HEMA 206 Test 1 | Answered with complete solutions Compare and contrast initiation and propagation based on the criteria below -thrombin produced -what cells it occurs on What is activated -What is the end product Ini
...
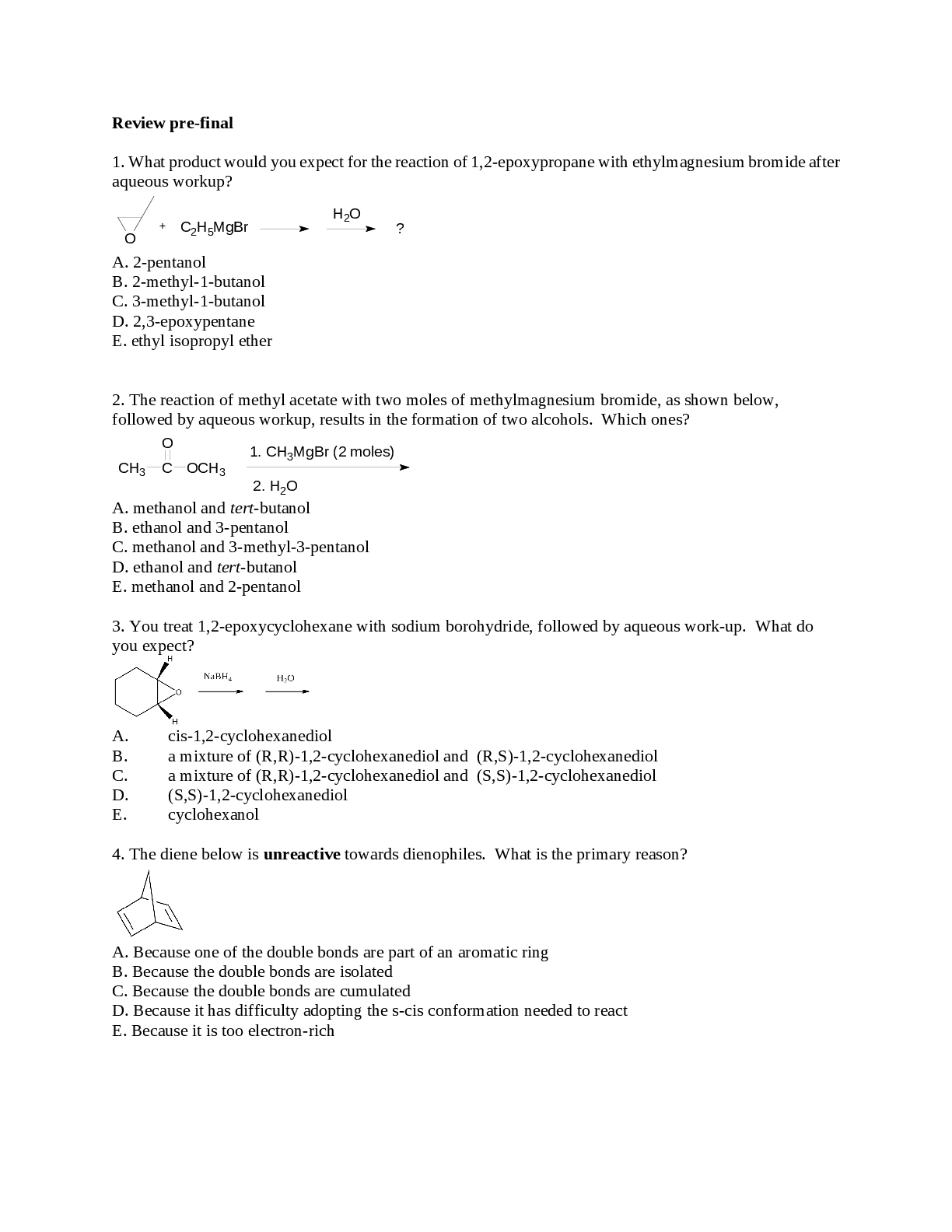
HEMA 206 Test 1 | Answered with complete solutions Compare and contrast initiation and propagation based on the criteria below -thrombin produced -what cells it occurs on What is activated -What is the end product Initiation: -2-5% thrombin -extravascular TF expressing cells - Platelets, coagulation factors, - platelet plug Propagation -95-97% - actrivated platelets - Intrinsic pathway - Stable fibrin clot T/F Activated platelets is where initiation occurs, while extravascular TF cells is where propagation occurs for the cell based theory of coagulation False – reverse Which of the below is false regarding the cell based theory initiation step? a) Platelets, coagulation factors, and cofactors become activated in this step b) 2-5% of the thrombin is produced c) Occurs on extravascular tissue factor expressing cells d) Causes a stable clot to form d) Causes a stable clot to form PLATLET PLUG FORMS Which of the below is false regarding the cell based theory of coagulation at the propagation step? a) Produces 95-97% of thrombin b) occurs on activated platelets c) The extrinsic tenase complex and prothrombinase complex form rapidly d) Causes the formation of the stable clot intrinsic tenase complex Which of the below is NOT a principle injibitory mechanism of coagulation cascade? a) Antithrombin b) Protein C & S c) TAFI d) TFPI **inhibitor of fibrinolysis (thrombin activated fibrinolysis inhibitor TFPI is tissue factor pathway inhibitor Which of the below is false regarding the TFPI? a) Principle inhibitor of the intrinsic pathway b) Domain 1 binds to TF:VIIa:Xa complex to inhibit coagulation c) Domain 2 binds to Xa to inhibit it d) Is synthesized by endothelial cells but expressed on platelets Explain how antithrombin blocks coagulation Inhibits serine proteases IXa, Xa, XIa, XIIa (and PK) to stop coagulation with the use of heparin (which accelarates its activity and induces a structural change in the AT molecule to allow it to bind coagulation factors Which of the below is responsible for the synthesis of heparin? a) Liver b) Endothelial cells c) Epithelial cells d) Platelets Which of the below is responsible for the synthesis of antithrombin? a) Liver b) Endothelial cells c) Epithelial cells d) Platelets Which of the below is responsible for the synthesis of Tissue factor pathway inhibitor? a) Liver b) Endothelial cells c) Epithelial cells d) Platelets **expressed on platelets Which of the below is responsible for the expressing Tissue factor pathway inhibitor? a) Liver b) Endothelial cells c) Epithelial cells d) Platelets Which of the below is the largest contributor to stopping the cell theory coagulation cascade? a) AT b) TFPI c) Protein C and S d) All of the above contribute equally **stops the extrinsic cascade which is the whole initiator for cell based theory Which of the below binds to thrombomodulin to activate the protein C system? a) Fibrin b) TFPI c) Heparin d) Thrombin Which of the below largely modulates the propagation step of the cell based theory? a) TFPI b) Antithrombin c) Protein C and S d) Two of the above d) Two of the above (b and c) Where is protein C synthesized? a) Liver b) Endothelial cells c) Epithelial cells d) Platelets Explain how the protein C system works? 