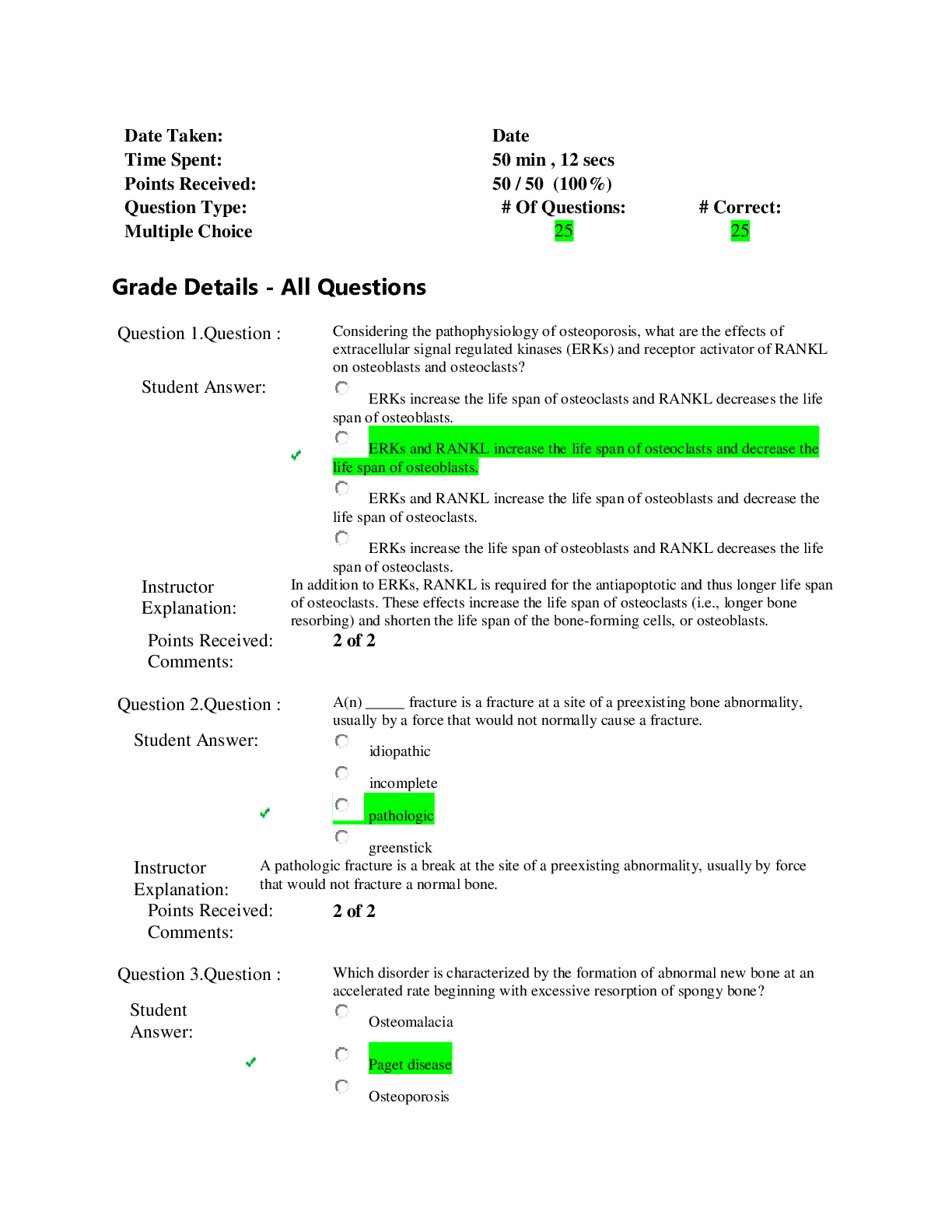
*NURSING > EXAM > Chamberlain College of Nursing - NR 509NR509_SOAP_Abdomen. Done and Completed. Grade A (All)
Chamberlain College of Nursing - NR 509NR509_SOAP_Abdomen. Done and Completed. Grade A
Document Content and Description Below
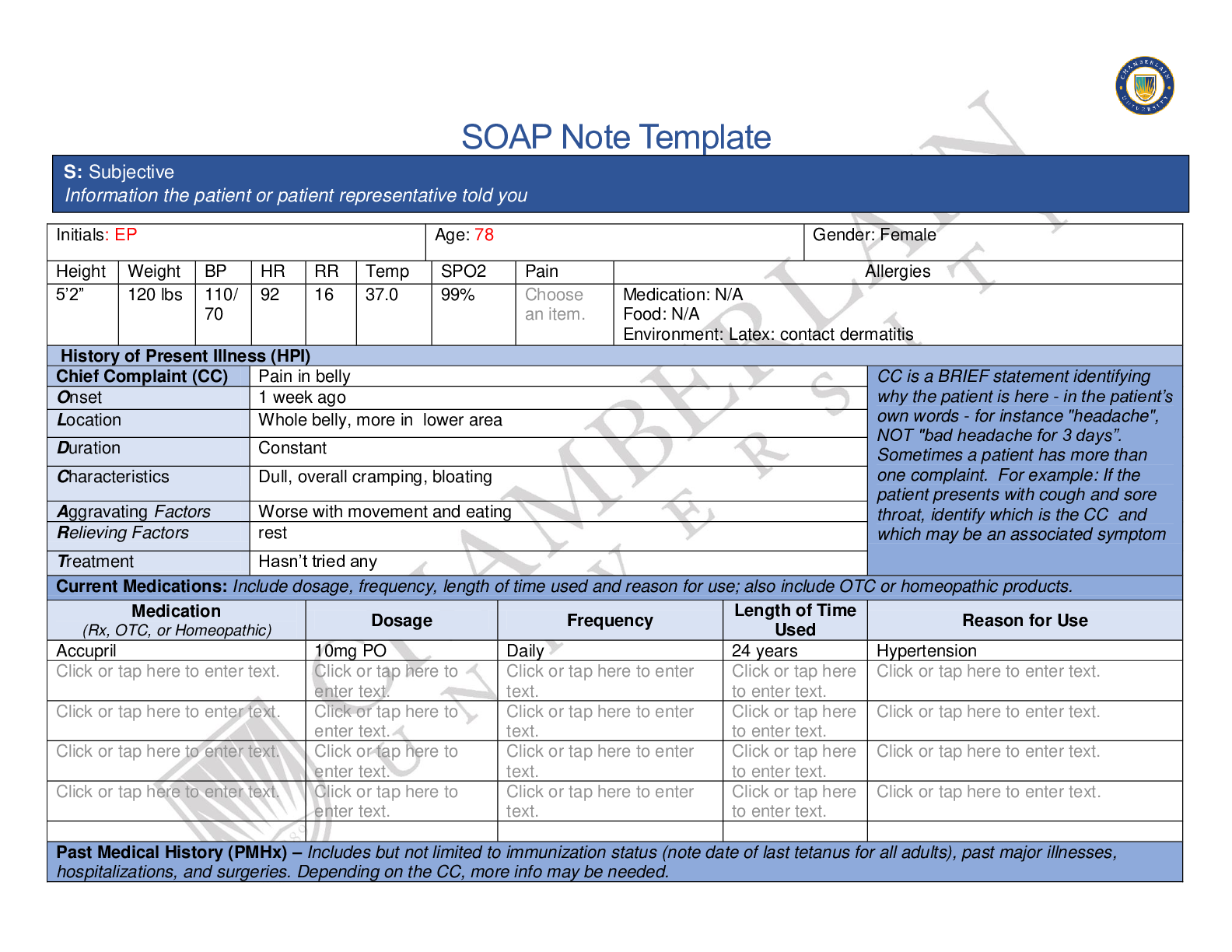
SOAP Note Template Initials: EP Age: 78 Gender: Female Height Weight BP HR RR Temp SPO2 Pain Allergies 5’2” 120 lbs 110/ 70 92 16 37.0 99% Choose an item. Medication: N/A Food: N/A Enviro... nment: Latex: contact dermatitis History of Present Illness (HPI) Chief Complaint (CC) Pain in belly CC is a BRIEF statement identifying why the patient is here - in the patient’s own words - for instance "headache", NOT "bad headache for 3 days”. Sometimes a patient has more than one complaint. For example: If the patient presents with cough and sore throat, identify which is the CC and which may be an associated symptom Onset 1 week ago Location Whole belly, more in lower area Duration Constant Characteristics Dull, overall cramping, bloating Aggravating Factors Worse with movement and eating Relieving Factors rest Treatment Hasn’t tried any Current Medications: Include dosage, frequency, length of time used and reason for use; also include OTC or homeopathic products. Medication (Rx, OTC, or Homeopathic) Dosage Frequency Length of Time Used Reason for Use Accupril 10mg PO Daily 24 years Hypertension Past Medical History (PMHx) – Includes but not limited to immunization status (note date of last tetanus for all adults), past major illnesses, hospitalizations, and surgeries. Depending on the CC, more info may be needed. S: Subjective Information the patient or patient representative told youCurrent with immunizations; has not had flu shot this year; unknown date of last tetanus shot. Diagnosed with hypertension at 54- medically managed. 3 pregnancies, 2 live births, one still birth. Surgical history: c-section (age 40) and cholecystectomy (age 42) Hospitalizations: post child birth (x3) and after cholecystectomy. Social History (Soc Hx) - Includes but not limited to occupation and major hobbies, family status, tobacco and alcohol use, and any other pertinent data. Include health promotion such as use seat belts all the time or working smoke detectors in the house. Denies smoking, smokeless tobacco, and illicit drug use. Has 1 glass of wine on Sundays (4 days a month). Exercises regularly (water aerobics). Family History (Fam Hx) - Includes