic heart defects
VSD – ventricular septal defect (increased pulmonary blood flow)
- Hole between both ventricles
- Oxygenated blood from the left ventricle is shunted to the right ventricle and recirculated to the lungs
- Small defects may close spontaneous
- Large defects cause Eisenmenger syndrome or CHF and require surgical closures
ASD – atrial septal defect (increased pulmonary blood flow)
- Hole between the atria
- Oxygenated blood from left atrium shunted to right atrium and lungs
- Most defects don’t compromise children seriously
- Surgical closure is recommended before school age – can lead to significant problems such as CHF, atrial dysrhythmias later in life if not corrected
PDA - Patent Ductus Arteriosus (increased pulmonary blood flow)
- Abnormal opening between the aorta and the pulmonary artery
- Usually closes within 72 hours after birth
- Increased blood flow to lungs = pulmonary hypertension
- May require medical intervention w/ indomethacin (Indocin) admin or surgical closure)
COA - Coarctation of the Aorta (obstruction of blood flow from the ventricles)
- There is an obstructive narrowing of the aorta
- Most common sites = aortic valve and aorta near ductus arteriosus
- Common finding = HTN in upper extremities and decreased/absent pulses in lower extremities
- May require surgical correction
AS - Aortic Stenosis (Obstruction of Blood flow from ventricles)
- Obstructive narrowing immediately before, at, or after the aortic valve (most commonly valvular)
- Oxygenated blood flow from left ventricle into systemic circulation = diminished
- Symptoms caused by low cardiac output
- May require surgical correction
The Traditional Three T’s of Cyanotic Heart Disease
- Polycythemia (blood cancer) is a common concern in children w/ cyanotic defects
TOF - Tetrology of Fallot (decreased pulmonary blood flow)
- Combination of four defects
- 1. VSD
- 2. Overriding aorta (over and above VSD)
- 3. PS – pulmonary stenosis, obstructs right ventricular outflow
- 4. Right ventricular hypertrophy – severity of pulmonary stenosis relates to hypertrophy and extent of shunting
TA – truncus Arteriosus (mixed blood flow)
- Pulmonary artery and aorta do not separate - one artery (truncus) rather than two arteries (aorta and pulmonary artery) arises from BOTH ventricles
- One main vessel receives blood from the left and right ventricles together
- Blood mixes in right and left ventricles through a large VSD cyanosis
- Increased pulmonary resistance increased cyanosis
- Congenital defect needs surgical correction; only presence of the large VSD allows for survival at birth
TGA – transposition of the great vessels (mixed blood flow)
- The great vessels are reversed – pulmonary artery leaves the left ventricle, the aorta exits from the right ventricle
- Pulmonary circulation arises from the left ventricle and the systemic circulation arises from the right ventricle
- This is incompatible w/ life unless coexisting VSD, ASD, and/or PDA present
- The diagnosis is a medical emergency. The child is given prostaglandin E (PGE) to keep the ductus open
*basic differences between cyanotic and Acyanotic defects*
- Acyanotic: has abnormal circulation – however, ALL blood entering the systemic circulation is oxygenated
- Cyanotic: has abnormal circulation w/ UN-oxygenated blood entering the systemic circulation
Care of the child w/ CHD (congenital heart disease)
- Manifestations of CHD
• Murmur (present, absent, thrill or rub)
• Cyanosis, clubbing of digits (usually after age 2)
• Poor feeding, poor weight gain (FTT)
• Frequent regurgitation
• Frequent resp. infections
• Activity intolerance, fatigue
- Assess:
• Heart rate, rhythm, and heart sounds
• Resp. status/difficulty
• Pulses (quality and symmetry)
• Blood pressure (upper and lower)
• Feeding difficulties, tired easily
- The heart rate of a child increases w/ crying or fever
- Infants may require tube feeding to conserve energy. Infants being tube-fed need to continue to satisfy their sucking needs
- Plans/interventions
• Provide care for the child w/ cardio dysfunction
Maintain hydration (polycythemia increases risk for thrombus formation)
Maintain neutral thermal environment
Monitor for fever
Plan frequent rest periods, organize activities to disturb child only as indicated
Admin. Digoxin and diuretics as prescribed
Monitor for signs of deteriorating condition or CHF
Teach family the need for prophylactic AB before any dental or invasive procedures due to risk for endocarditis
• Assist w/ diagnostic tests and support family during DX
ECG, ECHO
• Prep family and child for cardio cath (when surgery is probably or as an intervention for certain procedures)
Risks of catheterization are similar to those cardiac surgery
• Arrhythmias
• Bleeding
• Perforation
• Phlebitis
• Arterial obstruction at the entry site
Child requires reassurance and close monitoring after catheterization
• Vital signs
• Pulses
• Incision site
• Cardiac rhythm
Prep family and child for surgical intervention if necessary
Prepare child as appropriate for age
• Show ICU.
• Explain chest tubes, IV lines, monitors, dressings and ventilator
• Show family/child waiting area, provide emotional support
• Use a doll/drawing for explanations
• Include/incorporate family as much as possible in client teachings
Congestive Heart Failure (CHF) – more assoc. w/ Acyanotic defects (VSD, ASD, PDA, COA, AS)
- Condition in which the heart is unable to effectively pump the vol. of blood presented to it
- CHF is a common complication of CHD. It reflects the increased workload of the heart caused by shunts or obstructions. The two objectives in treating CHF are to reduce the workload of the heart and increase cardiac output
- Nursing assessment
• Tachypnea, tachycardia – SOB
• Difficulty breathing, cyanosis
• Grunting, wheezing, pulmonary congestion
• Edema (face, eyes of infants) weight gain
• Diaphoresis (sweating – esp. head)
• Hepatomegaly
- Plans/interventions
• Monitor vitals frequently + report signs of increasing distress
• Asses respiratory functioning frequently
• Elevate HOB or use infant seat
• Admin O2 therapy, digoxin, diuretics
• Weigh frequently, report unusual weight gains
• Maintain strict I/O, weigh diaper (1g=1mL)
• Provide low-sodium diet or formula
• Gavage feed infants if unable to get adequate nutrition by mouth
- When frequent weights are required, weigh client on the same scale at the same time of day so that accurate comparisons can be made
Managing Digoxin
- Before admin: nurse must take apical pulse for 1 min to assess for bradycardia. Hold if pulse is < normal heart rate for child’s age
- Therapeutic blood levels of digoxin are 0.8-2.0 mL
- Families should be taught safe home admin
• Admin on regular basis – DO NOT SKIP or make up for missed doses
• Give 1hr before meals are 2hrs after meals. DO NOT MIX W/ FORMULA OR FOOD
- Take a child’s pulse before admin and know when to call the HCP
- Keep in safe place (locked cabinet)
- Nurse must be acutely aware of signs of toxicity. A small child/infant CAN’T describe feeling bad or nauseous
- Vomiting is a common early sign of toxicity – often overlooked b/c infants commonly spit up
- Other GI symptoms include anorexia, diarrhea, and abd pain
- Neurologic signs – fatigue, muscle weakness, and drowsiness
- Hypokalemia can increase digoxin toxicity
Rheumatic Fever (inflammatory disease)
- Most common cause of acquired heart disease in children – usually affects the aortic and mitral valves of the heart
- Assoc. w/ antecedent beta-hemolytic streptococcal infection
- Collagen disease that injures the heart, blood vessels, joints, and subq tissue
- Nursing assessment
• Chest pain, SOB (carditis), tachycardia – even during sleep
• Migratory large-joint pain, chorea (irregular involuntary movements)
• Rash (erythema marginatum), subq nodules over bony prominences
• Fever
• Labs – elevated ESR, ASO (antistreptolysin O titer)
- Plans/intervention
• Monitor vitals, assess for increasing signs of cardiac distress
• Encourage bed rest (as needed during febrile illness)
• Assist w/ ambulation, reassure that chorea is temporary
• Admin penicillin/erythromycin and aspiring for anti-inflammatory/anticoagulation
Penicillin G IM: prophylaxis for recurrence of rheumatic fever
• Adverse reactions: allergic reactions ranging from rashes to anaphylactic shock and death
• Nursing implications: released VERY slowly, over several weeks = sustained levels of concentration – have emergency equipment available wherever meds are administered. Always determine existence of allergies to PCN and cephalosporins, check chart & record and inquire of client and family
• Teach home care
Necessity for prophylactics (AB – PO/IM), Penicillin G (IM each month)
Inform dentist and other HCP of dx to evaluate necessity for prophylactic AB
Kawasaki Disease (Mucocutaneous Lymph Node Syndrome)
- Acute systemic vasculitis that can cause damage to vessels, including the coronary arteries that supply blood flow to the heart
- Also affects the mucus membrane lining of the mouth, nose, and throat as well as the lymph nodes and skin
- Causes permanent damage to the main arteries of the heart aneurysm of the coronary artery
• Cause = unknown
• Usually seen in children < 5yrs
• Three phases – acute, subacute, convalescent
