PN3-EXAM2-Final
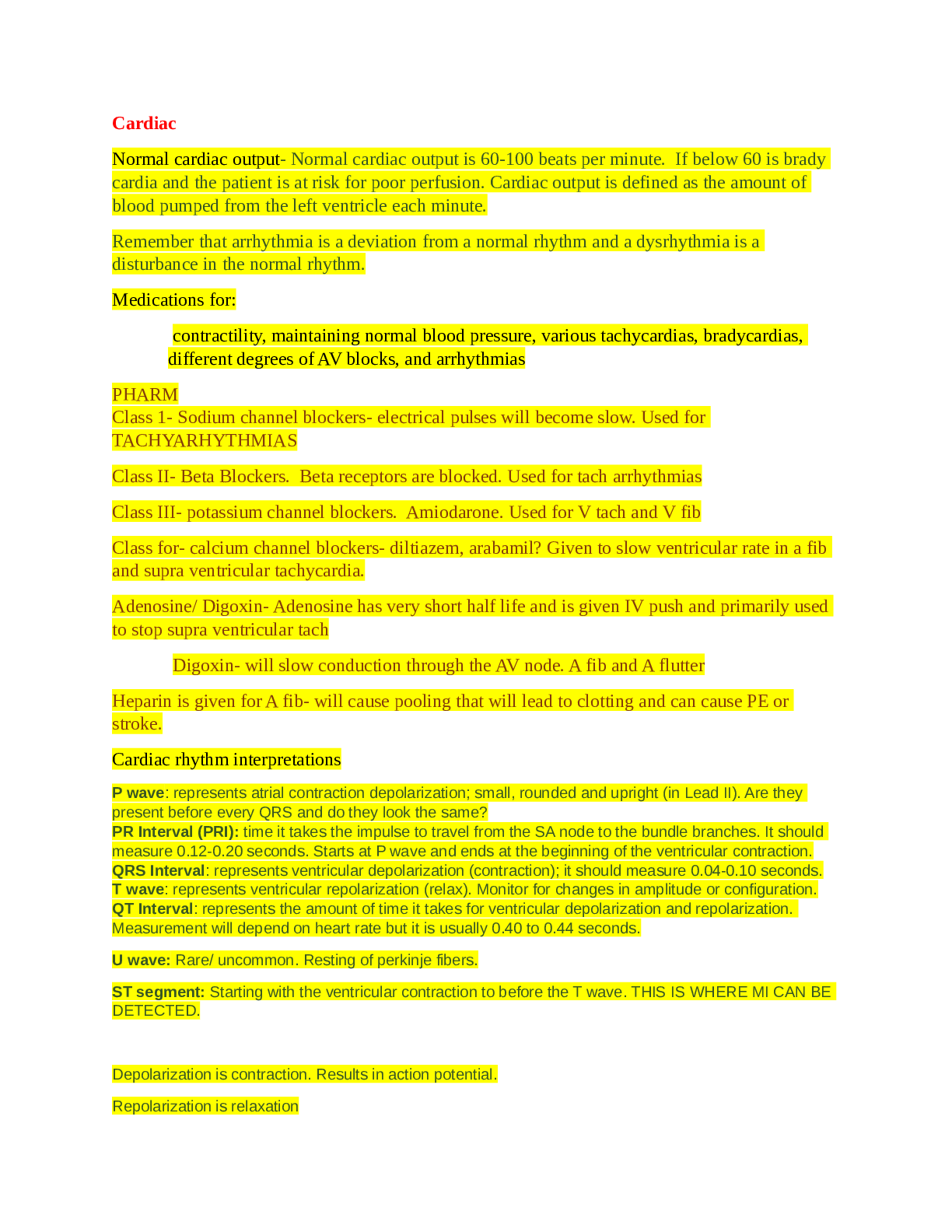
Cardiac
Normal cardiac output- Normal cardiac output is 60-100 beats per minute. If below 60 is brady cardia and the patient is at risk for poor perfusion. Cardiac output is defined as the amount of bl
...
PN3-EXAM2-Final
Cardiac
Normal cardiac output- Normal cardiac output is 60-100 beats per minute. If below 60 is brady cardia and the patient is at risk for poor perfusion. Cardiac output is defined as the amount of blood pumped from the left ventricle each minute.
Remember that arrhythmia is a deviation from a normal rhythm and a dysrhythmia is a disturbance in the normal rhythm.
