Second-Line Therapy
If the patient continues to have insomnia with first-line treatments, alternatives include switching to a benzodiazepine agent
or using the other benzodiazepine receptor agonist, zolpidem.
Again, t
...
Second-Line Therapy
If the patient continues to have insomnia with first-line treatments, alternatives include switching to a benzodiazepine agent
or using the other benzodiazepine receptor agonist, zolpidem.
Again, the prescriber must consider the kind of sleep defect being
treated and select a drug with the appropriate onset and half-life.
Third-Line Therapy
The practitioner should reassess the insomnia situation for
patients who fail to respond to both first- and second-line
therapies. Insomnia that has become chronic benefits most
from continual evaluation and behavioral therapy along
with the smallest dose possible of hypnotic medication. An
antidepressant may play a key role at this level.
Special Population Considerations
Pediatric
Use of barbiturates in the pediatric population is usually limited to those who have seizure disorders. In general,
Arcangelo_Chap42.indd 661 10/8/2011 2:19:59 PM
662 UNIT 9 | PHARMACOLOGY FOR NEUROLOGICAL/PSYCHOLOGICAL DISORDERS
benzodiazepines are not indicated for children younger than
age 15. Caution is necessary when very young patients use
antihistamines because of potential delirium or paradoxical
excitation. Melatonin may be considered as treatment for a
limited time (Ivanenko, et al., 2003).
Geriatric
It is important to evaluate the geriatric patient for underlying
comorbidities that contribute to insomnia. Treating the underlying illnesses is important and may assist with re-establishing
good sleeping patterns. Extreme caution is essential when prescribing hypnotic medications to elderly patients because these
drugs can increase the potential for delirium and subsequent
falls. In 1996, Zisselman, et al., analyzed hospital costs for the
elderly when sedative-hypnotics were used to promote sleep.
They found a statistically significant increase in cost resulting from increased length of hospital stay for patients who
took sedative-hypnotics. In 1990, Shorr, et al., analyzed the
quantity of prescriptions given to elderly patients along with
the number of refills. Their concern was the overuse of the
agents and the risks at which they place elderly patients over
time. They found that many different physician groups were
overprescribing sedative-hypnotics.
Consistent monitoring of the elderly patient can be
extremely important, especially when a long-acting hypnotic is
prescribed. Antihistamines can cause delirium or paradoxical
excitation.
Women
No sex differences exist in terms of the pharmacokinetics of
the various agents used to treat sleep disorders. Caution is
essential when prescribing all drugs to lactating women and
women of childbearing age. Both antihistamines and zaleplon
are pregnancy category C, whereas the barbiturates and benzodiazepines are pregnancy category D. Zolpidem, in category B,
is in the lowest-risk pregnancy category.
MONITORING PATIENT RESPONSE
Sleep can be a reliable predictor of psychological and physical health. Differences in monitoring are related to whether
the insomnia is an acute or chronic problem. Brief episodes of
acute insomnia can warrant treatment, with the goal of preventing it from progressing and becoming chronic. A short
course (up to 4 weeks) of sedative-hypnotic therapy is the current treatment of choice. Cognitive therapy can be included to
improve the chance of an optimal response.
When insomnia becomes a chronic problem, consistent
interaction between the patient and health care provider is
important, as is the use of behavioral techniques. With chronic
insomnia, issues of drug tolerance for the older benzodiazepines and rebound insomnia usually become paramount.
Current U.S. Food and Drug Administration guidelines allow only short-term prescription of hypnotic agents.
National Center on Sleep Disorders Research (NCSDR)
http://www.nhlbi.nih.gov/about/ncsdr
National Heart, Lung, and Blood Institute (NHLBI)
Health Information Network
http://www.nhlbi.nih.gov
Restless Legs Syndrome Foundation
http://www.rls.org
Sleep Foundation
http://sleepfoundation.org
BOX 42.4
Sleep Websites
Tolerance and rebound insomnia have been cited as problems
associated with these agents, but few studies have borne this
out. In practice, many people take low-dose hypnotic agents
for long periods with few side effects. Caution is warranted,
however, if a patient requires escalation of a previously stable dosage. Careful analysis of changes in the patient’s sleep
patterns is necessary in this event.
Patient Education
Patient education plays a key role in the treatment of insomnia.
A key side effect of most hypnotic agents is excessive drowsiness or hangover from the medication. The clinician must alert
the patient to this possibility and monitor the side effects of
each agent prescribed. (See Table 42.1 and Table 42.2.)
Patient-Oriented Information Sources
Major sleep centers across the country have websites that are
useful resources for patients and health care providers. These
sites can provide information about diagnosis of sleep disorders
and current research and therapies (Box 42.4).
Nutrition/Lifestyle Changes
Good sleep habits include setting a routine bedtime, getting
regular exercise, using the bed for sleeping only, and getting
in bed only when ready for sleep. Stimulants such as caffeine,
alcohol, and excess fluids should be avoided before bedtime.
Complementary and Alternative Medications
Herbs and botanicals are often used as a “natural” way of promoting sleep. However, this is not without a certain danger,
especially if these treatments are taken in conjunction with
prescription drugs. Older patients are often likely to use herbal
treatments: in 1997, it was reported that up to 3 million individuals over age 65 use such therapy (Desai & Grossberg, 2003).
Melatonin, an endogenous hormone, is synthesized
by the pineal gland from tryptophan. It is mainly secreted
at night and its level peaks during normal sleep hours. In
Arcangelo_Chap42.indd 662 10/8/2011 2:19:59 PM
CHAPTER 42 | INSOMNIA AND SLEEP DISORDERS 663
1997, Lavie discovered that endogenous melatonin opens
the nocturnal sleep gate and increases nocturnal melatonin
secretion. Melatonin does not induce sleep but acts as a
gatekeeper in the cascade of events that enables the CNS
to favor sleep over wakefulness. Most studies have examined
the use of melatonin to treat sleep disorders resulting from
jet lag; few have looked at the use of melatonin in primary
insomnia. A 1996 study by Attenburrow and Dowling on
melatonin and primary insomnia examined healthy volunteers compared with the elderly. Through analysis of urine
concentrations of endogenous melatonin, the study found
that the elderly volunteers had a lower concentration of the
melatonin metabolite and a delayed onset to peak secretion.
These findings supported the possibility that some patients,
especially those with delayed sleep phase insomnia, may benefit from the administration of exogenous melatonin; however, further study is necessary.
Valerian is a traditional sleep remedy that is derived from
the perennial herb Valeriana officinalis. The direct physiologic
activity is mediated by the active sesquiterpene components
of the volatile oil. This creates a synergistic effect with neurotransmitters such as GABA and produces a direct sedative
effect. Effective dosage ranges from 300 to 600 mg of the valerian root; 2 to 3 g of the dried root is soaked in a cup of hot
water for 10 to 15 minutes, and the patient then drinks the
tea. Administration can occur 30 minutes to 2 hours before
bedtime. Significant herb or drug interactions have not been
reported by the German E Commission.
RESTLESS LEG SYNDROME AND
PERIODIC LIMB MOVEMENT
DISORDER
Restless leg syndrome (RLS) and periodic limb movement
disorder (PLMD) are neurologic disorders. RLS is characterized by an intense need to move the legs, accompanied by
paresthesias and dysesthesias that worsen usually in the evening. Sometimes the sensations can occur in other large muscle
groups, but most often the legs are involved. Moving around
relieves the feeling, but only for a short time, as the sensation
soon returns. These sensations interfere with sleep. PLMD is
characterized by episodes of highly repetitive and stereotyped
limb movements only during sleep.
Both disorders interfere with sleep and contribute to sleep
deprivation and decreased alertness and daytime function.
Indications are that 2% to 15% of the population may experience RLS, but the diagnosis is made rarely in primary care.
CAUSES
As a primary CNS disorder, RLS can be found in patients with
end-stage renal disease, anemia, and sometimes in pregnancy
(Gigli et al., 2004). RLS can also be hereditary or drug induced.
1. A compelling urge to move limbs associated with
paresthesias/dysesthesias
2. Motor restlessness as evidenced by:
• Floor pacing
• Tossing and turning in bed
• Rubbing legs
3. Symptoms worse or exclusively present at rest
with variable and temporary relief by activity
4. Symptoms worse in the evening and at night
BOX 42.5
Diagnostic Criteria for
Restless Leg Syndrome
Allen (2004) argued that iron deficits may be a strong cause of
RLS, altering the iron–dopamine linkage, but this hypothesis
needs further study.