• Early treatment = essential to decrease chances of permanent heart damage
- Assessment (data collection)
- Acute phase
• High fever 39 C or 102.2 F (or higher) for > 5 days
• Conjunctival redness w/o discharge, cracked dried lips, strawberry tongue
• Swollen lymph nodes of neck
• Rash on trunk/genital area, red swollen hands and feet
- Subacute phase
• Peeling of hands and feet
• Cardio manifestations may be seen
• Skeletal joint pain
• GI manifestations: abd pain, vomiting, diarrhea
- Convalescent (last) phase
• Starts when all signs are gone, ends when labs are normal
- Extreme irritability is seen in the child during the disease process
- Plans/interventions
• IVIG and aspirin (salicylate therapy) to treat disease process, not treat the fecer
• Treat high fevers w/ acetaminophen
• Monitor cardiac status via I/O (clear liquids and soft foods) and daily weights
• Minimize skin discomfort w/ lotion and cool compresses
• Initiate meticulous mouth care
• Support family (comforting child during periods of irritability)
• Discharge teaching and home referral
Neuromuscular disorders
Down Syndrome (NURSING GOAL: help child reach optimal level of functioning)
- Most common chromosomal abnormality in children
• Various physical characteristics and cognitive impairment
Small head, flat-wide nasal bridge
Inner epicanthal eye fold
Upward, outward slant of the eyes
Brushfield spots on the iris (white spots)
Small, irregularly shaped ears; low-set
Small mouth and protruding tongue
Short neck, short-stubby hands w/ single crease in palm (simian crease)
Short arms and legs (compared to body) short in stature
Hypotonic flexibility, atlantoaxial instability
Short, stubby toes w/ enlarges space between big toe and other toes
Hyper extensible and lax joint (hypotonia)
• Occurs when cell division is abnormal – extra genetic material from chromosome 21
- Common assoc. problems
• Cardiac defects, respiratory infections
• Feeding difficulties, delayed developmental skills (mental retardation, IQ 20-70)
• Skeletal defects, altered immune function
• Endocrine dysfunctions, hypothyroidism, diabetic muscular infarction (DMI)
- Plans/interventions
• Assist and support parents during the dx process and management of problems
• Assess/monitor growth and development
• Teach use of bulb syringe, teach signs of respiratory infection
• Assist family w/ feeding problems (feed to back and side of mouth)
• Monitor for signs of cardiac difficulty or respiratory infection
• Refer to early intervention program and specialists (nutrition, speech, PT, and OT)
Cerebral Palsy
- Non-progressive injury to the motor centers of the brain neuromuscular problems of spasticity or dyskinesia (involuntary movements)
- Healthy infant during uterine development, the birthing process, or exposure to an infection (meningitis) during early years of development
- It is irreversible, extent of damage depends on location of trauma to the brain
- Symptoms worsen or improve over time
- Assoc w/ cognitive impairment and seizures
- Causes:
• Anoxic injury before, during, or after birth
• Maternal infections
• Kernicterus
• LBW (major risk factor)
- Nursing assessment
• Persistent neonatal reflexes after 6 months (moro, tonic neck)
• Delayed developmental problems
• Apparent early preference for one hand, poor suck, tongue thrust
• Spasticity (difficulty w/ diapering)
• Scissoring of legs (extended and crossed over each other/feet plantar flexed)
• Involuntary movements, seizures
- Plans/interventions
• ID CP via follow-up of high risk infants (premature, breech, cardiac/respiratory distress during birth, low apgar score, product of multiple pregnancies, severe jaundiced
• Refer to community-based agencies, coordinate w/ PT, OT, ST, nutritionist, OS, Neuro
• Support family thru grief process at dx and thru child’s life. Care is very challenging
• Anticonvulsants – phenytoin (Dilantin), diazepam (Valium)
- Feed infant or child w/ CP using nursing interventions aimed at preventing aspiration. Position child upright and support lower jaw.
ADHD – attention deficit disorder, attention deficit hyperactivity disorder
- Neurodevelopmental disorders: recent studies indicate they me be linked to genetics
- Children up to 16 y/o are identified as having ADD if they exhibit a minimum of SIX inattention symptoms
Spina Bifida
- Malformation of the vertebrae and spinal cord varying degrees of disability and deformity depending on the location of the malformation (neural tube defect)
- Types
• Spina bifida occulta: defect of vertebrae only. NO SAC, usually benign
Bladder and bowel problems may occur
• w/ meningocele and myelomeningocele: A SAC is present usually along spine
• meningocele: contains ONLY MENINGES AND SPINAL FLUID
less neurologic involvement than myelomeningocele
• myelomeningocele: SAC containing spinal fluid, meninges, and nerves
MORE SEVERE than meningocele
- Prevention: women in childbearing years before and during pregnancy should consume a minimum of 400 mcg of folic acid daily (supplements or folic-enriched foods)
• Egg yolks, dark green veggies, citrus fruits, juices, or beans
- Every child w/ hx of spina bifida should be screened for latex allergies
- Nursing assessment
• Occulta: dimple w/ or w/o hair tuft at base of spine
• Myelomeningocele: sac is usually lumbar or lumbosacral
• Flaccid paralysis and limited or no feeling below the defect
• HC w/ variance w/ norms on growth grids
• Associated problems
Hydrocephalus (90% of myelomeningocele)
Neurogenic bladder, poor anal sphincter tone
Congenital dislocated hips, club feet
Skin problems (due to anesthesia below defect)
Scoliosis
- Plans/interventions
• Preoperative: place infant in prone position
Keep sac free of stool and urine
Cover sac w/ moist sterile dressing
Elevate FOB, position child on his/her abdomen W/ legs abducted
Measure HC at least q8hrs, check fontanel
Assess neuro function, monitor for signs of infection
Empty bladder using Crede method, or catheterize if needed
Promote parent-infant bonding
• Postoperative phase: place infant in prone position
Make same assessments as pre-op
Assess incision for drainage and infection
Assess neuro function
• Long-term care
Teach catheterization program when child is young (help older w/ self)
Administer: propantheline (Pro-banthine) or bethanechol (Urecholine)
• To improve continence
Develop bowel program
• High fiber diet, increased (regular fluids)
• Suppositories as needed
Assess skin condition frequently
Assist w/ ROM, ambulation, and bracing (as tolerated)
Coordinate w/ neuro, orthopedist, urologist, PT, and nutritionist
• Support independent functioning of child
• Assist family to make realistic developmental expectations of the child
Hydrocephalus
- Condition characterized by abnormal accumulation of CSF within ventricles of the brain that does not drain properly from the cranium
• Usually caused by obstruction in the flow of CSF between ventricles
• Enlargement of the ventricles pressure on the brain tissue
• Often assoc. w/ spina bifida, can be a complication of meningitis
- Infants w/ hydrocephalus have enlarged HC as a result of widening fontanels that compensate for accumulating CSF and help relieve pressure of the developing brain
- Signs if increase ICP opposite of shock
• Shock: increased pulse, decreased BP
• Increased ICP: decreased pulse, increased BP
- Nursing assessment
• Toddlers and older children classic signs of increased ICP
Change in LOC, irritability, vomiting
Headache on awakening, motor dysfunction
Unequal pupil response, seizures
Decline in academics, change in personality
• Infants and Increased ICP
Irritability, lethargy, increasing HC
Bulging fontanels, widening suture lines
“sunset” eyes, high-pitched cry
Feeding difficulties, decreased muscle tone/strength
- Baseline data on the child’s usual behavior and level of development = essential so changes assoc. w/ increased ICP can be detected early
- Plans/interventions
• Prep infant/family for dx procedures
• Monitor for signs of increased ICP
• Maintain seizure precautions, elevate HOB
• Prep parents for surgery (ventricular shunt placement) drain excess fluid off brain
• Post-op care
Assess for signs of shunt malfunction
Infant
• Change in size, signs of bulging, tenseness in fontanels and separation of suture lines
• Irritability, lethargy, or seizure activity
• Altered vital signs and feeding behavior
Older child
• Change in LOC, complaint of headache
• Changes in customary behavior (sleep, developmental capabilities)
Assess for signs of infection (meningitis)
• Increased fever > 38.6 C or 100.5 F
• Shunt tract = reddened, tender, and swollen – drainage may be present
• Decreased feeding, increased vomiting
• Stiff neck and headache
Monitor I/O closely
Assess surgical site (head and abd)
• Home care program
Teach to watch signs of increased ICP and infection
Child will eventually outgrow shun and show difficulty
Child will need shunt revision
Anticipatory guidance for potential problems for growth and development
Seizures
- Uncontrolled electrical discharges of the neurons in the brain
• More common in children under the age of 2 years
• Can be assoc. w/ immaturity of the CNS – fever, infection, neoplasms cerebral anoxia, and metabolic disorders
- Categorized as generalized or partial
• Generalized:
Tonic-clonic (Grand-mal): consciousness is lost
(1) Tonic phase: generalized stiffness of entire body
(2) Clonic phase: spasm followed by relaxation
absence (petit-mal): momentary LOC, posture is maintained, minor face/eye/hand movements
myoclonic: sudden, brief contractures of a muscle or group of muscles, no postictal state – may be symmetrical or include LOC
• partial: arise from a specific area in the brain and cause limited symptoms
ex: focal and psychomotor seizures
- nursing assessment
• Tonic-clonic(grand mal)
Aura (warning sign of impending seizure)
LOC
Tonic phase generalized stiffness of entire body
Apnea, cyanosis
Clonic phase: spasms relaxation
Pupils dilated, nonreactive to light
Incontinence
Post seizure: disoriented, sleepy
• Absence seizure (petit mal)
Onset between 4-12y/o
Last 5-10 secs
Child appears to be inattentive, daydreaming
Poor performance in school
- Medication noncompliance is the most common cause of increased seizure activity
- Plans/interventions
• Maintain airway during seizure client to side to aid ventilation
• Do not restrain client, protect client from injury and support neck (avoid flexion)
• Document seizures, noting all data in assessment
• Maintain seizure precautions
Reduce environmental stimuli as much as possible
Pad side rails/crib rails
Have suction equipment and oxygen quickly accessible, set up at the bedside
Tape oral airway to the HOB
- DO NOT USE TONGUE BLADE (PADDED OR NOT) – during seizure activity – can cause traumatic damage to the oral cavity
• Support during dx tests (EEG, CT
• Support during workup for infections (ex: meningitis)
• Administer anticonvulsant meds as prescribed
Tonic-clonic phenytoin, carbamazepine, phenobarbital, and fosphenytoin
Absence ethosuximide, valproic acid
• Monitor therapeutic drug levels
• Teach family about drug admin: dosage, action, and side effects
Bacterial Meningitis
- Bacterial inflammatory disorder of the meninges that cover the brain and spinal cord
• Usually caused by H. influenza (less prevalent), S. pneumo, and N. meninges
• Source: middle ear or nasopharynx, wounds, fractures of skull, lumbar punctures, shunts
• Exudate covers brain cerebral edema occurs
• Lumbar puncture shows:
Increased WBC, decreased glucose, elevated protein
Increased ICP, positive culture for meningitis
- Decreased glucose and elevated protein occur b/c bacteria present in the CSF consume the glucose and then defecate the protein
- Nursing assessment
• Older children: classic signs of increased ICP (hydrocephalus), fever, chills, neck stiffness, opisthotonos, photophoia, (+) kernig sign (inability to extend leg when thigh is flexed anteriorly at hip), (+) Brudzinski sign (neck flexion causing adduction and flexion movements of lower extremities)
• Infants and younger children (3mos-2y/o): absence of classic signs, ill w/ generalized symptoms, poor feeding, vomiting, irritability, bulging fontanel (IMPORTANT), seizures
• Neonates (birth-2mos): very difficult to diagnose, temp = nonspecific – may be normal, hypothermia or hyperthermia, symptoms can appear a few days after birth. Infant has difficulty eating/refuses to eat. Weak cry, vomiting and diarrhea. movement decreases w/ tone, restless – sleep pattern changes. Late sign = bulging/tense fontanel
- Plans/interventions
• AB – ampicillin, ceftriaxone, or chloramphenicol
• Antipyretics
• Isolate for at least 24 hours
• Monitor vitals and neuro seizure precautions
• Position (comfort): HOB slightly elevated and client on side (if prescribed)
• HC daily (infants)
• Hib vaccine to protect against H.influenzae
- Monitor hydration status & IV therapy carefully. w/ meningitis, may be inappropriate ADH secretions fluid retention (cerebral edema) and dilution hyponatremia
Reye Syndrome
- Acute, rapidly progressing encephalopathy and hepatic dysfunction
• Causes: antecedent viral infections (flu, chicken pox), occurrence often assoc. w/ aspirin
• Staged according to the clinical manifestations to reflect severity of the condition
- Assessment
• School-age (usually)
• Lethargy, rapidly progressing to deep coma (marked cerebral edema), vomiting
• Labs: elevated AST, ALT, lactate dehydrogenase, serum ammonia
Decreased PT
- Plans/interventions
• Critical care early in syndrome
• Monitor neuro status: frequent noninvasive assessments and invasive ICP monitoring
• Maintain ventilation
• Monitor cardiac parameters/invasive cardiac monitoring
• Mannitol (if prescribed) increase blood osmolality
Osmotic diuretic used to reduce cerebral edema, postoperative swelling or trauma
Adverse reactions: circulatory overload, confusion, hypokalemia, hyponatremia
Nursing implications: use in-line filter for IV admin and avoid extravasation, monitor I/O, furosemide (Lasix) may also be prescribed
• Monitor I/O, Foley catheter care
• Emotional support
Brain Tumors
- Third most common cancer in children (after leukemia and lymphomas)
• Most: infratentorial difficult to excise surgically, close to vital structures
• Medullablastoma: most common childhood brain tumor
- Assessment
• Headache
Headache upon awakening = common presenting symptom of brain tumor in children
• Vomiting (usually morning) w/o nausea
• Loss of concentration, change in behavior/personality
• Vision problems, tilting of head
• Infants: widening sutures, increasing frontal occiput circumference, tense fontanel
- Plans/interventions
• ID baseline neuro functioning
• Support child/family during dx and tx (assess family’s response, plan teaching)
• Surgery provide preoperational teaching
Head will be shaved
Describe ICU, dressings, IV lines, etc
ID child’s developmental level, plan teaching accordingly
• After surgery: position client as prescribed by HCP
Most post-op clients w/ infratentorial tumors are prescribed to lie flat or turn to either side
Large tumor may require that child NOT be turned to the operative side
• Monitor IV fluids and output carefully. Overhydrating cerebral edema and increased ICP
Suctioning, coughing, straining, and turning can increased ICP
• Administer steroids and osmotic diuretics (as prescribed)
• Support child/family to promote optimal functioning post-op
Muscular dystrophy
- Inherited disease of the muscles muscle atrophy and weakness
• Most serious/common of the dystrophies: Duchenne muscular dystrophy: X-linked recessive disease affecting primarily males appears in early childhood (3-5yrs), children appear normal at birth until s/s of the disease manifest
• By 9-11yrs, child loses ability to walk independently
- Assessment
• Waddling gait, lordosis
• Increasing clumsiness, muscle weakness
• Gowers sign: difficulty rising to standing position, has to “walk-up” legs, by using hands
• Pseudo-hypertrophy of muscles (calves) due to fat deposits
• Muscle degeneration: especially of the thighs and fatty infiltrates, cardiac muscles (detection: muscle biopsy)
• Delayed cognitive development
• Later: scoliosis, respiratory difficulty, cardiac difficulties
• Eventual wheelchair dependency, confinement to bed
- Plans/interventions
• Provide supportive care, exercise (passive and active)
• Prevent exposure to respiratory infection
• Encourage a balanced diet (avoid obesity)
• Support family (grief), support MDA participation
• Coordinate w/ HCP: PT, OT, nutrition, neuro, ortho, and geneticist
- encourage the parents of children w/ any neuromuscular disease to allow child to do as much as possible for themselves – try to maintain muscle function and independence
Renal Diseases
AGN – acute glomerulonephritis
- Immune complex response to an antecedent beta-hemolytic strep infection of skin or pharynx
- Antigen-antibody complexes trapped in the membrane of glomeruli inflammation and decreased glomerular filtration
- Assessment
• Recent strep infection (strep throat)
• Mild to moderate edema (usually on face), abdomen, hands and feed
• Irritability, lethargy, hypertension
• Dark colored urine (hematuria), slight to moderate proteinuria
• Elevated ASO (anti-strep titer), BUN, and creatinine
• Oliguria
- Plans/interventions
• Supportive care
• Monitor vitals (especially BP) frequently (admin antihypertensives if prescribed)
• Monitor I/O, weight daily
• Provide low-sodium diet w/ no added salt, low potassium (if oliguric)
• Bed rest during acute phase (usually 4-10 days)
• Monitor for signs of CHF and renal failure
Decreased urine output is the first sign of renal failure
Nephrotic syndrome
- Disorder in which the basement membrane of the glomeruli become permeable to plasma proteins (most often idiopathic in nature)
- Usually occurs between 2-3 years
- May include exacerbations and remissions over several years
- Assessment
• Edema: begins insidiously, becomes severe and generalized
• Lethargy, anorexia, pallor
• Frothy-appearing urine, MASSIVE proteinuria decreased serum protein (hypoproteinemia)
• Elevated serum lipids
- Plans/interventions
• Supportive care
• Monitor temperature (assess for signs of infection)
• Provide skin care (edema = extremely vulnerable)
• Bed rest during edematous phase
• Meds: Steroids (prednisone, cyclophosphamide/cytoxan – if nonresponsive to prednisone), cholinergics (bethanechol/urecholine)
IV albumin followed by diuretic
• Monitor I/O
• Measure abdominal girth daily
• Small, frequent feedings: normal-protein, low-salt diet.