Medications for:
contractility, maintaining normal blood pressure, various tachycardias, bradycardias, different degrees of AV blocks, and arrhythmias
PHARM
Class 1- Sodium channel blockers- electrical pulses will become slow. Used for TACHYARHYTHMIAS
Class II- Beta Blockers. Beta receptors are blocked. Used for tach arrhythmias
Class III- potassium channel blockers. Amiodarone. Used for V tach and V fib
Class for- calcium channel blockers- diltiazem, arabamil? Given to slow ventricular rate in a fib and supra ventricular tachycardia.
Adenosine/ Digoxin- Adenosine has very short half life and is given IV push and primarily used to stop supra ventricular tach
Digoxin- will slow conduction through the AV node. A fib and A flutter
Heparin is given for A fib- will cause pooling that will lead to clotting and can cause PE or stroke.
Cardiac rhythm interpretations
P wave: represents atrial contraction depolarization; small, rounded and upright (in Lead II). Are they present before every QRS and do they look the same?
PR Interval (PRI): time it takes the impulse to travel from the SA node to the bundle branches. It should measure 0.12-0.20 seconds. Starts at P wave and ends at the beginning of the ventricular contraction.
QRS Interval: represents ventricular depolarization (contraction); it should measure 0.04-0.10 seconds.
T wave: represents ventricular repolarization (relax). Monitor for changes in amplitude or configuration.
QT Interval: represents the amount of time it takes for ventricular depolarization and repolarization. Measurement will depend on heart rate but it is usually 0.40 to 0.44 seconds.
U wave: Rare/ uncommon. Resting of perkinje fibers.
ST segment: Starting with the ventricular contraction to before the T wave. THIS IS WHERE MI CAN BE DETECTED.
Depolarization is contraction. Results in action potential.
Repolarization is relaxation
If AV conduction is not normal will see cardiac block.
Steps for Dysrhythmia Interpretation:
• Step 1: Determine rate
• Step 2: Determine regularity
• Step 3: Determine P waves
• Step 4: Determine PR interval (measurement)
• Step 5: Determine QRS interval (measurement)
• Step 6: Determine QT interval (measurement)
PLEASE SEE NOTES… TRIED TO EXPLAIN BUT IT WAS DIFFICULT.
6 Seconds = 30 small squares. Count for atrial or ventricular rate is to count 30 large squares (P Wave for Atrium contraction) (R wave for ventricular waves).
Example:
If four squares are counted in P wave then take 4x10= 40 and will give atrial rate.
External vs internal pacemaker- EXTERNAL is done in EMERGENT situations!! Is used until permanent pacemaker can be placed.
Internal pacemaker is either synchronous (demand) or asynchronous (fixed rate)
When a pacing stimulus is delivered to the heart, a spike (or pacemaker artifact) is seen on the monitor or ECG strip. The spike should be followed by evidence of depolarization (i.e., a P wave, indicating atrial depolarization, or a QRS complex, indicating ventricular depolarization). This pattern is referred to as capture, indicating that the pacemaker has successfully depolarized, or captured, the chamber.
Avoid placing ECG over pacemaker.
Activity of pacemaker as seen on ECG- When a pacing stimulus is delivered to the heart, a spike (or pacemaker artifact) is seen on the monitor or ECG strip. The spike should be followed by evidence of depolarization (i.e., a P wave, indicating atrial depolarization, or a QRS complex, indicating ventricular depolarization). This pattern is referred to as capture, indicating that the pacemaker has successfully depolarized, or captured, the chamber.
Avoid placing ECG over pacemaker.
Teaching for pt with arrhythmia – Causes of arrhythmias- result in a malfunction of the cardiac muscle. Some are common and benign. Other are very life threatening. Mechanisms- look at the conduction system. Heart block or reentry- reentry will usually cause tachycardia. The SA node is giving off the wrong amount. Some other causes are medication or electrolyte imbalances, dig toxicity, hypoxemia or myocardial infarction. Normal sinus rhythm- this is the overall goal of treatment. ATROPINE SULFATE is the drug of choice for bradycardia- it will increase the heart rate. It should only be used SHORT TERM!!! For tachycardia will look for pain, fever and exertion. Watch for stimulants, caffeine and nicotine- will increase heart rate.
Important to teach heart rate. Need to teach manually and to teach how to count quick/ fast beats.
