Midwifery Comprehensive Exam | Complete Solutions (Answered) Two products of impaired blood flow to the legs are thought to be linked to cramps? Pyruvic acid Lactic acid Name two prevention techniques for nocturnal leg
...
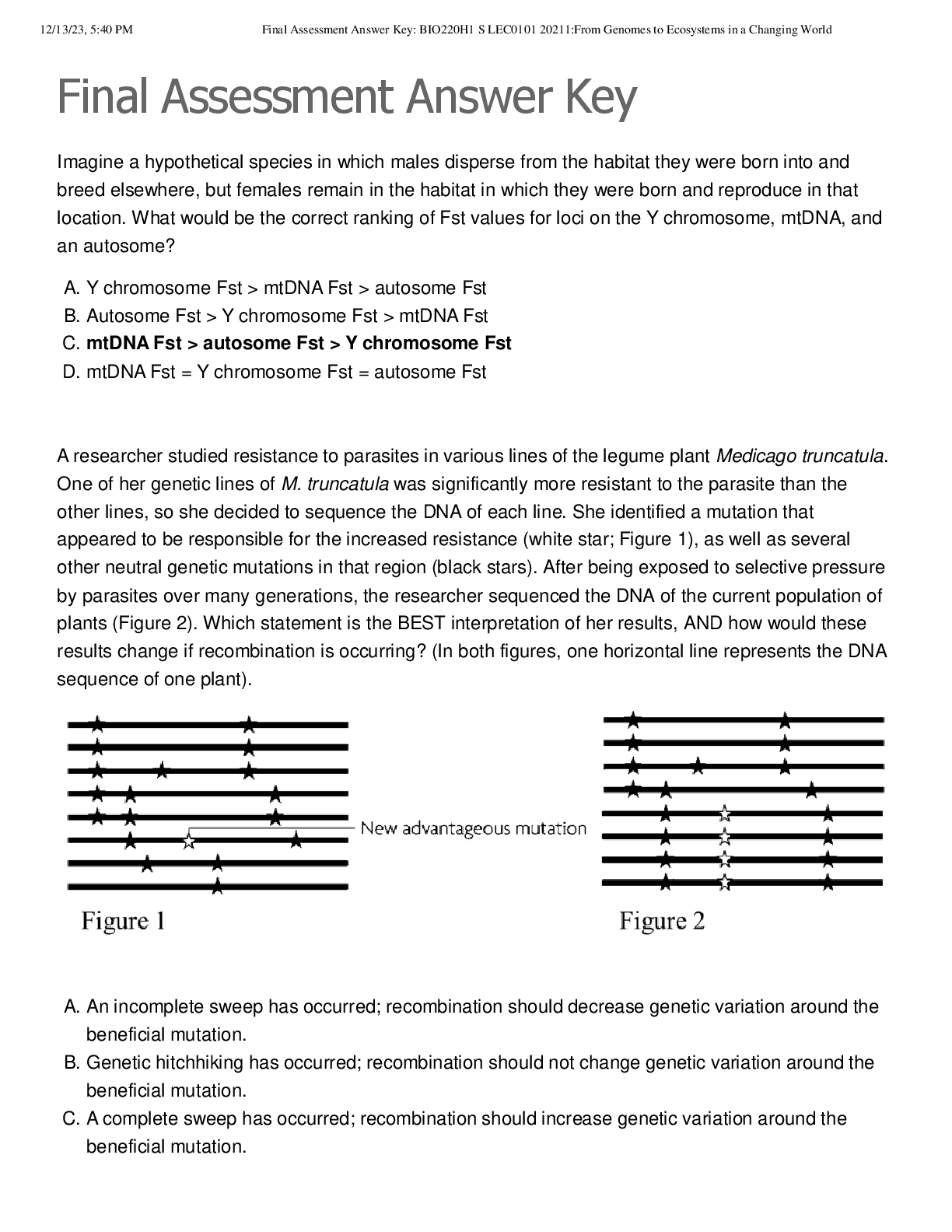
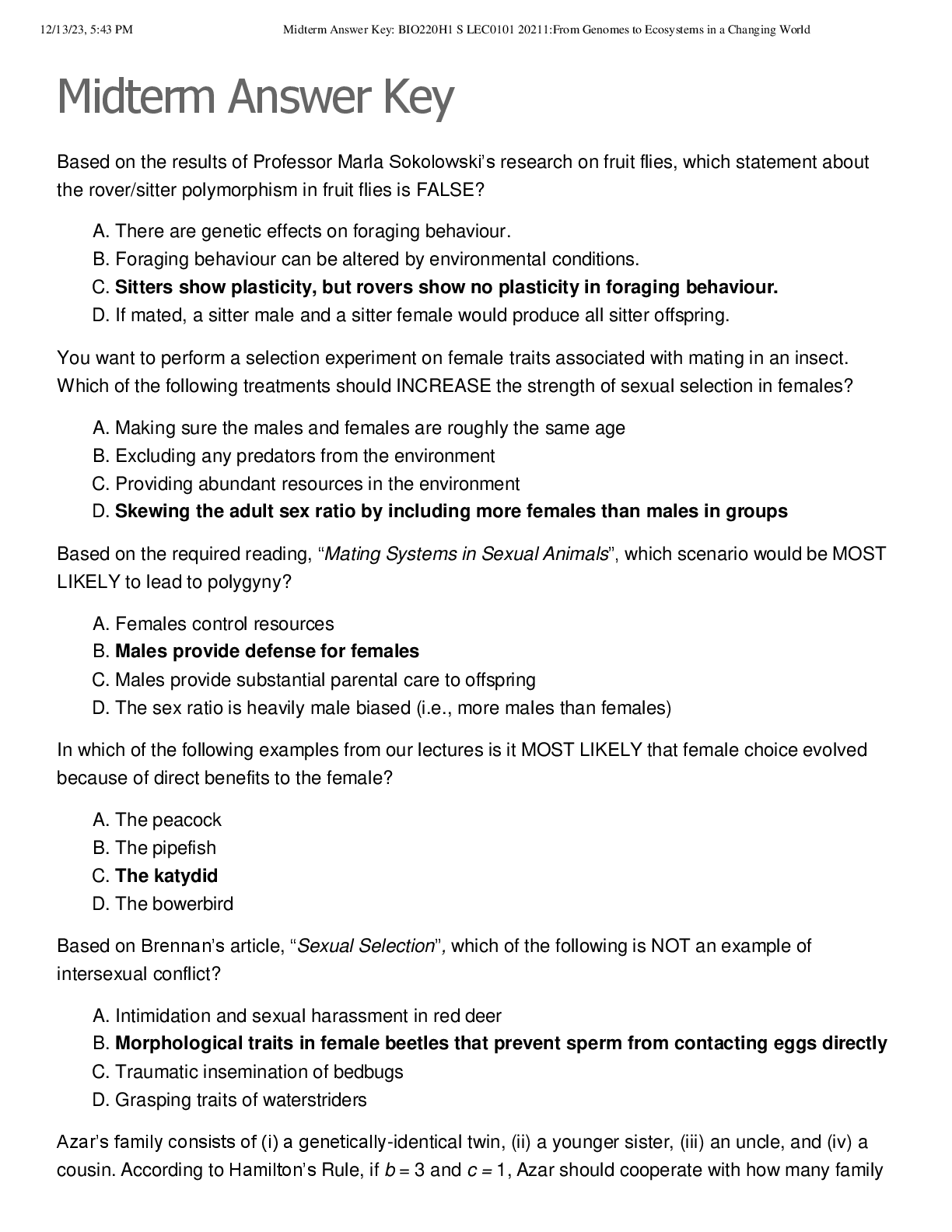
Midwifery Comprehensive Exam | Complete Solutions (Answered) Two products of impaired blood flow to the legs are thought to be linked to cramps? Pyruvic acid Lactic acid Name two prevention techniques for nocturnal leg cramps Hydration, stretching, avoid long periods of sitting or standing, warm baths, exercise What is the most important differential diagnosis to rule out when a pregnant patient comes in with complaints of leg cramping? Deep Vein Thrombosis: Look for warm red tender swollen leg. Conflicting evidence supports taking which supplement for leg cramps? Magnesium True or false. Women with NVP have lower rates of preterm births, low birth weight babies, congenital anomalies, and stillbirths. True How does progesterone contribute to NVP? Slows peristalsis and gastric emptying If dietary measures, lifestyle changes, and OTC remedies do not help with NVP, what medicine has shown to be effective with NVP? Antiemetics such Zofran (Ondansetron). Note: Not mentioned in Varney's True of False. Effective therapy for NVP will always remain the same for a woman throughout her pregnancy and subsequent pregnancies. False. Effectiveness of therapy may fluctuate over the course of pregnancy and varies greatly from pregnancy to pregnancy. True or False. To combat nausea during pregnancy, one should brush their teeth immediately after they eat. False. Brushing your teeth can stimulate the gag reflex, aggravating nausea and vomiting. What pre-existing conditions can contribute to NVP? H. pylori and GERD What is the most important differential diagnosis to rule out with leg cramps during pregnancy? Deep vein thrombosis True/false: Leg cramps during pregnancy are not normal and should be reported immediately to provider. False. Leg cramps are completely normal during pregnancy and occur more frequently during the 2nd and 3rd trimesters. How can your pregnant patient prevent leg cramps (select all that apply)? a. Walking or other exercise b. Drink plenty of water c. Stretch before bed d. Taking a warm bath e. Sitting for long periods of time True/false: Dorsiflexion of the affected foot when a cramp begins helps to alleviate the pain. True True/false: Magnesium supplements have been found to help with leg cramps. False. Research is mixed and taking magnesium supplements seem to have little effect on preventing leg cramps in pregnant women. True or False: Back pain may be a sign of preterm labor only if cramping is present. False: Cramping may or may not accompany preterm labor. What are some of the contributing factors causing back pain during pregnancy? A. The weight of a growing uterus B. A shift in her center of gravity C. Relaxation of sacroiliac ligaments D. All of the above True or False: Acupuncture is a holistic method that has not been correlated with effective pain relief. False: One study found that 60% of women reported a decrease in back pain after receiving acupuncture. True or False: It is safe to receive chiropractic manipulation