• Home care: daily weights, medication side effects
Signs of relapse, train to prevent infection
UTI – urinary tract infection
- Bacterial infection anywhere along the urinary tract (mast ascend)
• Infants: vague symptoms, fever, irritability, poor food intake, diarrhea, vomiting, jaundice, strong-smelling urine
• Older children: urinary frequency, hematuria, enuresis, dysuria, fever
- Plans/interventions
• Suspect/assess for UTI in infants who are ill
• Assess for recurrent UTI (infants/young boys UTI may indicate structural abnormalities of urinary system
• Collect clean voided or catheterized specimen
Clean catch: best obtained using a urine bag to catch the specimen
• Apply from side to side or back to front (diaper applied over bag)
• Check child frequently to note urination
Catheterization: sterile feeding tube often used to catheterize small children/infants
Sterile specimen: small infants – best collected by the physician performing a bladder tap: urine – aspirated thru a needle inserted directly onto the bladder. Nurse = responsible for making sure the infant is appropriately hydrated and restrained during the procedure
• AB
• Teach home program: finish all meds, follow-up specimens needed, avoid bubble baths, increases ACIDIC oral fluids (apple juice, cranberry juice), instruct to void frequently, clean genital front to back, and note symptoms of recurrence
Vesicoureteral Reflex
- Result of valvular malfunction and backflow of urine into ureters (and higher) from the bladder (severe cases = assoc. w/ hydronephrosis)
- Assessment
• Recurrent UTI
• Reflux common w/ neurogenic bladder
• Reflux noted on voiding cystourethogram (VCUG)
- Plans/interventions
• Home prevention for UTI
• Teach importance of medication compliance, usually leads to resolution of mild cases
• Provide support for child/family requiring surgery
Goal of ureteral reimplantation: stop reflux, prevent kidney damage
• Monitor post-op drainage (may be suprapubic or urethral)
Measure output from both catheters
Assess dressing/incision for drainage
Restrain child’s hands as necessary
• Maintain hydration (IV or oral fluids)
• Manage pain relief post-op (surgical pain, bladder spasms)
Wilms Tumor (nephoblastoma)
- Malignant renal tumor: embryonic in origin, tumor = encapsulated
- Occurs in preschool children
- Usually one kidney is affected
- Prognosis: good w/ early detection, surgery, adjuvant chemo, and post-op radiation therapy
- Assessment: fever, pallor, lethargy, elevated BP (excess renin secretion), hematuria (rare)
- Plans/interventions
• Support family during dx period, chemo, or radiation
• Protect child from injury: place a sign on bed “no abdominal palpation” to prevent accidental fragmentation and dislodging into the abdominal cavity
• Prep family/child for imminent nephrectomy
• Post-op care
Monitor for increased BP
Monitor kidney function (I/O, specific gravity)
Abdominal surgery client care: maintain NG tube, check for bowel sounds
Hypospadias
- Congenital defect of urethral meatus in males – urethra opens on ventral side of penis behind the glans
- Assessment
• Abnormal meatus, altered voiding stream
• Presence of chordee (penis is curved)
• Undescended tested and inguinal hernia (may occur concurrently)
- Plans/interventions
• Prep child/family for surgery (no circumcision before surgery)
• Assess circulation to tip of penis post-op
• urinary drainage after urethoplasty (foley catheter, suprapubic tube, urethral stent)
• restrain child’s arms/legs (if necessary)
• maintain hydration (IV and oral fluids)
• home care: care of catheters/drainage bag, prevention of catheter displacement/blockage. Instruct to increase oral fluids. Describe infection signs!
GI DISORDERS
Cleft Lip or Palate
- malformations of the face/oral cavity that seem to be multifactorial in hereditary origin
• cleft lip readily apparent
• cleft palate may not be identified until infant has difficulty w/ feeding
- Initial closure of left lip is performed when infant is approx. 10lbs and has and Hgb of 10 g/dl
- Closure of cleft palate defect at 1 year (to minimize speech impairment)
- Assessment
• Failure of fusion of the lip, palate, or both
• Difficulty swallowing and sucking
• Parent reaction to facial defect
- Plans/interventions
• Promote family bonding/grieving during newborn period
• Inform family: successful corrective surgery is available
• Newborn period: assist w/ feeding feed in upright position, slowly w/ frequent burping. Use soft, large nipples, lamb nipples, prosthetic palate, or rubber-tipped Asepto syringe (support breastfeeding mother if possible)
• ESSR method of feeding
Enlarge nipple opening
Stimulate the child to Suck
Swallow, normally
Rest (use caution to prevent aspiration)
• Post-op care:
maintain patent airway, proper positioning
• Remove oral secretions carefully (bulb syringe or Yankauer suction set)
• Cleft lip: position client upright in infant seat (NOT PRONE)
• Cleft palate: place client on side or abdomen
Protect surgical site
• Minimize crying to prevent strain on lip suture line
• Maintain logan bow to lip if applied
Provide care for restrained child age-appropriate stimulation
• Resume feeding as prescribed: clean suture w/ sterile water feeding
Formula remaining on suture line impede healing, infection
• Encourage family participation (care and feeding)
Fluids: via cup or asepto syringe w/ rubber tip (gravity feeder)
Diet progresses from clear to full liquid diet
Child may go home on soft diet (nothing harder than mashed potatoes)
• Cleft palate coordinate LTC w/ other team members (plastic surgeon, ENT, nutritionist, speech therapist, ortho, peds, and nurse))
- Typical parents/family reactions to a child w/ an obvious malformation such as cleft lip/palate are guilt, disappointment, grief, sense of loss, and anger
• Helpful to families provide pictures before and after surgical repair of children w/ cleft lip/palate
Esophageal Atresia w/ Tracheoesophageal Fistula (TEF)
- Congenital anomaly in which esophagus does not fully develop
- Most common: upper esophagus ends in a blind pouch, lower part of esophagus connected to the trachea
- CLINICAL AND SURGICAL EMERGENCY
- Assessment
• Three C’s of TEF
Choking, coughing, cyanosis
• Excess salivation, respiratory distress, aspiration pneumonia
- Plans/interventions
• Pre-op care
Monitor respiratory status
Remove excess secretions (suction all the way to blind pouch)
Elevate infant into anti-reflux position: 30 degrees
Provide oxygen, administer IV fluids as prescribed
MAINTAIN NPO
• Post-op care
MAINTAIN NPO
Administer IV fluids, monitor I/O
Provide g-tube care and feedings
Pacified to meet developmental needs
Monitor for post-op stricture of esophagus (poor feeding, dysphagia, drooling, regurgitating undigested food)
• Promote parent-infant bonding for high-risk infant
Pyloric Stenosis
- Thickening of the pylorus that results in stricture of the gastric outlet
- Result of hypertrophied/spastic muscle fibers surrounding the opening failing to relax sufficiently to allow food to pass easily from the stomach to the duodenum
- Assessment
• Usually in first-born males
• Vomiting (free of bile) around 3-6 weeks old (rarely seen in children >3yrs)
Projectile vomiting within minutes after eating
