*NURSING > QUESTIONS & ANSWERS > South University, Savannah - Pathophysiology NSG5003 Quiz 2 – Resp & Endo. Rated 100% (All)
South University, Savannah - Pathophysiology NSG5003 Quiz 2 – Resp & Endo. Rated 100%
Document Content and Description Below
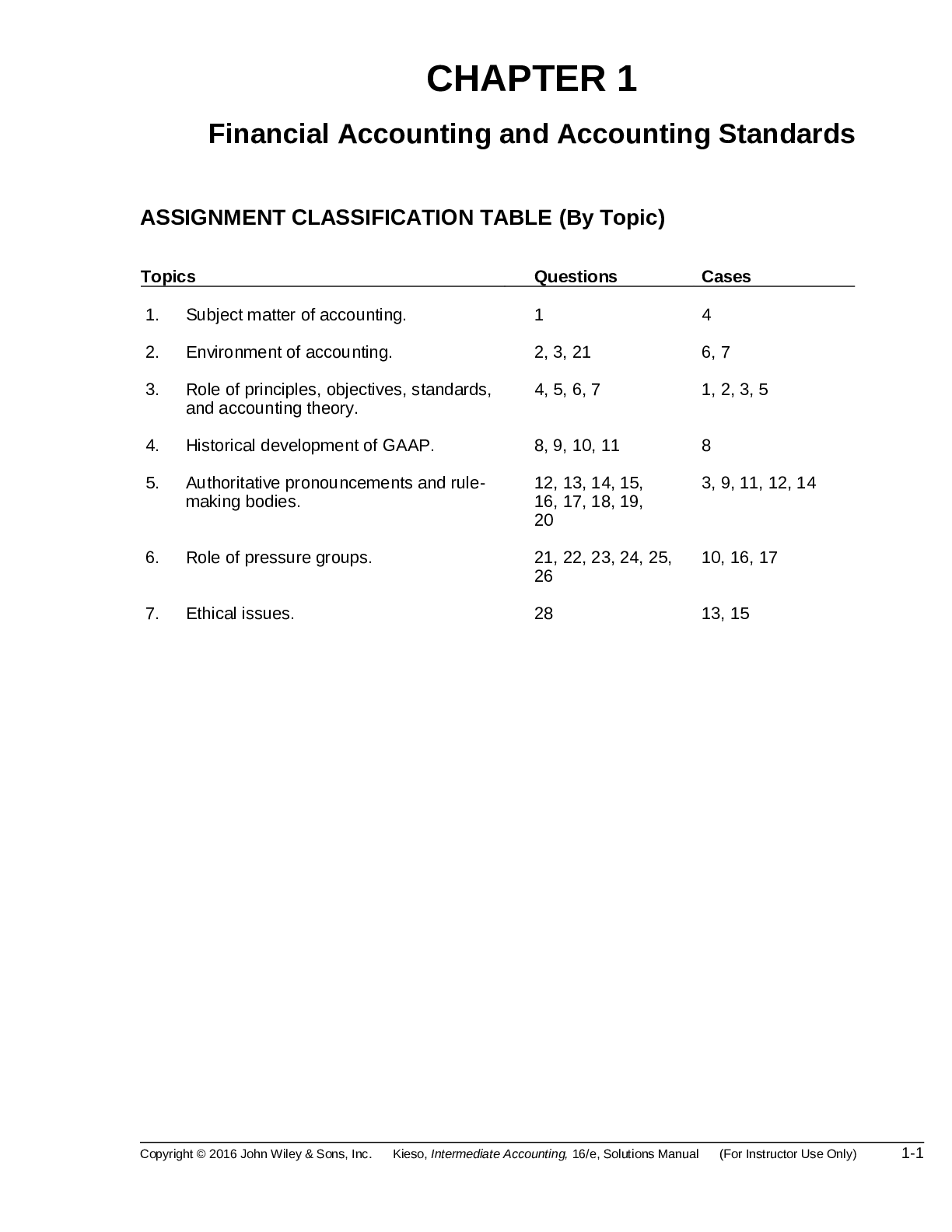
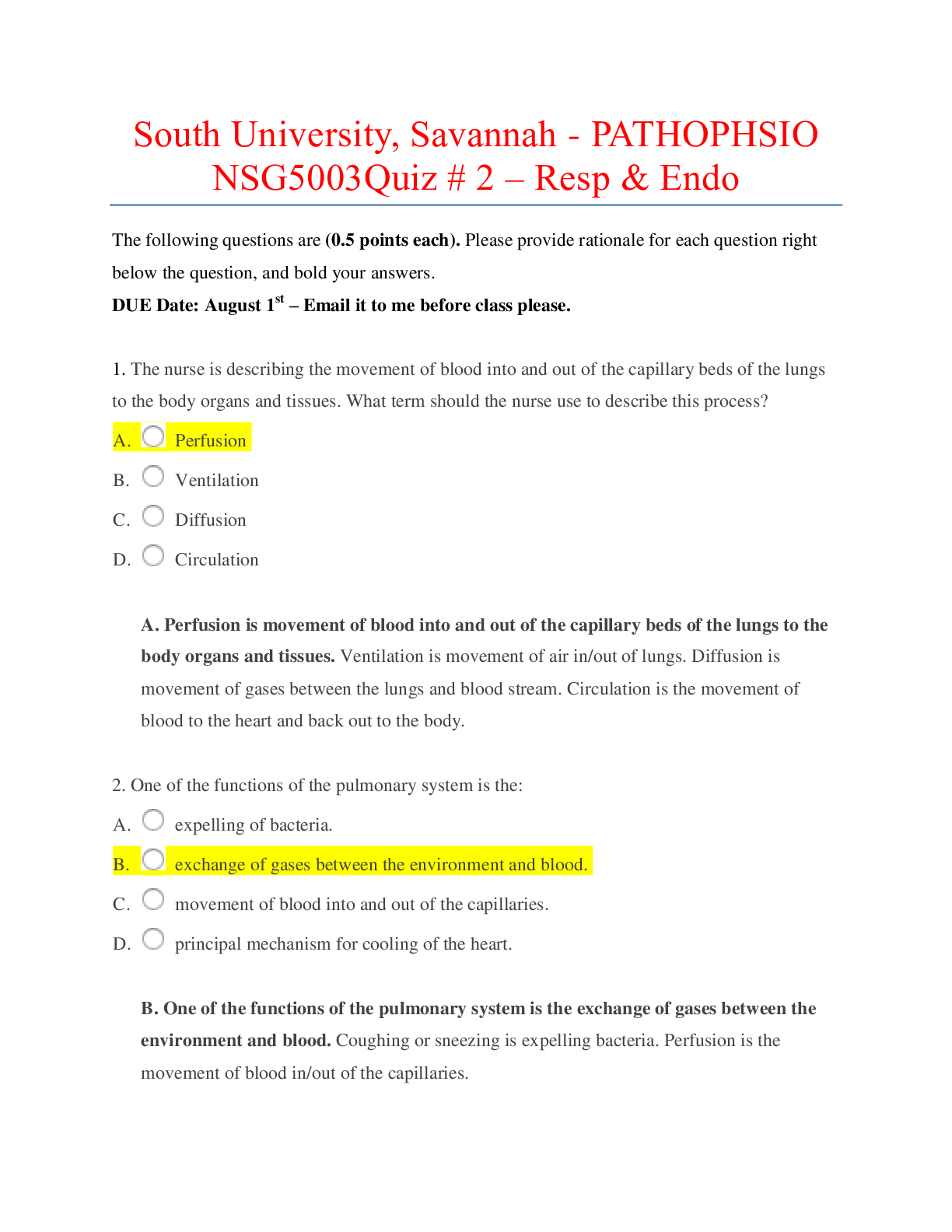
The following questions are (0.5 points each). Please provide rationale for each question right below the question, and bold your answers. DUE Date: August 1st – Email it to me before class please... . 1. The nurse is describing the movement of blood into and out of the capillary beds of the lungs to the body organs and tissues. What term should the nurse use to describe this process? A. Perfusion B. Ventilation C. Diffusion D. Circulation A. Perfusion is movement of blood into and out of the capillary beds of the lungs to the body organs and tissues. Ventilation is movement of air in/out of lungs. Diffusion is movement of gases between the lungs and blood stream. Circulation is the movement of blood to the heart and back out to the body. 2. One of the functions of the pulmonary system is the: A. expelling of bacteria. B. exchange of gases between the environment and blood. C. movement of blood into and out of the capillaries. D. principal mechanism for cooling of the heart. B. One of the functions of the pulmonary system is the exchange of gases between the environment and blood. Coughing or sneezing is expelling bacteria. Perfusion is the movement of blood in/out of the capillaries. 3. A newborn is in respiratory distress and requires ventilation. Tests reveal that he does not produce surfactant due to the absence of: A. mucus-producing cells. B. type II alveolar cells. C. alveolar macrophages. D. goblet cells. B. Type II alveolar cells are responsible for the production of surfactant. Goblet cells produce mucus. Alveolar macrophages ingest foreign material and remove it through the lymphatic system. 4. A patient involved in a motor vehicle accident experiences a severe head injury and dies as a result of the loss of respirations. The nurse suspects the area of the brain most likely damaged is the: A. cerebral cortex. B. thalamus. C. basal ganglia. D. brainstem. D. The brainstem is the respiratory control center. The cerebral cortex is part of the cerebrum. The thalamus is the center for pain perception. Basal ganglia are responsible for voluntary motor control. 5. The nurse is describing the receptors in the lung that decrease ventilatory rate and volume when stimulated. Which receptors is the nurse discussing? A. Carbon dioxide receptors B. Baroreceptors C. Stretch receptors D. Chemoreceptors C. Stretch receptors decrease ventilator rate and volume when stimulated, this is sometimes referred to as the Hering-Breur expiratory reflex. Carbon dioxide receptors are chemoreceptors. Chemoreceptors increase respiratory depth and rate. Baroreceptors function to sense pressure changes by responding to change in the tension of the arterial wall. 6. If an individual with respiratory difficulty were retaining too much carbon dioxide, which of the following compensatory responses would the nurse expect to be