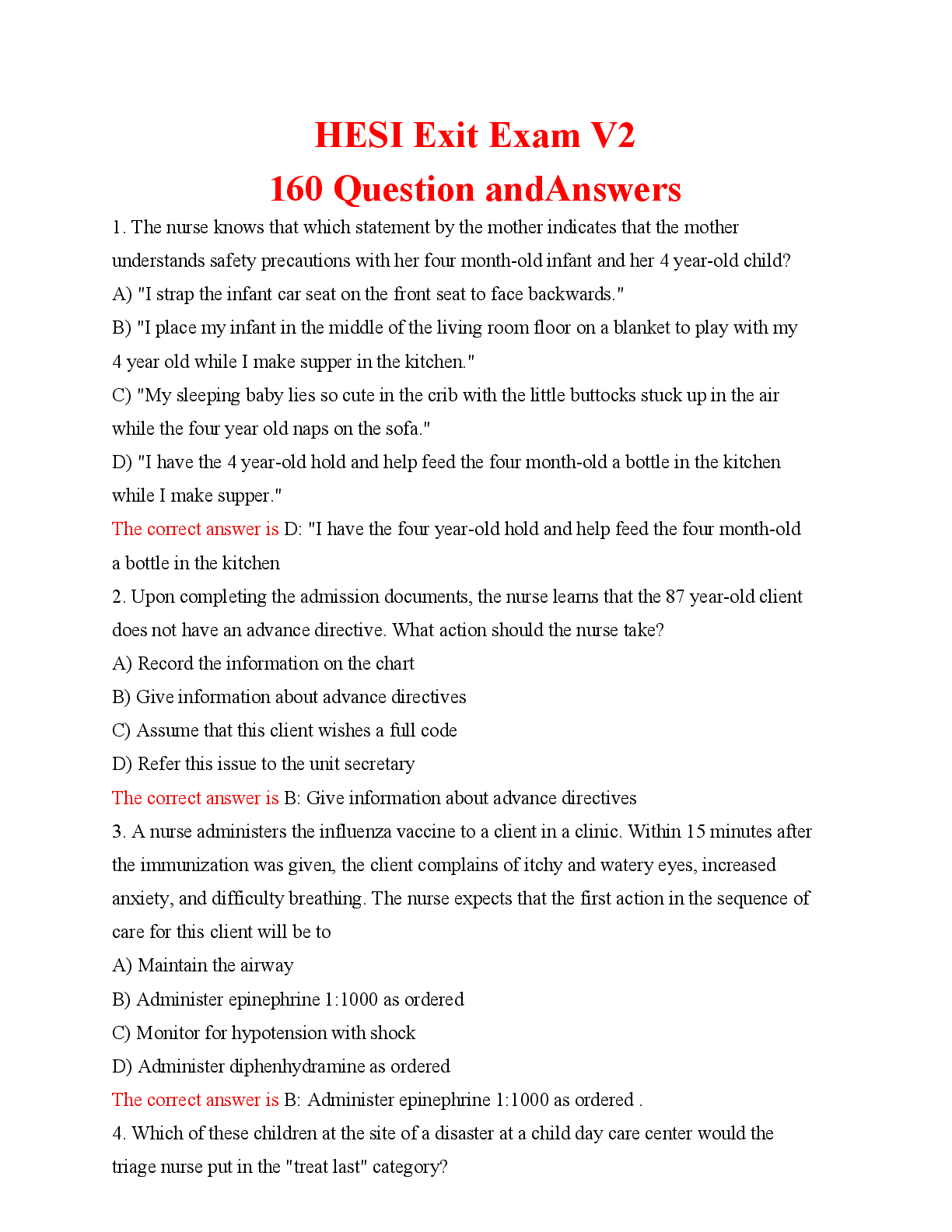
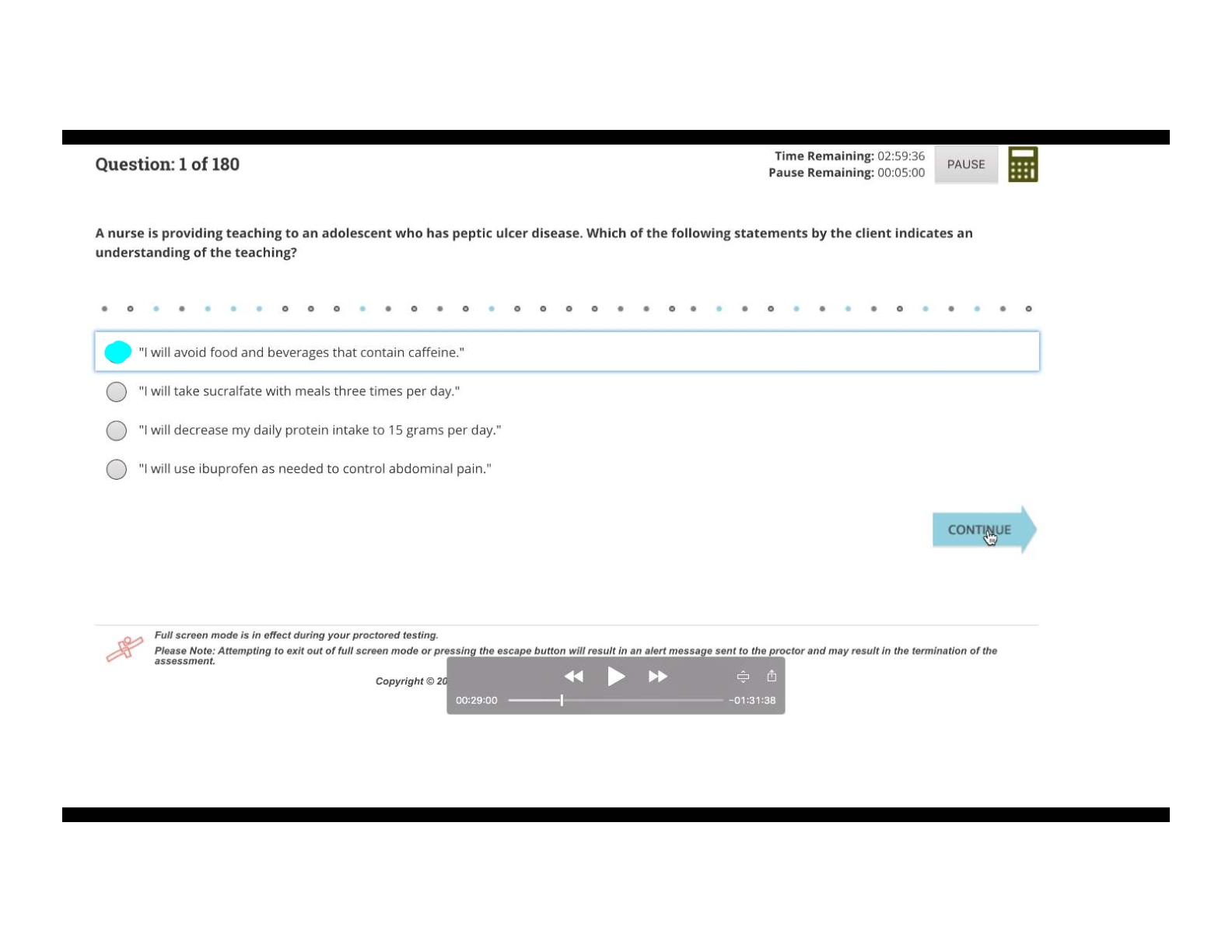
This scenario will assist students in assessing and responding appropriately to a child in respiratory distress due to pneumonia and asthma exacerbation. In 2009 the Centers for Disease Control reported that approximatel
...
This scenario will assist students in assessing and responding appropriately to a child in respiratory distress due to pneumonia and asthma exacerbation. In 2009 the Centers for Disease Control reported that approximately 10% of all American children have asthma. The World Health Organization reports that asthma is the most chronic disease among children and that it is often undertreated and under-diagnosed.