1) Thrombin binds to thrombomodulin which is expressed on endothelial cells 2) This activates protein C, which is bound to EPCR 3) APC pops off and must bind to protein S to be stabilized 4) APC:S complex inactivates Va and VIIIa Which of the following changes thrombins activity from procoagulant to anticoagulant? a) TFPI b) Antithrombin c) Protein C system d) Two of the above ______% of protein S is bound to _________, while _________% is free floating 60%; C4bBP; 40% What compliment protein binds to protein S? a) C3b b) C2a c) C4b d) C5b If your patient was in an inflammatory state, what would happen to the protein C S system? More protein S would be bound to C4b therefore less would be available to stabilize protein C, therefore you would get excess clotting Inflammation leads to ___________ due to interference in the __________ inhibitor pathway a) Bleeding; protein C system b) Bleeding; TFPI system c) Clotting; protein C system d) Clotting; TFPI system More C4b = less protein S available = less APC stabilized What does protein system C act on to prevent excess coagulation? Va and VIIIa Neonates with purpura fulminans often have a total loss of protein in which natural inhibitor? a) TFPI b) protein C system c) AT d) TAFI Which of the below is false regarding the Protein C resistance? a) Mutation in factor VIII gene is the typical cause preventing its cleavage by APC b) Mutation in factor V gene is the typical cause preventing its cleavage by APC c) Patient will typically have clotting tissues d) patients will typically have bleeding issues e) Two of the above e) Two of the above Protein Z dependent protease inhibitor a) Inhibits XIa b) Inhibits VIIa c) inhibits XIIa d) Inhibits Xa What is the difference between a passively obtained vs actively developed inhibitor? Passively obtained: therapeutic coumadin/heparin Actively developed: antibody or protein that interferes with clotting What are the two ways in which a patient could develop a specific acquired inhibitor? 1) Immune response to replacement therapy 2) Spontaneous generation Which of the below is not typically a routine test for detecting specific acquired inhibitors? a) PT b) APTT c) NP mixing studies d) Nijmegen-Bethesda assay typically used to detect factor VIII inhibitor Which factors are the most common to have inhibitors developed against them? Why do you think so? Factors VIII and IX, they are the hemophilia A and B factors, which means patients may be receiving coagulation supplements and thus their likilihood to develop antibodies increases The Nijmegen-Bethesda assay is typically used to detect which inhibitor? a) VII b) VIII c) IX d) X T/F Antiphopholipid antibodies cause bleeding because they block the ability of coagulation factors to bind to platelets FALSE - actually causes clotting issues because it ACTIVATES the coagulation cascade What percent of individuals with recurrent thrombotic disease have APLAs? a) 5-20% b) 5-15% c) 40-50% d) 70-80% Your Patients PT and APTT tests came back prolonged, however they have no sign of bleeding issues, what is the suspected culprit? a) Factor VIII inhibitor b) TFPI c) Protein C and S d) APLAs Which of the below does not happen in vivo when discussing APLAs? a) Disrupt natural anticoagulants b) Activate platelets, promote adhesion and aggregation c) Influence endothelial release of pro-inflammatory cytokines and acrivates compliment d) Bind to platelets to prevent binding of coagulation factors actually bind to them to activate them In vivo, APLAs promote ________ while in vitro, APLAs promote _________ Thrombosis; bleeding What is one way in which you can prevent APLAs from interfering with PT and APTT testing? a) Increase the amount of phospholipids within the reagents b) Decrease the amount of phospholipids in the reagents c) Completely remove the phospholipids in the reagent d) All of the above could work You ran a coagulation study and both the PT and APTT are prolonged. Your patient doesn't really show bleeding issues, however has had 2 miscarriages