initiated? A. Increase in respiratory rate B. Decrease in ventilation rate C. Increase in tidal volume D. Vasodilation of the pulmonary arterioles A. Increase in respiratory rate. An increase of CO2 leads to a decrease in the pH related to the production of hydrogen ions. Increased respiration ventilation causesPaCO2 to decrease and CO2 to diffuse out of the CSF and the pH returns to normal. Decreased ventilation rate would cause the CO2 to go higher. Increased tidal volume. Tidal volume should be kept low for proper oxygenation. Increased CO2 causes vasoconstriction, not vasodilation. 7. During inspiration, muscular contraction of the diaphragm causes air to move into the lung. The mechanism that drives air movement during inspiration results in a(n): A. decrease in intra-alveolar pressure and shortening of the rib cage. B. decrease in the size of the thorax and alveolar expansion. C. increase in the size of the thorax and decrease in intrapleural pressure. D. increase in atmospheric pressure and intrapleural pressure. C. During inspiration, the thorax expands taking in air which creates negative pressure to draw gas into the lungs. The thorax increases and alveolar expansion occurs. The intra-alveolar pressure is decreased and the ribs expands. Pressure in the lungs is decreased to draw gas into the lungs. 8. Surfactant facilitates alveolar distention and ventilation by: A. decreasing thoracic compliance. B. attracting water to the alveolar surface. C. decreasing surface tension in alveoli. D. increasing diffusion in alveoli. C. Surfactant facilitates alveolar distention and ventilation by decreasing surface tension in alveoli, which prevents alveolar collapse. Surfactant does not attract water to alveolar surface, surfactant decreases surface tension which keeps the alveoli free of fluid. Diffusion does not occur in the alveoli, it occurs between the lungs and bloodstream. Decreased thoracic compliance is stiffening of the lungs and is seen in ARDS, pneumonia, or fibrosis. 9. While reviewing the results of the pulmonary functions test, the nurse is aware that the maximum amount of gas that can be displaced (expired) from the lung is called: A. vital capacity (VC). B. total lung capacity. C. functional capacity. D. residual volume. A. Vital capacity is the greatest amount of air that can be expelled from the lungs after taking the deepest breath possible. Total lung capacity is the most amount of air you can take into your lungs on inspiration. Functional capacity is an exam done to evaluate a person’s capacity to perform a variety of activities. Residual volume is the amount of air left over after exhaling. 10. A patient asks how oxygen is transported in the body. The nurse’s best response is that most oxygen (O2) is transported: A. dissolved in the plasma. B. bound to hemoglobin. C. in the form of carbon dioxide (CO2). D. as a free-floating molecule. B. Oxygen is transported in the body by binding to hemoglobin (oxyhemoglobin). Waste products (CO2) and other nutrients are dissolved in the plasma. A free radical is a free-floating molecule. CO2 is transported out of the body during respiration. 