NR 511 Final Exam Study Guide
Week 1
1. Define diagnostic reasoning
-To solve problems, to promote health, and to screen for disease or illness all require a sensitivity to complex stories, to contextual factors,
...
NR 511 Final Exam Study Guide
Week 1
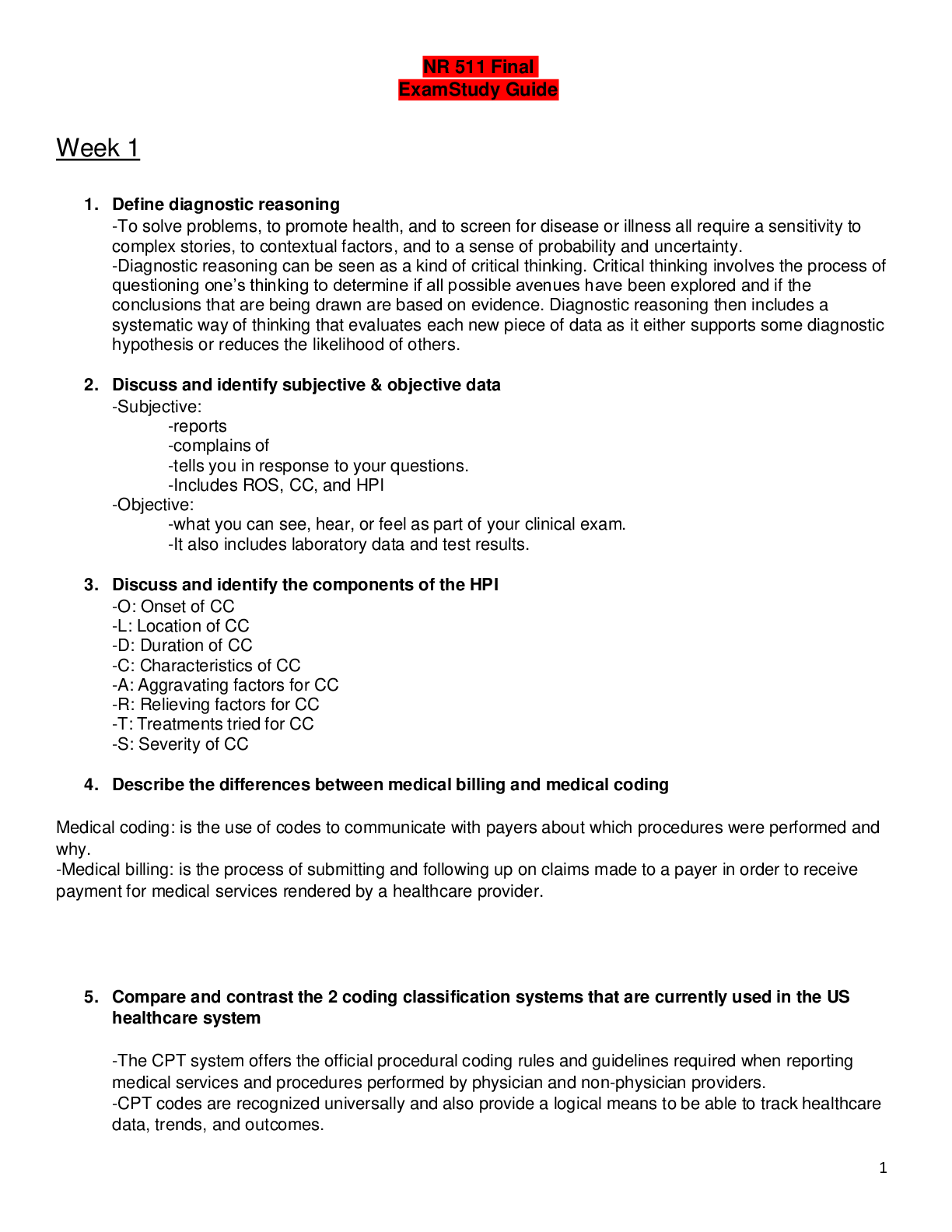
1. Define diagnostic reasoning
-To solve problems, to promote health, and to screen for disease or illness all require a sensitivity to complex stories, to contextual factors, and to a sense of probability and uncertainty.
-Diagnostic reasoning can be seen as a kind of critical thinking. Critical thinking involves the process of questioning one’s thinking to determine if all possible avenues have been explored and if the conclusions that are being drawn are based on evidence. Diagnostic reasoning then includes a systematic way of thinking that evaluates each new piece of data as it either supports some diagnostic hypothesis or reduces the likelihood of others.
