HESI Critical Care Exit STUDY GUIDE 2020/2021
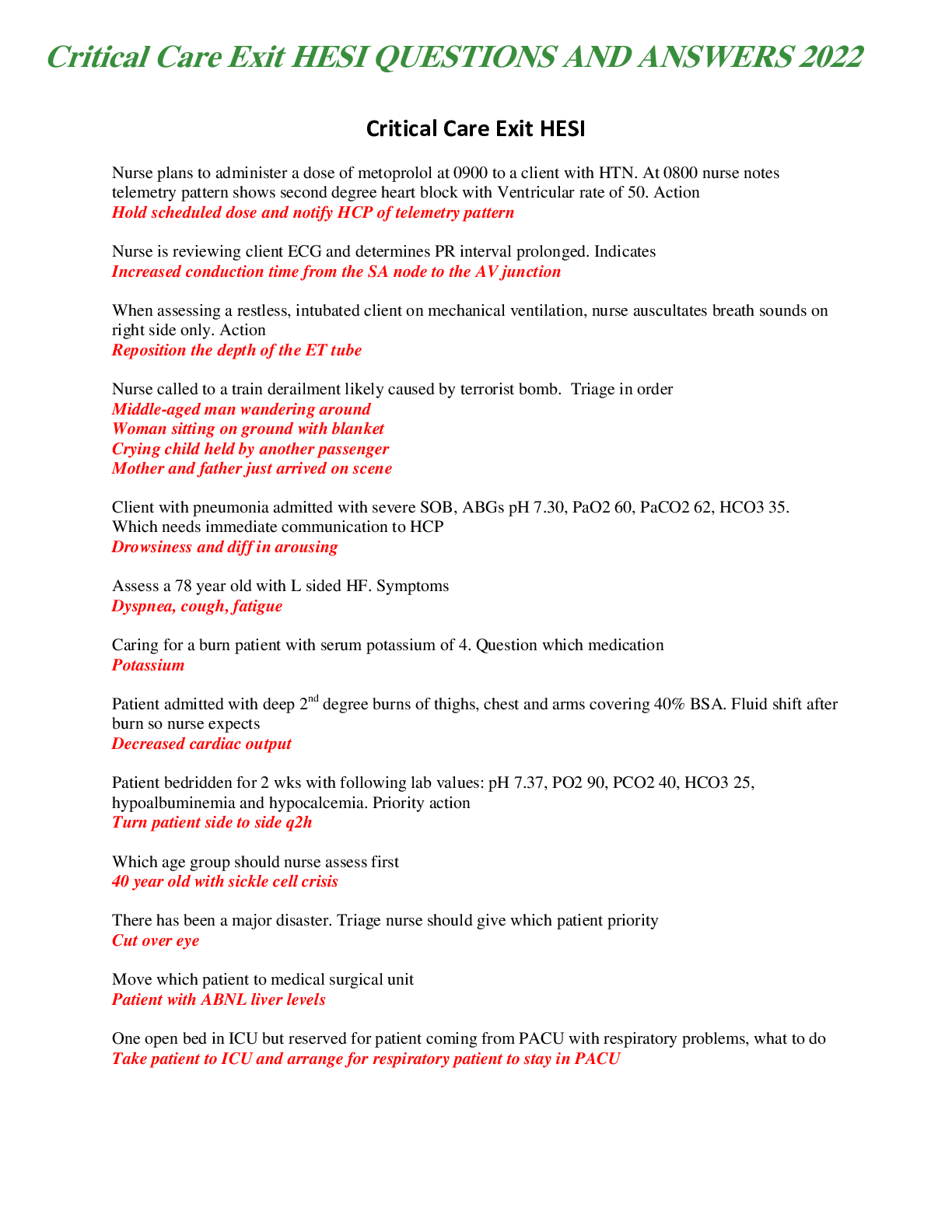
Nurse is reviewing client ECG and determines PR interval prolonged. Indicates
Determine the following acid-base disorders
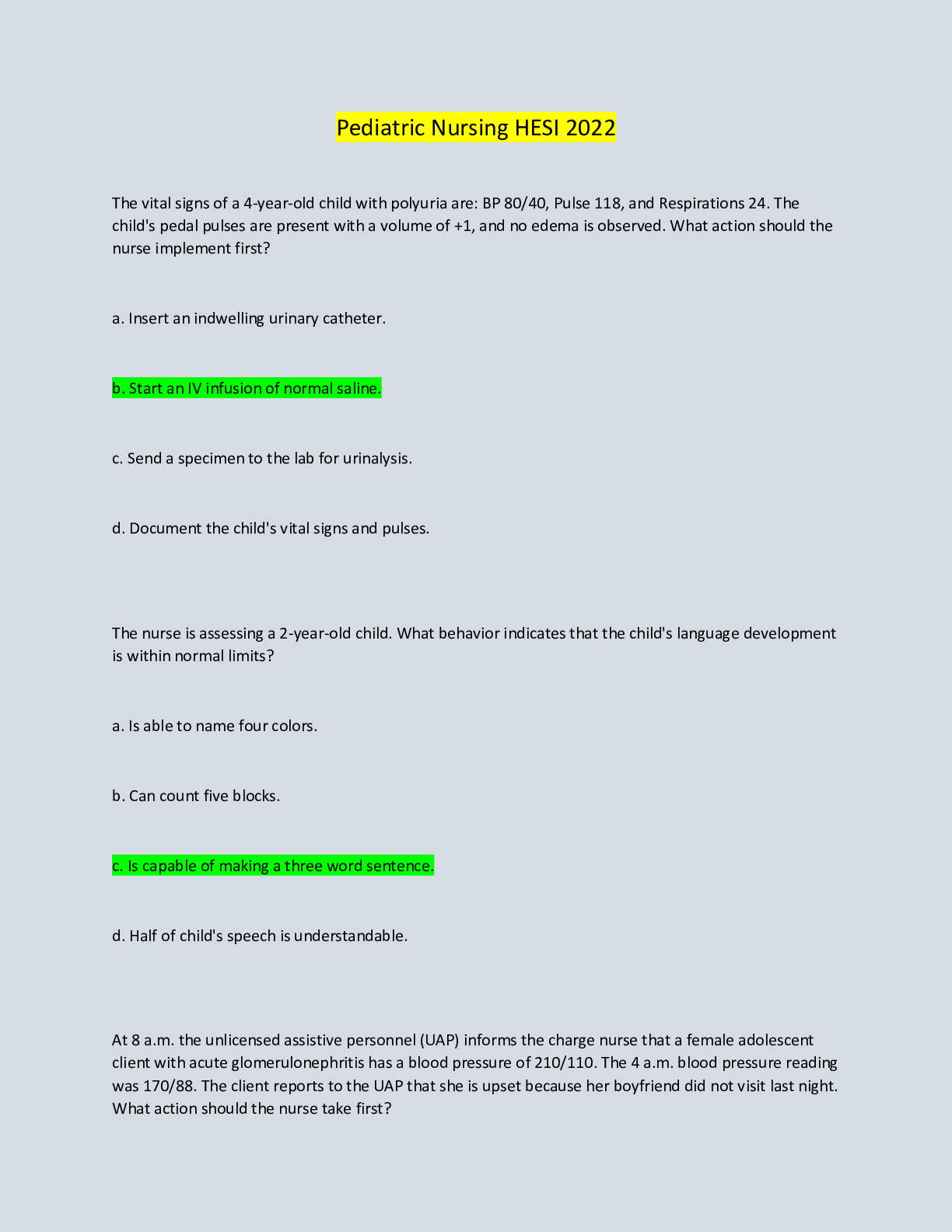
Assess a 78 year old with L sided HF. Sym
...
HESI Critical Care Exit STUDY GUIDE 2020/2021
Nurse is reviewing client ECG and determines PR interval prolonged. Indicates
Determine the following acid-base disorders
Assess a 78 year old with L sided HF. Symptoms
Caring for a burn patient with serum potassium of 4. Question which medication
Patient admitted with deep 2nd degree burns of thighs, chest and arms covering 40% BSA. Fluid shift after burn so nurse expects
Patient bedridden for 2 wks with following lab values: pH 7.37, PO2 90, PCO2 40, HCO3 25, hypoalbuminemia and hypocalcemia. Priority action
Which age group should nurse assess first
There has been a major disaster. Triage nurse should give which patient priority
Move which patient to medical surgical unit
One open bed in ICU but reserved for patient coming from PACU with respiratory problems, what to do
Carotid picture
Someone with wound vac how to make sure it is effective
Magnesium antidote
Patient having trouble swallowing when wife gives drink of water
Chest tube becomes disconnected
Patient in ventricular fibrillation
Know calcium levels….there was a question with calcium 5.0 and the answer was patient with hyperthyroidism taking inderal (propanalol)
Chest tube volume 125
Heart sounds audio
Patient on benzos
???