during pregnancy. True: As long as a patient sees a licensed chiropractor, studies have shown manual manipulation to be effective. Why does Round Ligament pain occur? As the uterus grows during pregnancy the ligaments stretch and thicken to accommodate and support it. These changes can occasionally cause pains. Where are Round Ligament pains felt? Round Ligament pain is a sharp pain or jabbing feeling often felt in the lower belly or groin area on one or both sides. What are some of the triggers of Round Ligament pains? Round Ligament pains can occur with position changes, getting up from a sitting, lying down, coughing, sneezing, and laughing. What non-pharmacological methods can be used to alleviate Round Ligament pains? Avoid sudden movements Side lying relaxation positions Flex hips: Bend and flex before coughing, sneezing, or laughing. Apply warmth: Heat or warm bath. Exercise: Walking True/False: Round Ligament pains lasting for more than 1 minute is normal. False: Round Ligament pain should only last for a few seconds. See your health care provider for pains lasting longer or not alleviate after a short rest. What are "dermatoses of pregnancy"? Dermatoses of pregnancy are rare severe pruritic inflammatory skin diseases that are specific to women during pregnant or postpartum period. MATCH the dermatoses of pregnancy with its clinical presentation. 1. Pruritic Urticarial papules and plaques of preganancy 2. Pemphigiod gastationis 3. Intrahepatic cholestasis of pregnancy 4. Atopic eruption of pregnancy A. Red painful itchy rash that begins as erythematous papules within the striae B. Eczematous type on face, neck and flexure surfaces C. Papules that begins around the umbilicus and spreads centrifugally. D. Intense pruritus on palms of hands and soles of feet, but with an absence of lesions. 1. Pruritic Urticarial papules and plaques of preganancy= A 2. Pemphigiod gastationis=C 3. Intrahepatic cholestasis of pregnancy=D 4. Atopic eruption of pregnancy=B Pemphigoid gestationis, which begins as plaques or papules around the womans's umbilicus and spreads centrifugally. TRUE or FALSE. The plaques and papules usually spreads to the face, scalp and mucus membrane also. FALSE. In pemphigoid gestationis, the face, scalp and mucus membrane are UNAFFECTED. Your patient Ms G is in her third trimester and is complaining of intense itching, dark colored urine and clay colored stools. You suspect which dermatoses of pregnancy? A. Pruritic Urticarial papules and plaques of preganancy B. Pemphigiod gastationis C. Intrahepatic cholestasis of pregnancy D. Atopic eruption of pregnancy Pruritic Urticarial papules and plaques of pregnancy usually presents: A. Before 12 weeks gestation B. Early in the second trimester C. Late in the third trimester True/False: Although it often appears during the first trimester, pregnancy rhinitis can occur at any point during pregnancy. True. What is the believed etiology of pregnancy rhinitis? Increased hormone levels. Increased blood flow. True/False: Caffeinated fluids help relieve the symptoms of pregnancy rhinitis. False. When does pregnancy rhinitis typically resolve? After delivery- typically disappears within 2 weeks after delivery. What common discomfort occurs in about 30% of pregnancies and involves the