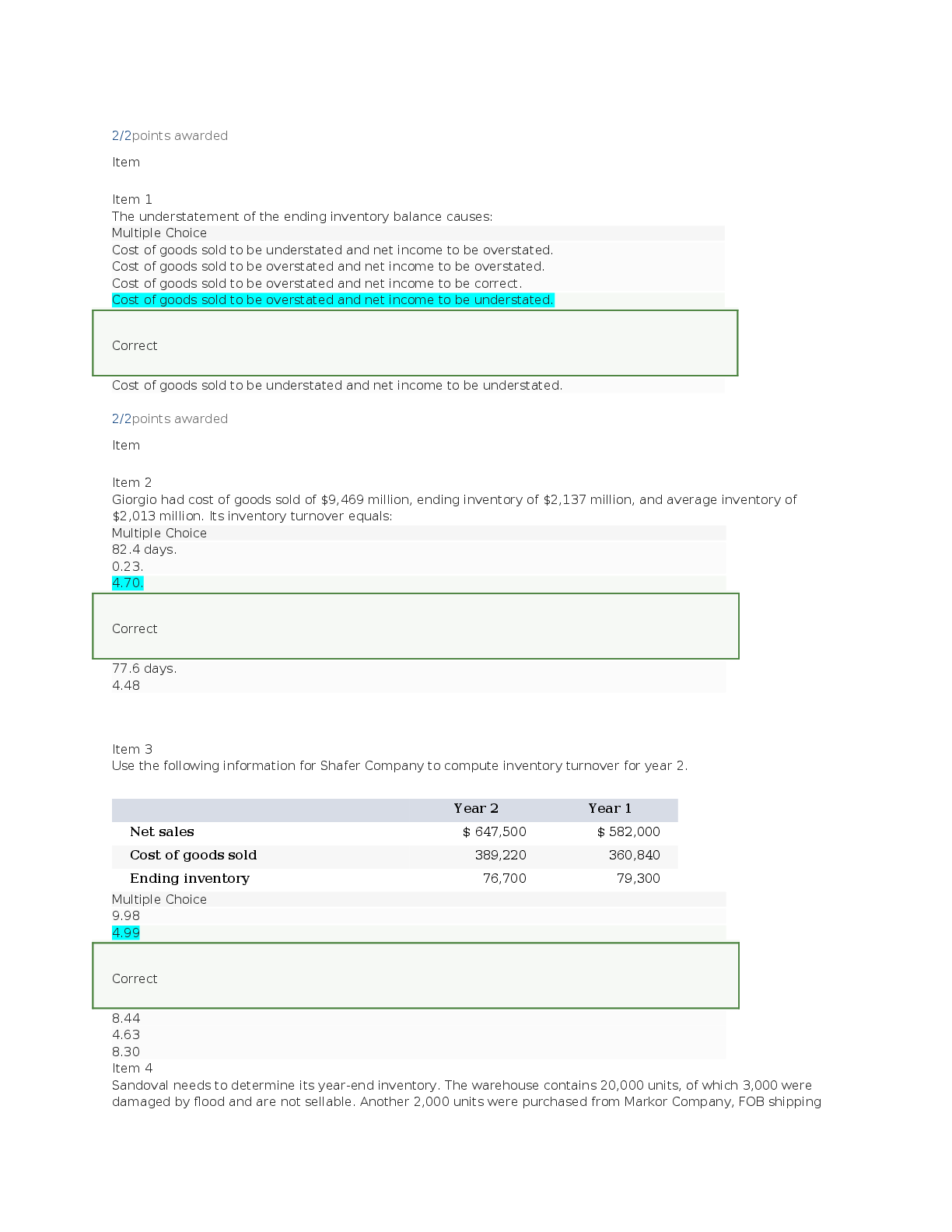
VM 535 Repro 2 Final Exam | Complete Solutions (Answered) What infectious agents specifically affect the reproductive tract of cattle Ureaplasma diversum epizootic bovine abortion (eba) tritrichomonas foetus What inf
...