previously, she also had preeclampsia in her most recent one. What is the likely cause of these results? Lupus anticoagulant T/F Specific inhibitors and non-specific (both acquired) both cause bleeding issues as seen by prolonged PT and APTT test results FALSE - specific cause bleeding, but non specific APLAs cause clotting T/F The Nijmegen-Bethesda assay is used to determine the presence of non-specific acquired inhibitors False - specific inhibitors titres Which of the below is secreted by membranes that line cavities and cover organs? a) Synovial fluid b) Serous fluid c) Cerebrospinal fluid d) Two of the above Pericardial, pleural, and peritoneal fluid are all considered a) Synovial fluid b) Serous fluid c) Cerebrospinal fluid T/F A normal healthy individual will have enough CSF, serous, and synovial fluid that we would be able to collect enough for laboratory analysis False - CSF yes, but serous and synovial fluid is typically NOT enough Which of the below can an adequate sample be drawn for in a healthy person? a) Serous fluid b) Synovial fluid c) CSF d) All of the above What are some limitations of automated analyzers for cell counts and differentials for body fluids? (4) - Differentiation only between PMNs and MNCs (not baso vs eo vs neut) - Fluid viscosity - Debris in fluid - Cell count high or low What is the time frame for WBC deterioration? a) 1H b) 2H c) 30min d) 45min Total nucleated cells include all but which of the following for manual cell counts of body fluids? a) WBC b) Malignant cells c) Tissue cells d) RBCs e) All of the above are apart of the TNC count Which of the below fluids requires a manual RBC count? a) Synovial b) CSF c) Serous d) None of the above, all just look for presence or absence Which of the below situations would you do a dilution on body fluids to get accurate cell counts? a) Fluid is clear and debris free b) Fluid has debris floating around c) Fluid is bloody or cloudy d) Always do a dilution to get accurate results You performed a WBC count using a hemocytometer. side A had a total of 31 and side B had a total of 32. No dilution was performed. What is the total number of WBCs? a) 31.5 x 10^6/L b) 78.8 x10^6/L c) 0.03x10^9/L d) 0.08 x10^9/L Which of the below is not an advantage of cytocentrifugation? a) retrievable and permanent records b) Ease and speed of prep c) Concentrates specimen d) Easy to tell morphologies apart e) All of the above are advantages Which of the below is not a disadvantage of cytocentrifugation? a) Distorts cells b) Can destroy malignant cells as they are fragile c) Cells in the center appear larger d) All of the above are disadvantages **appear smaller What is the normal range for WBCs in CSF? What about RBCs? WBCs: 0 - 5x10^6/L RBCs: NONE Which of the below is true a) Few RBCs and Few WBCs are normal in CSF b) Few RBCs and No WBCs are normal in CSF c) No RBCs and No WBCS are normal in CSF c) No RBCs and moderate WBCs are normal in CSF **a few WBCs are allowed T/F A CBC is completed on peripheral blood at the same time as CSF diffs are done True What is the correct lab location for CSF tube numbers? 1. Chemistry 2. Micro 3. Hematology Which of the below would not cause a high WBC count in CSF a) Bacterial meningitis b) Viral meningitis c) Malignancy d) Inflammatory process e) Traumatic puncture **RBC infiltration You typically see __________ in CSF when bacteria are causing meningitis, while you see __________ if its a virus Neutrophils; lymphocytes T/F WBC are higher in the CSF in viral meningitis vs bacterial False bacterial is in the 1000s while viral is in the 100s It is normal to see ____________ in the CSF of adults, while __________ can be seen in the CSF of newborns a) Monocytes; lymphocytes b) Lymphocytes; monocytes c) neutrophils; lymphocytes