but not limited to illnesses with possible genetic predisposition, contagious or chronic illnesses. Reason for death of any deceased first degree relatives should be included. Include parents, grandparents, siblings, and children. Include grandchildren if pertinent. Mother: deceased age 88; PMH: HTN and DM type 2 Dad: deceased age 82- MI; PMH: HTN and HLD Maternal gradmother: DM type 2 Maternal grandfather: CAD- deceased, MI Paternal grandmother: HTN, died from CA Paternal grandfather: CVA, obesity Brother: 80; PMH: HTN, HLD, prostate CA Brother: 81; PMH: HTN Son: age 48, healthy Daughter: 46, healthy Review of Systems (ROS): Address all body systems that may help rule in or out a differential diagnosis Check the box next to each positive symptom and provide additional details. Constitutional Skin HEENT ☒Fatigue recently with current issue ☒Weakness recently with current issue ☐Itching Click or tap here . ☐Rashes Click or tap here . ☐Diplopia Click or tap here . ☐Eye Pain Click or tap here . ☐Earache . ☐Tinnitus . ☐Hoarseness . ☐Oral Ulcers .☐Fever/Chills Click or tap here . ☐Weight Gain Click or tap here . ☐Weight Loss Click or tap here . ☐Trouble Sleeping Click or . ☐Night Sweats Click or tap here . ☐Other: enter text. ☐Nail Changes Click or to enter text. ☐Skin Color Changes . ☒Other: dry ☐Eye redness Click or . ☐Vision changes Click or . ☐Photophobia Click or . ☐Eye discharge Click or . ☐Epistaxis Click or tap here . ☐Vertigo . ☐Hearing Changes Click or . ☐Sore Throat . ☐Congestion . ☐Rhinorrhea . ☐Other: Respiratory Neuro Cardiovascular ☐Cough enter text. ☐Hemoptysis . ☐Dyspnea enter text. ☐Wheezing enter text. ☐Pain on Inspiration . ☐Sputum Production ☐Other: enter text. ☐Syncope or Lightheadedness Click or tap here . ☐Headache . ☐Numbness . ☐Tingling . ☐Sensation Changes ☐Speech Deficits Click or tap here . ☐Other: . ☐Chest pain enter text. ☐SOB ☐Exercise Intolerance . ☐Orthopnea enter text. ☐Edema ☐Murmurs enter text. ☐Palpitations Click or tap here . ☐Faintness . ☐OC Changes Click or tap here . ☐Claudications Click or tap here . ☐PND . ☐Other: . MSK GI GU PSYCH ☐Pain enter text. ☐Nausea/Vomiting . ☐Urgency . ☐Stress .☐Stiffness . ☐Crepitus . ☐Swelling . ☐Limited ROM ☐Redness . ☐Misalignment . ☐Other: enter text. ☐Dysphasia enter text. ☒Diarrhea : 3-4 times approx. 