4 patients-which one more concern
4 patients with conditions of concern-priority
Patient on Heparin going for surgery in a.m.,-priority
Patient with fever of 101-best nursing Dx
Listening and hearing silence, then kortokoff sound what to do
Patient with pancreatitis and elevated liver function-what expect of patient
When assessing a restless, intubated client on mechanical ventilation, nurse auscultates breath sounds on right side only. Action
Nurse called to a train derailment likely caused by terrorist bomb. Triage in order
Client with pneumonia admitted with severe SOB, ABGs pH 7.30, PaO2 60, PaCO2 62, HCO3 35. Which needs immediate communication to HCP
Patient with dark, tarry stool
Sign of GI bleed, pick NSAIDS
Patient receiving Morphine in PCA pump
Make sure the lock is on the machine
Vasopressin
Vasoconstrictor
Patient comes in with Hx of MRSA
put in isolation, get swabs
Patient with thick secretions
increase fluids
Chronic renal failure-S/S
Patient would get a black tag during a disaster if he/she exhibited which S/S Know your shocks S/S (hypovolemic, cardiogenic, etc-1 Q for each)
2 RNs must check blood products together before administration
Glasgow Coma Scale
<8 = coma
Myasthenia crisis vs. cholinergic crisis
Myasthenia-weakness with change in vitals (give more med)
Cholinergic crisis-weakness with no change in vitals (reduce med)
Diabetic ketoacidosis
Fruity breath
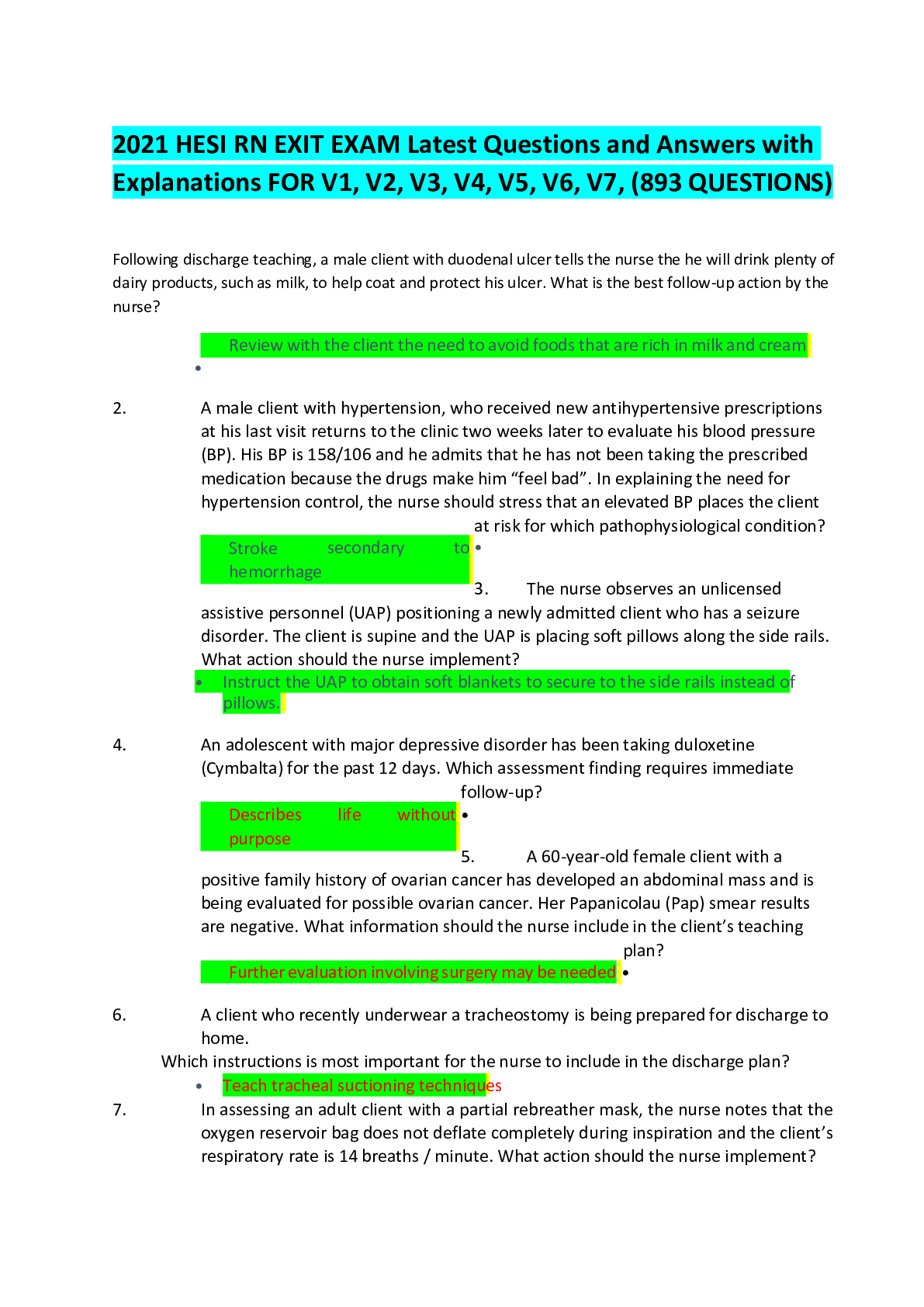
Hold Digoxin for HR <60 Stroke
Tongue points toward side of lesion (paralysis), uvula deviates away from the side of the lesion
(paralysis)
Pulmonary air embolus prevention
Trendelenburg (HOB down) and on left side to trap air in the right side of the heart
Head trauma and seizures
Maintain airway is primary concern
Hypoventilation
Acidosis (too much CO2)
Hyperventilation
Alkalosis (too little CO2)
Cardiac enzymes that you need to know how often to assess after initial CVA
Troponin (1 hour), CKMB (2-4 hrs), Myoglobin (1-4 hrs), LDH1 (12-24 hrs)
MI treatment
Morphine, oxygen, nitro, ASA (NO digoxin, betablockers or atropine for these patients)
Ventilators
