You washed your hands.
You should have asked the patient for his consent for letting his daughter be a part of the interview.
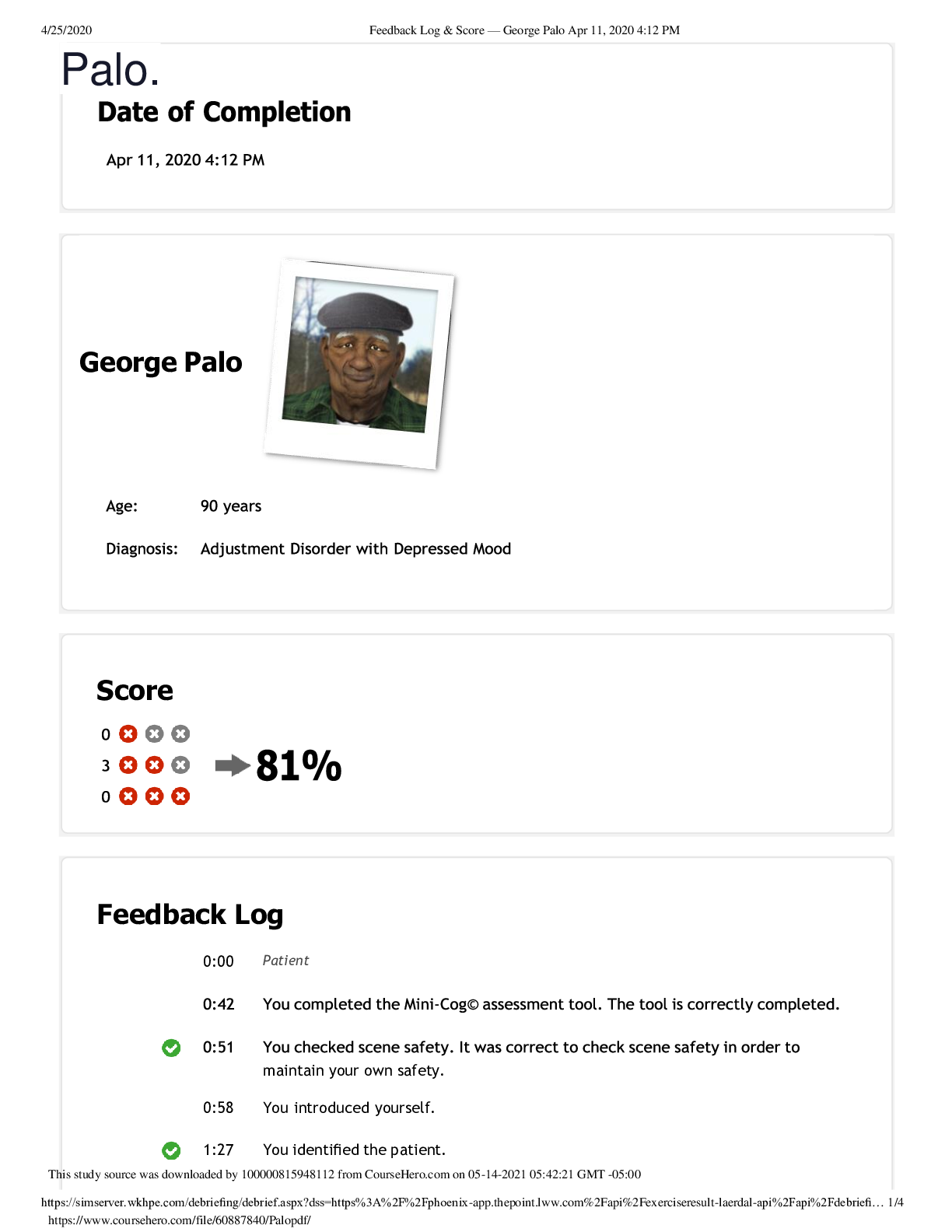
1:57 You asked if the patient had any known allergies.
...
You washed your hands.
You should have asked the patient for his consent for letting his daughter be a part of the interview.
1:57 You asked if the patient had any known allergies.
2:05 You made a safety check of the surroundings and the patient's belongings.
2:24 You called the community nurse.
2:40 You referred the patient to a physician.
3:15 You removed potentially dangerous objects.
3:48 You asked the patient: Can you tell me a little bit more about what's going on with you today? It was appropriate to ask the patient what was going on with him to get an understanding of this.
4:22 The patient said: Sometimes I'm not sure where I am or what is happening. It scares me.\nYou answered: What seems to lead up to those feelings? \nYou used the therapeutic technique of placing the event in time or sequence.