5 days ago ☒Appetite Change : decreased ☐Heartburn enter text. ☐Blood in Stool . ☐Abdominal Pain . ☐Excessive Flatus . ☐Food Intolerance . ☐Rectal Bleeding . ☒Other: Last BM 5 days ago ☐Dysuria . ☐Burning . ☐Hematuria . ☐Polyuria . ☐Nocturia . ☐Incontinence Click or tap here . ☒Other: darker color and decreased output ☐Anxiety . ☐Depression . ☐Suicidal/Homicidal Ideation ☐Memory Deficits Click or tap here . ☐Mood Changes Click or tap here . ☐Trouble Concentrating Click or . ☐Other: . GYN ☐Rash ☐Discharge ☐Itching ☐Irregular Menses ☐Dysmenorrhea ☐Foul Odor ☒Amenorrhea menopause ☒LMP: approx. when 54 years old ☒Contraception : not currently using ☒Other:Last pap smear about 10 years ago; currently sexually active with 1 man Body System Positive Findings Negative Findings General O: Objective Information gathered during the physical examination by inspection, palpation, auscultation, and palpation. If unable to assess a body system, write “Unable to assess”. Document pertinent positive and negative assessment findings. Some mild weakness/fatigue noted over last week r/t current issues N/A Skin Dry skin No lesions, discoloration, or abnormalities noted; no tenting HEENT N/A Normocephalic and atraumatic; nares pink and moist on inspection. Respiratory N/A Lungs auscultated anteriorly and posteriorly, clear and without shortness of breath. No adventitious lung sounds noted. Neuro Cardiovascular N/A Heart sounds auscultated aortic, pulonic, Erb’s point, tricuspid and mitral- clear S1 and S2, without abnormal heart sounds. No edema noted in bilateral lower extremeties Musculoskeletal Gastrointestinal Left lower quadrant tender on light and deep palpation with guarding; fecal mass noted in rectal canal. Auscultation: RLQ, RUQ, LUQ, and LLQ- normoactive Abdominal arteries renal, iliac, and femoral- bilaterally- no bruit noted; abdominal aorta- no bruit Spleen and Liver: no friction rub Percussion: abdomen- some areas dull, some tympanic Spleen- tympany Liver- between 6 and 12 cm Did not react to CVA tenderness Palpation: RLQ, RUQ, LUQ- nonreactive and nontender Aortic width 3cm or less; Liver palpable, spleen nonpalpable Genitourinary N/A Bladder nonpalpable; kidneys nonpalpableProblem List 1. Constipation 6 11 2 . Abdominal Pain 7 12 Diagnostics: List tests you will order this visit Test Rationale/Citation CT abdomen Patients who present with acute abdominal pain with unknown origin, it can help diagnose an Psychiatric Gynecological N/A No abnormal findings on pelvic exam Diagnosis ICD-10 Code Pertinent Findings Left Lower Quadrant Pain R10.32 LLQ pain on palpation Constipation K59.00 Fecal Mass in rectal canal Abdominal