Student Learning Outcomes
1. Student will review Sabina Vasquez’s ordered interventions, medications, and past medical history in DocuCare.
2. Student will navigate through their patient’s electronic health record viewing medication administration record, home medications, interventions, and medical history.
3. Student will compare and contrast Sabina Vasquez’s pharmacologic therapy to a patient hospitalized in the clinical setting.
Case Considerations
Pneumonia in children 5 years and older is most commonly due to Mycoplasma pneumoniae, Chlamydia pneumonia, or Streptococcus pneumonia; therefore treatment would include a macrolide and cephalosporin.
Viral upper respiratory infections and bacteria can increase airway responsiveness and inflammation in children with asthma.
English language learners are less able to use their second language during periods of high stress such as hospitalization, therefore interpretation services or additional explanations may be necessary.
Readings
Centers for Disease Control and Prevention (2011). CDC Fact Sheet. Retrieved March 15, 2011 from: https://www.cdc.gov/nchs/fastats/asthma.htm
National Asthma Education and Prevention Program (2007). Guidelines for the Diagnosis and Management of Asthma. Retrieved March 27, 2011
from: http://www.nhlbi.nih.gov/guidelines/asthma/
US Department of Health and Human Services; National Heart, Lung and Blood Institute (2007). Asthma Action Plan. Retrieved March 27, 2011
from: http://www.cdc.gov/asthma/actionplan.html
World Health Organization (2011). WHO Fact Sheet. Retrieved March 15, 2011 from: http://www.who.int/mediacentre/factsheets/fs307/en/
Wu, F., & Takaro, T. (2007). Childhood Asthma and Environmental Interventions.Environmental Health Perspectives, 115(6):971-5.
Case Study of Sabina Vasquez Student Instructions:
Review the chart for Sabina Vasquez in DocuCare.
• Patient Information
• Demographics and Current Visit
• History of Chief Present Concern under Admission Assessment
• Notes
• Orders
• Medication Administration Record
Time: 7 p.m.
Report from ED nurse:
Sabina Vasquez is a 5-year-old Hispanic girl admitted today from the emergency room with a diagnosis of pneumonia. She has a history of asthma and has had several episodes requiring use of an albuterol inhaler at home.
Sabina has had an upper airway infection for the past few days. She developed a fever of 39°C (102.2°F) early this morning. Her mother was concerned about her fever and breathing and brought her to the ED. She presented to the ED in moderate respiratory distress with mild substernal retractions, a productive cough, wheezing and rales throughout all lung fields, and an oxygen saturation of 90% on room air.
She was placed on oxygen via nasal cannula at 2 liters per minute. She received a 380 mL bolus of normal saline and an albuterol nebulizer treatment at 5 p.m. This improved her oxygen saturation to 94%. Chest x-ray revealed right lower lobe pneumonia with effusion. An IV of D5½ NS with 20 mEq KCl/L at 61 mL/hour is infusing. She just got settled in bed and her mother is at the bedside.
Reflective Questions
1. Have you ever care for a patient with asthma? Please give a brief synopsis.
a. Yes, I have. The patient I took care of needed breathing treatments every 6 hours. They had multiple medications. The time they were close to having an asthma attack their breathing was wheezing.
2. What are some anticipated diagnostic tests for a patient with asthma?
a. The patient could have a chest xray, they could also have a bronchoscopy, they could have pulmonary function testing, or a spirometry.
3. What are some anticipated physical findings for a patient with asthma?
a. The patient would have an increased respiratory rate, wheezing, shortness of breath, they could have chest tightness.
4. What medication was Sabina Vasquez prescribed to specifically help with oxygenation?
a. She was given 2.5mg of albuterol in a nebulizer.
5. How will these medications specifically help improve Sabina’s oxygenation?
a. This can treat her bronchospasm she is having. It relaxes the airway muscles, so it is easier for the patient to breathe.
