Physiology > EXAM > PHGY 216 Module 2 Exam | Questions with 100% Correct Answers (All)
PHGY 216 Module 2 Exam | Questions with 100% Correct Answers
Document Content and Description Below
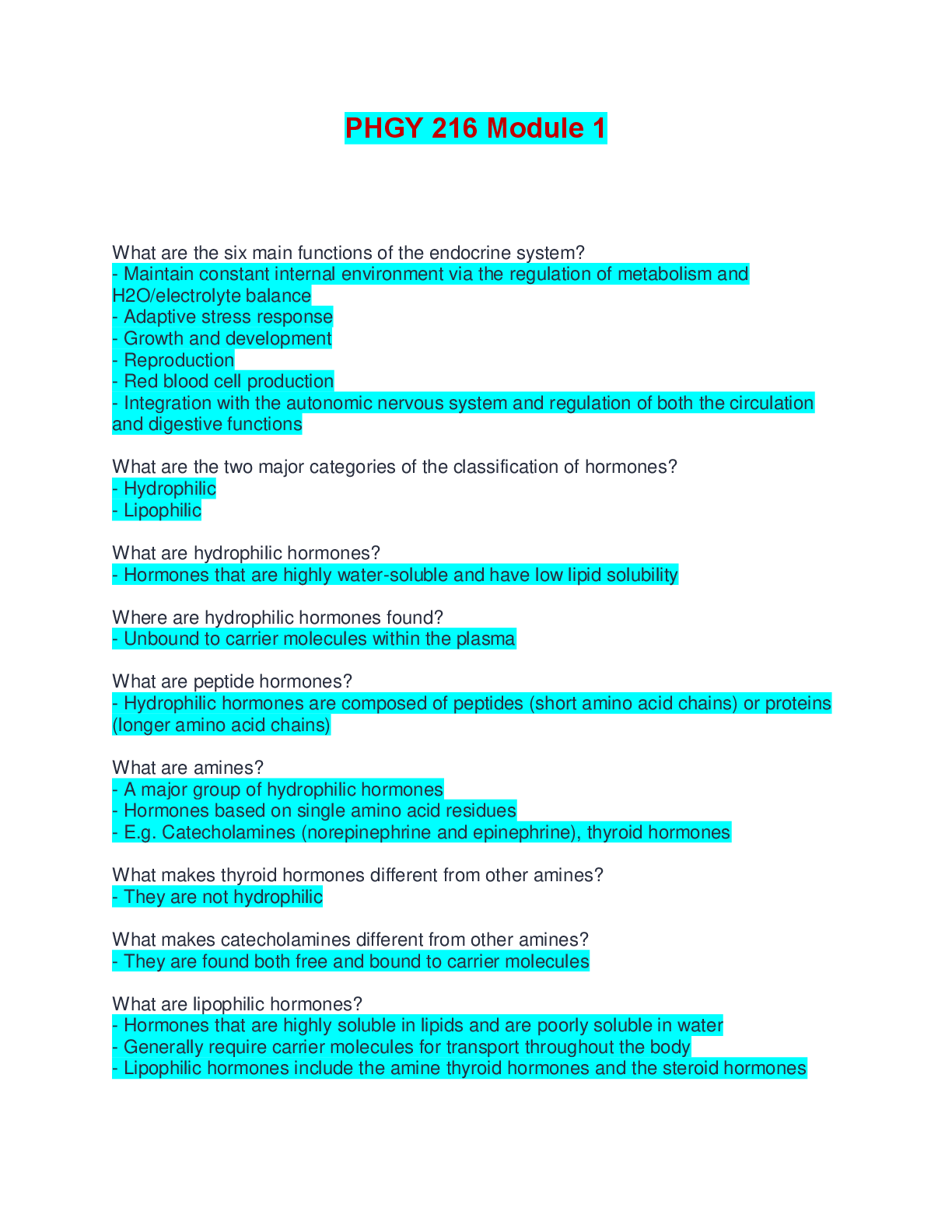
PHGY 216 Module 2 Exam | Questions with 100% Correct Answers What are gonads? - The primary reproductive organs What are the male gonads? -The testes What are the female gonads? - The ovaries What ... is the reproductive tract? - The system of ducts that are specialized to transport or house the gametes once they are produced What are the external genitalia? - The externally visible part of the reproductive tract What is sexual differentiation? - Refers to the embryonic development of both the external genitalia and the reproductive tract What are the genetic differences that lead to sexual differentiation? - Genetic sex is determined by the combination of sex chromosomes at conception How are the gametes produced? - Via meiosis - Diploid parent cells divide to produce haploid gamete cells (sperm and ova) How do fertilized ova obtain X and/or Y chromosomes? - Half of the sperm produced carry an X chromosome and the other has a Y chromosome - All ova produced carry a single X chromosome - When the two haploid cells combine they create a fertilized ovum with 2 sets of 23 chromosomes How is genetic sex determined? - If the developing embryo is formed from a sperm carrying an X chromosome then it will be an XX or female embryo - If the developing embryo is formed from a sperm carrying a Y chromosome then it will be an XY or male embryo What are the gonadal differences that lead to sexual differentiation? - Determined by the presence or absence of a Y chromosome When does gonadal differentiation occur? - For the first 6 weeks of gestation, the male and female reproductive embryo are identical - At week seven the sex-determining region of the Y chromosome (SRY) stimulates the production of H-Y antigen which acts on the gonads to differentiate into testes - The absence of H-Y antigen the gonads differentiate into ovaries What are the phenotypical differences in sex? - Dependent on the gonadal sex - Both sexes have the potential to develop either male or female external genitalia and reproductive tracts How do phenotypical differences in sex occur? - In the presence of androgens secreted by the developing testes male-type reproductive systems are developed - In the absence of androgens a female-type reproductive system is developed Describe meiosis I. - Replicated chromosomes containing an identical pair of chromatids sort themselves into homologous pairs - Each daughter cell receives a single set of chromosomes or one homologue from each pair What are the results of meiosis I? - Two daughter cells with a single set of chromosomes each containing a pair of sister chromatids Describe meiosis II. - The sister chromatids within the chromosome of each daughter cell separate and are distributed to two cells What are the results of meiosis II? - Four daughter cells each containing a single set of chromosomes containing one chromatid each What are the two primitive reproductive duct systems? - Wolffian ducts - Müllerian ducts How do the Wolffian ducts develop into the male reproductive system? - The placenta secreted human chorionic gonadotropin - If testes are present hCG stimulates them to produce and secrete testosterone - Testosterone will then stimulate the Wolffian ducts to develop into the male reproductive system How are the male external genitalia formed? - Testosterone is converted to dihydrotestosterone which develops the external male genitalia How do the Müllerian ducts degrade? - The testes secrete Müllerian-inhibiting factor How do the Müllerian ducts develop into the female reproductive system? - In the absence of testosterone, the Wolffian ducts degrade and the Müllerian ducts develop into the female reproductive tract and external genitalia Why is the differentiation of sex dependent on testosterone? - During development, the embryo is exposed to high levels of female sex hormones in the womb - Without testosterone, all fetuses would be feminized Where are the testes located? - Outside of the abdominal cavity - Within the scrotal sac When do the testes descend? - In the last months of fetal life What occurs when the testes do not descend? - For the majority of premature babies, the testes will descend in early childhood - If they remain undescended into adulthood this