Anthrax Teaching
Placed into grouping of how dangerous, and public panic. An investigation will be started to identify the agent and medical treatment. Greatest biochemical threat. Can be cutaneous (spores- direct contact), inhaled or GI (contaminated meat).Standard precautions can be used. CIPRO IV- post exposure is oral CIPRO. Health care workers will take as well.
Emotional care for clients after traumatic event- Need to keep patient calm and remove self emotionally. Nurses play an important role in helping the patient and need to encourage the patient to talk about event when they are ready!!! PTSD is normal and should subside within days and resolve in 30 days. Treated with psychotherapy and should be referred to someone who specializes in trauma. Need to monitor for suicidal tendencies. Give SSRI for treatment. Also need to help those who are not directly injured but are worried.
Chemical Spills- - All nurses are required to help patients that have been exposed to chemical. Need to wear specific PPE. Nurse cannot help if they are injured from the item that is exposed to the patient. Need to have designated area for exposure. There are rooms for small events or large events. Negative pressure air or filters to remove particles from the air. Outdoor areas are used or small or medium events.
--ECG strip complications
Any repetitive movement will cause artifact and could lead to inaccurate interpretation of the ECG.
For continuous ECG monitoring, the electrodes are not placed on the limbs because movement of the extremities causes “noise,” or motion artifact, on the ECG signal.
Electrode should not be placed on dry skin, the gel on each electrode must be moist and fresh, the contact site should be free of any lotion, tincture, or other substance that increases skin impedance. Electrodes cannot be placed on irritated skin or over scar tissue.
Artifacts are an interference seen on the monitor or rhythm stirp, which may look like a wandering or fuzzy baseline. These complications can be caused by patient movement, loose defective electrodes, improper grounding, or faulty ECG equipment such as broken wires or cables. Some artifacts can mimic lethal dysrhythmias such as ventricular tachycardia (with toothbrushing) or ventricular fibrillation (with tapping on the electrode).
ECG purpose and normal findings
An ECG provides a graphic representation, or picture, of cardiac electrical activity.
Electrodes, consisting of a conductive gel on an adhesive pad, are placed on specific sites on the body and attached to cables connected to an ECG machine or to a monitor.
Normal sinus rhythm (NSR) is the rhythm originating from the sinoatrial (SA) node (dominant pacemaker) that meets ECG criteria.
Both atrial and ventricular rhythms should be essentially regular (a slight variation in rhythm is normal).
Rate: Atrial and ventricular rates of 60 to 100 beats/min
Rhythm: Atrial and ventricular rhythms regular
P waves: Present, consistent configuration, one P wave before each QRS complex
PR interval: 0.12 to 0.20 seconds and constant
QRS duration: 0.04 to 0.10 seconds and constant
Pulseless 5 T’s and 5 H’s
Ventricular fibrillation: Chaotic firing in the ventricle. Patient is not producing any cardiac output.
Top 3 causes: MI, potassium imbalance, or a drug toxicity
In the absence of electrical activity, there is no pulse or cardiac output. The rhythm strip will look like a wavy line.
Healthcare providers want to confirm that the wavy line is not caused by any other reason (such as a loose lead or machine not hooked up correctly) because it is an extremely emergent situation.
5 T’s and 5 H’s: These will help a healthcare provider remember the potential cause for the pulseless electrical activity.
Hypovolemia
Hypoxia
Hydrogen ion – patient is in acidosis
Hyper- OR hypo- kalemia
Hypothermia
Tablets (drug overdose or ingestion)
Tamponade (cardiac)
Tension pneumothorax
Thrombosis coronary
Thrombosis pulmonary
(The two thrombi’s will depend on where it originates from)
Safe use of defibrillator
Defibrillation: Electrical shock to the heart
Completely depolarizes the cardiac cells in an effort to terminate V-fib (usually when you see defibrillation)
Special pads and paddles and put them onto the body accordingly (MAKE SURE YOU CLEAR THE BODY BEFORE you shock the patient)
Most vital intervention: V-fib and V-tach (without a pulse)
Other important reminders: Cables and connectors cannot be broken, stand clear, cannot be wet, do not place electrodes over a pacemaker or any other monitoring electrodes (such as from an EKG machine if a patient has one)
Anatomy of heart:
SA node, AV node, Purkinje fibers
SA node is located in the right atrium. The SA node is the personal (primary) pacemaker.