2. Discuss and identify subjective & objective data
-Subjective:
-reports
-complains of
-tells you in response to your questions.
-Includes ROS, CC, and HPI
-Objective:
-what you can see, hear, or feel as part of your clinical exam.
-It also includes laboratory data and test results.
3. Discuss and identify the components of the HPI
-O: Onset of CC
-L: Location of CC
-D: Duration of CC
-C: Characteristics of CC
-A: Aggravating factors for CC
-R: Relieving factors for CC
-T: Treatments tried for CC
-S: Severity of CC
4. Describe the differences between medical billing and medical coding
Medical coding: is the use of codes to communicate with payers about which procedures were performed and why.
-Medical billing: is the process of submitting and following up on claims made to a payer in order to receive payment for medical services rendered by a healthcare provider.
5. Compare and contrast the 2 coding classification systems that are currently used in the US healthcare system
-The CPT system offers the official procedural coding rules and guidelines required when reporting medical services and procedures performed by physician and non-physician providers.
-CPT codes are recognized universally and also provide a logical means to be able to track healthcare data, trends, and outcomes.
-ICD-10 codes are shorthand for the patient’s diagnoses, which are used to provide the payer information on the necessity of the visit or procedure performed.
6. Discuss how specificity, sensitivity & predictive value contribute to the usefulness of the diagnostic data
-Specificity of a test, we are referring to the ability of the test to correctly detect a specific condition.
-Predictive value is the likelihood that the patient actually has the condition and is, in part, dependent upon the prevalence of the condition in the population.
-When a test is very sensitive, we mean it has few false negatives.
7. Discuss the elements that need to be considered when developing a plan
Acknowledge the list
-Negotiate what to cover
-Be Honest
-Make a follow-up
8. Describe the components of Medical Decision Making in E&M coding
- There are three key components that determine risk-based E&M codes.
-History
-Physical
-Medical Decision Making (MDM) E&M coding requires a medical decision maker
-Medical decision making is another way of quantifying the complexity of the thinking that is required for the visit.
-Complexity of a visit is based on three criteria:
-Risk
-Data
-Diagnosis
-Now, medical decision making is a special category. Why is this so important? Well, the MDM score gives us credit for the excess work involved in management of a more complex patient.
9. Correctly order the E&M office visit codes based on complexity from least to most complex
99212 - 99214
10. Discuss a minimum of three purposes of the written history and physical in relation to the importance of documentation
-It is an important reference document that gives concise information about a patient's history and exam findings.
-It outlines a plan for addressing the issues that prompted the visit. This information should be presented in a logical fashion that prominently features all data immediately relevant to the patient's condition.
-It is a means of communicating information to all providers who are involved in the care of a particular patient.
-It is an important medical-legal document
-It is essential in order to accurately code and bill for services.
11. Accurately document why every procedure code must have a corresponding diagnosis code
-Every procedure code needs a diagnosis to explain the necessity whether the code represents an actual procedure performed or a nonprocedural encounter like an office visit.
12. Correctly identify a patient as new or established given the historical information
• Patient status
-New patient: one who has not received professional service from a provider from the same group practice within the past 3 years.
-Established patient of your practice: has received professional service from a provider of your office within the last 3 years
13. Identify the 3 components required in determining an outpatient, office visit E&M code
-Place of service -Type of service
-Inpatient -Consultation’s
-Outpatient -Office visit
-Hospital admission
-Patient status
-New patient: one who has not received professional service from a provider from the same group practice within the past 3 years.
-Established patient of your practice: has received professional
14. Describe the components of Medical Decision Making in E&M coding
- There are three key components that determine risk-based E&M codes.
-History
-Physical
-Medical Decision Making (MDM) E&M coding requires a medical decision maker
-Medical decision-making is another way of quantifying the complexity of the thinking that is required for the visit.
-Complexity of a visit is based on three criteria:
-Risk
-Data
-Diagnosis
-Now, medical decision making is a special category. Why is this so important? Well, the MDM score gives us credit for the excess work involved in management of a more complex patient.