Make sure the alarms are on (Check every 4 hours minimum), when suctioning give 100% O2 before and after and make no more than 3 passes-no longer than 15 seconds
Have to put in order of consideration to be delivered
Nasal cannula, simple face mask, nonrebreather mask, partial rebreather mask, venturi mask
Early signs of cerebral hypoxia
Restlessness and irritability
Necessary for Blood Product infusions
18-19 gauge needle with filter tubing
NS only run with blood within 30 minutes of hanging
Check vitals before infusing, at 15 minutes, 30 minutes, then every hour, and directly after
Checking blood before infusing
2 RNs
Check order (expiration date, clots, color, air bubbles, leaks) patient, product, previous transfusion Hx
Premedicate with Benadryl for previous rxn
What does the PR interval represent
Time required for the impulse to travel from atria through the AV node
Isotonic solutions
D5W NS
Lactated ringers
Tracheostomy
Keep Kelly clamp and obturator at the bedside
To assess CVA for hemorrhagic or ischemic
CT scan first
Heart conditions related to thrombus formation
A-fib and A-flutter
Aphasia, agraphia, slow, cautious, anxious, memory ok
Left hemisphere lesion
Cannot recognize faces, loss of depth perception, impulsive behavior, poor judgement, constant smile, loss of tonal hearing
Right hemisphere lesion
Most important indicator of increased ICP
Change in LOC
Spinal shock
Complete loss of all reflexes
If the U wave is most prominent what condition
hypokalemia
Burns
First degree- epidermis {superficial}
Second degree- epidermis and dermis {deep partial}
Third degree- epidermis, dermis, and subQ {full thickness}
Pic of patient and description of burns, need to decide what % burned
[Rule of 9s- head and neck=9%, UE=9% each, LE=18% each, front trunk=18%, back trunk=18%]
5 Ps of neurovascular status (important with fractures)
Pain, pallor, pulse, paresthesia, paralysis
S/S of shock
Increased pulse and decreased BP
S/S of IICP
Decreased pulse and increased BP with changes in LOC
Suspected Post op bleeding if assess
Frequent swallowing, vomiting blood, clearing of throat
Primary medications given in ED for respiratory distress