The electrical impulse starts at the atrium (SA node) and travels down to the AV node (ventricle) – the AV node causes a small pause. The AV node acts as a secondary pacemaker. Once the impulse has traveled through, it goes down into the bundle of his. From the bundle of his, the impulse then goes down into left and right and into the purkinje fibers. (Left and right side of the heart).
SA node: 60 to 100 BPM
AV node: 40-60 BPM
The impulse is then spread throughout the ventricles. The Purkinje fibers are known as the backup THIRD pacemaker.
These three things are known as the conduction system and what make up one heartbeat.
Triage
Fractured rib teachings
Splinting reduces breathing depth and clearance of secretions.
Management of uncomplicated rib fractures is simple because the fractured ribs reunite spontaneously. The chest is usually not splinted by tape or other materials.
The main focus is to decrease pain so adequate gas exchange is maintained. An intercostal nerve block may be used if pain is severe. Analgesics that cause respiratory depression are avoided.
How ER ranks clients
Emergent (life threatening): Category that implies that a condition exists that poses an immediate threat to life or limb.
Examples: Respiratory distress, chest pain with diaphoresis, stroke, active hemorrhage, unstable vital signs
Urgent (needs quick treatment, but not immediately life threatening): Indicates that these patients should be treated quickly but that an immediate threat to life does not exist at the moment
Examples: Severe abdominal pain, renal colic, displaced or multiple fractures, complex or multiple soft tissue injuries, new-onset respiratory infection (especially pneumonia in older adults)
Nonurgent (could wait several hours if needed without fear of deterioration):
Examples: skin rash, strains and sprains, “colds” and simple fractures
Ideal triage nurse
The triage nurse is the gatekeeper in the emergency care system.
The triage nurse requires appropriate training and experience in both emergency nursing and triage decision-making concepts to develop an expert knowledge base and provide ongoing mentoring and quality improvement feedback.
Color codes of mass casualty event
Emergent (class I) patients are identified with a red tag, indicating immediate threats to life.
Patients who can wait a short time for care (class II) are marked with a yellow tag, indicating major injuries that need treatment within a 30-minute to 2-hour time frame.
Nonurgent or “walking wounded” (class III) patients are given a green tag, indicating minor injuries that can be managed in a delayed fashion, generally more than 2 hours.
Patients who are expected to die or are dead are issued a black tag (class IV).
Mass vs. traditional triage
Mass: Most mass casualty response teams in the field (at the disaster site) and in the hospital setting use a disaster triage tag system that categorizes triage priority by color and number. Triage under mass casualty conditions consists of labeling patients by emergent or class I (red tag), urgent or class II (yellow tag), nonurgent or class III (green tag), or expectant or class IV (black tag).
Traditional: Practiced during usual emergency operations. Triage under usual conditions consists of labeling patients by emergent, urgent, and nonurgent.
Burns
1st vs 2nd vs 3rd vs 4th degree burns
Burn wounds are classified as:
• 1st - superficial-thickness wounds
Result in the least damage because the epidermis is the only part of the skin that is injured
Erythema, blanching on pressure, pain, mild swelling, no blistering
• 2nd - partial-thickness wounds
Involves the entire epidermis and varying depths of the dermis
Depending on the amount of dermal tissue damaged, partial-thickness wounds are further subdivided into superficial partial-thickness and deep partial-thickness injuries
• Superficial partial-thickness: increase pain sensation. Nerve endings are exposed, and any stimulation (touch or temperature change) causes intense pain.
• Deep partial-thickness injuries: extend deeper into the skin dermis, and fewer healthy cells remain. Blisters usually do not form because the dead tissue layer is thick, sticks to the underlying dermis, and does not readily lift off the surface.
Fluid-filled vesicles that are red, shiny, severe pain caused by nerve injury. Mild to moderate edema
• 3rd - full-thickness wounds
Involves destruction of the entire epidermis and dermis, leaving no true skin cells to repopulate; therefore, skin will not regrow
All full-thickness burns need early excision and grafting
• 4th - deep full-thickness wounds
Extend beyond the skin and damage muscle, bone, and tendons. These burns occur with flame, electrical, or chemical injuries. The wound is blackened and depressed, and sensation is completely absent
All full-thickness burns need early excision and grafting
Periods of burn treatment??
Emergent vs acute phase of treatment
Emergent
*24-48 hours, can be 72 hours- airway, fluid management, wound care
Immediate care focuses on maintaining an open airway, ensuring adequate breathing and circulation, limiting the extent of injury, and maintaining the function of vital organs.