15. Explain what a “well rounded” clinical experience means
-Includes both children from birth through young adult visits for well child and acute visits, as well as adults for wellness and acute or routine visits
16. State the maximum number of hours that time can be spent “rounding” in a facility
<25%
17. State 9 things that must be documented when inputting data into clinical encounter
-date of service -visit E&M code (e.g., 99203) -age
-gender and ethnicity -chief concern -procedures
-tests performed or ordered -diagnoses -level of involvement
18. Identify and explain each part of the acronym SNAPPS
-S: Summarize
-N: Narrow
-A: Analyze
-P: Probe
-P: Plan
-S: Self-directed learning
Week 2
1. Identify the most common type of pathogen responsible for acute gastroenteritis
-Viral: Norovirus (Leading cause for adults)
-Rotovirus (Leading cause for peds up to 2 years old)
Gastroenteritis, also known as enteritis or gastroenterocolitis, is defined as an inflammation of the stomach and intestine that manifests as anorexia, nausea, vomiting, and diarrhea. Acute gastroenteritis results most often from an infectious agent. The most common mode of transmission for acute infectious gastroenteritis is the fecal–oral route from contaminated food or water. Person-to-person transfer of the disease is more common within the hospital setting and within day-care centers where there are larger groups of people capable of transmitting the disease. Bacterial pathogens account for 30% to 80% of acute gastroenteritis cases and are an important cause of morbidity in tropical areas and in travelers to areas of high risk for the pathogens (traveler’s diarrhea). Page 526
2. Recognize that assessing for prior antibiotic use is a critical part of the history in patients presenting with diarrhea
Due to risk of C Diff infection
Some medications, such as antibiotics, can induce diarrhea by disrupting the normal balance of bacteria. Probiotics have been studied in the treatment of diarrhea. A systematic review of 63 probiotic studies of adults and children revealed that the duration of antibiotic-associated diarrhea was shortened by a mean of 25 hours with probiotics and hydration therapy. Page
512-513.
3. Describe the difference between Irritable Bowel Disease (IBS) and Inflammatory Bowel Disorder (IBD)
-IBS (Irritable bowel syndrome): disorder of bowel function not from anatomic abnormality
-constipation, diarrhea, bloating, urgency w/ diarrhea
-NOT assoc w/ serious medical consequences, IBD or CA
+S/S: result from disordered sensation or abnormal function of the small and large bowel
-IBD (Inflammatory bowel disease): chronic immunologic disease that manifests in intestinal inflammation
- UC/CD
Normal bowel function is regulated by segmental contractions that limit the movement of bowel contents through the colon. An increase in these contractions causes constipation, and a decrease in the contractions results in frequent stooling or diarrhea. Studies have confirmed alterations in colonic activity during periods of
emotional stress, in which motility is decreased or inhibited with depression and increased with feelings of hostility and anger. Up to one-third of patients with IBS develop the disorder after bacterial gastroenteritis. It appears that patients with increased life stressors are more prone to developing IBS post infection. See #4. Page 577-578.
4. Discuss two common Inflammatory Bowel Diseases
-Ulcerative colitis (UC): the mucosal surface of the colon is inflamed and ultimately results in friability, erosions, and bleeding.
- Most common in recto-sigmoid colon. Can involve entire colon
- Pain in LLQ
-Crohns (CD): the inflammation extends deeper into the intestinal wall and can involve all or any layer of the bowel wall and any portion of the GI tract from the mouth to the anus.
- Skipped lesions
- Pain in RLQ
Inflammatory bowel disease (IBD) is the term used to describe a chronic immunological disease that manifests in intestinal inflammation. The two most common IBDs are ulcerative colitis (UC) and Crohn’s disease (CD). UC involves only the mucosal surface of the colon, which ultimately results in friability, erosions, and bleeding. It occurs most often in the rectosigmoid area but can involve the entire colon. CD is also known as regional enteritis because of the characteristic segmental presentation of the diseased bowel, which is clearly separated by areas of normal mucosa, often referred to as “skipped lesions.” CD can involve all or any layer of the bowel wall and any portion of the gastrointestinal (GI) tract from the mouth to the anus. UC is more common in males, and CD is more common in females. Page 570-571.
5. Discuss the diagnosis of diverticulitis, risk factors, and treatments
Symptoms: LLQ pain/ tenderness, fever, N/V/D
Need imaging especially if perforation or peritonitis is suspected; free air = perforation; patient may have ileus, small or large bowel obstruction
Can use plain x-ray
CT or barium enema are preferred
CT with contrast is more sensitive and accurate
Diverticular disease is the term used to describe the inflammatory changes that occur within the diverticular mucosa of the intestine (diverticulitis), as well as the asymptomatic, uninflamed outpouchings called diverticulosis. Although there is no known cause for diverticular disease, a low-fiber diet has been implicated because it causes increased intraluminal pressures within the colon, which lead to mucosal herniation through the weaker areas in the bowel wall. Other factors believed to contribute to the formation of diverticula include hypertrophy of the segments of the circular muscle of the colon, chronic constipation and straining, irregular and uncoordinated bowel contractions, obesity, and weakness of the bowel muscle brought on by aging. Risk factors are directly related to the suspected causes of the disease: older than age 40, low-fiber diet, previous diverticulitis, and the number of diverticula present within the colon. Diverticula occur most often in the left lower quadrant (LLQ); a right lower quadrant presentation is a rare condition, with a higher incidence in Asian populations. Patients with diverticulosis characteristically present with pain in the LLQ of the abdomen. When the diverticula have become inflamed, there are the usual signs and symptoms of infection—fever, chills, and tachycardia. A physical exam reveals tenderness in the LLQ of the abdomen, and—if the patient can tolerate more vigorous examination
—a firm, fixed mass may be identified in the area of the diverticuli. Initial laboratory testing can show mild to moderate leukocytosis, depending on whether the patient presents with diverticulitis or with a more advanced inflammatory process such as peritoneal abscess. The white blood cell (WBC) count is usually normal in patients with diverticulosis.