PATHOPHYSIOLOGY
RLS and PLMD are sensory-motor disorders that are not
well understood. Primary RLS has a strong hereditary component, with 40% to 60% of patients having a familial association. Onset of familial RLS is before the age of 30 years,
and studies have indicated the strong action of a single major
gene (Zucconi & Ferini-Strambi, 2004). Secondary RLS can
be associated with neuropathies from changes in axonal and
small-fiber neural pathways. Patients with rheumatoid arthritis and diabetes also have shown a greater prevalence of RLS,
again presumably from changes due to neuropathy. Parkinson’s
disease is frequently associated with RLS, pointing to a commonality in reduced dopaminergic functioning (Zucconi &
Ferini-Strambi, 2004). A strong link has been established to
the dopaminergic system by the positive response to the dopaminergic agonist classification of drugs (Allen, 2004).
DIAGNOSTIC CRITERIA
RLS is diagnosed primarily through the patient history. Clinical
criteria have been established by the International Restless Legs
Syndrome Study Group (Box 42.5).
PLMD is associated more with stereotyped repetitive
movements of limbs (legs alone, or legs more than arms) that
occur only during sleep. PLMD is generally diagnosed only
through a sleep test.
The physical examination for RLS and PLMD should
include a full neurologic examination with emphasis on the spinal cord and peripheral nerve function. A vascular examination
is also necessary to rule out vascular disorders. Secondary causes
of RLS should be evaluated by a serum ferritin level and serum
Arcangelo_Chap42.indd 663 10/8/2011 2:19:59 PM
664 UNIT 9 | PHARMACOLOGY FOR NEUROLOGICAL/PSYCHOLOGICAL DISORDERS
chemistry to rule out uremia and diabetes. Polysomnography is
not routinely indicated for RLS but can be helpful to establish
the diagnosis. Box 42.6 lists other possible diagnoses.
INITIATING DRUG THERAPY
Pharmacotherapy should be tailored for each patient. Patients
with relatively mild symptoms may not need medications.
Nonpharmacologic therapy should be instituted, including
mental alerting activities and cessation of alcohol, nicotine, and
caffeine. Any medications that may precipitate or worsen RLS
symptoms, such as antidepressants and dopamine antagonists,
should be avoided. Correction of underlying serum iron deficits may be helpful. Short-term studies have shown that drug
therapy has significant benefits, but little is known about longterm treatment. A 3-year study of 70 patients by Clavadetscher
et al. (2004) found that a good long-term response with drug
therapy can be achieved in 80% of patients. This study helped
to establish the benefit of pharmacologic therapy in RLS.
Goals of Drug Therapy
The goal of drug therapy is to calm the restless legs or periodic
limb movements. Some patients can be refractory to pharmacologic treatment but still achieve partial relief of their symptoms.
Pharmacologic agents for RLS include dopaminergic agents,
dopamine agonists, opioids, benzodiazepines, anticonvulsants,
and iron. (See Table 42.1.) Other than dopamine agonists,
many of these drugs are being used in an “off-label” manner.
Dopaminergic Agents
These drugs are dopamine precursor combinations such as
carbidopa–levodopa (Sinemet). These agents are useful for intermittent RLS because they have a quicker onset than dopamine
agonists. This is useful for relief of sleep onset insomnia and
1. Nocturnal leg cramps
• Painful, palpable involuntary muscle contractions
• Focal with sudden onset
• Unilateral
2. Akathisia
Excessive movement without accompanying sensory complaints
3. Peripheral neuropathy
• Usually tingling, numbness, or pain sensations
• Not associated with motor restlessness
• Not helped by movement
• Evening or nighttime worsening
BOX 42.6
Differential Diagnoses
for RLS and PLMD
RLS that occurs during long car or airplane journeys. Dosage of
these agents is lower than used for Parkinson’s disease.
Adverse Events
The carbidopa–levodopa agents may actually worsen RLS symptoms in up to 80% of patients. The therapeutic effect may be
reduced if taken with high-protein food. Insomnia, sleepiness,
and gastrointestinal problems are other adverse events.
Dopamine Agonists
The initial dopamine agonists used for RLS were bromocriptine and pergolide, which were prone to side effects. The newer
dopamine agonists, such as pramipexole and ropinirole, are not
ergot based; while they have fewer side effects, they can cause
initial nausea and lightheadedness, nasal stuffiness, edema, and
rarely daytime sleepiness. Increasing the dose slowly will help
to mitigate these side effects.
Opioids
Opioids are reserved for the most severe cases of RLS or
PLMD that are refractory to treatment with other pharmacologic agents. This class of medications can be used on a daily or
intermittent basis. Clinical experience by sleep experts suggests
that only a few patients will require opioids (Silber, 2004).
Benzodiazepines
Benzodiazepines (see Table 42.1) are used concomitantly
with a dopamine agonist when use of a sole agent has failed.
Clinical experience is particularly crucial with clonazepam and
temazepam. These drugs may be helpful for patients who cannot tolerate the other medications. Caution is necessary when
using these agents with the elderly, and they can cause daytime
sleepiness and cognitive impairment.
Anticonvulsants
Anticonvulsants are considered when dopamine agonists have
failed and in patients who describe the RLS discomfort as pain.
Gabapentin is helpful in patients with RLS and peripheral neuropathy. It is useful in treatment of daily RLS. As with the dopamine agonists, lower dosages of gabapentin (100 to 600 mg one
to three times daily) can be successful. The side effect of hypersomnia often limits the dosage. Other side effects can include nausea,
sedation, and dizziness. See Chapter 39 for further discussion.
Selecting the Most Appropriate Agent
For treatment purposes, RLS can be classified as intermittent
(not often enough to require drug therapy), daily (troublesome
enough to require drug therapy), and refractory (not adequately
treated by a dopamine agonist). The ideal agent will minimize
or abate the symptoms of RLS. No one pharmacologic agent
appears to help all patients, and often a combination of medications is needed. The severity of RLS can vary, and pharmacologic
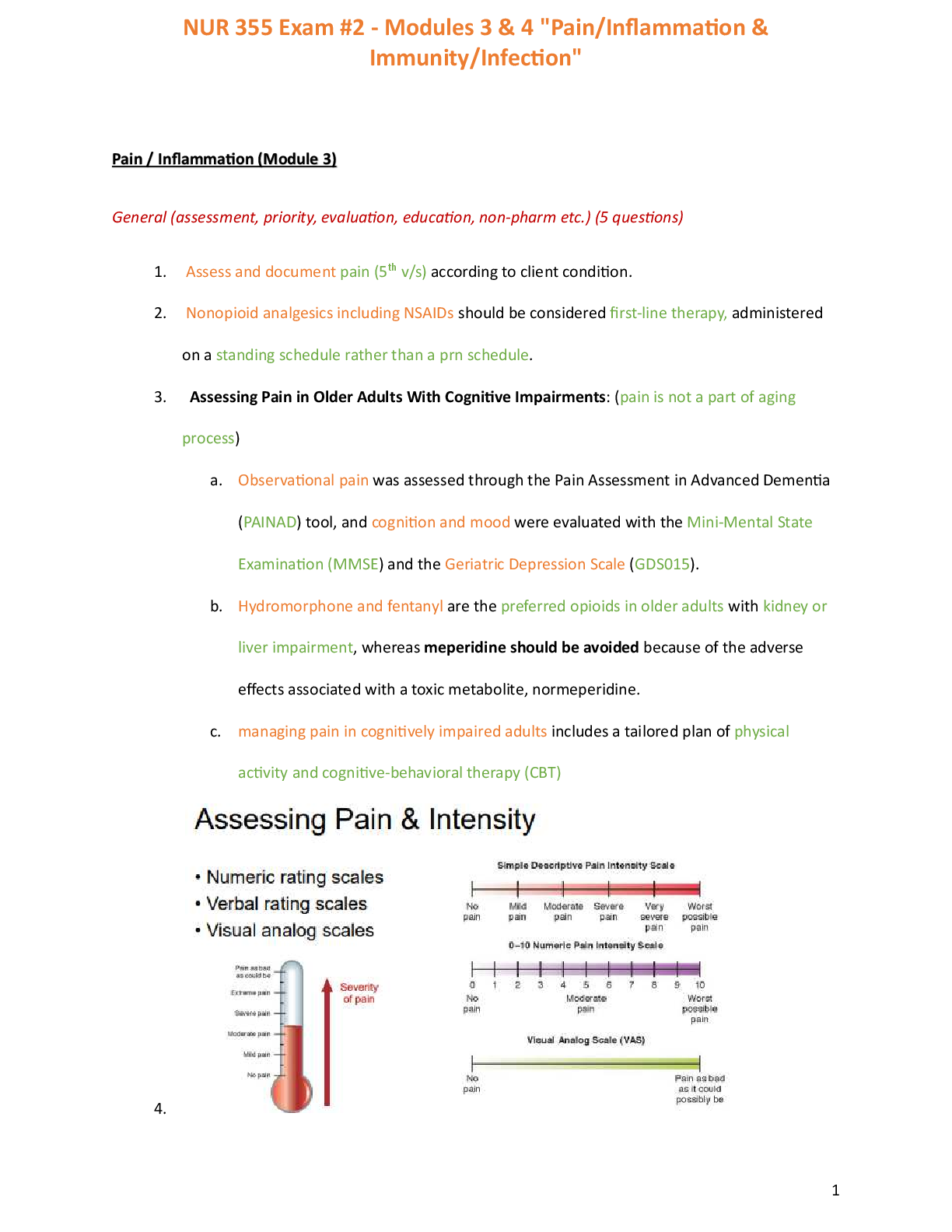
treatment needs to be individualized. See Box 42.7 for considerations when selecting a pharmacologic agent (Figure 42-2).