• Hungry, fretful infant
• Weight loss, failure to gain weight
• Dehydration (decreased sodium and potassium)
• Metabolic alkalosis (decreased serum chloride, increased pH, and bicarbonate or CO2 content)
• Palpable olive-shaped mass in upper-right quadrant of the abdomen
• Visible peristaltic waves
• Children w/ cleft lip/palate and pyloric stenosis BOTH have nursing dx of:
“alteration in nutrition, less than body requirements”
• Cleft lip/palate: decreased ability to suck
• Pyloric stenosis: frequent vomiting
- Plans/interventions
• Pre-op care
Assess for dehydration (administer IV fluids/electrolytes)
Daily weights, monitor I/O
Small, frequent feedings
• Surgery prep (family): hypertrophied wall = surgically corrected to allow proper drainage from the stomach to small intestines (prognosis is excellent)
• Post-op care:
Continuous IV fluids
Small frequent feedings w/ electrolyte solutions or glucose (4-6hrs post-op)
Position on RIGHT side, semi-fowlers after feeding
Burp frequently to avoid stomach distention and avoid pressure on surgical site
Daily weights, I/O
Intussusception
- Telescoping of one part of the intestine into another part of the intestine
• Usually ileum onto the colon (ileocolic)
- Partial/complete bowel obstruction occurs
- Blood vessels – trapped in the telescoping bowels necrosis
- Assessment
• Child <1yr
• Acute, intermittent abdominal pain screaming w/ legs drawn up to abdomen
• Vomiting
• “currant jelly” stools (mixed w/ blood and mucus)
• Sausage-shaped mass in URQ, and LRQ is empty
- Plans/interventions
• Monitor for shock and bowel perforation
• IV fluids as prescribed, monitor I/O
• Prep family for emergency intervention
• Prep child for barium enema
Hydrostatic reduction: 2/3 will respond, if not surgery is necessary
• Post-op care for infants w/ abd. Surgery
- Nutritional needs and fluid electrolyte balance are key problems for children w/ GI disorders
• the younger the child, the more vulnerable they are to fluid/electrolyte imbalances and the greater the need for the caloric intake required for growth
Congenital Aganglionic Megacolon (Hisrchsprung disease)
- congenital absence of autonomic parasympathetic ganglion cells in distal portion of colon and rectum
• lack of peristalsis in the area of the colon where ganglion cells are absent
• fecal contents accumulate above the Aganglionic area of the bowel
- correction: series of surgical procedures
• temporary colostomy until 12 mos
• reanastomosis and closure of the colostomy
- assessment
• suspicion in newborn who fails to pass meconium within 24 hours
• distended abdomen, chronic constipation alternating w/ diarrhea
• nutritionally deficit child
• enterocolitis (occurs as emergency event)
• RIBBON-LIKE stools in the older child
- Plans/interventions
• Pre-op care
Prep for abd. Surgery, Bowel-cleaning program, rectal tube
Observe for bowel perforation: abdominal distention (measure girth), vomiting, increased abdominal tenderness, irritability, dyspnea and cyanosis
Pre-op teaching regarding colostomy
• Post-op:
vitals, axillary temperature
IV fluids/monitor IO
Care for NG tube w/ connection to intermittent suction
Check dressings. Assess bowel sounds and bowel function
• Prep family for home care
Care of temporary colostomy, skin care
Refer to enterostomal therapist and social services
• prep for closure of temporary colostomy: after closure, encourage family to be patient w/ child when toileting (begin toilet training after age of 2)
Hematologic disorders
Iron Deficiency Anemia
- hemoglobin levels below normal range due to inadequate supply, intake, or absorption of iron
- leading hematologic disorder in children
- need for iron greater in children than adults b/c of accelerated growth
- causes of anemia
• inadequate stores during fetal development
• deficient dietary intake
• chronic blood loss
• poor utilization of iron by the body
- assessment
• pallor, paleness of mucus membranes
• tiredness/fatigue
• usually in 6-24 mos during growth spurt, toddlers/adolescent females most affected
• overweight “milky” baby
• dietary intake low in iron, PICA habit
• milk intake greater than 32 oz/day
• Labs: decreased Hgb, low serum ion level, elevated total iron binding capacity (TIBC)
- Hemoglobin norms
• Newborn 12-24
• Infant 10-17
• Child 9.5-15.5
- Plans/interventions
• Support need to limit child’s activity, provide rest periods
• Oral iron (ferrous sulfate) as prescribed
• Teach family about administration of oral iron
Give on empty stomach (better absorption) or w/ citrus juices (vit. C) for increased absorption
Dropper/straw avoid teeth discoloration
Teach stools will become tarry
Can be fatal in severe overdose, keep away from other children
DO NOT GIVE w/ any dairy products
• Teach family about nutritional facts concerning iron deficiency
Limit milk to 32oz/day
Dietary sources of iron: meat, green-leafy veggies, fish, liver, whole grains, legumes, iron-fortified cereal/formula (infants)
• Be aware of family’s income and cultural food preferences
• Refer family to nutritionist and WIC
Hemophilia
- Inherited bleeding disorder: transmitted by an X-linked recessive chromosome
• Mother = carrier, sons may express disease)
- Normal: 50-200% factor activity in the blood
- Hemophiliac: 0-25% activity
- Affected individual usually missing factor VII or IX
- Assessment
• Male child: first red flag prolonged bleeding at umbilical cord or injection site (vitamin K), or after circumcision
• Prolonged bleeding w/ minor trauma
• Hemarthrosis: bleeding into joint spaces (most frequent site of bleeding)
• Spontaneous bleeding into muscles and tissues
• Loss of motion in joints, PAIN
• Labs: prolonged PTT, factor assays <25%
- Plans/interventions
• Administer fresh-frozen plasma, cryoprecipitate of fresh plasma, or lyophilized (freeze-dried) concentrate as prescribed
• Pain meds (analgesics w/ NO ASPIRIN)
• Follow blood precautions, risk for hepatitis
• Child/family home care teaching
Recognize early signs of bleeding into joints
Local tx for minor bleeds (pressure, splinting, ice)
Admin of factor replacement routine tx of clotting factors (port-a-cath)
Dental hygiene: soft toothbrushes
Protective care: soft toys, padded bed rails
Medic-Alert ID
• refer to genetic counseling
• support during periods of growth and development where bleeding may occur
learning to walk, losing teeth
- inherited bleeding disorders (hemophilia/sickle cell) often used to test knowledge of genetic transmission patters
• autosomal recessive BOTH parents must be heterozygous or carriers of the recessive trait for the disease to be expressed
each pregnancy: 25% chance that infant will have the disease
ex: sickle cell, CF, and PKU
• x-linked recessive trait is carried on the X chromosome so it usually affects male offspring
each pregnancy: the woman who is a carrier, 25% chance
• if the child is a male, he has a 50% chance of having it
• if the child is female, she has 50% chance of being a carrier
ex: hemophilia
Sickle cell disease
- genetic disorder that results in the formation of abnormal Hgb chains
<1% African American newborns, 8% of A. Americans carry the gene
- also affects: Indians, Mediterranean, and middle Easters
- usually appears after 6mos.