swelling of the nasal mucosa? Pregnancy rhinitis True/False Patients have found great long term success with using intranasal decongestants for pregnancy rhinitis. False Which aspect of health is most affected by the breathing issues of pregnancy rhinitis? Sleep Which two differential diagnoses must be carefully assessed with pregnancy rhinitis? Allergic rhinitis and sinusitis True/False: Moderate levels of exercise worsen the swelling of the nasal mucosa during pregnancy rhinitis. False At how many weeks does the NVP tend to disappear? 20 weeks True or False. Sucking on hard candy in-between meals can improve nausea and vomiting? True True or False. Eating a high protein meal before bed can decrease NVP? True True or false. Acupressure is a CAM treatment for NVP that has been helpful for some women. True Is it better for women with NVP to eat 3 large meals a day or several smaller meals? Several smaller meals What is an important differential that a woman with NVP could experience that would require hospitalization? How would you differentiate between the two? Hyperemesis Gravidarum; make sure the woman is not dehydrated and not losing excessive amounts of weight. Check lab values such as CMP, CBC, AST & ALT, UA. Monitor fetal wellbeing as well. What is constipation? Relaxation of the smooth muscle of the large bowel: Decreased peristalsis/motility Classified: <1 bowel movement in 3 days, and straining with painful defecation What hormone is causes constipation by slowing down muscle contractions, intestinal muscles, and bowel activity in pregnancy? Progesterone What are three risk factors for constipation in pregnancy? low fiber diet, lack of physical activity, and decreased intake of water. What helps the absorption of iron to decrease constipation? Taking iron with orange juice. When does round ligament pain usually occur? Second trimester What is the etiology of Round ligament pain? Round ligament pain probably results from this stretching and possibly from the pressure of the increasingly heavy uterus on the ligaments Where is round ligament pain felt? Hips and Groin What are some relief measures for round ligament pain? -Acetaminophen 325-650 q4-6 or paracetamol. -Pelvic tilt exercises, re-positioning into positions that place less stress on the ligaments, and wearing a maternity support or girdle. -Slow position changes. -Walk daily - 30 min. -Stretching- Downward Dog, Bring knees to chest. -Lie on side - one pillow under belly for support, one pillow between legs -Heat, warm bath What are some differential diagnoses for round ligament pain? -Appendicitis -Constipation -Muscle strain or pain -Symphysis Pubis Diathesis -Ectopic pregnancy -Kidney / UTI Infection -Placental abruption -Chorioamnionitis -Preterm Labor What causes heartburn in pregnancy? The relaxation of the lower esophageal sphincter (s/t high levels of estrogen/progesterone), and the upward pressure of the uterus on stomach/intestines. Digested food is pushed from the stomach into the lower esophagus, causing an uncomfortable burning Approximately what percentage of women are affected by heartburn in the third trimester of pregnancy? 72% Approximately what percentage of women are affected by heartburn in the second trimester of pregnancy? 