Arcangelo_Chap42.indd 664 10/8/2011 2:19:59 PM
CHAPTER 42 | INSOMNIA AND SLEEP DISORDERS 665
Age of patient Benzodiazepines can cause cognitive impairment in elderly.
Severity of symptoms Mild symptoms: no medication, or levodopa or dopamine a gonist
Severe symptoms: strong opioid
Frequency/regularity of symptoms Patients with infrequent symptoms may benefit from prn medication.
Presence of pregnancy No safety and efficacy clinical trials on treatment of RLS with medications
in pregnancy
Renal failure Need to decrease dosage if drugs are renally excreted
Considerations in Pharmacologic Agent Selection in RLS
BOX 42.7
Identification of symptoms:
"Creepy, crawly feeling"
worse at night
Must walk to relieve
symptoms
H & P
Labs: CBC, ferritin level
(treat low iron)
Review medications
Intermittent
symptoms
Persistent
symptoms
Persistent with
neuropathy
Refraction
symptoms
Change to a different
dopamine agonist
Add low-dose
opioid
Treat prn
with carbidopa/
levodopa
Trial dopamine
agonist:
ropinirole,
pramixole
Gabapentin
Key Starting point for decision making Clinial actions (assessing, prescribing, monitoring) Decision point
FIGURE 42–2 Algorithm for treatment for RLS.
Arcangelo_Chap42.indd 665 10/8/2011 2:19:59 PM
666 UNIT 9 | PHARMACOLOGY FOR NEUROLOGICAL/PSYCHOLOGICAL DISORDERS
First-Line Therapy
Dopaminergic antagonists such as low-dose carbidopa–
levodopa should be reserved for patients with intermittent
RLS. The first choice of therapy for daily RLS is one of the
dopamine agonists. The largest placebo-controlled trial has
been conducted on ropinirole (Requip) (Trenkwalder, et al.,
2004). Other medications in this class include pramipexole
(Mirapex). Nausea, dizziness, dyskinesia, and somnolence are
potential side effects of both the dopaminergic antagonists
and agonists.
Second-Line Therapy
Pharmacologic agents approved for neuropathic pain such
as gabapentin (Neurontin) can be used alone or in conjunction with other agents. It is especially helpful for patients who
describe RLS symptoms as painful. Other anticonvulsant
agents such as carbamazepine (Tegretol) can be considered,
but the older agents carry an increased risk of side effects such
as dizziness, drowsiness, and lack of coordination. Patients also
may experience nausea with these older agents. An opioid or
opioid receptor agonist, tramadol (Ultram), may be added or
used alone at low doses. If either the anticonvulsant or opioid
fails, a repeat trial of dopamine agonists should be attempted
(Silber, 2004).
Third-Line Therapy
Patients who continue to have symptoms may be refractory
to treatment. Therapeutic doses may not have been obtained,
or the patients could not tolerate the side effects of the medications. Substitution of different medications in the dopamine agonist class or adding higher-potency opioids should
be considered. Consultation with a sleep specialist should be
considered.
Monitoring Patient Response
Most patients will have remittance of symptoms with the first
therapeutic dose of medication. This supports the theory that
dopaminergic abnormality is a cause of this disorder. Another
indicator of improvement is a decrease in excessive daytime
sleepiness from lack of REM sleep. Patients need to be monitored for side effects of the pharmacologic agents. The longterm efficacy of these pharmacologic agents is uncertain, and
monitoring for relapse of symptoms is important. It is also
important to monitor for dependence when benzodiazepines
or opioids are used.
PATIENT EDUCATION
Many patients who have RLS use OTC sleep medications,
and poor sleep hygiene may contribute to the lack of sleep
in RLS sufferers. Implementing cognitive sleep hygiene techniques may provide a modest improvement in short-term sleep
symptoms (Edinger, 2003). Patients should inform all of their
health care providers about their RLS diagnosis, and health
care providers should be aware that the patient’s inability to
keep his or her limbs still is not due to lack of cooperation.
Improper restraint of patients with this syndrome has resulted
in mortality and morbidity.
Drug Information
A higher dosage of ropinirole (Requip) is needed compared
to pramipexole (Mirapex) to achieve the same therapeutic
effect. This may contribute to side effects and tolerability of
the drug.
Patient-Oriented Information Sources
The Restless Legs’ Syndrome Foundation supports research and
provides information for patients and health care providers.
Extensive international research is also being conducted on
this serious sleep problem. (See Box 42.4.)
NARCOLEPSY
Narcolepsy is a sleep disorder caused by malfunctions in the
primary brain mechanism that induces sleep. Individuals with
narcolepsy achieve REM sleep in less than a minute, bypassing the other sleep stages. The other features of narcolepsy
include excessive daytime sleepiness, cataplexy (attacks of muscle weakness), sleep paralysis, and hypnagogic hallucinations.
Narcolepsy is the second leading cause of excessive daytime
sleepiness and has an overall incidence in the world of 0.2 to
1.6 per thousand individuals (Stanford Center for Narcolepsy,
2004). Narcolepsy can have a dramatic impact on virtually all
areas of life.
CAUSES
Narcolepsy usually starts in the second or third decade of
life, but it has been identified in children as young as age
3. Excessive daytime sleepiness or cataplexy may be the first
symptoms, but most often cataplexy is delayed 2 to 3 years.
Cataplexy attacks are often precipitated by highly specific
situations or triggers of strong emotions. Hypnagogic hallucinations can be present but are rarely the first manifestation
of narcolepsy.
PATHOPHYSIOLOGY
The pathophysiology of narcolepsy is not well understood.
It appears to be a disease where daily periods of internal
clock-dependent alerting appear to be missing. Narcolepsy
is sporadic and without a familial predisposition. Some evidence has shown a genetic component with specific human
leukocyte antigens. It is possible that hypocretin-producing
Arcangelo_Chap42.indd 666 10/8/2011 2:20:00 PM
CHAPTER 42 | INSOMNIA AND SLEEP DISORDERS 667
cells express toxins that provoke an autoimmune cascade
that triggers narcolepsy.
DIAGNOSTIC CRITERIA
The International Classification of Sleep Disorders states
that individuals with narcolepsy have excessive sleepiness,
cataplexy, sleep paralysis, and hypnagogic hallucinations (the
“narcoleptic tetrad”). Many narcolepsy patients also have
disrupted nighttime sleep and automatic behaviors. Not all
patients with narcolepsy have all symptoms of the narcoleptic
tetrad, but excessive sleepiness is present in virtually every
patient.
Silber et al. (2002) researched whether including human
leukocyte antigen (HLA) typing provides a higher reliability
of diagnosis. They used clinical and neurophysiologic data to
evaluate 69 patients in four categories: definite narcolepsy,
probable narcolepsy with two subgroups (confirmed by laboratory study), and probable narcolepsy (clinical). Seventy-four
percent of patients had a positive HLA that helped to confirm
the diagnosis of narcolepsy.
INITIATING DRUG THERAPY
There is no cure for narcolepsy, and pharmacologic therapy must be initiated to control the attacks. Evaluation for
cataplexy, hypnagogic hallucinations, and sleep paralysis is
important to identify the best agent for treatment. Most
often antidepressants are used to block the REM paralysis of cataplexy. The mainstay of pharmacologic therapy
until now has been amphetamines and amphetamine-like
drugs such as methylphenidate (Ritalin). These are used to
combat the abnormal sleepiness. Two newer pharmacologic
agents that accomplish the same effect as amphetamines
are modafinil (Provigil) and armodafinil (Nuvigil). These
agents are nonamphetamines and are classified as Schedule
IV controlled substances.
Goals of Drug Therapy
Pharmacologic therapy should be titrated to promote the
optimal dose of stimulation. The health care provider
needs to work with the patient to identify personal treatment goals such as staying awake in a classroom or social
situation or while driving. The main goal is to achieve as
normal a life as possible, staying awake in situations of
normal daily living.
