*NURSING > STUDY GUIDE > Chapter 4 The Complete Health History Jarvis Physical Examination & Health Assessment, 7th Edition. (All)
Chapter 4 The Complete Health History Jarvis Physical Examination & Health Assessment, 7th Edition.
Document Content and Description Below
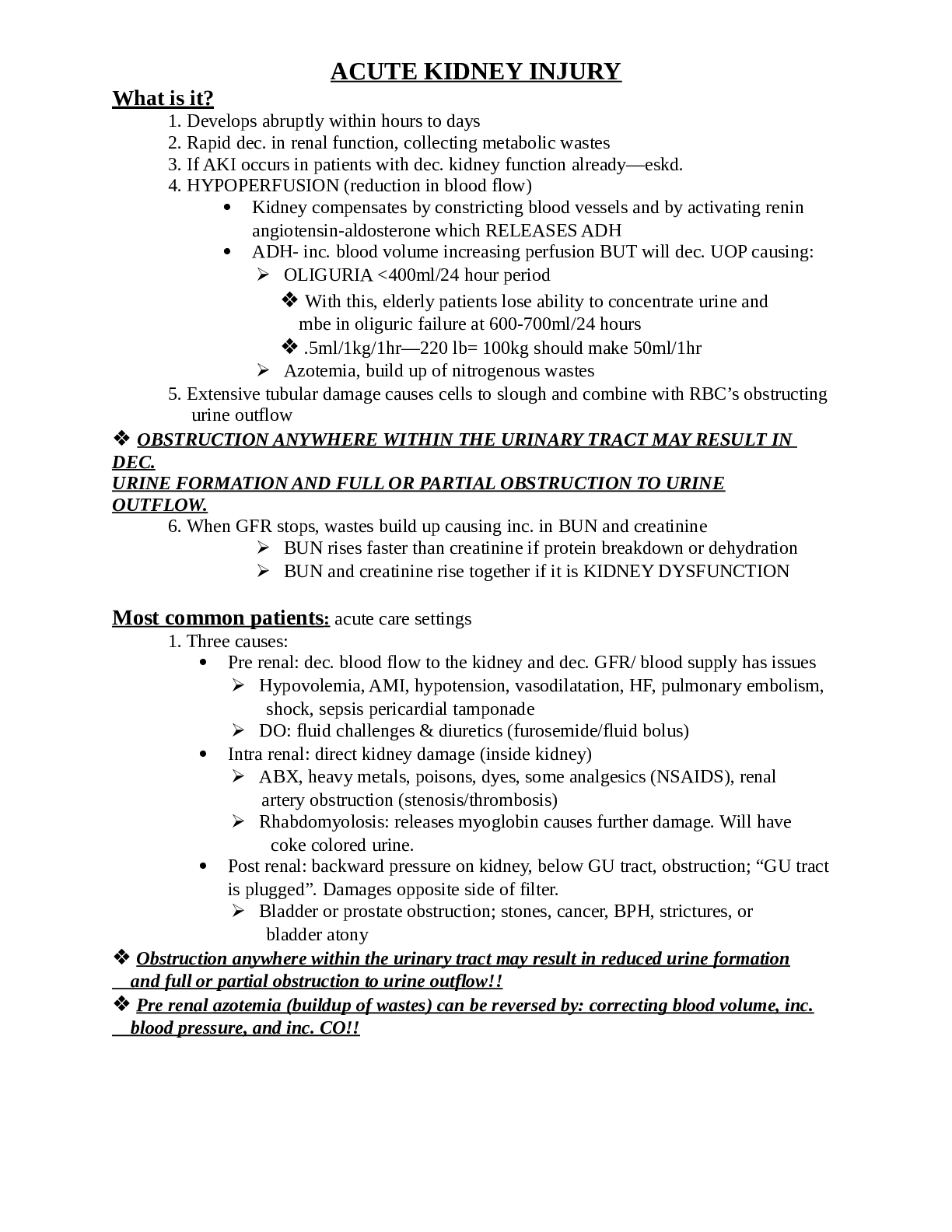
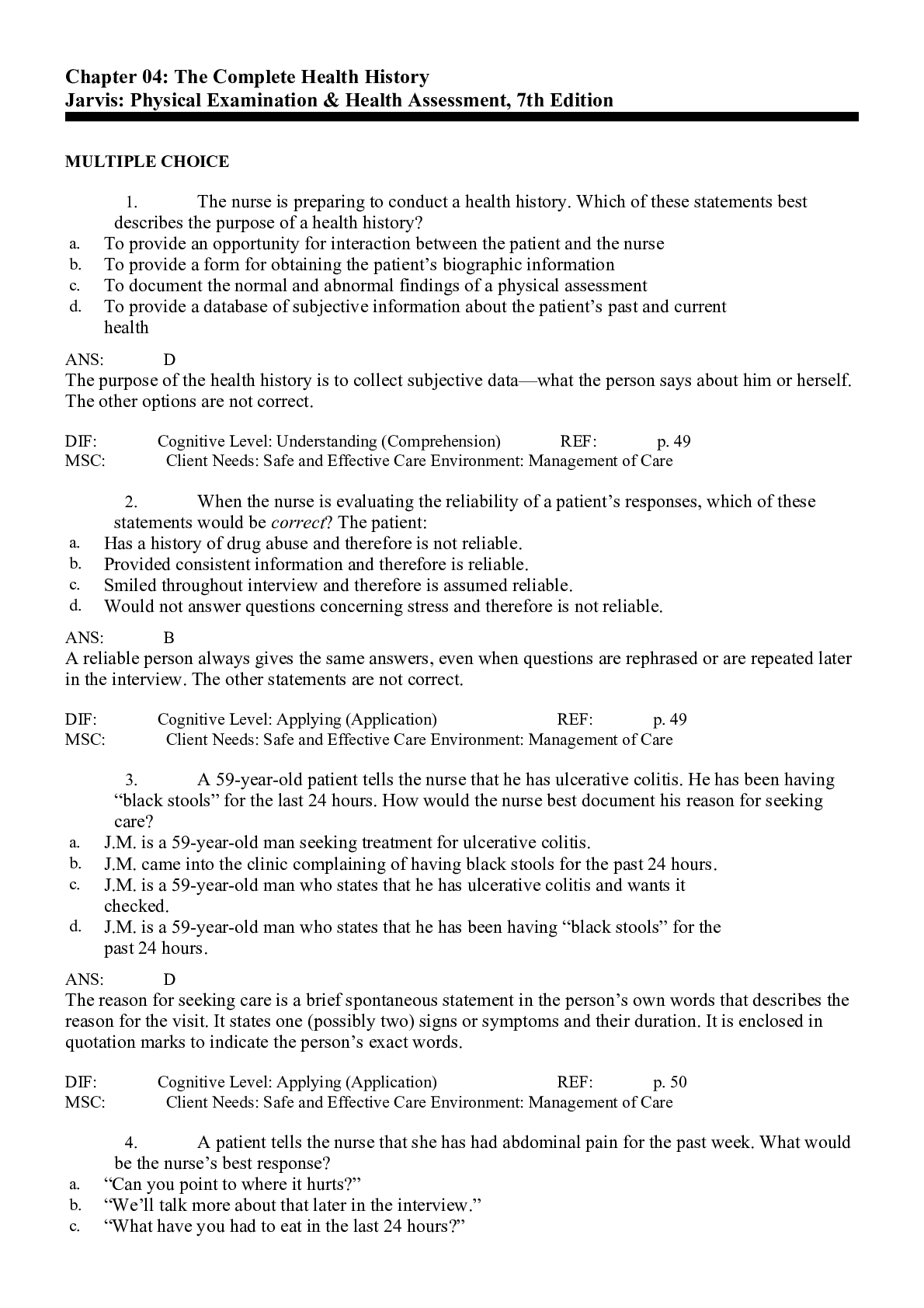
1. The nurse is preparing to conduct a health history. Which of these statements best describes the purpose of a health history? a. To provide an opportunity for interaction between the patient and ... the nurse b. To provide a form for obtaining the patient’s biographic information c. To document the normal and abnormal findings of a physical assessment d. To provide a database of subjective information about the patient’s past and current health ANS: D The purpose of the health history is to collect subjective data—what the person says about him or herself. The other options are not correct. DIF: Cognitive Level: Understanding (Comprehension) REF: p. 49 MSC: Client Needs: Safe and Effective Care Environment: Management of Care 2. When the nurse is evaluating the reliability of a patient’s responses, which of these statements would be correct? The patient: a. Has a history of drug abuse and therefore is not reliable. b. Provided consistent information and therefore is reliable. c. Smiled throughout interview and therefore is assumed reliable. d. Would not answer questions concerning stress and therefore is not reliable. ANS: B A reliable person always gives the same answers, even when questions are rephrased or are repeated later in the interview. The other statements are not correct. DIF: Cognitive Level: Applying (Application) REF: p. 49 MSC: Client Needs: Safe and Effective Care Environment: Management of Care 3. A 59-year-old patient tells the nurse that he has ulcerative colitis. He has been having “black stools” for the last 24 hours. How would the nurse best document his reason for seeking care? a. J.M. is a 59-year-old man seeking treatment for ulcerative colitis. b. J.M. came into the clinic complaining of having black stools for the past 24 hours. c. J.M. is a 59-year-old man who states that he has ulcerative colitis and wants it checked. d. J.M. is a 59-year-old man who states that he has been having “black stools” for the past 24 hours. ANS: D The reason for seeking care is a brief spontaneous statement in the person’s own words that describes the reason for the visit. It states one (possibly two) signs or symptoms and their duration. It is enclosed in quotation marks to indicate the person’s exact words. DIF: Cognitive Level: Applying (Application) REF: p. 50 MSC: Client Needs: Safe and Effective Care Environment: Management of Care 4. A patient tells the nurse