condition is called cryptorchidism and results in sterility What is the importance of the location of the testes? - Spermatogenesis is very temperature-sensitive - The temperature within the scrotum averages several degrees Celsius less than the core body temperature Why are individuals with cryptorchidism sterile? - They are unable to produce viable sperm because spermatogenesis cannot occur at a normal body temperature What occurs when the testes are too cold for spermatogenesis? - The cremaster and the dartos muscles contract to bring the testes closer to the body to gain heat What occurs when the testes are too hot for spermatogenesis? - The scrotal muscles relax to move the testes away from the body What structurally composes the majority of the testes? - The coiled seminiferous tubules in which sperm are produced What are Leydig cells? - The cells that produce and secrete testosterone under the control of luteinizing hormone Where does the testosterone travel? - Testosterone enters the bloodstream and circulates to distant target cells - Most testosterone enters the lumen of the seminiferous tubules where it supports sperm production What are the effects of testosterone before birth? - The masculinization of the reproductive tract and external genitalia - The descent of the testes into the scrotum What are the effects of testosterone on sex-specific tissue after birth? - Maintains the reproductive tract throughout adulthood - Promotes spermatogenesis - Promotes maturation of the reproductive system at puberty What are the effects of testosterone on other reproductive effects? - Develops sex drive pat puberty and controls the secretion of gonadotropin hormone What are the effects of testosterone on secondary sexual characteristics? - Causes the voice to deepen - Development of male pattern of body hair - Promotion of muscle growth (protein metabolism) What are the effects of testosterone on non-reproductive actions? - Promotes bone growth at puberty - Plays a role in closing the epiphyseal plates - Induces aggressive behaviour What are the two cell types that compose the majority of seminiferous tubules? - Germ cells - Sertoli cells What is spermatogenesis? - The process in which diploid (46 chromosomes) primordial germ cells are converted into motile sperm cells with a haploid (23 chromosomes) set of chromosomes What are the steps of spermatogenesis? - Mitotic proliferation - Meiosis - Packaging Describe the mitotic proliferation step of spermatogenesis. - The primordial germ cells called spermatogonia undergo mitotic division to create a constant supply of new germ cells - Following each division one of the daughter cells remains at the outer edge while the other starts to migrate toward the lumen of the tubule - The sperm-forming daughter cell will undergo mitotic divisions twice more to produce four identical primary spermatocytes - The identical spermatocytes enter a resting phase in preparation for meiosis Where are spermatogonia located? - In the outermost layer of the seminiferous tubule Describe the meiosis step of spermatogenesis. - Each primary spermatocyte forms two secondary spermatocytes each with 23 double-stranded chromosomes - During meiosis II each secondary spermatocyte results in two spermatids - Each spermatid has 23 single-stranded chromosomes - At this point there are no further divisions How many spermatids are produced from each spermatogonia? - 16 spermatids Describe the packaging step of spermatogenesis. - Cells are stripped down of all non-essentials - Cytosol and most organelles - Spermatids become spermatozoa What are the four parts of a mature spermatozoa? - Head - Acrosome - Midpiece - Tail Describe the head of the spermatozoa. - Consists of the nucleus Describe the acrosome. - Enzyme-packed vesicle at the tip of the head - Necessary to penetrate the ovum Describe the midpiece. - Packed full of mitochondria - Provides energy for locomotion Describe the flagellum. - Movement provides the propulsion What are the Sertoli cells? - Cells that make up the single-layer walls of the seminiferous tubules How are Sertoli cells connected? - Tight junctions When are the Sertoli cells permeable? - During spermatogenesis, developing sperm cells can pass between the Sertoli cells as they migrate toward the lumen What are the functions of Sertoli cells? - Form the blood-testes barrier - Nourish sperm cells - Absorb developing sperm cytoplasm and remove any defective germ cells - Secrete seminiferous tubule fluid into the lumen - Secrete androgen binding protein - Site of action for testosterone and FSH to regulate spermatogenesis Describe the blood-testes barrier. - Formed by tight junctions between the Sertoli cells - Allow the Sertoli cells to control the intratubular environment optimal for developing spermatozoa What is the purpose of seminiferous tubule fluid? - Flush released sperm into the epididymis for storage What is the purpose of androgen-binding protein? - Helps to concentrate testosterone in the lumen Which hormones control the testes? - Luteinizing hormone - Follicle-stimulating hormone What is the function of LH in males? - LH stimulates the Leydig cells to secrete testosterone What is the function of FSH in males? - FSH acts on the Sertoli cells to stimulate spermatogenesis and secrete inhibin What effect does testosterone have on the hypothalamus? - A direct negative-feedback pathway that decreases GnRH release What effect does testosterone have on the anterior pituitary? - Decrease LH and FSH release What are the effects of inhibin? - Feeds back to the anterior pituitary to decrease FSH release Describe the pathway of sperm from the seminiferous tubules to the urethra. - Non-motile sperm enter the epididymis - The epididymal ducts from each testis converge to form the ductus deferens - The ductus deferens from each testis empties into the urethra How long can sperm be stored in the epididymis? - For months What is the epididymis? - A tightly coiled tube in the testes Why aren't sperm motile when they enter the epididymis? - Due to the low pH What are the male accessory glands, and what purpose do they serve? - Seminal vesicles - Prostate gland - Bulbourethral glands - Their secretions make up the bulk of semen Where are the seminal vesicles empty? - One empties into each of the ductus deferens just before the urethra What is the purpose of the seminal vesicles? - Provide the bulk of the semen - Supple fructose as an energy source for ejaculated sperm - Secrete prostaglandins to cause smooth muscle contraction in both the male and female reproductive tracts - Secrete fibrinogen What is the prostate gland? - The large gland that surrounds the ejaculatory ducts and urethra What are the two purposes of the prostate gland? - To secrete an alkaline fluid to neutralize the acidic environment of the vagina - Secretes clotting enzymes which act on the fibrinogen from the seminal vesicles to produce fibrin which clots the semen and keep it within the female reproductive tract What is another name for the bulbourethral glands? - Cowper's glands Where do the bulbourethral glands empty? - Into the urethra - One on each side before the urethra enters the penis What is the function of the bulbourethral glands? - Secrete a clear substance during sexual arousal - The fluid helps to lubricate the urethra for sperm to pass through Describe the first step of oogenesis. - Undifferentiated primordial germ cells in the ovaries undergo mitotic division during fetal life - By month 5 of gestation, the oogonia have divided to give rise to 6-7 million primary oocytes - The process ceases with the primary oocytes arrested just before their first meiotic division Describe the structure of primary oocytes. What are they called at this stage? - Surrounded by a single layer of granulosa cells - Primordial follicles How many primary oocytes remain at birth? - The number of primary oocytes starts to decay immediately - Only 2 million remain at birth Describe the second step of oogenesis. - Primordial follicles give rise to an ongoing trickle of developing follicles - Once the follicles begin development the entire structure is called a primary follicle - The developing primary follicle either results in the release of an ova or it will undergo atresia decay - Before puberty, all primary follicles all primary follicles that develop undergo atresia What is atresia? - The process of degenerating into scar tissue How many primary follicles will mature and release ova after puberty? - About 400 What occurs to primary follicles at menopause? - The pool of primary follicles is exhausted and a woman's reproductive capacity ceases Describe the third step of oogenesis. - From puberty until menopause, a small fraction of the primary follicles will develop into secondary follicles on a cyclic basis - Primary follicles get over 1000 fold larger - Just before ovulation the primary oocyte undergoes its