Psychostimulants
Modafinil and armodafinil (the R-enantiomer of modafinil)
are psychostimulants with unique properties to promote
wakefulness. The potential for abuse of these agents is much
lower than with other stimulants, although it still needs to
be monitored. The mechanism of action of modafinil and
armodafinil is not well understood, but it appears to attenuate the central alpha-1 adrenergic system. The primary sites
of action are the subregions of the hippocampus, the centrolateral nucleus of the thalamus, and the central nucleus of the
amygdala. Modafinil can produce euphoria and psychoactive
effects similar to other CNS stimulants. Absorption of the
drug occurs rapidly, with peak plasma concentration in 2 to 4
hours and a half-life of 15 hours. Distribution of the drug is
throughout the tissues, and it is moderately bound to plasma
proteins. The drug is metabolized in the liver and excreted
in the urine. In a recent study of the long-term efficacy of
modafinil conducted by the Narcolepsy Multicenter Study
Group (Mitler, et al., 2000), the most common adverse side
effects of the drug were headache, nausea, nervousness, and
anxiety. Most side effects are mild to moderate and transient.
(See Table 42.1.)
SPECIAL POPULATIONS
Pediatrics
Modafinil has not been studied in children. The alternative
drug of choice would be methylphenidate.
Geriatrics
Care must be taken when prescribing modafinil to the
elderly population. The oral clearance of modafinil is
reduced in the elderly by 20% to 50%. Renal failure does
not influence the pharmacokinetics of the drug but does
increase the inactive metabolite accumulation. Liver impairment can reduce the modafinil clearance and double serum
concentrations.
MONITORING PATIENT RESPONSE
Narcolepsy is a life-long disease process, and patients must
use the medications for their entire lives. Patient response is
monitored by improvement in the disease’s severity. Achieving
the goals identified by the patient can help to improve
compliance.
PATIENT EDUCATION
Patients and their families need to be aware of all available
options to treat narcolepsy. Psychological distress is a consequence, not the cause, of the disease. Discussion of potential side effects of the drugs is important for compliance.
Offering counseling and support groups when necessary is
important.
Arcangelo_Chap42.indd 667 10/8/2011 2:20:00 PM
668 UNIT 9 | PHARMACOLOGY FOR NEUROLOGICAL/PSYCHOLOGICAL DISORDERS
Case Study 1
. H., age 47, reports difficulty falling asleep and
staying asleep. These problems have been ongoing for many years, but she has never mentioned
them to her health care provider. She has generally “lived
with it” and self-treated the problem with OTC Tylenol
PM. Currently she is also experiencing perimenopausal
symptoms of night sweats and mood swings. Current
medical problems include hypertension controlled with
medications. Past medical history includes childhood illnesses of measles, chickenpox, and mumps. Family history
is positive for diabetes on the maternal side and hypertension on the paternal side. Her only medication is an
angiotensin-converting enzyme inhibitor and diuretic
combination for hypertension control. She generally does
not like taking medication and does not take any other
OTC products.
DIAGNOSIS: INSOMNIA
1. List specific goals of therapy for S. H.
2. What drug therapy would you prescribe? Why?
3. What are the parameters for monitoring the success of
the therapy?
4. Discuss specific patient education based on the prescribed therapy.
5. List one or two adverse reactions for the selected agent
that would cause you to change therapy.
6. What would be the choice for second-line therapy?
7. What OTC and/or alternative medicines might be
appropriate for this patient?
8. What dietary and lifestyle changes might you recommend?
9. Describe one or two drug–drug or drug–food interactions for the selected agent.
S
Case Study 2
. F., age 73, reports a “funny sensation in my
legs at night.” To get rid of this sensation, she
has to move. She can sleep only 2 or 3 hours at
a time before the sensation wakes her up. This problem
has been ongoing from her early twenties but has steadily
worsened with age. She finds herself walking around a lot
in the early evening. She has tried to self-treat the problem with OTC Tylenol PM. Current medical problems
include hypertension, hyperlipidemia, coronary artery
disease, and depression. Family history is positive for
coronary artery disease on the paternal side. Medications
include Prinivil 10 mg qd, Zocor 40 mg qd, Lexapro
10 mg qd, and ASA 81 mg qd. She does not want to
take any more medication but wants to help her legs stop
moving at night.
DIAGNOSIS: RESTLESS LEG SYNDROME
1. List specific goals of therapy for J. F.
2. What drug therapy would you prescribe? Why?
3. What are the parameters for monitoring the success of
the therapy?
4. Discuss specific patient education based on the
prescribed therapy.
5. List one or two adverse reactions for the selected agent
that would cause you to change therapy.
6. What would be the choice for second-line therapy?
7. What OTC and/or alternative medicines might be
appropriate for this patient?
8. What dietary and lifestyle changes might you recommend?
9. Describe one or two drug–drug or drug–food interactions for the selected agent.
J
Drug Information
Patients who are switched from amphetamine stimulants to
modafinil may not experience the same euphoric effects, and this
may make the switch undesirable to the patient. Amphetamines
tend to produce a feeling of improved well-being and arousal,
while modafinil increases arousal without a change in affect.
Patient-Oriented Sources
Health care providers and patients can find information about
narcolepsy from a variety of sources. Online support groups
exist. (See Box 42.4.)
Arcangelo_Chap42.indd 668 10/8/2011 2:20:00 PM
CHAPTER 42 | INSOMNIA AND SLEEP DISORDERS 669
BIBLIOGRAPHY
*Starred references are cited in the text.
Ahmed, M. (2004). Circadian rhythm sleep disorders. [On-line.] Available:
http://sleepmed.bsd.chicago.edu/circadianrhythm.html.
*Allen, R. (2004). Dopamine and iron in the pathophysiology of restless legs
syndrome (RLS). Sleep Medicine, 5, 385–391.
Anacoli-Israel, S. (1997). Sleeping problems in older adults: Putting myths to
bed. Geriatrics, 52(1), 20–28.
*Attenburrow, M., & Dowling, B. (1996). Case-control study of evening
melatonin concentration in primary insomnia. British Medical Journal,
312 [On-line], 1263. Available: http://gw5. epnet.com.
Bateson, A. (2004). The benzodiazepine site of the GABAA receptor: An old
target with new potential? Sleep Medicine, 5(Suppl. 1), S9–S15.
Belinger, J., Fins, A., Goeke, J., et al. (1996). The empirical identification of
insomnia subtypes: A cluster analytic approach. Sleep, 19, 398–411.
Boeve, B., Silber, M., & Ferman, T. (2003). Melatonin for treatment of REM
sleep behavior disorders in neurologic disorders: Results in 14 patients.
Sleep Medicine, 4, 281–284.
*Bonnet, M., & Arand, D. (1996). The consequences of a week of insomnia.
Sleep, 19, 453.
Brostrom, A., Stromberg, A., Dahlstrom, U., & Fridlund, B. (2004). Sleep
difficulties, daytime sleepiness, and health-related quality of life in
patients with chronic heart failure. Journal of Cardiovascular Nursing,
19(4), 234–242.
Brown, D. (1999). Managing sleep disorders: Solutions in primary care.
Clinician Reviews, 9(10), 51–69.
Bruck, D. (2001). The impact of narcolepsy on psychological health and role
behaviours: Negative effects and comparisons with other illness groups.
Sleep Medicine, 2, 437–446.
Buyssee, D. (2004). Insomnia, depression, and aging: Assessing sleep and
mood interactions in older adults. Geriatrics, 59(2), 47–51.
*Clavadetscher, S., Gugger, M., & Bassetti, C. (2004). Restless legs syndrome:
Clinical experience with long-term treatment. Sleep Medicine, 5, 495–500.
Clinical Pharmacology. (2004). Melatonin. [On-line]. Available: http://www.
gsm.com.
Clinical Pharmacology. (2004) Available:. Valerian, valeriana officinalis. [On-line].
http://www.gsm.com.
*Cochran, H. (2003). Diagnose and treat primary insomnia. Nurse Practitioner,
28(9), 13–27.
Dato, C. (1999). Sleeping disorders. In J. Singleton, S. Sandowski, C. GreenHernandez, et al. (Eds.), Primary care (pp. 686–691). Philadelphia:
Lippincott Williams & Wilkins.
*Dement, W., & Vaughan, C. (1999). The promise of sleep. New York: Dell.
*Desai, A. K., & Grossberg, G. T. (2003). Herbals and botanicals in geriatric
psychiatry. American Journal of Geriatric Psychology, 11, 498–506.
Drake, C., Roehers, T., & Roth, T. (2003). Insomnia cause, consequences, and
therapeutics: An overview. Depression and Anxiety, 18, 163–176.
Dunn, S. (1998). Insomnia. In Primary care consultant (pp. 320–321). St.
Louis: Mosby.
*Edinger, J. (2003). Cognitive and behavioral anomalies among insomnia
patients with mixed restless legs and periodic limb movement disorder.
Behavioral Sleep Medicine, 1(1), 37–53.
*Everitt, D. E., Avorn, J., & Baker, M. W. (1990). Clinical decision-making in
the evaluation and treatment of insomnia. American Journal of Medicine,
89, 357–362.