Assess the burn patient’s airway and adequacy of breathing before assessing any other body system
Nonsurgical interventions include airway maintenance, promotion of ventilation, monitoring gas exchange, oxygen therapy, drug therapy, positioning, and deep breathing.
Hypovolemia shock is a common cause of death in the resuscitation phase in patients with serious injuries
Keep an endotracheal kit or tracheostomy kit at the bedside of any patient with facial burns, burns inside the mouth, singed nasal hairs, or a “smoky” smell to the breath
Check ventilator alarms hourly for patients who are receiving paralytic drugs during mechanical ventilation
Notify the physician immediately if the patient with an inhalation injury becomes more breathless or audible wheezes disappear
When signs of pulmonary edema are present, elevate the head of the bed to at least 45 degrees, apply oxygen and facilitate immediate intubation
Use strict aseptic technique when caring for patients who have open burn wounds.
Notes:
Environment needs to be controlled, warmer than usual, remained at 80-85 degree temp., cover patient with sheets and or warm blankets to help keep heat in
Circulation checks every 15 min!
Escarotomy- incision through middle of the burn in the escar tissue (allows breathing room, allows circulation, allows nerve ending decreased pressure to reduce more damage
Acute
The acute phase of burn injury begins about 36 to 48 hours after injury, when the fluid shift resolves, and lasts until wound closure is complete.
During this phase, the nurse coordinates interprofessional care that is directed toward continued assessment and maintenance of the cardiovascular and respiratory systems, as well as toward GI and NUTRITION status, burn wound care, pain control, and psychosocial interventions.
Monitor for any renal disease or heart failure
Goals-
Prevent infection
Minimize pain
Burn treatments, meds, and teachings to community/families
Community/family teachings
Teach all people to use home smoke detectors and carbon monoxide detectors, and to ensure that the detectors are in good working order.
Teach people to reduce the risk for house fires by never smoking in bed, avoiding smoking when drinking alcohol or taking drugs that induce sleep, and keeping matches or lighters out of the reach of children or anyone who is cognitively impaired.
Teach all people to assess how hot the water is before bathing, showering, or immersing a body part in it.
Instruct patients who have reduced sensation in hands or feet to use a bath thermometer to check water temperature before bathing.
Teach patients to avoid exposing burned skin to the sun or to temperature extremes.
If space heaters must be used, stress the importance of keeping clothing, bedding, and other flammable objects away from them.
Remind people to keep the screens and doors closed on the fronts of fireplaces and to have chimneys swept each year to prevent creosote buildup.
Burn Treatments
Grafting: Areas of the wound not closed by wound contraction will require grafting
Debridement: remove all the devitalized tissue from the wound bed to promote wound healing.
Hydrotherapy: use for removal of any topical medications or debris eschar or drainage
Water is temperature controlled
Drug therapy
Antibiotics- Gentamycin, Cephalosporin’s
Isolated room
Environment manipulation
Notes:
Equipment is not shared! Never! A lot of disposable stuff is used.
Daily cleaning is essential for equipment
Visitors are restricted when patients are compromised! Upper res infection, distinct illness, or small children (not allowed direct contact)
PPE- gowns gloves, mask, everything should be covered! Reduce cross contamination
Isolation methods need proper hand washing methods
Wear gloves with ALL contact with open wounds.
Medications
Drug therapy for pain usually requires opioid analgesics (e.g., morphine sulfate, hydromorphone [Dilaudid], fentanyl) and nonopioid analgesics.
Oral meds are not as effective because of poor circulation! IV is preferred!
Silver sulfadiazine (Silvadene) to the burn wounds: Reduction of bacterial growth in the wound and prevention of systemic sepsis
Cimetidine (Tagamet) is used to treat ulcers of the stomach and intestines
Burn unit criteria
Partial-thickness burns greater than 10% TBSA
Burns that involve the face, hands, feet, genitalia, perineum, or major joints
Third-degree burns in any group
Electrical burns, including lightning injury
Chemical burns
Inhalation injury
Burn injury in patients with preexisting medical disorders that could complicate management, prolong recovery, or affect mortality
Any patient with burns and concomitant trauma (such as fractures) in which the burn injury poses the greatest risk of morbidity or mortality
Burned children in hospitals without qualified personnel or equipment for the care of children
Burn injury in patients who will require special social, emotional, or long-term rehabilitative intervention
Parkland formula
For adults the formula is: 2 to 4 mL of lactated Ringer’s solution × body weight (in kg) × percentage burn (rule of nine).
