Talent Acquisition and Employee Retention Plan | Download for quality grades |
$ 2
WGU C810 A communication plan is being developed to reduce mistrust and miscommunication in a healthcare setting.
$ 7
ABRET PRACTICE EXAM PART 1
$ 10.5
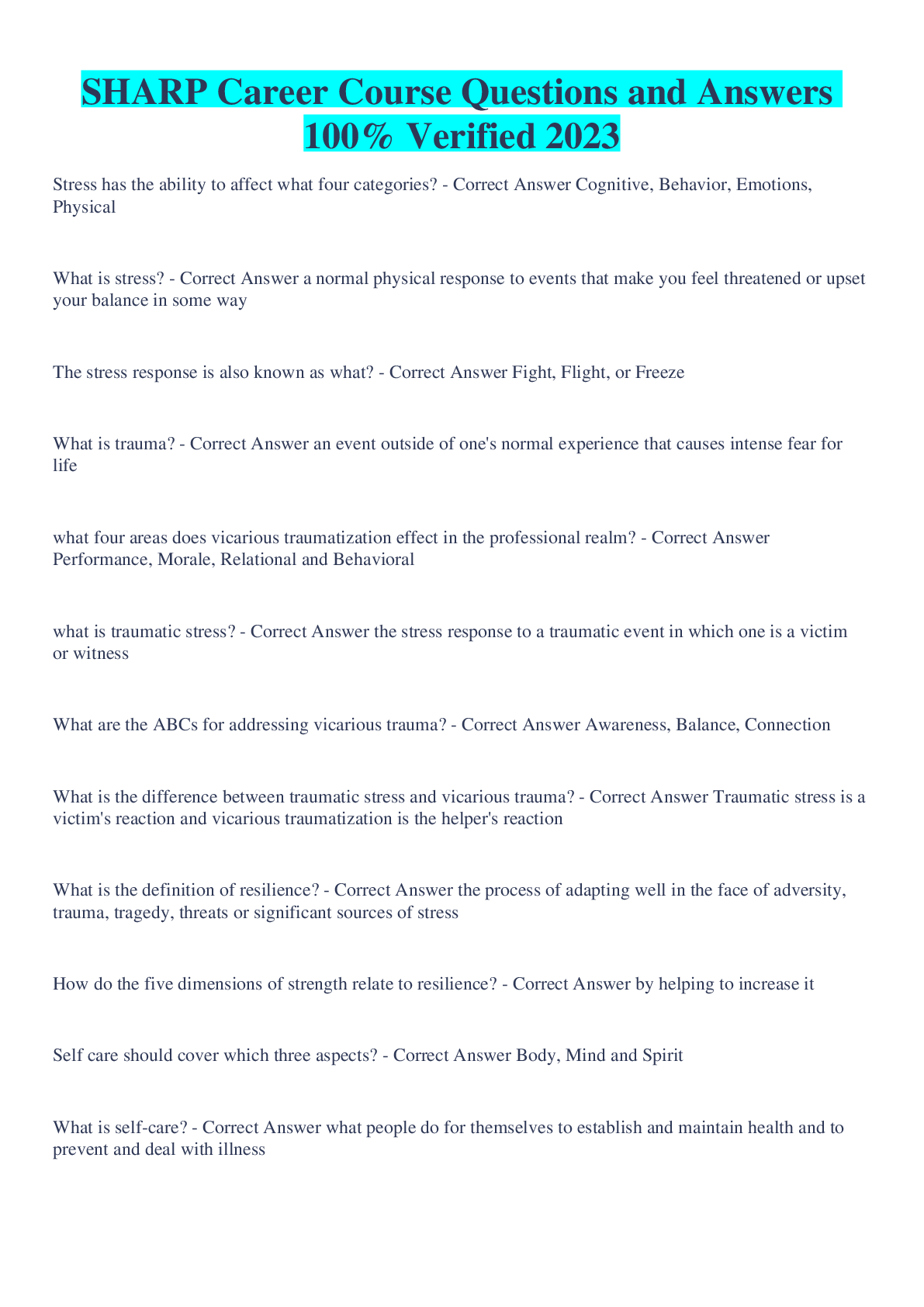
SHARP Career Course Questions and Answers 100% Verified 2023
$ 9.5
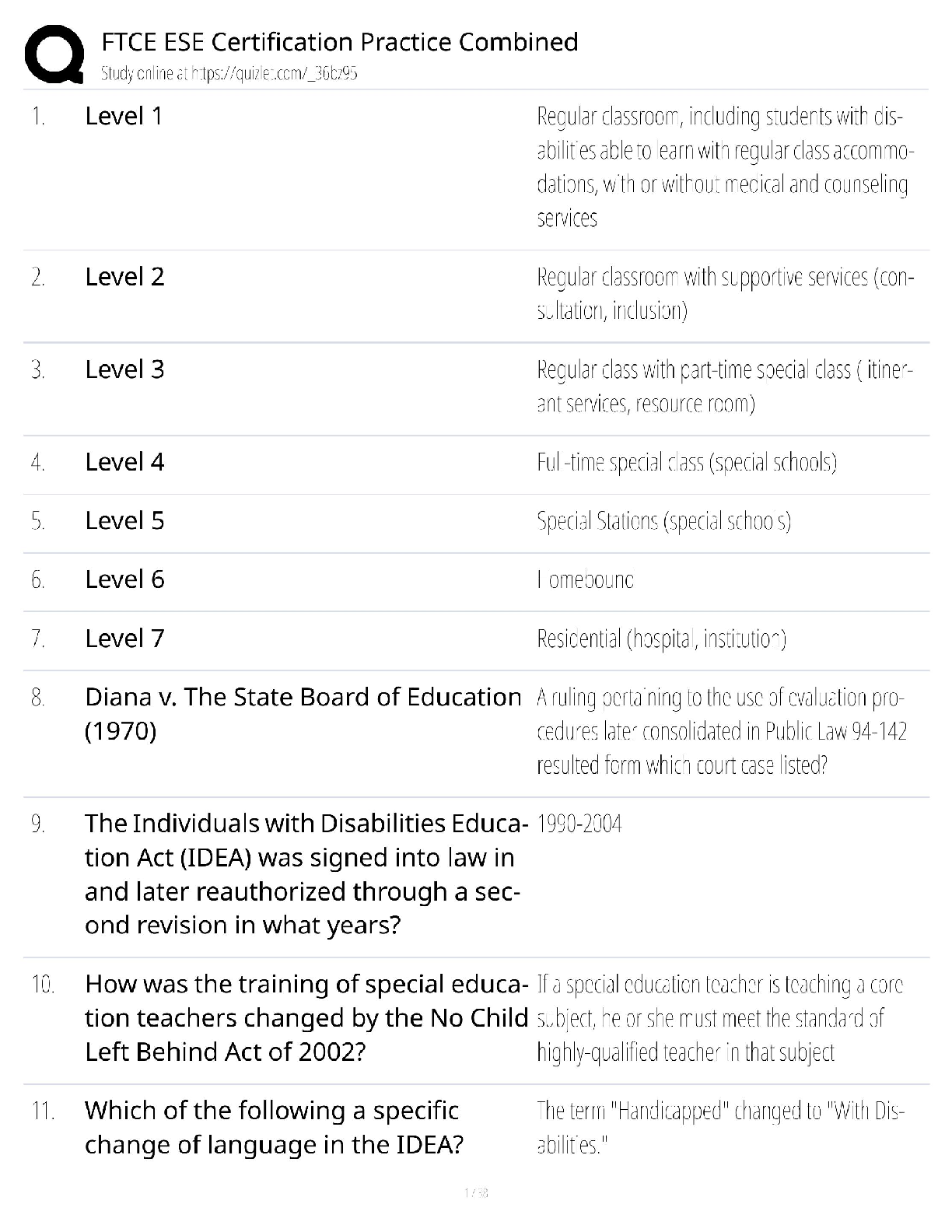