*Gigli, G., Adorati, M., Dolso, P., et al. (2004). Restless legs syndrome in
end-stage renal disease. Sleep Medicine, 5, 309–315.
Gillian, J. C., & Byerley, W. (1990). The diagnosis and management of insomnia. New England Journal of Medicine, 322, 239–248.
Hauri, P. (1987). Specific effects of sedative/hypnotic drugs in the treatment
of incapacitating chronic insomnia. American Journal of Medicine, 83,
925–926.
Hauri, P. (1998). Sleep disorders: Insomnia. Clinics in Chest Medicine, 19,
157–168.
Hening, W., Walthers, A., Allen, R., et al. (2004). Impact, diagnosis and
treatment of restless legs syndrome (RLS) in a primary care population:
The REST (RLS Epidemiology, Symptoms, and Treatment) primary care
study. Sleep Medicine, 5, 237–240.
*Ivanenko, A., Crabtree, V., Tauman, R., & Gozal, D. (Jan./Feb. 2003).
Melatonin in children and adolescents with insomnia: A retrospective
study. Clinical Pediatrics, 51–58.
Karch, A. (2000). 2001 Lippincott’s nursing drug guide. Philadelphia: Lippincott
Williams & Wilkins.
Katz, D., & McHorney, C. (2002). The relationship between insomnia and
health-related quality of life in patients with chronic illness. Journal of
Family Practice, 51(3), 229. [On-line]. Available: http//www.jfponline
.com/content/2002/03/jfp_0302_00229.asp.
Kryger, M., Monjan, A., Bliwise, D., & Ancoli-Israel, S. (2004). Sleep,
health and aging: Bridging the gap between science and clinical practice.
Geriatrics, 59(1), 24–30.
Late-life insomnia: Psychiatric and medical comorbidity common. (2004).
Geriatric Psychopharmacology Update, 8(7), 1–7.
*Lavie, P. (1997). Melatonin: Role in gating nocturnal rise in sleep propensity.
Journal of Biological Rhythms, 12, 657–668.
Case Study 3
. W., age 35, mentions during a routine visit that he
has been having horrible nightmares. He states that
during the nightmares he is aware of his surroundings but just cannot seem to move. He also reports excessive
daytime sleepiness, which he cannot understand since he is
usually in bed by 10 pm and doesn’t get up until 8 am. This
has been a problem for about the past 6 months. His family
history is negative for any illnesses and sleep disorders. He
does not take any medications or OTC products routinely.
DIAGNOSIS: POSSIBLE NARCOLEPSY
1. List specific goals of therapy for D. W.
2. What drug therapy would you prescribe? Why?
3. What are the parameters for monitoring the success of
the therapy?
4. Discuss specific patient education based on the prescribed therapy.
5. List one or two adverse reactions for the selected agent
that would cause you to change therapy.
6. What would be the choice for second-line therapy?
7. What OTC and/or alternative medicines might be
appropriate for this patient?
8. What dietary and lifestyle changes might you recommend?
9. Describe one or two drug–drug or drug–food interactions for the selected agent.
D
Arcangelo_Chap42.indd 669 10/8/2011 2:20:00 PM
670 UNIT 9 | PHARMACOLOGY FOR NEUROLOGICAL/PSYCHOLOGICAL DISORDERS
Leger, D., Guilleminault, C., Biol, D., et al. (2002). Medical and socioprofessional impact of insomnia. Sleep, 25(6), 625–629.
Lindberg, E., & Gisiason, T. (2000). Epidemiology of sleep-related obstructive
breathing. Sleep Medicine Reviews, 4(5), 411–433.
Lustbader, A., Morgan, C., Pelayo, R. et al. (1997). Psychiatry: Insomnia.
In L. Rucker (Ed.), Essentials of adult ambulatory care (pp. 607–615).
Baltimore: Williams & Wilkins.
Lyznicki, J., Doege, T., Davis, R., & Williams, M. (1998). Sleepiness, driving,
and motor vehicle crashes. Journal of the American Medical Association,
279, 1908–1913.
Medical Letter of Drugs and Therapeutics. (1995). (Issue 962). Melatonin:
Therapeutic uses [On-line]. Available: http://gw5.epnet.com.
Mendelson, W., Thompson, C., & Firanko, T. (1996). Adverse reactions to
sedative/hypnotics: Three years’ experience. Sleep, 19, 702–706.
*Mitler, M., Harsh, J., Hirschowitz, M., & Guilleminault, C. (2000). Longterm efficacy and safety of modafinil (Provigil) for the treatment of excessive daytime sleepiness associated with narcolepsy. Sleep Medicine, 1,
231–243.
Morrish, E., King, M., Smith, I., & Shneerson, J. (2004). Factors associated
with a delay in the diagnosis of narcolepsy. Sleep Medicine, 5, 37–41.
National Center on Sleep Disorders Research and Office of Prevention,
Education, and Control. (1997a). Problem sleepiness in your patient.
U.S. Department of Health and Human Services. NIH Publication No.
97-4073.
National Center on Sleep Disorders Research and Office of Prevention,
Education, and Control. (1997b). Working group report on problem sleepiness. U.S. Department of Health and Human Services.
National Center on Sleep Disorders Research and Office of Prevention,
Education, and Control. (2000). Restless legs syndrome: Detection and management in primary care. U.S. Department of Health and Human Services.
NIH Publication No 00-3788.
National Heart, Lung, and Blood Institute Working Group on Insomnia.
(1999). Insomnia: Assessment and management in primary care. American
Family Physician, 59, 3029–3038.
National Institutes of Health Consensus Development Program. (1990). The
treatment of sleep disorders of older people. NIH Consensus Statement.
[On-line]. Available: http://home.mdconsult.com/das/article/body/jorg.
*National Institutes of Health State-of-the-Science. (2005). Conference on
manifestation and management of chronic insomnia in adults. NIH
22(2), 1–30.
National Sleep Foundation. (1999). Is melatonin a treatment for insomnia and
jet lag? [On-line]. Available: http://www.sleepfoundation.org/ publications/
melatonin.html.
National Sleep Foundation. (2002). Sleep in America poll. [On-line].
Available: http://www.sleepfoundation.org.
*National Sleep Foundation. (2004). Melatonin: The basic facts. [On-line].
Available http://www.sleepfoundation.org/publications/melatoninthefact
.cfm.
Neubauer, D. (1999). Sleep problems in the elderly. American Family Physician,
59, 2551–2558.
Pagel, J., Zafralotifi, S., & Zammit, G. (1997). How to prescribe a good
night’s sleep. Patient Care, 31(4), 87.
Quan, S., & Zee, P. (2004). A sleep review of systems: Evaluating the effects of
medical disorders on sleep in the older patient. Geriatrics, 59(3), 37–42.
*Regestein, Q., Dambrosia, J., Hallett, M., et al. (1993). Daytime alertness
in patients with primary insomnia. American Journal of Psychiatry, 150,
1529–1534.
Requip improves symptoms of restless legs syndrome at 1 week, studies show.
(July 5, 2004). Health & Medicine Week, 952.
*Rosekind, M., Gregory, K., Mallis, M., et al. (2010). The cost of poor sleep:
Workplace productivity loss and associated costs. Journal of Occupational
& Environmental Medicine, 52(1), 91–98.
Roth, T., & Drake, C. (2004). Evolution of insomnia: Current status and
future directions. Sleep Medicine, 5(Suppl. 1), S23–S30.
Schwartz, J., Feldman, N., Fry, J., & Harsh, J. (2003). Efficacy of modafinil
for improving daytime wakefulness in patients treated previously with
psychostimulants. Sleep Medicine, 4, 43–49.
*Shorr, R., Bauwens, S., & Landefeld, C. S. (1990). Failure to limit quantities
of benzodiazepine hypnotic drugs for outpatients: Placing the elderly at
risk. American Journal of Medicine, 89, 725–732.
*Silber, M. (2004). Calming restless legs. Sleep, 27(5), 839–841.
*Silber, M., Krahn, L., & Olson, E. (2002). Diagnosing narcolepsy: Validity
and reliability of a new diagnostic criteria. Sleep Medicine, 3, 109–113.
Silva, J., Chase, M., Sartorius, N., & Roth, T. (1996). Special report from
a symposium held by the World Health Organization and the World
Federation of Sleep Research Societies: An overview of insomnias and
related disorders—recognition, epidemiology, and rational management.
Sleep, 19, 412–416.
*Sleep Facts and Stats. (2004). 2004 Sleep in America Poll. [On-line].
Available: http://www.sleepfoundation.org/NSAW1/pk_sleepfacts.cfm.
*Sleep Facts and Stats. (2009). 2009 Sleep in America Poll [On-line]. Available:
http://healthyliving.ocregister.com/files/2009/03/2009sleeppoll.pdf.