- Hemoglobin S (Hgb S) replaces all or part of the normal Hgb causes RBC to sickle when O2 is released into the tissues
• Sickled cells CANNOT flow thru capillary beds
• Dehydration promotes sickling
Hydration is very important in the tx of sickle cell disease. It promotes hemodilution and circulation of red cells thru blood vessels
• Increased sickling episodes occur w/ cold causes constriction of the vessels
- HgbS less-than normal life span (<40 days) chronic anemia
- Tissue ischemia widespread pathologic changes in spleen, liver, kidney, bones, and CNS
- Important terms
• HgbAS: Heterozygous gene – sickle cell trait
• HbSS: homozygous gene – sickle cell disease
• HgbS: abnormal hemoglobin – disease and trait
- Assessment
• African American descent, usually over 6mos. Of age
• Parent w/ trait or disease
• Labs: Hgb electrophoresis (differentiates trait from disease)
• Frequent infections (nonfunctional spleen)
• Tiredness, chronic hemolytic anemia
• Delayed physical growth
• Vasoocclussive crisis (classic signs)
Fever, severe abdominal pain, hand-foot syndrome (infants – painful edematous hands/feet), arthralgia
• Leg ulcers (adolescents)
• Cerebrovascular accidents (increased risk w/ dehydration)
- Plans/interventions
• Teach family to prevent crisis (hypoxia)
Keep child away from strenuous exercise, high altitudes, infection (seek care at first sign of infection)
Prophylactic PCN
Maintain hydration, DO NOT withhold fluids at night b/c enuresis is a complication of both the disease and TX
• Hospitalized child w/ Vasoocclussive crisis
IV fluids (1-2 times TFM) and electrolytes (increase hydration, treat acidosis)
Monitor I/O,
Administer blood precuts, analgesics (parenteral morphine – severe pain), AB
Warm compresses (not ice)
• Pneumococcal vaccine, meningococcal vaccine, and Hib vaccine
• Hep B vaccine for child at risk b/c of transfusions
• Refer to genetic counselor
• Support to child/family (chronic disease)
- Supplemental iron is NOT given to clients w/ sickle cell disease b/c anemia is not caused by iron deficiency. INSTEAD, folic acid is given to orally stimulate RBC synthesis
Acute Lymphocytic Leukemia
- Cancer of the blood-forming organs
- 80% of childhood leukemia
- Noted for presence of lymphoblasts (immature lymphocytes) which replaces normal cells in the bone marrow (also seen in the peripheral blood)
- Classification according to whether it involves T vs B lymphocytes vs null cells
• Null – neither T or B (75% - best prognosis)
- s/s of leukemia replacement of normal cells by leukemic cells in the bone marrow and extramedullary stress
- treatment has four phases (I, S, C, M)
• induction, sanctuary, consolidation, and maintenance
- assessment
• pallor, tiredness, weakness, lethargy (due to anemia)
• petechia, bleeding, bruising (due to thrombocytopenia)
• infection, fever (due to neutropenia)
• enlarged lymph nodes (hepatosplenomegaly)
• headache and vomiting (signs of CNS involvement)
• anorexia, weight loss
• labs: bone marrow aspiration shows 80-90% immature blast cells
- plans/interventions
• recommend private room and reverse isolation (if prescribed)
• age-appropriate explanations of diagnostic tests, tx, and nursing care
• examine child for infection of skin, needle-stick site, and dental problems
• administer blood products, antineoplastic chemo as prescribed
• monitor for side effects of chemo
Vincristine (induction
L-asparaginase (induction)
• Have epinephrine and oxygen readily available to treat anaphylaxis when administering L-asparaginase
Methotrexate (sanctuary and maintenance)
Mercaptopurine (6-MP) (maintenance)
• Provide care directed toward managing side-effects and toxic effects of antineoplastic agents (Anti-emetics, monitor fluid balance, monitor for signs of infection/bleeding, monitor for cumulative toxic effects of drugs – hepatic/cardiac/renal and neuro toxicity)
Provide oral hygiene
Small, appealing meals (increase calories and protein) refer to nutritionist
Promote self-esteem and (+) body image
• Alopecia, severe weight loss
Provide care to prevent infection
• Emotional support for family in crisis encourage family/child input and control in determining plans and tx
- Prednisone is frequently used in combo w/ antineoplastic drugs to reduce mitosis of lymphocytes
- Allopurinol (xanthine oxidase inhibitor) also administered to prevent renal damage due to uric acid buildup and cellular lysis
Metabolic and Endocrine Disorders
Congenital Hypothyroidism
- Congenital condition resulting from inadequate thyroid tissue development in utero. Cognitive impairment and growth failure occur if not detected and treated in early infancy
- Assessment
• Newborn screening = low t4 (thyroxine) and high thyroid stimulating hormone (TSH)
• Symptoms in newborn
Long gestation (>42 weeks)
Large hypoactive infant, delayed meconium passage
Feeding problems (poor sucks)
Prolonged physiologic jaundice
Hypothermia
• Symptoms in early infancy if untreated w. thyroxine
Large, protruding tonge
Coarse hair, low hairline
Lethargy, sleepiness, flat expression
Constipation and hypotonia
Delay of serum phenylalanine testing will lead to CNS damage
• Mental retardation
- Prognosis is good if the condition is recognized and treated infant’s intelligence usually not affected if tx is initiated within first month of life
- Plans/interventions
• Newborn screening prior to discharge
• Assess newborn for signs of congenital hypothyroidism
Once identified, teach family about replacement therapy for thyroid hormone
• Lifelong therapy, single dose in the morning
• Check pulse before giving medication
• Signs of overdose: rapid pulse, irritability, fever, weight loss, diarrhea
• Signs of under dose: lethargy, fatigue, constipation, poor feeding
• Periodic thyroid testing necessary
Phenylketonuria (PKU)
- rare autosomal-recessive disorder in which the body cannot metabolize the essential amino acid phenylalanine – which accumulates in the blood after the infant begins consuming breast milk or formula
- usually detected thru early newborn screenings 24 hours after the infant’s firs ingested mean and subsequent tests 2-3 weeks after birth
- individuals diagnoses w/ PKU must limit their intake pf phenylalanine containing foods throughout their lives
- assessment (if undetected and/or untreated)
• newborn screening – Guthrie test; positive result; serum phenylalanine level of 4mg/Dl
• frequent vomiting, failure to gain weight, irritability, musty odor of urine, peculiar B.O.
• delayed growth and development, FTT
• often fair-skinned blonde and blue-eyed children
• may have microcephaly
• mothers w/ PKU who DO NOT maintain a low-phenylalanine diet during pregnancy can cause problems for their children who DO inherit PKU – infants at risk for:
cognitive impairment, microcephaly, birth weight <2500g, disrupted growth and development, and congenital heart anomalies
- early detection of PKU and hypothyroidism is ESSENTIAL in preventing cognitive impairment in infants. Knowledge of normal growth and developmental patterns is important because lack of attainment can be used to detect the presence of disease, evaluate treatment’s effects
- plans/interventions
• perform newborn screening as close to discharge as possible and no later than 7 days after birth (subsequent sample no later than 2 weeks if initial specimen <24 hrs)
screen infants born at home/no hospital contact and adopted babies
• refer to genetic counseling
• dietary management: low-phenylalanine diet
avoid high-protein foods (meat, milk, dairy, and eggs
low-p foods: veggies, fruit juices, cereals, breads, and starches
provide special formula for infant: Lofenalac, Phenex-1
encourage family to work w/ nutritionist
diet must be maintained at least until brain growth is complete (6-8yrs)
• limit cognitive defects
- nutra-sweet (aspartame) contains phenylalanine and therefore should NOT be given to a child w/ PKU
insulin-dependent diabetes mellitus (diabetes type-1)
- metabolic disorder in which the insulin-producing cells of the pancreas are nonfunctioning as a result of some insult
• hereditary, viral infections and autoimmune processes are implicated in DM
• causes altered metabolism of carbs, proteins, and fats (macros)
• insulin replacement, dietary management, and exercise = treatment
- assessment
• classic 3 P’s
polyphagia, polydipsia, and polyuria (enuresis in previously continent child)
• irritability, fatigue, weight loss
• abdominal complaints, nausea, and vomiting
• usually in school-age children, can occur in infancy
- plans/interventions
• assist w/ dx: fasting blood sugar >120mg/dL
• if child is in ketoacidosis care for seriously ill child (may be unconscious)
monitor vitals, neuro status, blood glucose, pH, and serum electrolytes
administer regular insulin IV in normal saline (as prescribed)
administer IV fluids and electrolytes
assess hydration, maintain strict I/O
• initiate home teaching program ASAP
Teach insulin admin.
• Child usually receives multiple doses/day (Subq or via pump)
Dietary management (carb counting is preferred)
• Meals and snack
• Growth and exercise needs
o Regular, planned activities
o Snacks before or during exercise
• Four basic food groups, NO CONCENTRATED SWEETS
• Advice from nutritionist
Home glucose monitoring/testing
s/s of hyperglycemia and hypoglycemia
sick-day management
ensure parent involves school nurse/day care
• initiate program for school-age child as appropriate
ID issues specific to school (=
• PE class/exercise, scheduled times for meals and snacks, cooperation w/ school staff, need to be like peers
Teach that school-age child should be responsible for most management
Medic-Alert bracelet
- There has been an increase in the number of children diagnosed w/ diabetes TYPE 2. the increasing rate of childhood obesity is thought to be a contributing factor as well as lack of physical activity and family hx.