Pain, uncertain cause R10.30 Pt complain of diffuse abdominal pain P: Plan Address all 5 parts of the comprehensive treatment plan. If you do not wish to order an intervention for any part of the treatment plan, write “None at this time” but do not leave any heading blank. No intervention is self-evident. Provide a rationale and evidence-based in-text citation for each intervention. A: Assessment Medical Diagnoses. Provide 3 differential diagnoses which may provide an etiology for the CC. The first diagnosis (presumptive diagnosis) is the diagnosis with the highest priority. Provide the ICD-10 code and pertinent findings to support each diagnosis.underlying issue; this test is used as a screening test and is reliable, accurate, valid, and causes minimal discomfort (Bax, Macha, & Mayberry, 2019). CMP If CT requires IV contrast, this will ensure the safety of the patient’s kidneys. Medications: List medications/treatments including OTC drugs you will order and “continue previous meds” if pertinent. Drug Dosage Length of Treatment Rationale/Citation Ducosate Sodium (Colace) 100 mg PO daily Until constipation resolves, then PRN Acute constipation can be a result of abdominal issues and once resolved, constipation may not be an issue. Continue previous medications Referral/Consults: Gastroenterology Rationale/Citation If CT shows diverticulosis or diverticulitis, Education: Diet Rationale/Citation Education on high fiber foods can assist with decreased constipation Follow Up: Indicate when patient should return to clinic and provide detailed instructions indicating if the patient should return sooner than scheduled or seek attention elsewhere. 1 week Rationale/Citation Follow up after CT if indicated, unless follow up with GI specialist needed. References Include at least one evidence-based peer-reviewed journal article which relates to this case. Use the correct APA 6th edition formatting. Bax, T., Macha, M., & Mayberry, J. (2019). The utility of CT scan for the diagnostic evaluation of acute abdominal pain. The American Journal of Surgery, 217(5), 959–966. https://doi-org.chamberlainuniversity.idm.oclc.org/10.1016/j.amjsurg.2019.02.003 [Show More]
Last updated: 2 years ago
Preview 1 out of 7 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$17.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Jun 07, 2020
Number of pages
7
Written in
Additional information
This document has been written for:
Uploaded
Jun 07, 2020
Downloads
0
Views
71