*Sleep Facts and Stats. (2010). 2010 Sleep in America Poll [On-line].
Available: http://www.sleepfoundation.org/sites/default/files/nsaw/NSF%
20Sleep%20in%20%20America%20Poll%20-%20Summary%20of%20
Findings%20.pdf.
Smith, D., Simonson, W., & Zammit, G. (1999, March). New ideas for the
management of sleep disorders. Symposium conducted at the meeting of the
American Medical Directors Association Annual Symposium, Orlando,
Florida.
*Stanford Center for Narcolepsy. (2004). http://med.stanford.edu/school/
Psychiatry/narcolepsy/symptoms.html.
Terzano, M., Rossi, M., Palomba, V., et al. (2003). New drugs for insomnia: Comparative tolerability of zopiclone, zolpidem and zaleplon. Drug
Safety, 26(4), 261–282.
*Trenkwalder, C., Garcia-Borreguero, D., Montagna, P., et al. (2004). Therapy
with ropinirole: Efficacy and tolerability in RLS 1 Study Group. Journal of
Neurological and Neurosurgical Psychiatry, 75(1), 92–97.
Trevena, L. (2004). Practice corner: Sleepless in Sydney—Is valerian an effective alternative to benzodiazepines in the treatment of insomnia? ACP
Journal Club, 141(1), 14.
Vitiello, M., Larsen, L., & Moe, K. (2004). Age-related sleep change: Gender
and estrogen effects on the subjective-objective sleep quality relationships of healthy, noncomplaining older men and women. Journal of
Psychosomatic Research, 56, 503–510.
Wagner, D. (1996). Sleep disorders I: Disorders of the circadian sleep–wake
cycle. Neurologic Clinics, 14, 651–670.
Wallace, K., & Morbunas, A. (1997). Commonly abused prescription
sedative-hypnotic drugs. Topics in Emergency Medicine, 19(4), 23–24.
What are the risks when elderly patients combine herbal and prescription
medications? (2004). Geriatric Psychopharmacology Update, 8(1), 1–6.
*Zisselman, M., Rovner, B., Yuen, E., & Louis, D. (1996). Sedative-hypnotic
use and increased hospital stay and costs in older people. Journal of the
American Geriatric Society, 44, 1371–1374.
*Zucconi, M., & Ferini-Strambi, L. (2004). Epidemiology and clinical
findings of restless legs syndrome. Sleep Medicine, 5, 293–299.
Arcangelo_Chap42.indd 670 10/8/2011 2:20:00 PM
671
CHAPTER
Andrew M. Peterson 43 Dharmi Patel
have been studied. These include a baseline norepinephrine
level that is too high, a central epinephrine level that is
too high, a problem with the functioning of epinephrine
in the peripheral system, or problems involving dopamine
receptors or dopamine-mediated functions (Pliszka, et al.,
1996). All these mechanisms may work together to cause
ADHD symptoms. The complete pathophysiologic process
of these mechanisms is not completely understood, but
there appears to be a connection between the D4 receptor and activity of the major neurotransmitters, epinephrine, norepinephrine and dopamine (Adler & Chua, 2002;
Daley, 2004).
Risk factors may be involved in the development of
ADHD, although many are only associations and do not indicate that ADHD is present. The practitioner must ascertain
the patient’s drug history and examine for visual disturbances
and hearing dysfunction as possible causes of the child’s
behavior (Dulcan, et al., 1997). A rare genetic disorder, generalized resistance to thyroid hormone, has been associated
with ADHD (Hauser, et al., 1993). Fragile X syndrome, fetal
alcohol syndrome, glucose-6-phosphate dehydrogenase deficiency, and phenylketonuria are also associated risks for development of ADHD (Dulcan, et al., 1997). Limited numbers
of cases have been associated with other risk factors, including such pregnancy variables as poor maternal health, young
maternal age, maternal use of alcohol or cigarettes, toxemia or
eclampsia, postmaturity, and extended labor (Dulcan, et al.,
1997; Markussen, et al., 2003). Medical conditions and malnutrition in infancy may also play a role in ADHD, although
this has not been proved (Dulcan, et al., 1997).
DIAGNOSTIC CRITERIA
The diagnostic criteria for ADHD are listed in Box 43.1.
Children are required to show symptoms by age 7, and most
children show symptoms for many years before the diagnosis is made (APA, 2000). For a definitive diagnosis, the child
also must show symptoms in more than one setting, such as
at home and in school. The adult with ADHD may display
symptoms at home and at work. Adult patients also have trouble maintaining relationships as a result of their inattentiveness. In children and adults, the symptoms must interfere with
Attention-Deficit/Hyperactivity Disorder
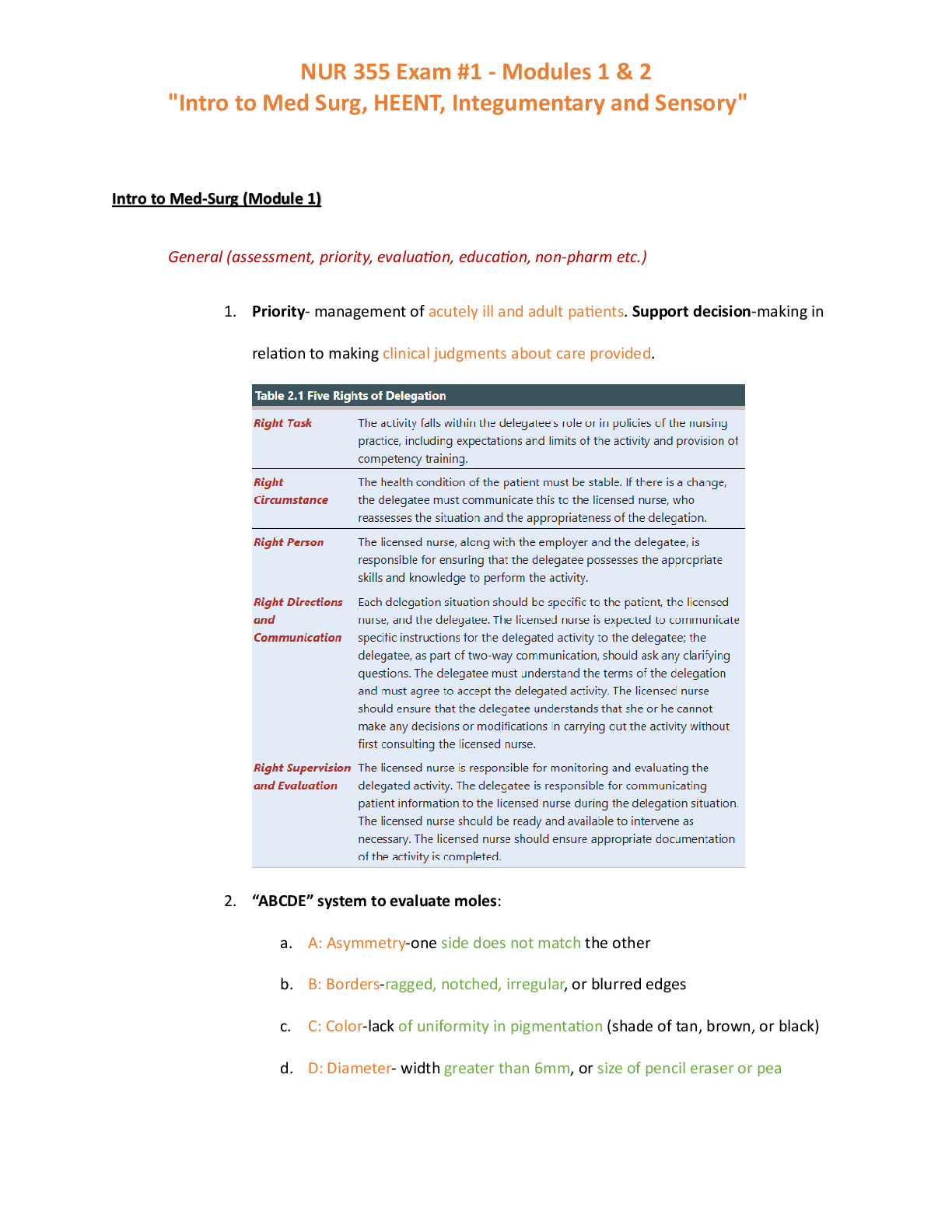
Attention-deficit/hyperactivity disorder (ADHD) has become
a commonly diagnosed condition among today’s children.
Hallmark symptoms include hyperactivity, impulsivity, and
inattention. The American Psychiatric Association (APA)
estimated in the Diagnostic and Statistical Manual of Mental
Disorders (DSM-IV) that 3% to 5% of school-aged children
had ADHD. The disorder is more common in boys than in
girls, with a ratio ranging from 4:1 to 9:1 (APA, 2000; Spencer,
et al., 2002). Research is increasingly revealing that ADHD also
affects adults, with estimates of prevalence ranging from 2% to
7% (Wender, 1995). This realization is changing perceptions
of ADHD because it is becoming imperative to understand the
disorder as diagnosed in adulthood.