11. In a patient with acidosis, the nurse would expect the oxyhemoglobin dissociation curve to shift: A. to the right, causing more O2 to be released to the cells. B. to the left, allowing less O2 to be released to the cells. C. downward, allowing less O2 to dissolve in the plasma. D. upward, allowing more O2 to dissolve in the plasma. A. In a patient with acidosis, a shift to the right, which causes more oxygen to be released to the cells (tissues) due to increased CO2 in the blood. A shift to the left is seen in alkalosis, this allow less oxygen to be released to the cells (tissues) due to decreased CO2 in the blood. CO2 is dissolved in the plasma. 12. Carbon dioxide (CO2) is mainly transported in the blood: A. attached to oxygen (O2). B. dissolved in red blood cells. C. combined with albumin. D. in the form of bicarbonate. D. Approximately 60% of CO2 in venous blood and 90% of CO2 in arterial blood are carried in the form of bicarbonate. CO2 is buffered in the RBCs where it becomes bicarbonate. CO2 does not attach to oxygen or combine with albumin. 13. A 10-year-old develops pneumonia. Physical exam reveals subcostal and intercostal retractions. The child reports that breathing is difficult with feelings that, “I cannot get enough air.” What term should the nurse use to document this condition? A. Cyanosis B. Dyspnea C. Hyperpnea D. Orthopnea B. Dyspnea is a subjective sensation of uncomfortable breathing or feeling of shortness of breath. Orthopnea is difficulty breathing while lying down. Hyperpnea is an increased breathing rate. Cyanosis is blue color of skin, lips, nails. 14. What type of breathing will the nurse observe while assessing a patient experiencing both metabolic acidosis and Kussmaul respirations? A. Audible wheezing or stridor B. Increased rate, large tidal volumes, and no expiratory pause C. Rapid respirations with periods of apnea D. Very slow inhalations and rapid expirations B. Kussmaul respirations (hyerpnea) is an increased ventilatory rate, large tidal volume, and no expiratory pause. Audible wheezing or stridor are sounds. Rapid respirations with periods of apnea are Cheyne-Stokes respirations. 15. As a result of a severe head injury, a patient is now experiencing respiratory abnormalities characterized by alternating periods of deep and shallow breathing with periods of apnea. What term should the nurse use when charting this condition? A. Cheyne-Stokes B. Frank-Starling C. Apnea D. Orthopnea A. Cheyne-Stokes respirations consist of alternating deep and shallow breathing with periods of apnea. Apnea is the temporary cessation of breathing. Orthopnea with difficulty breathing while lying flat. Frank-Starling is related to the length-tension relationship of the cardiac muscle. 16. A patient’s arterial blood gas reveals decreased carbon dioxide (CO2) levels. What is the most likely cause of this situation? A. Hyperventilation B. Hypoventilation C. Apnea D. Cyanosis A. Hyperventilation leads to hypocapnea (decreased CO2) due to CO2 being removed from the lungs at a faster rate than it is produced. Hypoventilation causes CO2 build up because it is not being removed as production continues. Apnea is the temporary cessation of breathing. Cyanosis is the bluish discoloration of skin & mucous membranes. 