Time- needs to be absolute to when the injury actually occurred! Information typically comes from EMT or who brings patient in
Rule of 9’s
The rule of nines is the most rapid method for calculating the size of a burn injury in adult patients whose weights are in normal proportion to their heights. With this method, the body is divided into areas that are multiples of 9%.
Burn nurse assessments (normal and abnormal)
Seen in burns:
The tissue destruction caused by a burn injury affects FLUID AND ELECTROLYTE BALANCE, and leads to local and systemic problems, including protein losses, sepsis, and changes in metabolic, endocrine, respiratory, cardiac, hematologic, and immune functioning.
Circulatory disruption occurs at the burn site immediately after a burn injury.
Blood vessels to the burned skin are occluded, and blood flow is reduced or stopped.
Damaged macrophages within the tissues release chemical mediators that cause blood vessel constriction.
Blood vessel thrombosis may occur, causing necrosis.
After a burn injury, there is a massive FLUID loss through excess evaporation.
A fluid shift occurs after initial vasoconstriction as a result of blood vessels near the burn dilating and leaking FLUIDS into the interstitial space.
This impaired FLUID AND ELECTROLYTE BALANCE leads to a continuous leak of plasma fluids and proteins from the vascular space into the interstitial space, which decreases blood volume and blood pressure.
Profound disruptions of FLUID AND ELECTROLYTE BALANCE and acid–base balance occur as a result of the fluid shift and cell damage.
These imbalances include hypovolemia, metabolic acidosis, hyperkalemia, and hyponatremia.
Fluid remobilization starts about 24 hours after injury, when the capillary leak stops and capillary integrity is restored.
The diuretic stage begins at about 48 to 72 hours after the burn injury as capillary membrane integrity returns.
Heart rate increases and cardiac output decreases because of the initial fluid shifts and hypovolemia that occur after a burn injury.
Cardiac output may remain low until 18 to 36 hours after the burn injury.
Cardiac output increases with fluid resuscitation and reaches normal levels before plasma volume is restored completely.
Other organs, including the GI tract, have decreased blood flow.
Gastric mucosal integrity and motility are impaired
Nurse priorities with burns
Infection prevention
IV
Airway
Fluid volume
I&O
Thermal regulation
Pain control
Skin graft interventions
After surgery, graft sites are immobilized with bulky cotton pressure dressings for 3 to 5 days to allow vascularization, or “take,” of the newly grafted skin.
Do not disturb the dressing and encourage elevation and complete rest of the grafted area to allow blood vessels to connect the graft with the wound bed.
Any activity that might cause movement of the dressing against the body and separation of the graft from the wound is prohibited.
Grafts and donor sites on posterior body surfaces present special problems. For the graft to become fully vascularized or for the donor sites to dry, the patient must be immobilized in a side-lying or prone position for 7 to 10 days.
Compression dressings are applied after grafts heal to help prevent contractures and tight hypertrophic scars, which can inhibit MOBILITY
Zone of injuries
Zone of coagulation
This occurs at the point of maximum damage. In this zone there is irreversible tissue loss due to coagulation of the constituent proteins.
Zone of stasis
The surrounding zone of stasis is characterized by decreased tissue perfusion.
The tissue in this zone is potentially salvageable. The main aim of burns resuscitation is to increase tissue perfusion here and prevent any damage becoming irreversible.
Additional insults—such as prolonged hypotension, infection, or edema—can convert this zone into an area of complete tissue loss.
Zone of hyperaemia
In this outermost zone tissue perfusion is increased. The tissue here will invariably recover unless there is severe sepsis or prolonged hypo-perfusion.
refers to the inflammation part (red warm swelling, puffy)
Lower Airway/Respiratory
S/S of Cor Pulmonale
Chronic productive cough from an accumulation of fluid in the lungs
Dyspnea
Cyanosis
Hoarseness due to compression of the laryngeal nerve
Chest pain may occur resulting from pulmonary artery dilation and right ventricle cell death
Hypoxia
Fatigue
Severe S/S
o Fluid back-up
o Distended neck veins
o Liver enlargement
o Peripheral edema
o S3 – abnormal heart sound develops
Pulmonary HTN Treatment
UNCURABLE DISEASE
Give oxygen to keep 02 stats about 92% oxygen
Diuretics (Lasix, furosemide): causes the ventricle to work more effectively (monitor fluid & electrolyte balance, teach to avoid excessive heat to avoid dehydration)
Anticoagulants: assists the right ventricle to be more effective
o Coumadin: prevents the blood from clotting (watch PT and INR)
o Heparin: subQ or IV (watch aPTT)
Vasodilators
Surgery: lung transplant
Pulmonary Wedge Pressure S/S if Altered
Pulmonary Artery Wedge Pressure (PAWP) is an indirect measurement of the left ventricular function.