FTCE ESE Certification Practice 2024 (K-12 Combined) / Florida Teacher Exam Prep / Inclusion & Special Ed Test Bank / Pass Guaranteed
$ 15.5
eBook Orchids For Dummies 1st Edition By Steven A.Frowine, National Gardening Association
$ 30
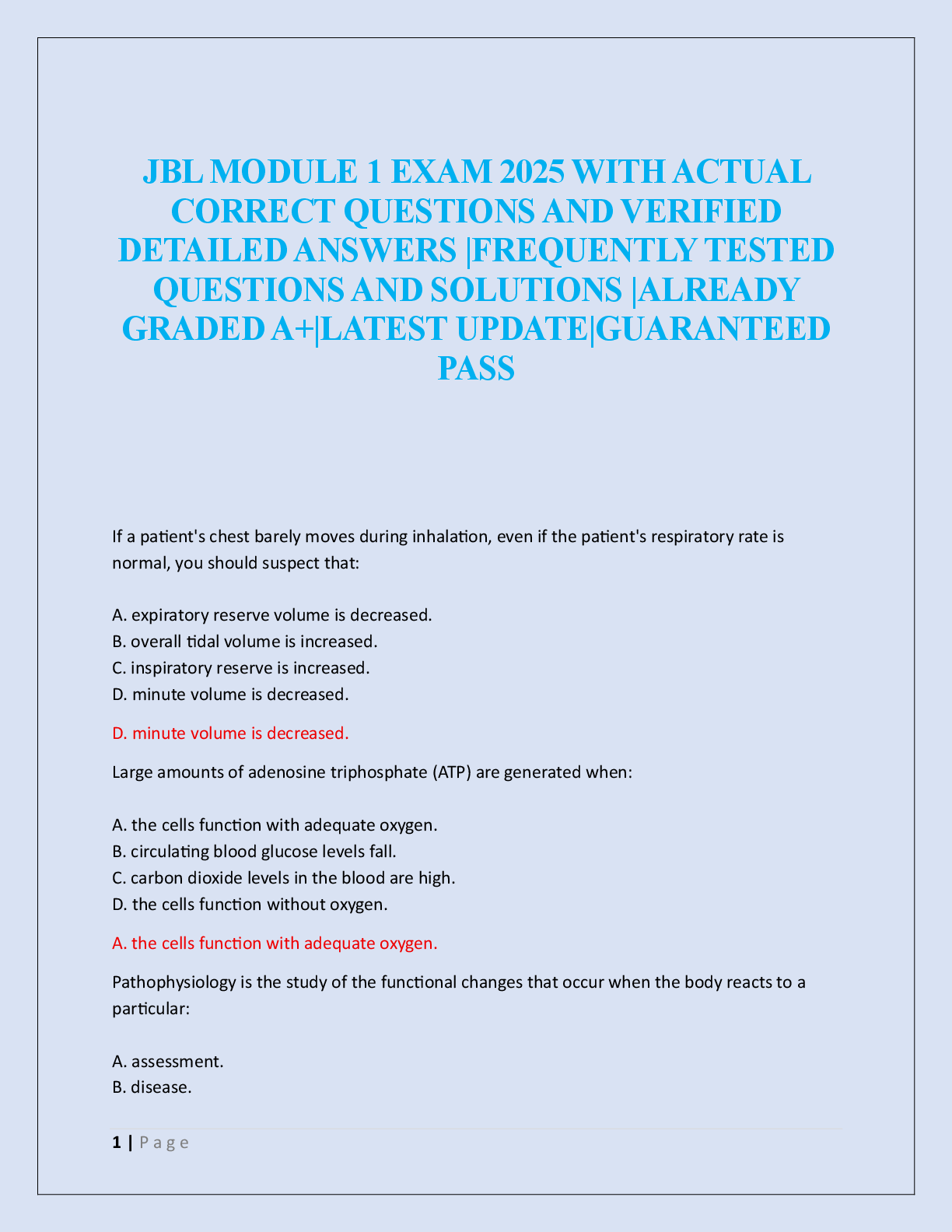
JBL MODULE 1 EXAM 2025
$ 20.5
Quiz# 3.doc
$ 10
Pathophysiology Final Exam Study Guide Modules 1-10
$ 10
BIOD 171 EXAM MODULE 5
$ 12
BIOL 235 Midterm Exam 2 With Complete Solution(100% Verified) 185 Questions with 100% Correct Answers