17. A nurse is reviewing the results of an arterial blood gas (ABG) and finds reduced oxygenation of arterial blood. What term should the nurse use to describe this condition? A. Ischemia B. Hypoxia C. Hypoxemia D. Hypocapnia C. Hypoxemia is reduced oxygenation of arterial blood. Ischemia is inadequate blood supply to an organ or part of the body. Hypoxia is reduced oxygen of cells in tissues. Hypocapnea is a decreased amount of CO2. 18. A 50-year-old presents with hypotension, hypoxemia, and tracheal deviation to the left. Tests reveal that the air pressure in the pleural cavity exceeds barometric pressure in the atmosphere. Based upon these assessment findings, what does the nurse suspect the patient is experiencing? A. Pleural effusion B. Tension pneumothorax C. Open pneumothorax D. Transudative pneumothorax B. A tension pneumothorax is a site of pleural rupture that acts as a one way valve allowing air into the lung but not letting it escape during expiration. Pleural effusion is fluid in the pleural space. With an open pneumothorax air that is drawn into the airspace in inspiration is forced back out during expiration. Transudative is not a kind of pneumothorax. 19. The most common cause of pulmonary edema is: A. right heart failure. B. left heart failure. C. asthma. D. lung cancer. B. Left sided heart failure (CHF) is the inability of the heart to generate adequate output to perfuse tissues. Right sided heart failure leads to peripheral edema. Asthma is bronchial inflammation. Lung cancer is not a cause of pulmonary edema. 20. A 42-year-old presents with dyspnea; rapid, shallow breathing; inspiratory crackles; decreased lung compliance; and hypoxemia. Tests reveal a fulminant form of respiratory failure characterized by acute lung inflammation and diffuse alveolocapillary injury. What is the most likely diagnosis supported by the patient’s condition? A. Acute respiratory distress syndrome (ARDS) B. Sarcoidosis C. Postoperative respiratory failure D. Malignant respiratory failure A. ARDS is characterized by edema and atelectasis, inflammation and diffuse alveolocapillary injury. Sarcoidosis is a disease that involves abnormal collections of inflammatory cells that for granulomas. Post-op respiratory failure occurs after surgery and the patient has not had surgery recently. 21. Airway obstruction contributing to increased airflow resistance and hypoventilation in asthma is caused by: A. type II alveolar cell injury and decreased surfactant. B. alveolar fibrosis and pulmonary edema. C. mucous secretion, bronchoconstriction, and airway edema. D. collapse of the cartilaginous rings in the bronchi. C. Mucous secretion, bronchoconstriction and airway edema are indicators of asthma, in late asthmatic response obstruction from mucous plugs can form leading to hypoventilation and hypoxemia. Alveolar fibrosis and pulmonary edema are related to ARDS. The bronchi do not have cartilaginous rings. Decreased surfactant is seen in premature infants and causes RDS. 22. Which of the following patients is at highest risk for developing pulmonary embolism (PE)? A. 21-year-old male with a hemophilia bleeding disorder B. 28-year-old woman who had a baby 6 months earlier C. 36-year-old woman with a history of alcohol abuse who is recovering from a gastric ulcer D. 72-year-old male who is recovering from hip replacement surgery in the hospital D. a 72 year old who is recovering from hip replacement surgery in the hospital is more at risk for PE due to increased risk of DVT related to decreased mobility from surgery. 