Bronchodilators [Sus-phrine (Epinephrine HCI) and Theophylline (Theo-dur)]
ABG normals for the following: pH, pCO2, HCO3
pH: 7.35-7.45, pCO2: 34-45 mmHg, HCO3: 22-26 mEq/L
Calculation of the heart rate using an EKG rhythm strip
count the number of R-R intervals in the 30 large squares and multiply by 10
Intracranial hypertension from a traumatic brain injury is admitted to the trauma unit
Elevated head of bed
CPR-Arrange in other of priority Establish unresponsiveness Call for help
Assess patent airway Assess pt carotid pulses
Endometrial carcinoma receiving brachytherapy and has radioactive Cesium (Cs) loaded in a vaginal applicator
Wear a dosimeter film badge when in the client’s room
65-year-old female arrives in the ER with shortness of breath and chest pain, nurse accidentally administers 10 mg of morphine sulfate instead of 4 mg as prescribed. Later, the client's respiratory rate is 10 breaths/minute, oxygen saturation is 98%, and she states that her pain has subsided
The client would not be able to prove malpractice in court
Deep vein thrombosis on heparin protocol based on a tPTT of 65 to 95 seconds. The current PTT result is 35 seconds
Increase the rate of the heparin infusion
Calculate the rate of this rhythm strip
(It should be 90-100 depending on which set of 6 squares you use)
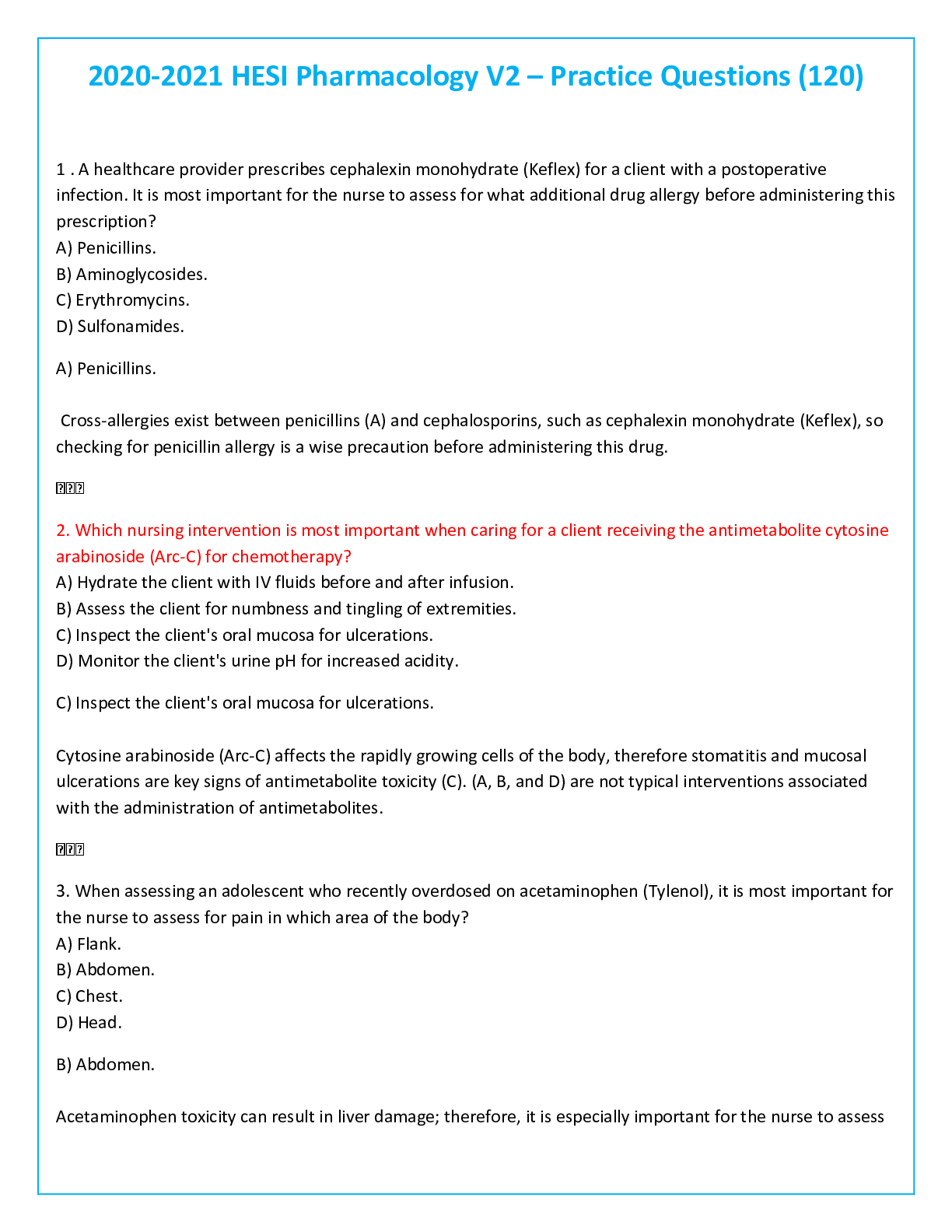
A client is admitted to the emergency room because of an overdose of acetaminophen (Tylenol)
Acetylcysteine (Mucomyst) The antidote for acetaminophen (Tylenol) is acetylcysteine (Mucomyst)
For increase magnesium level
Give calcium gluconate
Patient admitted with a Dx of diabetic ketoacidosis (DKA) with scant urinary output, K+2.5 mEq/l, pH of 7.26, T 98ºF, HR 128 bpm, RR 36, and BP 90/52
Pottasium IV at 20 mEq/250 ml over 1 hour
Irregular respiratory rate with periods of apnea lasting 10 to 15 seconds
Apply supplemental O2
The alarm of a client’s pulse oximeter sounds and the nurse notes that the oxygen saturation rate is indicated at 85%
Administer oxygen by face mask
Doing CPR on intubated client with palpable pulse during 2-min cycle of chest compressions, absent breath sounds over left lung