6. What were Sabina Vasquez’s daily home medications? How do these medications help improve oxygenation for Sabina?
a. No home medications were listed in the patient chart that were different. She has an albuterol inhaler with spacer. There were the medications ordered and the PRN orders. But she could be prescribed a number of inhalers or nebulizers to help with her airway. She could also get a steroid medication to help with the inflammation.
7. There were no medications listed for home meds, what would you suspect Sabina has at home for her Intermittent asthma exacerbations?
a. I would expect that she has albuterol inhaler at home for her asthma exacerbations.
8. Were the home medications prescribed for your patient different than Sabina Vasquez’s home medications? If so, how are they different?
a. The patient that I had they had were on long term inhaler which was Advair and they were on a rescue inhaler albuterol and they were also on prednisone to help with the inflammation. The Advair is taken every day to help prevent asthma exacerbations. The prednisone helps decrease inflammation.
9. What are 5 prioritized Nursing Interventions with rationale that you can provide for a patient with asthma?
a. Assess the clients vitals as needed while in distress- increased rr and hr can occur during initial hypoxia and hypercapnia.
b. Assess the client’s level of anxiety- the client could be anxious from not being able to breathe properly.
c. Assess breath sounds and adventitious sounds such as wheezing- adventious sounds may indicate a worsening condition. Wheezing also shows bronchospasm.
d. Assess for fatigue- fatigue could be a sign that indicates distress, leading to respiratory failure.
e. Maintain head of bed elevated- This promotes maximum lung expansion and assist the patient with breathing.
Scenario Progression Asthma – Pneumonia Leading to Respiratory Distress in a Child with Known Asthma Sabina Vasquez
Monitor Settings
Patient/Simulator Actions
Students Interventions
Cue/Prompt
Initial state:
Anxious Auscultation sounds:
Wheezing throughout lungs
Vocal sounds:
Productive cough “I can’t breathe.”
Wash hands Introduce self Identify patient Obtain vital signs Obtain SpO2
Auscultate heart, lungs, and abdomen
Assess IV site Assess IV fluids
Assess skin for cyanosis
Perform visual inspection to determine work of breathing
HR: 125
RR: 30
BP: 108/70
Temp: 39.2°C Mother:
(102.6°F) SpO2: 94% Mother is soothing the patient
Going to: If students do not respond to abnormal vital signs, mother
HR: 130
RR: 35 should state: “She breathe very fast. She no feeling good.”
BP: 110/75
SpO2: 89%
Over 5
minutes
After increase in oxygen, going towards: HR: 128
Auscultation sounds: Wheezing
Vocal sounds: Coughing
Call primary care provider with assessment, potential increase in oxygen and additional nebulizer treatment
(Stat orders are provided)
Mother:
If students do not call MD, mother should state: “You no can help her? Where the doctor?”
RR: 32
BP: 108/73 SpO2: 91%
on 4 L oxygen Using one-word answers to student questions due to coughing
Receive orders
Review and verify orders Respiratory therapist:
If students call RT before MD, RT should say: “What do you want me to do? I don’t have an
Increase oxygen
order.” MD:
If students do not call RT, MD should ask: “How is her sats? Describe her lung sounds.”
Mother:
If students do not explain the treatments and rationales, mother should point to nasal cannula or medication and say: “What is this? (Que es esto?) This is asthma?”
Assess IV site and fluid
Begin antibiotics
Patient’s anxiety decreases with O2 application
Administer acetaminophen PO
Explain treatment to patient and family
Administer albuterol nebulizer treatment
After
Assess family’s understanding of treatments and need for interpreter
Educate family about differences between pneumonia and an asthma exacerbation
albuterol,
going
Auscultation sounds 2
towards: HR: minutes after albuterol:
136 Coarse crackles
RR: 28
Vocal sounds:
SpO2: 94%
on 4 L Cough decreases
oxygen over
5 minutes
Learning Technology by Laerdal
*Approximate
[Show More]