d) Lymphocytes; neutrophils You see eosinophils and basophils within the CSF of your patient, which of the below is the most likely cause? a) Bacterial infection b) Viral infection c) Malignant process d) Parasitic infection e) CSF shunt f) Two of the above Two of the above (d and e) What WBCs are considered normal vs abnormal in CSF? Normal - monocytes (newborns) -lymphocytes (adults) Abnormal - neutrophils (bacteria) - Eos and baso (parasite, allergy, foreign material) - Blasts (malignancy) You receive CSF tubes in the hematology lab. The first tube is dark red, the second tube is a lighter orange, and the 3rd tube is pretty much clear, is this caused by a traumatic puncture or intracranial hemorrhage? Traumatic puncture Compare and contrast a traumatic puncture vs intracranial hemorrhage for what is contained in CSF tubes in regards to -when centrifuged -clotting - cells present Traumatic puncture - clear supernatent - clotting - cartilage and nucleated RBCs Intracranial hemorrhage - hemolyzed supernatent - no clotting - siderophages - erythrophages Which of the below would you NOT expect in the CSF for an intracranial hemorrhage? a) hemolyzed supernatent when centrifuged b) Erythrophages and siderophages c) Clotting d) even amounts of blood throughout all tubes Which of the below would you NOT expect in the CSF for a traumatic puncture? a) Each tube see decreasing amounts of blood b) Clear supernatent c) Siderophages and erythrophages d) Clotting would see NRBCs (bone marrow contamination) and cartilage cells What would you expect to see in your patients CSF who is experiencing an intracranial hemorrhage that started 2-4 hours ago? a) Neutrophils and macrophages b) Erythrophages and neutrophils c) Siderophages d) Erythrophages What would you expect to see in your patients CSF who is experiencing an intracranial hemorrhage that started 1 day ago? a) Neutrophils and macrophages b) Erythrophages and neutrophils c) Siderophages d) Erythrophages and siderophages e) Erythrophages What would you expect to see in your patients CSF who is experiencing an intracranial hemorrhage that started 4 days ago? a) Neutrophils and macrophages b) Erythrophages and neutrophils c) Siderophages d) Erythrophages and siderophages e) Erythrophages What would you expect to see in your patients CSF who is experiencing an intracranial hemorrhage that started 5 weeks ago? a) Neutrophils and macrophages b) Erythrophages and neutrophils c) Siderophages d) Erythrophages and siderophages e) Erythrophages What is the timeline for seeing the below within CSF? Neutrophils and macrophages Erythrophages Siderophages with hemosiderin Neutrophils and macrophages : 2-4 hours Erythrophages: 1-7 days Siderophages with hemosiderin: 48H to 8wks Which of the below would not be an appropriate time to do a bone marrow exam? a) Patient has unexplained pancytopenia b) There are circulating blasts in PB c) The patient has a multi-linearge abnormality (RBCs, WBCs, etc.) d) Patient has severe hemolytic anemia Which of the below is a bone marrow exam not used to diagnose? a) Hematologic neoplasia b) Confirm or exclude metabolic disorders c) Iron deficiency anemia d) Some infectious disease e) All of the above are commonly diagnosed with bone marrow exams Which of the below is the best collection site for bone marrow studies including core and aspirate for adults and children? a) Sterum b) Anterior medial surface of tibia c) Posterior superior iliac crest b) Anterior superior iliac crest d) Any of the above may be used Which of the below is the easiest collection site for bone marrow studies including core and aspirates for newborns and infants? a) Sterum b) Anterior medial surface of tibia c) Posterior superior iliac crest d) Anterior superior iliac crest e) Any