prepare for the endotracheal tube to be repositioned
Unresponsive client who ingested an unknown number of meperidine (DEMOROL) 50mg tablets. Naloxone (NARCAN) 0.4mg IV is administered, and the client is now responding to verbal stimuli. Which finding in the next hour requires immediate action by the nurse
Difficulty in arousing
Patient in the MICU. What problem is a client probably experiencing who has an easily obliterated radial pulse and below-normal pressures, (BP), (CVP), (PAP), and pulmonary under pressure
Hypovolemic shock
PRI interval
depolarization and repolarization
Which is the highest for carcinogenic shock
traumatic amputation from the groin down (there one of the choice a pt w/ gunshot wound to the chest and abdomen)
*HESI HINT: if Cardiogenic shock exits in the presence of pulmonary edema (ex. from pump failure), position pt to reduce venous return (high fowler’s w/ legs down) in order to reduce further venous return to the left ventricle
Patient with wrist restraints the nurse first slides two fingers under the restraints and then notes that the ties are secured to the side rail using a quick-release tie
Reposition the restraints ties, securing them to the bed frame
Nursing home patient admitted with urinary sepsis and has a single-lumen, peripherally-inserted central catheter (PICC). Four medications are prescribed for 9:00 a.m.and the nurse is running behind schedule (Zosyn) over 30 minutes q8 hours first
During a family baseball game, an adult male is hot on the head with a bat, and he is suspected of sustaining an epidural bleed
“Was your husband knocked out by the blow”
CPR for a pregnant lady
Heimlich w/ chest compression
*HESI HINT: At 20wks gestation & beyond, the gravid uterus should be shifted to the left by placing the women in a 15-30 degree angled, left lateral position or by using a wedge under her right side to tilt her to her left
Patient has received 250 ml of 0.9% normal saline through the IV line in the last hour and is now tachypneic, and has a pulse rate of 120 beats/minute, with a pulse volume of +4.