$ 10
NES Special Education Exam 601 Questions and Answers with Certified Solutions
$ 10
TEXAS CDL AIR BRAKES EXAM, PRACTICE EXAM AND STUDY GUIDE NEWEST 2025 ACTUAL EXAM 60 QUESTIONS AND CORRECT DETAILED ANSWERS
$ 14.5
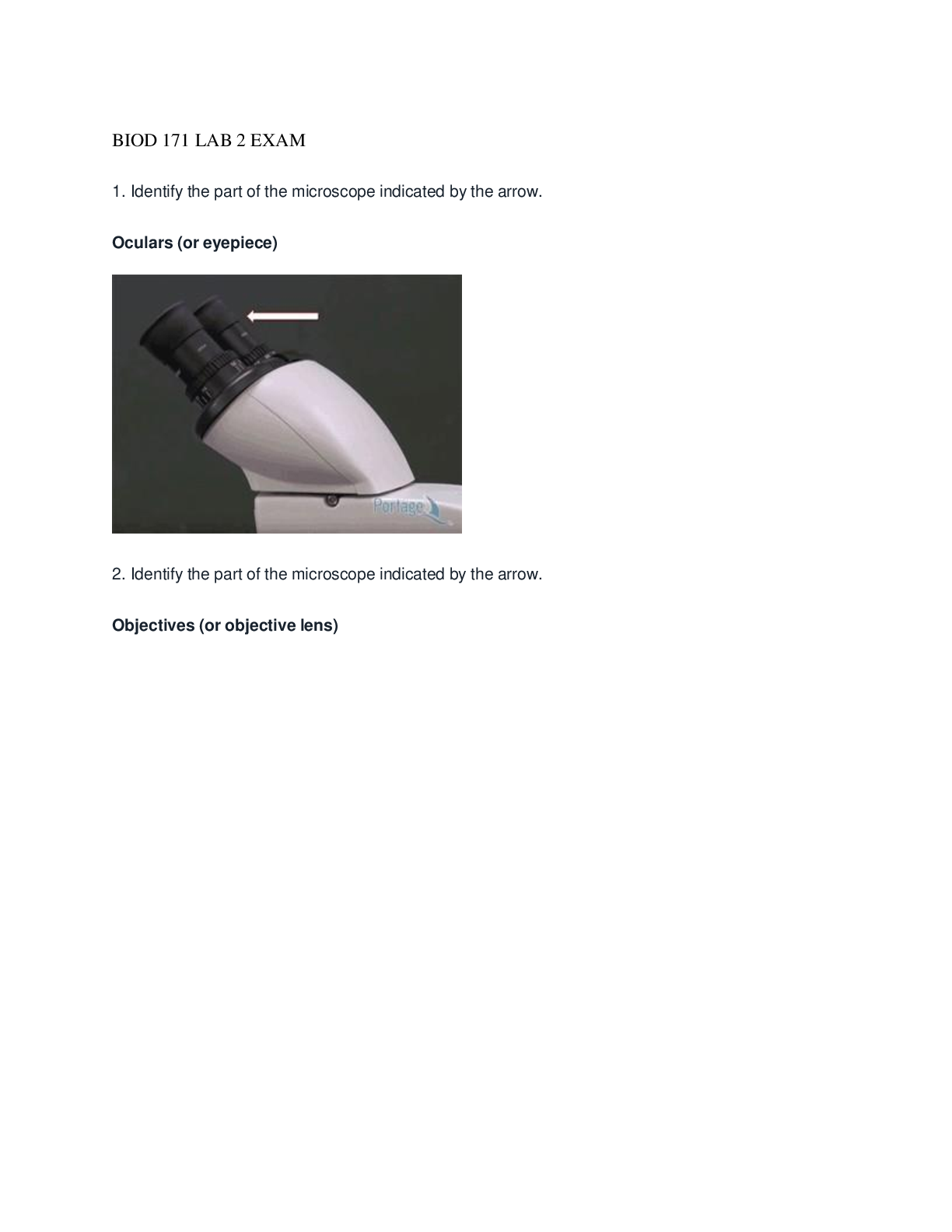
BIOD 171 LAB 2 EXAM
$ 11
HESI A2 COMPREHENSIVE NURSING ENTRANCE EXAM- Complete Test Banks- All subjects with tips and guidelines
$ 31