VM 535 Repro 2 Final Exam | Complete Solutions (Answered) What infectious agents specifically affect the reproductive tract of cattle Ureaplasma diversum epizootic bovine abortion (eba) tritrichomonas foetus What infectious agent specifically affects the reproductive tract of the sheep Flexaspira rappini What infectious pathogens are capable of infecting multiple species Leptosporosis herpesvirus other bacterial infections What are some common viral diseases that affect cattle during pregnancy Bvdv akabane virus cache valley fever virus What are some common viral diseases that affect sheep during pregnancy Border disease virus bluetongue virus veratrum californicum cache valley fever virus What viral disease may cause the fetal sheep to be a cyclops Veratrum californicum What viral disease affects pregnancy in cats Feline panleukopenia What malformation can feline panleukopenia cause in the fetus Cerebellar hypoplasia What malformation in the fetus do parvoviruses cause in many species Mummification In dogs specifically, what malformation in the fetus do parvoviruses cause Necrotizing myocarditis What are some common bacterial diseases that affect pregnancy Brucellosis campylobacter listeriosis monocytogenes mycotic infections Fetal lesions due to brucellosis Bronchopneumonia Fetal lesions due to capylobacter Large foci of necrosis on liver Fetal lesions due to listeriosis monocytogenes Pinpoint foci of necrosis on liver Fetal lesions due to mycotic infections Leathery plaques on skin What is the most common cause of pregnancy failure Failure to implant What factors cause pregnancy failures Inadequate progesterone failure to implant embryonic or fetal death inadequate placental development placental infection or damage Causes of fetal death Fetal ischemia fetal malnutrition fetal infection congenital defects What are causes of fetal ischemia Umbilical cord twisting or knotting premature placental separation Congenital defects are caused by Teratogens What is the most important sample for submission for an abortion investigation Placenta What organ is the target of bluetongue virus Spleen In which organ may we see some strains of BVD and immature lymphocytes upon investigation of an abortion Thymus What organ is the target for hematogenous pathogens and herpesviruses Liver Which organ is the second most important for an abortion investigation as it contains balt tissues, hematogenous bacteria and also collects pathogens from amniotic fluid in the fetus Lungs Describe normal post partum involution Sloughing of maternal placenta remodeling of the endometrium contraction of the myometrium Describe post partum involution in the cow Expulsion of the placenta necrosis of the caruncles re-epithelialization of caruncles by day 30 Describe post partum involution of the dog Expulsion of the placenta formation of collagenous masses remodeling over 12 weeks Subinvolution of placental sites (sips) Delayed or incomplete post partum remodeling of the uterus What can cause sips Retained fetal membranes infection In what type of bitch is sips most common Primiparous What clinical sign will we see in a bitch with sips Prolonged postpartum bleeding from placental sites Mastitis is most common in Professional lactaters What is the primary cause of mastitis Bacteria Most mastitis cases are from _______ infections due to damage to the ______ ______ Ascending teat sphincter Mastitis: streptococcus agalatiae Chronic slow burn Mastitis: staphylococcus sp. Catastrophic gangrenous Mastitis: arcanobacterium pyrogenes Chronic slow burn Mastitis: coliforms Gangrenous Besides bacteria, what are some other infectious causes of mastitis that are less common Algae viruses Which infectious agent of mastitis can be transmitted to the young Mycoplasma What are the most common hyperplastic lesions in the dog/cat Fibroadenomatous hyperplasia in cats on progestins duct hyperplasia and ectasia T or f: spaying can be protective against mammary cancer if done prior to first heat True Common mammary neoplasms in the dog/cat Papilloma adenomas fibroadenomas complex adenomas/mixed mammary tumors adenocarcinoma/carcinoma Protozoa commonly affect _______ in the fetus Muscles Most common mammary tumor in dogs Complex adenomas/mixed mammary tumors Most common mammary tumor in queens Adenocarcinomas What initiates stage 1 of parturition Fetal stress (fetal ACTH) What happens to hormones during parturition Progesterone decreases estrogen increases PGF2alpha increases Why does estrogen increase during parturition Increases secretions for lubrication increases myometrial contractions Why does