Researchers have found that many of the core symptoms
of ADHD are treatable. Treatment should be individualized
to the patient’s symptoms. The treatment plan usually is multimodal. Even when treatment begins early in childhood, the
patient may still show symptoms in adolescence or adulthood.
The outcome of the childhood disorder is uncertain, as is
determining which children will have the disorder.
CAUSES
Many causes of ADHD have been suggested, but none has yet
to be accepted. Evidence suggests that the disorder may have a
genetic link (Farone & Biederman, 1994). Estimates are that
children who have a sibling with ADHD have a two to three
times greater chance of being diagnosed with ADHD (Dulcan,
et al., 1997). Growing evidence suggests that the principal
cause of ADHD is genetic (Pliszka, 2007). ADHD has been
associated with the dopamine transporter gene and the dopamine D4 gene (Adler & Chua, 2002; Daley, 2004). Possible
nongenetic causes are neurobiological, such as perinatal stress,
low birth weight, traumatic brain injury, maternal smoking
during pregnancy, and severe early deprivation (Pliszka, 2007).
Other theories involve dietary intake of certain chemicals and
sugars, but data are lacking.
PATHOPHYSIOLOGY
Neurotransmitter dysfunction is a proposed mechanism for
ADHD, and several different pathways for this dysfunction
Arcangelo_Chap43.indd 671 10/8/2011 2:20:15 PM
672 UNIT 9 | PHARMACOLOGY FOR NEUROLOGICAL/PSYCHOLOGICAL DISORDERS
the person’s ability to function. The criteria are further broken
into subtypes, and based on the symptoms, the patient’s disorder is coded (Box 43.2).
Diagnosing ADHD in a child may be difficult because
children often behave differently in the health care setting,
therefore making it impossible for the provider to observe
symptoms. For this reason, the practitioner must use other
methods to evaluate behavior. Such methods include rating scales, which usually are administered by parents and
teachers. All scales are similar, but each has its own criteria
and rating system. Some commonly used scales include the
parent-completed Child Behavior Checklist (Achenbach,
1991; Biederman, et al., 1993), the Teacher Report Form of the
Child Behavior Checklist (Achenbach, 1991; Edelbrock, et al.,
1984), the Conners Parent and Teacher Rating Scale (Ullmann,
et al., 1985), the Barkley Home Situations Questionnaire and
School Situations Questionnaire (Barkley, 1990), and the
Child Attention Problems Profile (Barkley, 1990; Barkley et al.,
1989). These rating scales have been found to be accurate measures of ADHD behavior (Dulcan, et al., 1997). Practitioners
may use these rating scales to follow a child’s behavior after the
initial diagnosis of ADHD.
Making the initial diagnosis also requires detailed parent
interviews that focus on a family history of ADHD or other
psychiatric disorders, psychosocial adversity (e.g., poverty,
parental psychopathology or absence, family conflict), school
behavior, learning, attendance and test reports, and medical
evaluations (Dulcan, et al., 1997).
A. Either (1) or (2)
1. Six (or more) of the following symptoms of inattention have persisted for at least 6 months to a degree
that is maladaptive and inconsistent with developmental level:
Inattention
a. often fails to give close attention to details or
makes careless mistakes in schoolwork, work,
or other activities
b. often has difficulty sustaining attention in tasks
or play activities
c. often does not seem to listen when spoken to
directly
d. often does not follow through on instructions
and fails to finish schoolwork, chores, or duties
in the workplace (not due to oppositional behavior or failure to understand instructions)
e. often has difficulty organizing tasks and activities
f. often avoids, dislikes, or is reluctant to engage in
tasks that require sustained mental effort (such
as schoolwork or homework)
g. often loses things necessary for tasks or activities (e.g., toys, school assignments, pencils,
books, or tools)
h. is often easily distracted by extraneous stimuli
i. is often forgetful in daily activities
2. Six (or more) of the following symptoms of
hyperactivity-impulsivity have persisted for at
least 6 months to a degree that is maladaptive and
inconsistent with developmental level:
Hyperactivity
a. often fidgets with hands or feet or squirms in seat
b. often leaves seat in classroom or in other situations in which remaining seated is expected
c. often runs about or climbs excessively in situations in which it is inappropriate (in adolescents
or adults, may be limited to subjective feelings of
restlessness)
d. often has difficulty playing or engaging in leisure
activities quietly
e. is often “on the go” or often acts as if “driven by
a motor”
f. often talks excessively
Impulsivity
g. often blurts out answers before questions have
been completed
h. often has difficulty awaiting turn
i. often interrupts or intrudes on others (e.g., butts
into conversation or games)
B. Some hyperactive–impulsive or inattentive symptoms that
caused impairment were present before age of 7 years.
C. Some impairment from the symptoms is present in two
or more settings (e.g., at school [or work] and at home).
D. There must be clear evidence of clinically significant
impairment in social, academic, or occupational
functioning.
E. The symptoms do not occur exclusively during the
course of a Pervasive Developmental Disorder,
Schizophrenia, or other Psychotic Disorder and are
not better accounted for by another mental disorder
(e.g., Mood Disorder, Anxiety Disorder, Dissociative
Disorder, or Personality Disorder).
Criteria for Diagnosing Attention-Deficit/Hyperactivity Disorder
BOX 43.1
From American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text revision) .
Washington, DC: Author, with permission.
Arcangelo_Chap43.indd 672 10/8/2011 2:20:16 PM
CHAPTER 43 | ATTENTION-DEFICIT/HYPERACTIVITY DISORDER 673
A confounding factor in the diagnosis is the probability of
comorbid disorders. Mood disorders, anxiety disorders, learning disorders, and communication disorders are more common
in the child with ADHD (APA, 2000). Laboratory findings,
physical examination, and evaluation of concurrent medical
problems cannot be used to confirm the diagnosis. Minor physical anomalies such as hypertelorism, a highly arched palate, and
low-set ears may be more common in this population (APA,
2000), but such characteristics do not mean that the child has
ADHD. Many children diagnosed with ADHD can be expected
to have some impaired social functioning in adult life.
The diagnosis of ADHD in the adolescent is less clear
since as an ADHD child matures into adolescence, the symptoms change (Nahlik, 2004). Moodiness, laziness, boredom,
or impatience may be common symptoms in the ADHD adolescent but may also be typical adolescent behavior or even
another mood disorder.
Diagnosis in an adult consists of a complete psychiatric
evaluation; childhood history; information from spouse or significant others, parents, or employers; and a review of school
records. A medical history and physical examination can be
used to rule out comorbid conditions. As with childhood
diagnosis, rating scales and questionnaires may also be used
(Weiss & Murray, 2003), such as the Conners Abbreviated
Teacher’s Rating Scale and the Wender Utah Rating Scale.
Practitioners cannot use a patient’s response to stimulant
therapy to determine ADHD status. A child not diagnosed
with ADHD has the same response of reduced hyperactivity, impulsivity, and inattentiveness as a child diagnosed with
ADHD (Goldman, et al., 1998).
INITIATING DRUG THERAPY
Many practitioners today follow a multimodal treatment plan.
Multimodal treatment plans seem logical because different symptoms respond to different types of treatment. The Multimodal
Treatment Study (MTA) showed that children receiving intensive behavioral management combined with medication fared
better than those receiving intensive behavioral management
alone (Anonymous, 1999). The core symptoms of the disorder
(i.e., inattention, hyperactivity, and impulsivity) respond to medication, with or without the behavioral intervention. Behavioral
symptoms seem to respond to environmental modification,
while skills in sports, academics, and social situations may not
respond to medication or behavior modification. Relationship
problems usually can be treated through psychotherapy.
Nonpharmacologic aspects of a multimodal treatment
plan consist of behavior modification, parent training, family
therapy, social skills training, academic skills training, individual psychotherapy, cognitive behavior modification, and therapeutic recreation. These are discussed further in the Nutrition/
Lifestyle section later in this chapter.
Goals of Drug Therapy
When a child is diagnosed with ADHD, questions arise regarding the outcome of this disorder. Parents want to know if there is
a cure and, if so, what treatment will increase the chance for cure.
However, the outcome of ADHD cannot be predicted, and the
child will not always “grow out of it.” Three outcomes have been
identified. The first possible outcome is developmental delay,
which occurs in approximately 30% of diagnosed children; this
means that the child will outgrow the symptoms. The second
possible outcome, which occurs in 40% of children, is continual
display, which is marked by adult life with ADHD. Continual
display may lead to social and emotional difficulties. The third
possible outcome is developmental decay (30% of children with
ADHD), which involves the continual display of core ADHD
symptoms along with pathologic conditions such as substance
abuse and antisocial personality disorder. Developmental decay
is the most severe outcome (Sudak, 1998).