23. A newborn is diagnosed with respiratory distress syndrome. When obtaining the patient’s history, which of the following is the most important predisposing factor for this condition? A. Low birth weight B. Alcohol consumption by the mother during pregnancy C. Premature birth D. Smoking by the mother during pregnancy C. The more premature the infant, the higher the risk for RDS. Decreased surfactant is seen in premature infants. It is produced by 20-24 weeks gestation and is secreted into the fetal airways by 30 weeks gestation. 24. To help confirm a diagnosis of cystic fibrosis in a 1-year-old child which substance will be monitored for in the child’s sweat? A. Potassium B. Chloride C. Magnesium D. Carbonic acid B. Chloride transport is abnormal in cystic fibrosis 25. Which control mechanism will a patient’s target cells implement in order to adapt to high hormone concentrations? A. Negative feedback B. Positive feedback C. Down-regulation D. Up-regulation C. Down regulation occurs when high concentrations of hormones decrease the number of receptors. Negative feedback occurs when you have enough of something and need production to stop; opposite for positive feedback. 26. When a staff member asks the nurse which gland secretes ADH and oxytocin, how should the nurse respond? A. Anterior pituitary B. Posterior pituitary C. Hypothalamus D. Pineal B. The posterior pituitary gland secretes ADH & oxytocin. Anterior pituitary gland produces ACTH, TSH, FSH, LH, MSH, GH & Prolactin. Pineal produces Melatonin. 27. If a patient’s posterior pituitary is removed, which hormone would the nurse expect to decrease? A. PRF B. ADH C. ACTH D. Growth hormone (GH) B. ADH is produced in the posterior pituitary gland 28. Which assessment finding would the nurse expect to be increased in a patient with deficient ADH production? A. Blood volume B. Urine osmolality C. Urine volume D. Arterial vasoconstriction C. Deficient ADH relates to diabetes insipidus which is characterized by increased output of dilute urine due to excessive thirst. Urine volume is 8-12L per day in a person with diabetes insipidus. 29. A 70-year-old female has brittle bones secondary to osteoporosis. Her primary care provider prescribes calcitonin to: A. activate vitamin D. B. stimulate osteoclastic activity. C. inhibit calcium resorption from bones. D. promote thyroid hormone release C. Calcitonin lowers serum calcium levels by inhibiting bone-reabsorbing osteoclasts. It is used in the treatment of osteoporosis. 