pgf2alpha increase during parturition Luteolyisis stimulates relaxin which allows for ligament straingin What reflex is initiated during phase 1 of parturition Fergusons reflex Fergusons reflex Stretching of cervix -> oxytocin release -> more contractions -> more pressure on cervix How long can phase 1 of parturition take in horses 30 min to 4 hours Why may you need to go out to examine a mare if she is 2 hours into phase 1 but showing no progression She could be truly colicking Signs of phase 1 of parturition in the mare Colic signs frequent urination restlessness sweating Stage 2 of parturition is defined by the Rupture of the chorioallantois What is added to uterine contractions during phase 2 of parturition Abdominal contractions What ends stage 2 of parturition Expulsion of the fetus How long should phase 2 of parturition take in the mare 30 minutes When should you examine a mare during phase 2 of parturition If no progress within 10-15 minutes of rupture What is the most common cause of dystocia in the mare Postural abnormalities What happens during stage 3 of parturition Expulsion of the placenta How long does this normally take in the mare 3 hours What are the normal avillous areas on the placenta of the mare Cervical star location of uterotubular locations endometrial cups placental folding yolk sac remnant What are the 3 Ps of parturition Presentation, position, posture Presentation of the fetus Orientation of the spinal axis of the fetus to that of the dam What is normal presentation of the fetus Cranio-longitudinal Position of the fetus Fetal orientation in relation to quadrants of maternal pelvis What is the normal position of the fetus Dorsosacral Posture of the fetus Relationship of the fetal extremities with respect to the body of the fetus Neonate requirements include Clean airway umbilical cord treatment dry neonate, provide warmth protection from trauma nourishment T or f: it is acceptable to swing a neonate from its hindlimbs to rid the airways of amniotic fluid False What are the steps required to perform an obstetrical exam in the mare Cleanliness lubrication exam birth canal for lesions evaluation of vulva, vestibule, vagina, cervix determine the 3 Ps of parturition assess fetal viability Where is the most common location of retained fetal membranes in the mare Non-gravid horn Pathology of retained fetal membranes in the mare Attached membranes become necrotic severe inflammatory growth/bacterial growth metritis, endotoxemia, laminitis What symptoms may you see by 12-24 hours in the mare with retained fetal membranes Depressed lethargic decreased appetite febrile How to treat a mare with retained fetal membranes if some of the placenta is outside the vulva Light weight on placenta (rectal sleeve with grain or lube) oxytocin walk the mare/apply gentle traction uterine lavage to distend chorioallantois What does a uterine lavage do for retained fetal membranes Promotes endogenous release of oxytocin Treatment for retained fetal membranes once they have passed includes Systemic antibiotics NSAIDS uterine lavage cryotherapy What is the Dutch method for retained fetal membranes in the mare Infuse water into one of the uterine vessels to help separate the microcotyledons Time window to perform the Dutch method in the mare 3 hours post partum T or f: red bag happens frequently in equine reproduction False What is "red bag" Premature separation of the chorioallantois Causes of red bag include Ascending bacterial placentitis fescue toxicosis What must you do immediately if red bag is occurring Puncture/tear placenta to pull foal out When would uterine torsion happen in the mare Mid to late gestation Signs of acute uterine torsion in the mare Mild to moderate signs of colic Signs of chronic uterine torsion in the mare Pyrexia, anorexia, depression How do you diagnose a uterine torsion in the mare Transrectal palpation (taut broad ligamant) Which way should you rotate the mare to correct a uterine torsion Same degree/direction to which the uterus is rotated Why do we not use boards when correcting a uterine torsion in the mare like we do in cattle Horses are more prone to uterine tears Can you surgically correct a uterine torsion in the mare if rotating does not work Yes Preprubic tendon ruptures are often seen in what kinds of mares Aged mares with hydrallantois or carrying a large fetus What may be a predisposing factor for a prepubic tendon rupture in the mare Extreme dependent edema Signs of a prepubic tendon rupture in the mare Sawhorse stance edema reluctance to move Treatment of a prepubic tendon rupture in the mare: goal is