of the above may be used **easier to hold them down Which of the below would you only perform an aspirate and NOT a core biopsy on? a) Sterum b) Anterior medial surface of tibia c) Posterior superior iliac crest b) Anterior superior iliac crest d) Any of the above may be used Which of the below is the correct tube for BM biopsy and aspiration? a) Pink b) Purple c) Blue d) Gold e) Green What must the MLT do <24 hours before a bone marrow biopsy and aspirate? Collect an peripheral blood sample to run a CBC and blood smear on T/F After a bone marrow aspirate is completed, an MLT will draw blood to do a CBC and blood smear to compare results FALSE - must be done prior to the biopsy because the PB numbers would change How many hours prior to a bone marrow aspirate must a PB smear and CBC be collected and done? a) <8hours b) <6 hours c) <24 hours d) <4 hours T/F Part of the bone marrow aspirate goes into an EDTA tube to make a bood smear True Which of the below is used to prevent bone core and tissue from clogging the bone marrow biopsy/aspirate device? a) Jam shidi needle b) Stylet c) Shepards hook d) None of the above T/F The BM aspirate is done after collecting the core sample False Which of the below is false regarding bone marrow aspirates? a) For a direct smear aspirate, 1.5mL of sample should be present, any excess indicates peripheral blood contamination b) the total sample volume should be 5-10mL c) A buffy coat aspirate smear is performed when we expect cell counts to be low d) Spicules present in the direct smear indicate drawing sample from the incorrect location in the bone want spicules and 1.5mL For a direct BM smear you want __________mL of sample, and you want to see ________. 1.5mL bone spicules T/F You can draw a bone marrow aspirate and collect the biopsy from the same location to prevent patient discomfort False - need to be from two sites Which of the below is used to remove the bone marrow biopsy? a) Stylet b) Shepards hook c) Jam shidi d) None of the above Which of the below is the correct minimum size for a bone marrow biopsy? a) 2cm b) 1cm c) 0.5cm d) 3 cm You have to make ___________ or ___________ immediately after removing the bone marrow biopsy touch prep; impression slides T/F You place the BM biopsy into a sterile histology container with sterile saline after completing touch prep slides False - into fixative Which of the below is false regarding bone marrow aspirate smears? a) May not represent all cells b) No need for decalcification of thet specimen c) Material used for ancillary studies d) Represents architecture and we can analyze the stroma e) Able to quantify the cell types present via diff Which of the below is false regarding marrow core biopsies? a) Slow processing and requires decalcification which precldues ancillary studies b) Ability to analyze both cells and stroma c) Represents all cell types and we are able to perform a differential on them d) A sample can still be obtained if there is a dry tap e) Represents the architecture **all cell types but NO diff When would you perform a buffy coat smear on a BM aspirate? a) When cell count in the aspirate is high b) When a cell count in the aspirate is normal c) When a cell count in the aspirate is low d) We perform them always as they are easier What is contained in each layer of a Wintrobe tube and where are we collecting from for a buffy coat smear? -Top layer -2nd layer -3rd layer - Bottom layer -Top layer: fat -2nd layer: plasma -3rd layer: M:E - Bottom layer: RBCs 3rd layer The BM cellularity is the ratio of __________ cells to _________ cells? The formula to calculate it is? hematopoietic; adipose 100-age +/- 10 years A patient who is 52 years old should have a BM cellularity of a) 48 to 58% b) 38 to 58%
[Show More]