Quiz# 7.doc
$ 10.5

HUM 115 Week 5 Critical Thinking Scenario; Essay | 100% Verified
$ 7
eBook PDF Introduction to Communication Disorders A Lifespan Evidence-Based Perspective 7th Edition By Robert Owens, Kimberly Farinella
$ 30
.png)
University of Florida - EEL 6509chapter09 problems
$ 3
Technological Design and Problem Solving Sample Questions Answer
$ 10
HESI PHARMACOLOGY ACTUAL EXAM QESTIONS 2023/2024
$ 9.5

Winged Corkscrew Description
$ 9
HAP midterm banks
$ 9
PALS HEARTCODE 2025 EXAM, PRACTICE EXAM AND STUDY GUIDE NEWEST 140 QUESTIONS AND CORRECT DETAILED ANSWERS WITH RATIONALES (VERIFIED ANSWERS) ALREADY GRADED A+
$ 17.5
eBook Metabolomics for Personalized Vaccinology 1st Edition By Mahbuba Rahman
$ 30
eBook High Performance Python Practical Performant Programming for Humans 3rd Edition By Micha Gorelick , Ian Ozsvald
$ 30
[eTextBook] [PDF] (Scan Copy) A Modern Approach to Quantum Mechanics 2nd Edition By John Townsend
$ 15

CSE 565 – Software Verification and Validation Project #1 Part 2 – Design of Experiments | Download for quality grades |
$ 3
eBook [PDF] Kinks and Domain Walls An Introduction to Classical and Quantum Solitons 1st Edition By Tanmay Vachaspati

![Preview image of PN1-Exam-2-Study-Guide (Complete solution graded A] document](https://scholarfriends.com/storage/PN1_Exam_2_Study_Guide__Complete_.png)




 (2).png)

.png)