first meiotic division to produce two daughter cells each with 23 pairs of chromosomes - One daughter cell receives the majority of the cytoplasm to form the secondary oocyte - The other daughter cell forms the first polar body which degenerates eventually Describe the last step of oogenesis. - The secondary oocyte is released during ovulation If it is fertilized by sperm it will undergo the second meiotic division - 23 single-stranded chromosomes form the second polar body - The remaining 23 chromosomes combine with the 23 single-stranded chromosomes from the sperm What are the two phases of the ovarian cycle? - The follicular phase - The luteal phase What is the purpose of the follicular phase? - Prepare the mature egg What is the purpose of the luteal phase? - Prepares the reproductive tract for potential implantation Describe the first stage of the follicular phase. - Granulosa cells proliferate in a primary follicle - The granulosa cells divide to form several layers around the oocyte Describe the second stage of the follicular phase. - Development of the primary follicle - The granulosa cells secrete glycoproteins that form the zona pellucida - Specialized ovarian connective tissue cells differentiate and surround the granulosa cells during proliferation with a layer of thecal cells - Form follicular cells - Caused by the influence of FSH and estrogen What is the zona pellucida? - A thick extracellular matrix that surrounds the oocyte and separates it from the granulosa cells Describe the third stage of the follicular phase. - The follicle enlarges and becomes a secondary follicle - Secondary follicles are now capable of secretin estrogens, primarily estradiol - The formation of the secondary follicle is mainly due to FSH and estrogen Describe the fourth sage of the follicular phase. - The fluid-filled cavity known as the antrum is formed within the granulosa cells - Expansion of the antrum increases the size of the follicle as it matures - Estrogen secretion increases Describe the fifth stage of the follicular phase. - Around day 14 one of the follicles developed faster than the others into a mature follicle - In the mature follicle, the oocyte has undergone its first meiotic division to become a secondary oocyte Where is the oocyte located during the fifth stage of the follicular phase? - Growing off to the side of the growing follicle Describe the sixth stage of the follicular phase. - Under the influence of LH and FSH ovulation occurs around day 14 - The ovarian follicle ruptures to release the ovum into the abdominal cavity - The leaking antral fluid helps push the ovum into the oviduct - The release of the ovum represents the end of the follicular phase When does the luteal phase occur? - During the last 14 days of the ovarian cycle Describe the first stage of the luteal phase. - Follicular cells remaining after ovum release undergo luteinization to form the corpus luteum - The corpus luteum becomes highly vascularized and active in secreting hormones Which hormones are secreted by the corpus luteum? - Mainly progesterone - Some estrogens Describe the second stage of the luteal phase. - If the ovum is not implanted within 14 days, the corpus luteum rapidly degenerates to form the corpus albicans - This signifies the end of one ovarian cycle and the follicular phase begins again Which hormones control the ovarian cycle? - FSH and LH What is the importance of FSH and estrogen? - The formation of the secondary follicle What is the importance of LH? - The production of estrogen How is the secretion of LH increased? - The secondary follicle Describe the feedback action of estrogen and LH. - During the follicular phase, the anterior pituitary releases LH - Circulating estrogen inhibits the actions of GnRH on FSH-secreting cells - Estrogen levels continue to rise, exerting a positive feedback action on the anterior pituitary to cause a surge in LH secretion [Show More]
Last updated: 9 months ago
Preview 4 out of 19 pages

Loading document previews ...
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Also available in bundle (1)
Click Below to Access Bundle(s)
PHGY 216 MODULE 1-3 AND MIDTERM EXAM BUNDLE
PHGY 216 MODULE 1-3 AND MIDTERM EXAM BUNDLE
By Ajay25 9 months ago
$30
4
Reviews( 0 )
$15.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Feb 18, 2025
Number of pages
19
Written in
All
Additional information
This document has been written for:
Uploaded
Feb 18, 2025
Downloads
0
Views
18