o Normal reading: 4-12 mmHg
o Elevated: altered left ventricular function, hypervolemia, mitral regurgitation, or intracardiac shunt, elevations in blood volume
o Decreased: hypovolemia (from dehydration or hemorrhage) or afterload reduction
Critical Care
Criteria for placement of tracheostomy
Patient who needs long term ventilation (longer that 10-14 days).
Failure to wean from mechanical ventilation
Traumatic neurologic insult.
Pneumothorax vs pneumonia
Pneumothorax affects the chest wall, pleura and the respiratory muscles – OUTSIDE the lung but other organs are not involved.
Pneumonia is a disease of lung tissue, affects alveoli and is located INSIDE the lung
Both you will see hypoxia
Types of pneumothoraxes
Flail Chest: two or more ribs are fractured, leads to rib cage instability, extremely painful, needs to be intubated.
Pneumothorax: is air in the pleural space causing negative pressure in the chest cavity, a rise in chest pressure, and reduction in vital capacity, caused by blunt trauma
Hemothorax: is bleeding into the chest cavity
Tension pneumothorax: life threatening complication of pneumothorax in which air continues to enter the pleural space during inspiration and does not exit during expiration.
Open pneumothorax: pleural cavity is exposed to outside air (open wound)
Closed pneumothorax: spontaneous pneumothorax (COPD)
Pneumothorax teachings
Patient need to understand the signs and symptoms, must have emergency number available. Avoid smoking, no high altitude, in non-pressured airplanes, scuba diving for at least 6 months.
Patient has 50% change to get a pneumothorax again.
Preventative measures and interventions for those mechanically ventilated
Ambu bag close by and connected
Continuous pulse oxi
Monitoring ABG
Documentation of CpO2 every hour
Breath sounds every 2-4 hours
Suction of secretions,
Monitor for high pressure alarms
Perform oral care every 2 hours
Monitor for restlessness meaning hypoxia
Auscultate bilateral lung fields to ensure placement
Make sure artificial airway is secure
Check trach cuff pressure every shift
Check ABG for adjustment of ventilator
Endotracheal tube removal interventions
Explain the procedure
Set up prescribed oxygen system at bedside and bring in the equipment for emergency reintubation
Hyper oxygenate the patient
Suction both the ET tube and the oral cavity, then rapidly deflate the cuff and remove the tube at the PEAK inspiration, immediately instruct the patient to cough
Monitor vital signs after extubating every 5 minutes at first and asses the ventilatory pattern for signs of respiratory distress.
It is common for patient to be hoarse and have a sore throat for few days.
Teach patient semi flower position, take deep breaths every half hour and use incentive spirometer every 2 hours, limit speaking.
Other note from Vanessa presentation.
Cardiac output is 4 to 8 liter per minute.
Increase of cardiac contractility causes an increase in myocardium oxygen demand,
ischemia, hypocalcemia acidosis are conditions that decreases contractility
Beta blockers and calcium channel blockers these will have negative inotropic effect and therefore reduce myocardium oxygen demand.
Vasoactive intravenous medication = to maintain normal blood pressure.
Example of vasoactive medication are adrenaline. Noradrenaline, dopamine, dobutamine, isoprenaline dopexamine.
PAWP normal pressure is 4 to 12 mmHg it indirect measures the left ventricle function.
When the wedge pressure is elevated patient has a altered left ventricle function or have a elevated blood volume.
When the wedge pressure is low patient are hypovolemic from dehydration or hemorrhage.
Increased intracranial pressure S/S decreased LOC, hypotension, bradycardia, N/V, changes in respiratory, edema of the eyes, headache.
To lower ICP- use of osmotic diuretics such as mannitol (pulls of extra fluids from the brain tissue. And loop diuretics and corticosteroids, head needs to be in midline, HOB 30 to 45 degrees, NEVER Trendelenburg.
[Show More]


.png)





.png)