39% Approximately what percentage of women are affected by heartburn in the first trimester of pregnancy? 22% What medications are safe to use to treat or prevent heartburn? First try using antacids containing magnesium, calcium, aluminum based (Maalox, mylanta, tums...) If not effective, move onto H2 receptor antagonists (Ranitidine (Zantac), cimetidine (Tagamet)). Sodium bicarbonate antacids (Alka-Seltzer) should be avoided. What are behavior modifications that can help relieve or prevent heartburn? smaller meals avoid drinking large amounts of liquid with meals avoid laying down right after eating wear nonrestrictive clothing around the waist especially. What is important to rule out when a pregnant woman complains of chest pain? Myocardial infarction! Also: pulmonary embolism and asthma attack. What are differential diagnoses for heartburn? hiatal hernia (need endoscopy to confirm) Peptic ulcer disease (pain 2-5 hours after meal, vomiting, relief with food and antacids, need endoscopy to confirm) cholecystitis (fever, nausea, vomiting, anorexia, right upper quadrant pain) Pancreatitis (pain lasting for days, radiates to back, nausea, vomiting, abdominal distention, Turner's and Cullen's sign. test serum amylase and lipase) What might you expect in a normal/problem-free vaginal exam? Clear/white discharge, pH 3.8-4.2, negative whiff test, Lacto-bacilli present on wet mount Your patient has trichomoniasis. What might you expect in her exam? May c/o of itching, have frothy, gray, green, or malodorous discharge, "strawberry cervix", pH greater than 4.5, positive whiff test, protozoa and WBCs on wet mount Your patient has candidiasis. What might you expect in her exam? May c/o itching, discomfort, dysuria. Thick, white, clumping discharge, with vaginal inflammation/erythema. pH less than 4.5, negative whiff test, few WBCs on wet mount, yeast present on KOH wet mount Your patient has bacterial vaginosis. What might you expect in her exam? May c/o odor, discharge, itching. Discharge, thin, malodorous, milky white, homogenous, adherent. pH greater than 4.5, positive whiff test, clue cells, no/few WBCs What is the normal vaginal pH? 3.8-4.2 What conditions can cause the vaginal pH to rise above 4.5? Trichomoniasis, Bacterial Vaginosis What condition can cause "strawberry cervix"? Trichomoniasis, though candidiasis can cause inflammation/erythema What conditions can cause a positive whiff test? Trichomoniasis, Bacterial vaginosis What condition presents with clue cells? BV What conditions present with WBCs on wet-mount? Trich (many), candidiasis (few), BV (very few, may not be present) What is hyperemesis? N/V that persists beyond the first trimester of pregnancy. May result in >5% weight loss, and/or fluid/electrolyte imbalance What are the risk factors for hyperemesis? History of hyperemesis, pre-existing GI disorders (GERD, PUD, cholecystitis, gastroenteritis), pre-existing psychiatric disorders, hyperthyroidism, high HCG (due to molar pregnancy or multiple gestation) What pregnancy category is Zofran? Category B What pregnancy category is Phenergan? Category C What pregnancy category is Reglan? Category B What is the recommended dosage for zofran? 4-8 mg IV or PO What is the recommended dosage for phenergan? 12.5-25 mg PO/IM What is the recommended dosage for reglan? 