to save the mare Induce parturition Treatment of a prepubic tendon rupture in the mare: goal is to save the fetus Supportive care until induction T or f: you can rebreed a mare that has a prepubic tendon rupture False What ruptures to cause internal hemorrhage in the mare Utero-ovarian or uterine artery What types of mares are predisposed to internal hemorrhage during parturition Aged mares with degenerated vessel walls T or f: internal hemorrhage in the mare during parturition is rare True If a mare is experiencing a dystocia, what do you do Try controlled vaginal delivery if cvd does not work then perform a c-section When is the earliest time to breed a mare post foaling 9 days post How long does it take post foaling for the mares endometrium to repair/prepare for another embryo 15 days How long may uterine involution take in the mare 1 month How long is it normal to see lochia post foaling in the mare 5-6 days post partum Describe the 3 rules in 3 hours with foals Hour 1 - foal stands hour 2 - foal nurses hour 3 - placenta is passed When is a newborn exam recommended for a foal Within the first 24 hours of life What level igg do you want in the foal to know that it has received adequate colostrum > 800 If it is after 24 hours and the foal's igg is below 800, what should you do Give plasma When should meconium be passed in the foal post foaling Within 3-6 hours When should a foal urinate post foaling 9-10 hour post What percentage of BW of milk should a foal consume per day 21-25% Foals spend ______ of their day recumbent 1/3 Why should you not pick a foal up by their abdomen Bladder can rupture A foal should have a suckle reflex within _____ minutes 30 When should heart murmurs be investigated in the foal If they persist past 1 week of age If a foal has bloody diarrhea, what should we be concerned for Salmonella clostridium If a foals umbilicus is wet, we would be concerned of a Patent urachus What percentage of foals are born with rib fracture 5% What are the signs of impending parturition in bitches Declining progesterone ~48 hours prior drop in body temp (98) decreased appetite nesting behavior panting 6-12 hours prior white/clear mucoid vulvar discharge (cervical plug) Signs of impending parturition in queens Tachypnea restlessness +/- vocalization loud purr Stage 1 of parturition in the bitch 6-12 hours onset of uterine contractions until full cervical dilation T or f: stage 2 and stage 3 of parturition happen simultaneously in dogs and cats True When would you expect to see the first puppy after the onset of strong contractions in the bitch Within 4 hours What is the time interval between delivery of puppies 30-60 minutes What is the time interval between delivery of kittens 10-60 minutes T or f: puppies and kittens can have a cranial or caudal presentation and it will not affect birthing True Dystocia occurs in about ___% of dogs 5 Clinical signs of dystocia in the dog Stage 1 >14-16 hours stage 2 > 4 hours without delivery strong/frequent abdominal contractions without delivery of fetus within 30 minutes or lack of progression in 15 min colored discharge without delivery of fetus signs of maternal illness/distress Primary uterine inertia Failure to go into labor Causes of primary uterine intertia in the bitch Small litters/singleton pregnancies hypocalcemia/hypovitaminosis d environmental substances Secondary uterine inertia Cessation of uterine contractions due to myometrial fatigue Causes of secondary uterine inertia in the bitch Obstructive dystocia large litters hypocalcemia What does the presence of gas around fetal skeletons on a radiograph indicate Fetal death Why is it important to differentiate canine dystocia from pre-term labor/abortion? Depending on the underlying cause it may be possible to rescue the pregnancy or remaining viable fetuses What is a normal fetal heart rate 2-3 times moms What is moderate fetal stress (hr) 180-220 bpm What fetal hr would indicate that intervention is required < 140 bpm Maternal predisposing factors for dystocia in dogs/cats Breed disposition (brachycephalics, terriers) small/abnormal pelvic canal inadequate BCS systemic illness Fetal predisposing factors for dystocia in dogs/cats Fetal-maternal disproportion oversized fetus abnormal fetal disposition large litter sizes congenital defects fetal death Iatrogenic factors of dystocia in dogs/cats Excessive use of ecbolics Why is medical management contraindicated in cases of obstructive dystocia Uterine rupture could occur What should you assess/correct when performing medical management on a canine dystocia Hypoglycemia/ketosis
[Show More]