30. A 40-year-old patient undergoes surgery for a PTH-secreting tumor in which the parathyroid is removed. Which physiological alteration would the nurse expect following surgery? A. Increased serum calcium B. Decreased bone formation C. Decreased calcium reabsorption in the kidney D. Increased calcitonin C. PTH promotes calcium reabsorption in the kidney so if a PTH-secreting tumor is removed, less calcium is absorbed. Calcitonin reduces blood calcium levels. PTH causes increased calcium in the blood. 31. A patient with one kidney underwent surgery for an adrenal tumor that removed a large portion of the zona glomerulosa. The nurse would expect a postsurgical decrease in the patient’s: A. sodium. B. aldosterone. C. potassium. D. acid. B. If a large portion of the zona glomerulosa was removed, the nurse would expect a postsurgical decrease in aldosterone because aldosterone is produced by the zona glomerulosa. 32. If the patient has a problem with the pineal gland, which substance would the nurse monitor? A. Melatonin B. Epinephrine C. Cortisol D. Somatostatin A. Melatonin is secreted by the photoreceptive cells that make up the pineal gland. 33. A 54-year-old patient with pulmonary tuberculosis is evaluated for syndrome of inappropriate ADH secretion (SIADH). Which electrolyte imbalance would be expected in this patient? A. Hyponatremia B. Hyperkalemia C. Hypernatremia D. Hypokalemia A. With SIADH, there is increased water reabsorbed by the kidneys and higher urine osmolality, causing more sodium to leave the body. 34. A 44-year-old patient with pulmonary tuberculosis is evaluated for SIADH. Which assessment finding would support this diagnosis? A. Peripheral edema B. Tachycardia C. Low blood pressure D. Concentrated urine D. The urine has a higher osmolality, which is higher concentration, due to water retention in the kidneys. 35. A patient is admitted to the intensive care unit with a closed head injury sustained in a motorcycle accident. The injury has caused severe damage to the posterior pituitary. Which of the following complications should the nurse anticipate? A. Dilutional hyponatremia B. Dehydration from polyuria C. Cardiac arrest from hyperkalemia D. Metabolic acidosis B. Damage to the posterior pituitary gland would cause hypofunction of the gland which is linked to diabetes insipidus. With diabetes insipidus there is insufficient ADH which causes increased urine output (polyuria) which can lead to dehydration and hypernatremia. 36. Which assessment result would the nurse expect to find associated with a patient diagnosed with Graves disease? A. High levels of circulating thyroid-stimulating autoantibodies B. Ectopic secretion of thyroid-stimulating hormone (TSH) C. Low circulating levels of thyroid hormones D. Increased circulation of iodine A. High levels of circulating thyroid-stimulating antibodies, called thyroid-stimulating immunoglobins (TSI), resulting in Graves disease. The TSI are responsible for the manifestations of pre-tibial myxedema (leg swelling) and opthalmopathy (exophthalmos or protruding eyeballs) 37. Visual disturbances are a common occurrence in patients with untreated Graves disease. The endocrinologist explains to the patient that the main cause of these complications is: A. decreased blood flow to the eye. B. orbital edema and protrusion of the eyeball. C. TSH neurotoxicity to retinal cells. D. local lactic acidosis. B. Orbital edema and protrusion of the eyeball are due to infiltrative changes involving orbital contents with enlargement of ocular muscles. 