Medication therapy is usually one of the first options
in treating patients newly diagnosed with ADHD.
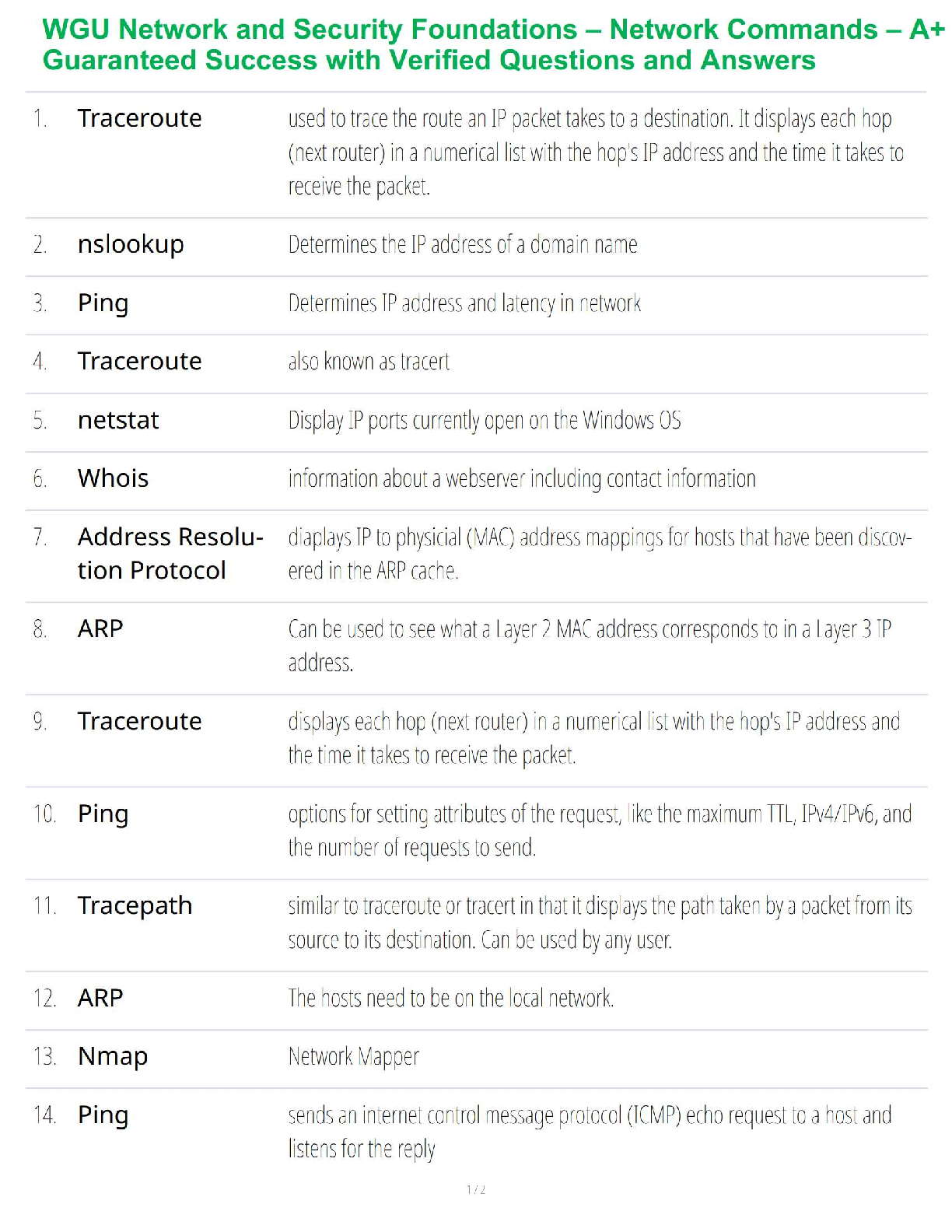
Pharmacotherapy offers several alternatives (Table 43.1). The
medication class primarily used is stimulants, such as amphetamines and methylphenidate. Nonstimulant alternatives are
atomoxetine (Strattera), buproprion (Wellbutrin), tricyclic
antidepressants (TCAs), selective serotonin reuptake inhibitors (SSRIs), monoamine oxidase (MAO) inhibitors and
alpha-adrenergic agonists (Pliszka, 2007). Although it is not
clear how these medications actually affect the primary symptoms of ADHD, it is known which neurotransmitters they
affect (Table 43.2).
314 .01 Attention-Deficit/Hyperactivity Disorder, Combined Type: if both Criteria A1 and A2 are met for
the past 6 months
314 .00 Attention-Deficit/Hyperactivity Disorder, Predominantly Inattentive Type: if Criterion A1 is met
but Criterion A2 is not met for the past 6 months
314 .01 Attention-Deficit/Hyperactivity Disorder, Predominantly Hyperactive-Impulsive Type: if Criterion
A2 is met but Criterion A1 is not met for the past
6 months
Coding note: For individuals (especially adolescents
and adults) who currently have symptoms that no
longer meet full criteria, “In Partial Remission”
should be specified.
From American Psychiatric Association. (2000). Diagnostic
and statistical manual of mental disorders (4th ed., text
revision, p. 93). Washington, DC: Author, with permission.
BOX 43.2
Diagnostic and Statistical
Manual of Mental
Disorders—IV: Coding
Based on Type
Arcangelo_Chap43.indd 673 10/8/2011 2:20:16 PM
674 UNIT 9 | PHARMACOLOGY FOR NEUROLOGICAL/PSYCHOLOGICAL DISORDERS
The long-term benefits of medication therapy have
not been determined. It is clear that they work in the short
term to improve symptoms, but there is a lack of long-term
studies (Goldman, et al., 1998). The following information
addresses concerns for the pediatric population using these
medications.
Stimulants
A stimulant is usually the first-choice medication, based on
60 years of research and clinical experience (Dulcan, et al.,
1997). Daley (2004) reported that nearly 70% of patients will
respond to stimulant therapy. The most commonly used stimulants are methylphenidate (Ritalin, Concerta) and amphetamine
salts (Adderall, Dexedrine). Either stimulant is appropriate;
both are equally efficacious in the treatment of ADHD.
Dosage
Amphetamines should be started at the lowest dosage and
titrated upward until the desired response is seen. Dosing is
usually based on weight and titrated to a dosage that controls
the symptoms of ADHD. Table 43.3 lists medications and
their dosages.
There is equal efficacy between long-acting and
immediate-release formulations. Longer-acting formulations
may provide improved convenience and compliance. A patient
may be initially started on a long-acting form, but children
(<16 kg) are often started on shorter-acting doses because
long-acting forms are not manufactured in low doses (Pliszka,
2007). For immediate-release methylphenidate, the typical
starting dose for children under age 6 is 5 mg before breakfast and 5 mg at lunch. The dose may be increased by 5 to
10 mg weekly, with a maximum recommended dose of 60 mg.
Long-acting preparations are available if the immediate-release
formulation is impossible or inconvenient to give, or if
rebound is a problem. The long-acting methylphenidate
Ritalin LA should be started after the patient is taking 20 mg
of the immediate-release preparation. For patients taking 10 to
20 mg of immediate-release methylphenidate daily, Concerta
18 mg or Metadate ER 10 or 20 mg may also be used.
Dose titrations occur every 1 to 3 weeks until the maximum
allowed dose, symptom remission, or side effects prevent further titrations, whichever occurs first.
Mechanism of Action
As mentioned previously, it is not clear how stimulants help to
reduce the core symptoms of ADHD. In addition to increasing
levels of epinephrine and norepinephrine, these agents also can
bind to central dopamine receptors and increase the systemic
levels of dopamine.
Adverse Events
The primary adverse events related to stimulant therapy include
palpitations, tachycardia, elevated blood pressure, and potentially arrhythmias. Changes in appetite, nausea, vomiting, and
other gastrointestinal (GI) disturbances may occur. The neurologic adverse events range from headache and insomnia to seizure activity, particularly in patients predisposed to seizures.
In general, adverse events are manageable, results are
quick and predictable with the first dose, and the medications
are easy to titrate (Buitelaar, et al., 1995). The adverse events of
the stimulants, such as headaches, dizziness, appetite suppression, tics, dyskinesias, sleep disturbances, abuse potential, and
in particular growth retardation (below height or weight on
normal growth charts), may be of concern. One study found
a significant difference in growth between patients who took
stimulants and those who did not. Other studies have shown a
decrease in height or weight in patients taking stimulants. The
clinician must assess the growth progress, need for continued
treatment, and overall functioning of the ADHD patient every
1 to 3 months (Daley, 2004).
[Show More]
-3.png)

-3.png)