Decrease the saline to keep-open rate
In EKG reading which complex represents depolarization of the ventricles
QRS complex
The risk for metabolic shock syndrome
Toxic Shock Syndrome
23 year-old male brought to the ER by a group of fraternity brothers after a hazing event at the university. Blood alcohol level (BAL) of 3.8 and a Glasgow Coma Scale of 3
Initiate IV access using Lactated Ringer’s solution 1000ml with thiamine 100mg
The nurse in the emergency department is using the simple triage and rapid transport (START) system to assess victims of a hurricane
A yellow disaster tag means critical injuries and require immediate intervention
Electrical burn pt
put him in a cardiac telemetry monitor
A pt on a trachea/endotrach with gurgling sound
always pick suctioning
Metabolic syndrome
high cholesterol & high BP (cardiac strip)
IV Line
Flush line before and after compatible IV solution
Priority pt
Ruptured spleen life threatening
Endotrach has slipped into right main bronchus of no breath sounds are heard (Audio/Visual)
Pleaurvac, know how to set vac at 850
39 to 48 Glucose
Notify healthcare provider of client’s status
Disseminated intravascular coagulation (DIC)
best test to diagnose, D-Dimer
Septic shock-best class of medicine to give are
Anti infectives
A 6-year old boy was hit with a bat while playing at school. He has a splinter of wood imbedded in his eye
Have the parent take the child for emergency help
Patient admitted two hours ago with confusion, Kussmaul respirations, and warm, flushed skin. The healthcare provider determines the client is in acute renal failure (ARF)
Hourly neurological assessments
14-year-old male arrives at the ER in status epilepticus. He was diagnosed with a seizure disorder in childhood
Acute withdrawal from anticonvulsant medication
Most important symptom the nurse should monitor the client for while assisting with the insertion of a subclavian central venous catheter
Shortness of breath
Patient with Hx of chronic atrial fibrillation
Be sure to take the prescribed daily aspirin
Most important for the nurse to use an IV pump and/or Buretrol when initiating IV therapy after which surgical procedure
Craniotomy
Acute renal failure with a serum potassium of 7.5mEq/L. based on this finding
Administer a retention enema of Kayexalate
A client admitted to the hospital is suspected of having meningitis
Lumbar puncture
infant admitted to the NICU is tachypneic, tachycardic, and has bounding brachial pulses
Monitor for congestive heart failure
Feedings for low albumin
Nepro, Ensure or TPN if pt is NPO
BNP 500, prescribed diuretic
indicates HF
Acute Pancreatitis
withhold food and fluid intake
Mechanical life support
Know equipment used
Pulmonary Edema
Fluid leaks out of the small blood vessels into the air sacs of the lungs
CVP via PA port
Cover the cap w/ tape and label the port as being obstructed (While flushing the proximal port triple lumen central venous cath w/heparin lock meets resistance)
In EKG reading which wave represents depolarization of the atrium
P wave
Math IV
mg/kg/minute-dopamine
Allen's test
test for occlusion of the radial or ulnar artery, in which one of these arteries is compressed after blood has been forced out of the hand by clenching it into a fist; failure of the blood to diffuse into the hand when opened indicates that the artery not compressed is occluded
Pacemaker-Failure to sense
Fails to sense patient’s own intrinsic rhythm and generates a pacer spike (when output is too low resulting in failure to depolarize the ventricle results in Bradycardia **Use Atropine)
DIC
most often seen in leukemia and in adenocarcinomas of the lung, pancreas, stomach, and prostate
Diabetes -acute confusion
Give 4 oz. apple juice
Priority-compartment syndrome
Surgery needed. Emergency! Fasciotomy may be necessary
Head injury
major desired outcome for rehabilitation after head injury is to maximize the patient's ability to return to his or her highest level of functioning
Pulmonary embolism-S&S
Dyspnea, sudden onset Pleuritic chest pain Apprehension, restlessness Feeling of impending doom Cough Hemoptysis Tachypnea Crackles Pleural friction rub Tachycardia S3 or S4 heart sound Diaphoresis Fever, low-grade Petechiae over chest and axillae Decreased arterial oxygen saturation (Sao2)
Subcutaneous emphysema is felt as a crackling sensation beneath the fingertips MODS (Multiple Organ Dysfunction Syndrome) after an Abdominal Gunshot wound Apply pressure & keep flat
Ventilator-ET
to check placement listen to breath sounds
Anaphylactic-bracelet
patient should wear bracelet stating he is allergic to certain medication
Shock –hemorrhagic
give isotonic 0 .9% NS or LR
Heat stroke
increase IV fluids to 200ml/hr, apply cool packs to persons body
CPR-absent lung sounds
ventilate with two mouth to mouth breaths over 1 second and make the chest rise then palpate for pulse, if no pulse do CPR
Myxedema coma S&S
hypothermia, bradycardia, hypotension, res. Acidosis. Happens when patient suddenly stops taking thyroid med. Give thyroid replacement meds, Airway must be kept open
Burn
airway, administer LR, premedicate with sulfamylon
CVA – Anosognosia
lack of awareness or a denial of a neurological defect paralysis
Patient in cardiac arrest and monitor shows pulseless VT
Defibrillation with 200 to 360 joules
Identify the waveforms found in a normal EKG
P wave, QRS complex, T wave, ST segment, PR interval
Nurse plans to administer a dose of metoprolol at 0900 to a client with HTN. At 0800 nurse notes telemetry pattern shows second degree heart block with Ventricular rate of 50. Action
Hold scheduled dose and notify HCP of telemetry pattern
[Show More]