Hemoglobin and hematocrit may be low if there is associated rectal bleeding. Patients with signs suggestive of peritonitis should have a blood culture to assess for bacteremia. An incidental finding of uncomplicated diverticulosis requires no further intervention and can be managed with a high-fiber diet or daily fiber supplementation with psyllium. Treatment of a patient presenting with mild symptoms can often be managed on an outpatient basis with rest, oral antibiotics, and a clear liquid diet. Initial antibiotic therapy varies with the extent of the inflammatory process and can include metronidazole (Flagyl) 500 mg by mouth three times daily with ciprofloxacin (Cipro) 500 mg by mouth twice daily, or trimethoprim/sulfamethoxazole (Bactrim DS) 160/800 mg by mouth twice daily for 7 to 10 days. The symptoms usually
subside quickly; then the diet can be advanced to soft, low roughage and next to high fiber as tolerated. Pain due to spasms can be managed with antispasmodics such as hyoscyamine (Levsin) 0.125 mg every 4 hours, dicyclomine (Bentyl) 20 to 40 mg four times daily, buspirone (BuSpar) 15 to 30 mg/day, and/or meperidine (Demerol) 100 to 150 mg/day in divided doses. To evaluate or diagnose diverticular disease, all patients will require colonoscopy at some point during their disease process; therefore, referral to a gastroenterologist is indicated for symptoms that do not respond to treatment after 6 months. Patients diagnosed with diverticular disease will need to make modifications in their diets with an emphasis on increasing the amount of dietary fiber. The goal of diet therapy is to avoid constipation and straining during bowel movements, which can further increase intraluminal pressures and cause complications. Patients should also be instructed to drink at least ten 8-ounce glasses of water a day to have regular, soft bowel movements. Pages 584-586
6. Identify the significance of Barrett’s esophagus
After repeated exposure to gastric contents, inflammation of the esophageal mucosa becomes chronic.
· Blood flow increases, erosion occurs
· As erosion heals, normal squamous epithelium replaced with metaplastic columnar epithelium containing goblet and columnar cells
· More resistant to acid and supports esophageal healing
· Premalignant tissue
· 40-fold risk for development of esophageal adenocarcinoma
· Fibrosis and scarring during healing of erosions; leads to strictures
As the erosion heals, the body replaces the normal squamous epithelium with metaplastic columnar epithelium (Barrett’s epithelium) containing goblet and columnar cells. This new epithelium is more resistant to acid and, therefore, supports esophageal healing. Barrett’s epithelium is a premalignant tissue, however, and presents a 40-fold increased risk for the development of esophageal adenocarcinoma. Fibrosis and scarring also accompany the healing process, leading to esophageal strictures. Page 523.
7. Discuss the diagnosis of GERD, risk factors, and treatments
- Diagnosis made on history alone; sensitivity of 80%
- If symptoms are unclear/patient doesn’t respond to 4 weeks of empiric treatment
- Dx made by ambulatory esophageal pH monitoring
- pH < 4 above the lower esophageal sphincter and correlates with symptoms = GERD
- EGD with biopsy – Barrett’s esophagus
- Normal results in 50% of symptomatic patients
- Risks
o Obesity
o Increases after age 50
o Equal across gender, ethnic, and cultural groups
- Treatment
o Small, frequent meals – main meal at midday
o Avoid trigger foods
o No bedtime snacks; no eating < 4 hours prior to bed
o Eliminate caffeine
o Stop smoking
o Avoid tight fitting clothing
o Sleep with head elevated
- Medication:
o Step 1: antacids or OTC H2 (Tagamet, zantac, axid)
o Step 2: Rx-strength H2 (ranitidine 150mg BID, famotidine 20mg BID) or PPI (pantoprazole 40mg daily, omeprazole 20mg daily)
...........................................CONTINUED...........................................
[Show More]