that she has had abdominal pain for the past week. What would be the nurse’s best response? a. “Can you point to where it hurts?” b. “We’ll talk more about that later in the interview.” c. “What have you had to eat in the last 24 hours?” d. “Have you ever had any surgeries on your abdomen?” ANS: A A final summary of any symptom the person has should include, along with seven other critical characteristics, “Location: specific.” The person is asked to point to the location. DIF: Cognitive Level: Applying (Application) REF: p. 50 MSC: Client Needs: Safe and Effective Care Environment: Management of Care 5. A 29-year-old woman tells the nurse that she has “excruciating pain” in her back. Which would be the nurse’s appropriate response to the woman’s statement? a. “How does your family react to your pain?” b. “The pain must be terrible. You probably pinched a nerve.” c. “I’ve had back pain myself, and it can be excruciating.” d. “How would you say the pain affects your ability to do your daily activities?” ANS: D The symptom of pain is difficult to quantify because of individual interpretation. With pain, adjectives should be avoided and the patient should be asked how the pain affects his or her daily activities. The other responses are not appropriate. DIF: Cognitive Level: Applying (Application) REF: p. 50 MSC: Client Needs: Safe and Effective Care Environment: Management of Care 6. In recording the childhood illnesses of a patient who denies having had any, which note by the nurse would be most accurate? a. Patient denies usual childhood illnesses. b. Patient states he was a “very healthy” child. c. Patient states his sister had measles, but he didn’t. d. Patient denies measles, mumps, rubella, chickenpox, pertussis, and strep throat. ANS: D Childhood illnesses include measles, mumps, rubella, chickenpox, pertussis, and strep throat. Avoid recording “usual childhood illnesses” because an illness common in the person’s childhood may be unusual today (e.g., measles). DIF: Cognitive Level: Remembering (Knowledge) REF: p. 51 MSC: Client Needs: Safe and Effective Care Environment: Management of Care 7. A female patient tells the nurse that she has had six pregnancies, with four live births at term and two spontaneous abortions. Her four children are still living. How would the nurse record this information? a. P-6, B-4, (S)Ab-2 b. Grav 6, Term 4, (S)Ab-2, Living 4 c. Patient has had four living babies. d. Patient has been pregnant six times. ANS: B Obstetric history includes the number of pregnancies (gravidity), number of deliveries in which the fetus reached term (term), number of preterm pregnancies (preterm), number of incomplete pregnancies (abortions), and number of children living (living). This is recorded: Grav _____ Term _____ Preterm _____ Ab _____ Living _____. For any incomplete pregnancies, the duration is recorded and whether the pregnancy resulted in a spontaneous (S) or an induced (I) abortion. DIF: Cognitive Level: Applying (Application) REF: p. 51 MSC: Client Needs: Safe and Effective Care Environment: Management of Care 8. A patient tells the nurse that he is allergic to penicillin. What would be the nurse’s best response to this information? a. “Are you allergic to any other drugs?” b. “How often have you received penicillin?” c. “I’ll write your allergy on your chart so you won’t receive any penicillin.” d. “Describe what happens to you when you take penicillin.” ANS: D Note both the allergen (medication, food, or contact agent, such as fabric or environmental agent) and the reaction (rash, itching, runny nose, watery eyes, or difficulty breathing). With a drug, this symptom should not be a side effect but a true allergic reaction. DIF: Cognitive Level: Understanding (Comprehension) REF: p. 52 MSC: Client Needs: Safe and Effective Care Environment: Management of Care 9. The nurse is taking a family history. Important diseases or problems about which the patient should be specifically asked include: a. Emphysema. b. Head trauma. c. Mental illness. d. Fractured bones. ANS: C Questions concerning any family history of heart disease, high blood pressure, stroke, diabetes, obesity, blood disorders, breast and ovarian cancers, colon cancer, sickle cell anemia, arthritis, allergies, alcohol or drug addiction, mental illness, suicide, seizure disorder, kidney disease, and tuberculosis should be asked. DIF: Cognitive Level: Remembering (Knowledge) REF: pp. 53-54 MSC: Client Needs: Safe and Effective Care Environment: Management of Care 10. The review of systems provides the nurse with: a. Physical findings related to each system. b. Information regarding health promotion practices. c. An opportunity to teach the patient medical terms. d. Information necessary for the nurse to diagnose the patient’s medical problem. ANS: B The purposes of the review of systems are to: (1) evaluate the past and current health state of each body system, (2) double check facts in case any significant data were omitted in the present illness section, and (3) evaluate health promotion practices. DIF: Cognitive Level: Remembering (Knowledge) REF: p. 54 MSC: Client Needs: Safe and Effective Care Environment: Management of Care [Show More]
Last updated: 2 years ago
Preview 1 out of 10 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$12.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
May 09, 2021
Number of pages
10
Written in
Additional information
This document has been written for:
Uploaded
May 09, 2021
Downloads
0
Views
94

.png)
.png)

.png)
.png)