5:05 You asked the patient: Over the past year, when did you feel your best? It was appropriate to ask the patient about when he felt his best.
5:29 The patient said: Max gave me a reason to live and now he's gone too.\nYou answered: Are you saying you feel hopeless? \nYou used the therapeutic technique of translating to feelings.
5:45 You supported the patient about frustrations.
6:00 You supported the patient's daughter about seeing dad ill.
6:09 You supported the patient about loss of wife.
6:33 You asked the patient: Have you ever tried to harm or kill yourself?
6:50 The patient said: Why should I care about myself? I have nothing else to live for.\nYou answered: Mr. Palo, are you considering hurting yourself? \nYou used the therapeutic technique of seeking information.
6:58 You educated about coping.
7:32 You asked the patient: Is it OK for your daughter to be here, while we talk? The patient said: Yes.
8:20 You asked the patient: Do you have any pain? The patient said: No, I don't have any pain.
8:27 You asked the patient: Do you have any difficulty with your breathing? The patient said: No.
8:34 You asked the patient: Have you had any changes in your appetite over the past month?
9:00 The patient said: If I try to eat or shower, I get so tired that I give up.\nYou answered: Physical symptoms are often related to grief. You must miss your wife and Max very much. \nYou used the therapeutic technique of giving information.
9:02 You asked the patient: Tell me about any changes you have had in your sleep over the past few weeks? The patient said: I have a hard time falling asleep. Sometimes I lay in bed for quite some time staring at the clock before I go to sleep, and then I wake up a few times during the night.
9:27 You asked the patient: Do you have energy to do the normal activities necessary to get through the day? The patient said: No, it is not as good as it was, and now I don't have Max to nudge me along, so I find myself sitting on that sofa most of the day.
9:48 You educated about getting active.
10:29 You educated about home care needs.
11:04 You asked the patient: Have you lost interest in activities that you once enjoyed?
The patient said: I used to love to go hunting, but I couldn't really manage that over the past few years so I would watch hunting shows on television. At least it made me remember what it was like to be back there in the woods. But lately I don't even turn the television on.
11:35 You educated about the difference between grief and depression.
12:33 You said: I would like to ask you a few questions and for you to draw a specific thing, which will help me to better assess you. May I ask you these questions? The patient said: Yes.
12:47 You said: Please listen carefully. I am going to say three words that I want you to repeat back to me now and try to remember. The words are banana, sunrise, chair. Please say them for me now. The patient said: Banana, sunrise, chair.
12:52 You said: I want you to draw a clock for me. First, put in all of the numbers where they go. Then, set the hands to ten past eleven. The patient said: Ok.
12:59 You said: What are the three words I asked you to remember? The patient said: Banana...chair I don't know.
13:03 You said: What are the three words I asked you to remember? The patient said: Banana...chair I don't know.
13:28 You assessed the respiration. 13:40 You checked the pulse oximetry.
13:59 You checked the radial pulse.
14:12 You measured the blood pressure.
14:29 You measured the temperature.
14:48 You auscultated the lung sounds. 15:02 You auscultated the heart sounds. 15:23 You checked the patient's skin.
You should have supported Mr. Palo for the loss of his dog. You should have asked about changes in the patient's weight.
15:41 You observed the appearance. 15:52 You assessed the attention.
15:59 You observed the motor activity. 16:09 You assessed the speech.
16:28 You assessed the thought processes.
17:54 You supported the patient about frustrations.
It is important to differentiate between depression and neurocognitive disorder. Sometimes the symptoms of depression can mirror symptoms of neurocognitive disorder. Depression may also exacerbate some of the behavioral and cognitive symptoms that accompany neurocognitive disorder, resulting in some instances in increased aggression, confusion, problems with sleeping and nutrition, or forgetfulness. Changes in speech, inability to reason, or lack of spatial perception would be unusual features of depression but could be impairments seen with neurocognitive disorder. With cases of severe depression, lack of reasoning and memory may mirror that of neurocognitive disorder; however, with appropriate treatment for depression, this feature often reverses, whereas it does not with neurocognitive disorder.lt;/p>lt;p>The relationship between grief and depression is complex, yet the two can be differentiated. Responding to loss of any kind can precipitate feelings of sadness, changes in sleeping and eating patterns, etc. These are not unusual symptoms and generally resolve. Grief symptoms that persist longer than a few months have likely triggered the onset of a depressive episode. Patients should then have a more extensive evaluation, as treatment for depression and grief can significantly improve outcomes.lt;/p>lt;p>Note that changes in physical appearance will require the completion of a physical assessment in addition to assessing mental and cognitive health. The physical assessment will inform how severe the mental and cognitive health deficits are.lt;/p>
[Show More]