5-10 mg PO/IV What are risk factors for thyroid disorders in pregnancy? Family/personal history, history of HEENT radiation, iodine insufficiency/malnutrition, Type I DM, morbid obesity, age > 30, history of recurrent miscarriage How would you screen a patient with risk factors for thyroid disease? Get a TSH in the first trimester--if greater than 2.5, draw a free T4 What is the dosage for iodine supplementation? 250 mcg/day in pregnancy and when BF (150 mcg if not) What is a normal TSH level in the first trimester? .1-2.5 What is a normal TSH level in the second trimester? .2-3 What is a normal TSH level in the third trimester? .3-3 How are free T3/T4 values altered in pregnancy? They're not, at any gestation--refer to normal lab values How are total T4 values altered in pregnancy? They are normally elevated in the first and second trimester, and normalize in the third How are total T3 values altered in pregnancy? They are normally elevated in all trimesters How does hyperthyroidism occur in pregnant women? 1. Graves Disease (antibodies stimulate the thyroid cells to produce more thyroid hormone) 2. hCG mimics TSH and causes transient hyperthyroidism (should resolve by 18-20 weeks) What are s/s of hyperthyroidism? Weight loss, nervousness, tachycardia, tremors, brittle hair May be missed/covered with an anxiety diagnosis--if you ever put someone on an SSRI, draw a TSH What complications are associated with maternal hyperthyroidism? Increased SAB, LBW, PTL, IUFD, IUGR, increased incidence of PIH, maternal thyroid storm, neonatal hyperthyroidism, maternal HF What lab values would you expect to find in a patient with hyperthyroidism? Low TSH, elevated free T4, T3 If due to Graves, positive thyroid receptor antibodies What causes hypothyroidism? Hashimoto's (chronic autoimmune disease), ablation therapy, iodine deficiency What are s/s of hypothyroidism? fatigue, depression, cold intolerance, dry skin/hair, hair loss, constipation, muscle cramps, weight gain, bradycardia What are some possible complications s/t maternal hypothyroidism? PIH, gestational HTN, anemia, placental abnormalities, PPH, PTL, LBW, increased c/s incidence, low IQ in offspring What lab values might you expect to see in a patient with hypothyroidism? Elevated TSH, reduced or normal T4 Central hypothyroidism will present with normal TSH values--treat for symptoms and refer as appropriate What is the goal of levothyroxine therapy in pregnancy? To improve fetal/maternal outcomes--alter dose to keep normal TSH range per trimester (may need to elevate as pregnancy progresses) How often are labs ordered for a woman with hypothyroidism? Every 4-6 weeks for first 20 weeks of pregnancy Once stable: every trimester Postpartum: decrease to pre-pregnancy level, or stop Retest at 6-week f/u What is postpartum thyroiditis? Abnormal TSH level in the first 12 months without nodules or TRA antibodies. Mimics normal postpartum s/s, but with more pronounced fatigue and depression (may also occur post-AB) What are risk factors for diabetes in pregnancy? Morbid obesity, personal history, PCOS, family history, glycosuria > +1 twice Describe normal diabetes screening in pregnant women? Screened at 24-28 weeks (1 hour screen + 3 hours test PRN, or a single 2-hour test)
[Show More]