Skeletal Disorders
Fractures
- Traumatic injury to the bone (younger children may be at risk for child abuse)
- Incident must match the injury/sound plausible
- Fractures classified according to type
• Complete: bone fragments completely separate
• Incomplete: bone fragments remain attached (greenstick, bend, buckle)
• Comminuted: bone fragments from the shaft break free and lie in surrounding tissue (RARE IN CHILDREN)
• Spiral: fracture line results from twisting force, forms a spiral encircling the bone
May be related to child abuse
- Fractures occurring in the epiphyseal/growth plate may affect growth of the limb
- Fractures are common in older children b/c they fall during play and are involved in motor vehicle accidents
- Assessment (general condition)
• Visible bone fragments, misalignment of the limb, pain, and swelling
• Contusions, child guarding/protecting extremity, limited ROM
• Possible use of fractured extremity due to intact periosteum
• 5 P’S of possible ischemia (compartment syndrome)
PAIN, PALLOR, PULSELESSNESS, PARESTHESIA, PARALYSIS
• Plans/interventions
Obtain baseline date and frequently perform neurovascular assessment
• Pulses: DISTAL to injury (for circulation)
• Color: pink, brisk, cap refill
• Movement and sensation: nerve impairment, compare symmetry
• Temperature: check extremity for warmth
• Pain: monitor for severe pain NOT relieved by analgesics
• Newly fractured sites splinted/braced until swelling subsides
• Cast applied to affected extremity
Report abnormal assessment promptly! Compartment syndrome may occur permanent damage to the nerves and vasculature of the injured extremity due to compression
Compromised circulation w/ abnormal neurovascular checks are a result of compartment syndrome: progressive decrease of tissue perfusion as a result of increased pressure from edema/swelling pressing on tissue/vessels
Maintain traction (if prescribed) – note bed position, type of traction, weights, pulleys, pins, pin sites, adhesive strips, ace wraps, splints, and casts
Pin sites can be a source of infection. Monitor for signs of infection. Cleanse/dress pin sites as prescribed
When moving the client in bed w/ traction, it is necessary for someone to hold and move weights of the traction as the client changes position to avoid additional tension on the traction and fracture sites
• Skin traction: force applied to skin
o Buck extension traction: lower extremity, legs extended, no hip flexion
o Dunlop traction: two lines of pull on the arm
o Russel traction: two lines of pull on the lower extremity
One perpendicular, one longitudinal
o Bryant traction: both lower extremities flexed 90 degrees at hip (rarely used b/c extreme elevation of lower extremities decreased peripheral circulation)
• Skeletal traction: pin/wire applies pull directly to the distal bone fragment
o 90 degree traction: 90 degree flexion of hip and knee; lower extremity is in a boot cast, can also be used on upper extremities
o Dunlop traction: may be used as skeletal traction
Maintain child in proper body alignment, restrain if necessary
Monitor for problems of immobility
Provide age-appropriate play/toys
Prepare child for cast application (age-appropriate terms)
Provide routine cast care after application; petal case edges
Teach home cast care to family
• Neurovascular assessment of casted extremity
• DO NOT get cast wet
• Hip spica: family may use a Bardford frame under a small child to help w/ toileting, they must NOT use abduction bar to turn child
• Teach to seek follow-up care w/ HCP
- Skeletal disorders affect the infant’s/child’s physical mobility and typical NCLEX-RN questions focus on appropriate toys/activities for the child who is confined to bed rest/immobilized
Developmental Dysplasia of Hip (DDH)
- Abnormal development of the femoral head in the acetabulum (usually dx at birth)
- Contributing factors:
• Breech position in utero
• Family hx of DDH
• Oligohydramnios
- Assessment
• Infant
Positive Ortolani sign: “clicking” w/ abduction heard when HCP maneuvers the femoral head and it slips back into the acetabulum
Positive Barlow maneuver: “feel” the dislocation as the femur leaves the acetabulum when the HCP adducts and extends the hips while stabilizing the pelvis
• Older child
Limp on affected side, Trendelenburg sign (abnormal gait)
- Plans/interventions
• Newborn assessment at birth
• Apply abduction device/splint as prescribed
Pavlik Harness, Frejka, or von Rosen splint)
Therapy: positioning legs in flexed abducted position
• Teach parents home care
Application/removal of device (worn 24hrs daily)
Teach diapering
Follow-up care: frequent adjustments due to growth
• Teach how to provide care for infant in Bryant traction (used if splinting is ineffective)
Maintain hips in 90 degree flexion, elevate buttocks off bed
Monitor circulation to feet
Meet developmental needs of immobilized infant, incorporate family care
Prepare family for spica cast application
• Provide care for child requiring surgical correction
Pre-op teaching, including cast application
Post-op care
• Assess vitals, check cast for drainage and bleeding
• Perform neurovascular assessment of extremities
• Promote respiratory hygient
• Administer narcotic analgesics or morphine (IV or IM)
• Teach family cast care when child gets home, check for “hot spots” possible indicators of infection
- Children do not like injections and will deny pain to avoid “shots”
Scoliosis
- Lateral curvature of the spine that usually occurs during rapid growth spurs in adolescents
- Hereditary conditions, neuromuscular diseases, congenital spinal defects, trauma/infections to the spine may factor in to the development of scoliosis
- Treatment depends on the curvature of the spine
- Assessment
• Occurs most commonly in adolescent females (10-15yrs)
• Elevated shoulder/hip. Head and hips not aligned.
• Child bends forward rib hump apparent
Ask child to bend forward from the hips w/ arms hanging free. Examine child for a curve of the spine, rib hump, and hip asymmetry
- Plans/interventions
• Screen all adolescent children especially females during growth spurt
• Prep child/family for conservative tx such as the use of a brace
A brace does not correct the spine’s curve in a child w/ scoliosis, it only stops or slows the progression
Teach brace application (Boston, Wilmington, and Milwaukee)
Wear 23 hours a day
Wear t-shirt under brace to decrease skin irritation
Check skin for areas of irritation or break down
Suggest clothing modifications to camouflage brace
Reinforce prescribed exercise regimen for back and abdominal muscles
Plan ways to improve self-concept w/ the adolescent
Teach family severe, untreated scoliosis can cause respiratory difficulty
• Prep child/family for surgical correction if required
Log-rolling technique (2+ people, move client on draw sheet and turn)
Practice respiratory hygiene
Orient to ICU
Discuss post-op tubes (foley, NG tube, and chest tube)
Describe post-op pain management (PCA may be used)
Obtain baseline neuro assessment
• Provide post-op care
Perform frequent neuro assessments
Log-roll for 5 days
Administer IV fluids/analgesics
Client is NPO, provide oral hygiene
Monitor NG tube and bowel sounds
Assist w/ ambulation, provide body jacket, progressively ambulate
Teach child and family that body jacket will be born for several months until the bone fusion is stable
Determine need for a teacher in the home
Encourage child’s participation in care to promote self-esteem
Juvenile Arthritis (JA) or Juvenile Idiopathic Arthritis (JIA)
- Chronic inflammatory disorder of the join synovium. Considered to be one of the most common rheumatoid conditions occurring in children <17.
- JIA diagnosed when client presents w/ following symptoms for a minimum of 6 weeks
• Continuous arthritic pain in single or multiple joints
• Repetitive fevers: 39.44 C/103 F.