38. What is the purpose of the glycosylated hemoglobin (hemoglobin A1c) test? A. Measuring fasting glucose levels. B. Monitoring long-term serum glucose control. C. Detecting acute complications of diabetes. D. Checking for hyperlipidemia. B. Glycosylated hemoglobin (HgA1c )refers to the permanent attachment od glucose to hemoglobin molecules and reflects the average plasma glucose over the life of the red blood cell (120 days). 39. An 11-year-old is newly diagnosed with type 1 DM. Which classic symptoms should the nurse assess the patient for? A. Recurrent infections, visual changes, fatigue, and paresthesia B. Polydipsia, polyuria, polyphagia, and weight loss C. Vomiting, abdominal pain, sweet, fruity breath, dehydration, and Kussmaul breathing D. Weakness, vomiting, hypotension, and mental confusion B. Type 1 diabetes clinical manifestations are polydipsia, polyuria, polyphagia, weight loss and fatigue. Type 1 DM is the most common form of diabetes for those under age 12. 40. 19-year-old female with type 1 DM was admitted to the hospital with the following lab values: serum glucose 500 milligrams per deciliter (high), urine glucose and ketones 4+ (high), and arterial pH 7.20 (low). Her parents state that she has been sick with the “flu” for a week. Which of the following statements best explains her acidotic state? A. Increased insulin levels promote protein breakdown and ketone formation. B. Her uncontrolled diabetes has led to renal failure. C. Low serum insulin promotes lipid storage and a corresponding release of ketones. D. Insulin deficiency promotes lipid metabolism and ketone formation. D. With type 1 DM, there is an insulin deficiency which breaks down lipids/fats leading to hyperglycemia. Glucose accumulates in the blood and appears in the urine as ketones because the renal threshold for glucose has exceeded. Following are extra credit question (0.5 point each) – Do not need Rationales for this 41. A nurse checks lab results as both Cushing disease and Addison disease can manifest with elevated levels of: A. ADH. B. estrogen. C. adrenocorticotropic hormone (ACTH). D. aldosterone. Answer: C - ACTH 42. Which of the following alterations would the nurse expect to find in a patient with untreated Cushing disease or syndrome? A. Bradycardia B. Tachypnea C. Hyperkalemia D. Hypertension Answer: D - Hypertension 43. Which symptom would the nurse expect in a patient diagnosed with hyperaldosteronism? A. Hypovolemia B. Hypotension C. Hypokalemia D. Hyponatremia Answer: C - Hypokalemia 44. A patient diagnosed with Addison disease reports weakness and is easily fatigued. What is the root of these symptoms? A. Hyperkalemia B. Hypoglycemia C. Hypocortisolism D. Metabolic acidosis Answer: C - Hypocortisolism [Show More]
Last updated: 2 years ago
Preview 1 out of 18 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$10.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Jul 14, 2020
Number of pages
18
Written in
Additional information
This document has been written for:
Uploaded
Jul 14, 2020
Downloads
0
Views
131