• Systemic indications: pinkish/reddish rash on the legs, arms, and trunk
• Exact cause: unknown, child’s immune system attacks synovial lining of joints
- Assessment
• Joint swelling/stiffness usually large joints
• Painful joints
• Generalized symptoms: fever malaise, and rash
• Periods of exacerbations and remissions
• Verifying severity: mild and self-limited or severe and disabling
• Labs: latex fixation test (usually negative), elevated ESR
• Poorest prognosis
Positive rheumatoid factor
Polyarticular systemic onset
- Plans/interventions
• Plan home program of prescribed exercise, splinting and activity
• Assist in identifying adaptations in routine (Velcro fasteners, frequent rest periods)
• Support the maintaining of school schedule and activities appropriate for age
• Medication regiment: combination drugs are used
NSAIDS (aspiring, tolmetin sodium, ibuprofen, naproxen)
Antirhumatic drugs
Corticosteroids (prednisone)
• Often-used in short-term or low doses during exacerbations. Long-term use is avoided due to side effects and adverse effects on growth
Cytotoxic drugs (cyclophosphamide, methotrexate)
• Teach the child/family about side effects and toxic effects of prescribed drugs
• Inform child/family that optimum inflammatory effects of drugs may take a month
• Encourage periodic eye exams for early detection of iris inflammation (iridocyclitis) to prevent vision loss
• Encourage family to allow child’s independence
-
[Show More]
Last updated: 3 years ago
Preview 1 out of 52 pages
Buy Now
Instant download
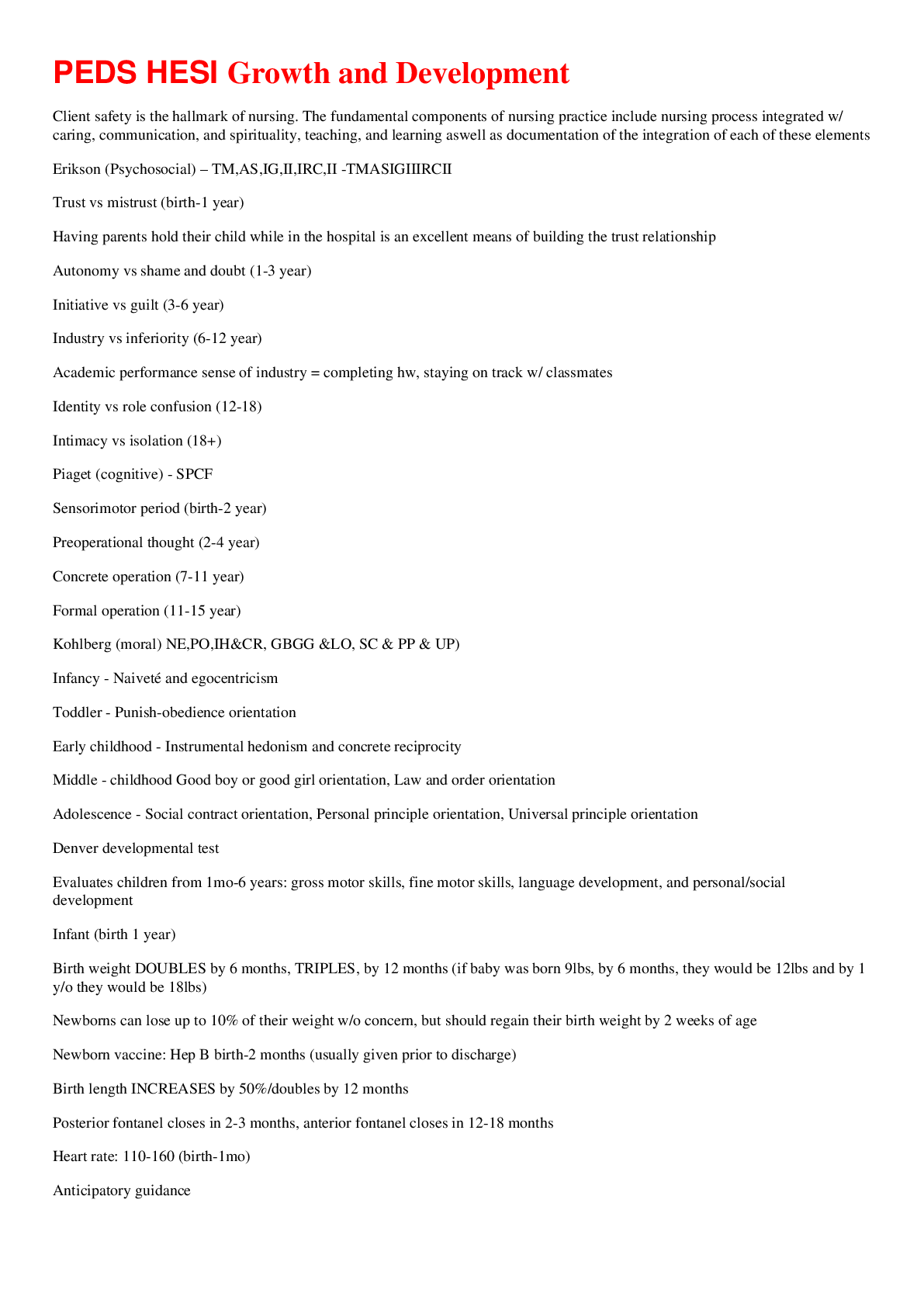
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$15.00
Can't find what you want? Try our AI powered Search
79
0
Document information
Connected school, study & course
About the document
Uploaded On
Feb 25, 2021
Number of pages
52
Written in
All
Seller

Reviews Received
24
3
3
0
5
Additional information
This document has been written for:
Uploaded
Feb 25, 2021
Downloads
0
Views
79


.png)


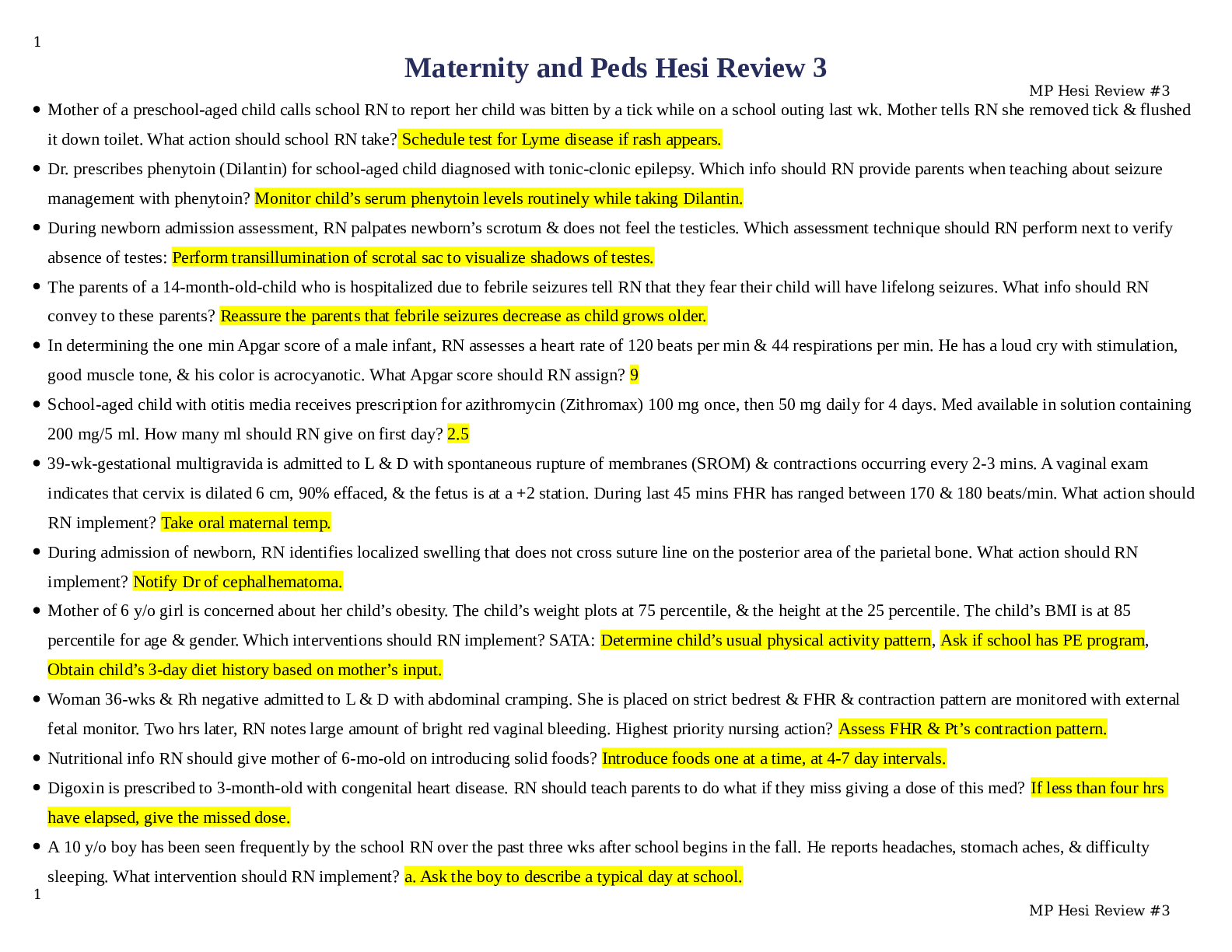

.png)